Abstract
The essential package of palliative care for cervical cancer (EPPCCC), described elsewhere, is designed to be safe and effective for preventing and relieving most suffering associated with cervical cancer and universally accessible. However, it appears that women with cervical cancer, more frequently than patients with other cancers, experience various types of suffering that are refractory to basic palliative care such as what can be provided with the EPPCCC. In particular, relief of refractory pain, vomiting because of bowel obstruction, bleeding, and psychosocial suffering may require additional expertise, medicines, or equipment. Therefore, we convened a group of experienced experts in all aspects of care for women with cervical cancer, and from countries of all income levels, to create an augmented package of palliative care for cervical cancer with which even suffering refractory to the EPPCCC often can be relieved. The package consists of medicines, radiotherapy, surgical procedures, and psycho-oncologic therapies that require advanced or specialized training. Each item in this package should be made accessible whenever the necessary resources and expertise are available.
INTRODUCTION
Cervical cancer, the fourth most common cancer in women globally and the most common cause of cancer-related death in sub-Saharan Africa,1 is associated with suffering that is more prevalent, complex, and severe than that associated with other malignancies.2,3 Elsewhere, we reported that women with cervical cancer have a higher prevalence of moderate or severe pain, anxiety, and depression than patients with cancer on average.2 They also suffer from a high prevalence of moderate or severe malodorous vaginal discharge, bleeding, sexual dysfunction, and financial distress, and more than 40% are abandoned by their intimate partners.2 In light of this extraordinarily prevalent, severe, and complex suffering, we convened a panel of experts in treatment and palliative care of women with cervical cancer to devise an essential package of palliative care for cervical cancer (EPPCCC).3
CONTEXT
Key Objective
Existing evidence indicates that patients with cervical cancer, more often than patients with other cancers, experience suffering that is refractory to basic palliative care such as what can be provided with an essential package of palliative care for cervical cancer. Therefore, a panel of experts in all aspects of cervical cancer treatment and palliation created an augmented package of palliative care for cervical cancer intended to make possible relief even of refractory suffering.
Knowledge Generated
The augmented package of palliative care for cervical cancer consists of carefully selected medicines, radiotherapy, nerve blocks, surgical procedures, and psycho-oncologic therapies that require advanced or specialized training. Each item in this package should be made accessible whenever the necessary resources and expertise are available.
Relevance
The augmented package of palliative care for cervical cancer will make possible relief of many types of severe, refractory suffering due not only to cervical cancer but also any cancer or serious illness.
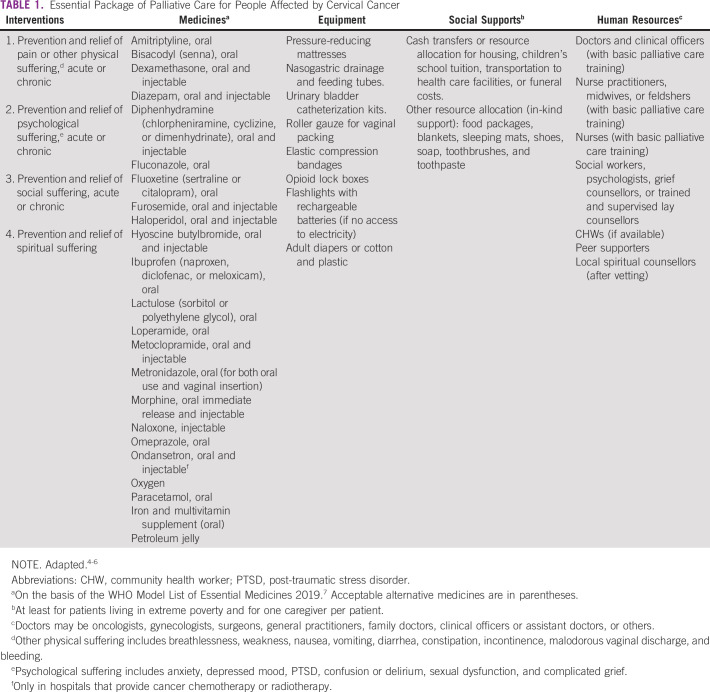
The EPPCCC, described elsewhere and summarized in Table 1, is designed to be the minimum package that can safely and effectively prevent and relieve most suffering associated with cervical cancer, to be applicable by any clinicians with basic palliative care training, and to be inexpensive enough to be made universally accessible free of charge to the patient even in the lowest-income settings.3 However, both available evidence and expert opinion suggest that cervical cancer frequently results in suffering too severe, complex, or refractory to be adequately relieved by basic palliative care.8-11 A variety of anatomic, physiologic, psychological, and social factors appear to contribute to this phenomenon. For example, the proximity of major nerve plexuses to the cervix makes them susceptible to tumor invasion that often results in severe or refractory neuropathic pain.8,12 The large blood supply to the uterus and vagina puts patients with cervical cancer at risk of difficult-to-control hemorrhage,13-15 and disruption by necrotic tumor of the vaginal microbial environment often results in difficult-to-treat, psychosocially disabling vaginal discharge.15,16 The proximity of the cervix to bowel and bladder puts patients at risk for bowel obstruction with resultant intractable vomiting; rectovaginal, vesicovaginal, and enterovesical fistulae with distressing leakage of stool and urine; and hydronephrosis with resultant renal failure. These distressing problems may be palliated best by surgical procedures.17 Severe psychosocial suffering that is difficult to relieve may result when invasive cervical cancer or its treatment injures the genitals and causes sexual dysfunction.18,19
TABLE 1.
Essential Package of Palliative Care for People Affected by Cervical Cancer
These data suggest that women with cervical cancer often experience suffering too severe, complex, or refractory to be controlled by basic palliative care. Thus, the group of experienced experts in cervical cancer treatment and palliation from countries of all income levels that created the EPPCCC agreed that an augmented package was necessary as a supplement to the EPPCCC. The augmented package includes the following:
Palliative radiotherapy
Advanced medical therapies
Nerve blocks for pain control
Palliative surgery
Psycho-oncology.
Governments should assure that the EPPCCC is universally accessible before approving even partial insurance coverage of expensive elements of the augmented package for which the poor may be unable to afford the co-payment. However, all governments should aspire to make accessible as much as possible of the augmented package as soon as possible. Implementation of each element of the augmented package requires advanced or specialist training in one or more of several disciplines: palliative care, radiation oncology, pain medicine, surgery, or psychiatry. Thus, the effort to make the augmented package accessible must entail efforts to create capacity for training in these disciplines wherever it is inadequate or nonexistent. Implementation of both packages will benefit not only women with cervical cancer but also patients with any serious illness.
PALLIATIVE RADIATION THERAPY
Patients with cervical cancer in low- and middle-income countries (LMICs) frequently present with locally advanced disease and associated symptoms.20,21 For these patients, palliative external beam radiation therapy (EBRT) often can provide rapid relief of vaginal bleeding or discharge and of pain because of the primary lesion, nodal disease, or metastatic disease in the mediastinum, neck, bone, or brain.22 Yet radiotherapy often is difficult or impossible to access in LMICs. Thus, making EBRT universally accessible with simple, reliable machines is crucial to fulfill the human right of patients with cancer to the highest attainable standard of health.23
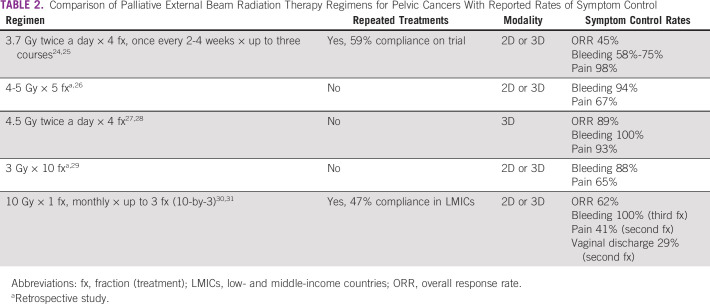
The most common palliative EBRT regimens for symptomatic pelvic cancers are shown in Table 2. They are ordered from most commonly used to least commonly used globally. Choice of regimen should be based on the patient's prognosis, specific symptoms, performance status, ability to attend the radiotherapy center, and capacity of the treating center.22,26,32,33 Short regimens, such as 3.7 Gy twice daily for four fractions and up to three courses or 4-5 Gy daily for five fractions, are favored to balance effective symptom palliation with minimum logistical burden for patients, particularly when the prognosis may be limited. Conventional palliative regimens, such as 3 Gy for 10 fractions, are also safe and effective. However, they may be more burdensome for both patients and treatment centers and do not offer better symptom response. Single treatment regimens, such as 10 Gy for one fraction, offer convenience but have higher toxicity.
TABLE 2.
Comparison of Palliative External Beam Radiation Therapy Regimens for Pelvic Cancers With Reported Rates of Symptom Control
Ideally, radiotherapy clinics should be distributed widely enough to assure universal access and should be officially and operationally integrated with comprehensive palliative care services.34-36 Living accommodations should be made available for patients who must spend one or more nights at the radiotherapy facility. All radiation oncologists should have intermediate-level palliative care training, at least 60 hours per WHO recommendation, to promote this integration and to help assure an appreciation for the full spectrum of palliative interventions.37 Conversely, all levels of palliative care training should include instruction on indications for radiotherapy.38 Available evidence indicates good economic return on investment in radiation therapy in LMICs, especially for cervical cancer.36,39
ADVANCED MEDICAL THERAPIES
In addition to the medicines in the EPPCCC, several others can significantly improve comfort of women in specific clinical situations such as advanced-stage kidney disease or neuropathic pain refractory to all other medicines in the EPPCCC.4,6 Some of these medicines are more expensive than those in the EPPCCC, and others are not as well-studied, but they should be made accessible whenever possible for patients with these conditions. However, morphine in oral fast-acting and injectable preparations should be accessible to everyone in need before any more expensive opioid preparations are made available.40
Lidocaine, Injectable
For moderate or severe pain that is refractory to opioids, or when opioids cause intolerable adverse effects, particularly near the end of life, an intravenous bolus (1-2 mg/kg over 30 minutes) can be given.41,42 If the bolus provides relief, a continuous infusion can be started (0.5-2 mg/kg/h) to maintain analgesia. The common side effects are usually mild or self-limited and dose-related and include perioral numbness, sedation, confusion, lightheadedness, and headache. Cardiac arrhythmia is a potential serious but low-risk adverse effect. Lidocaine can be combined with opioids as needed.
Ketamine, Oral or Injectable
For moderate or severe pain that is refractory to opioids, or when effective opioid doses cause intolerable adverse effects, ketamine can be added to enable reduction of opioid dose and improve analgesia.8,43-51 A typical starting dose is 2.5 mg orally or intravenously every 8 hours. If there is no benefit and also no adverse effect, the dose can be doubled on day 2 and again on day 3. The maximum dose is 0.5 mg/kg/dose. It can also be given as an intravenously infusion at 0.05-0.3 mg/kg/h. Contraindications include uncontrolled hypertension or high stroke risk. There is some evidence that ketamine can be used safely in patients with increased intracranial pressure and psychiatric illness.
Slow-Release Oral Morphine
For patients with moderate or severe cancer pain that is frequent or constant who can take oral medicines, slow-release oral morphine can reduce pill burden and provide more steady relief.
Fentanyl Transdermal Patches
This opioid preparation generally is better than morphine to treat moderate or severe cancer pain in noncachectic patients whose opioid requirement is stable and who are unable to take oral medicines or who have renal failure.
Fentanyl, Injectable
This is useful as a continuous infusion, with rescue bolus doses as needed, for moderate or severe pain that is frequent or constant in patients with renal failure or cachexia who are unable to take oral medicines. It is also useful for dose finding in noncachectic patients before applying fentanyl transdermal patch. Because of the rapid onset of action and short duration of action of injectable fentanyl, bolus doses alone are a good choice for preventing pain from brief procedures or dressing changes.
Injectable lidocaine, ketamine, and fentanyl are for use mainly in hospitals, but they can be provided in the home by palliative care specialist doctors if permitted by law and if clinically indicated.
Besides morphine and fentanyl, the other strong opioid on the WHO Model List of Essential Medicines for Pain and Palliative Care 2019 is methadone.7 Although methadone often can provide better relief for neuropathic pain than other opioids, we did not include it in the augmented package because opioid-refractory neuropathic pain can also be treated with other medicines in the essential and augmented packages, because of the relative complexity of its safe use, and so as not to risk complicating extremely important efforts in LMICs to use it to treat opioid use disorder.
NEUROLYTIC PROCEDURES FOR RELIEF OF SEVERE OR REFRACTORY PAIN
Pain impulses from the pelvic region are transmitted via somatic nerves from muscle, bone, skin, and connective tissue and via sympathetic and parasympathetic nerves and plexuses from visceral organs. Neurolytic procedures, and in some cases also neural stimulation, often can interrupt or modulate pain impulses transmitted within this neural network.52-54 However, because of the complexity of this pain network, adequate relief often requires multimodal treatment such as with both a neurolytic procedure and systemic pharmacotherapy.
Nerve Blocks
Neurolysis is the targeted destruction of a nerve or nerve plexus with chemical agents (alcohol or phenol), heat (radiofrequency ablation), or cold (cryoablation). If the appropriate and adequately trained staff member(s) and necessary equipment are available, these procedures should be considered when pharmacologic pain treatment results in inadequate pain control or intolerable side effects. Typically, neurolytic blocks should be performed with fluoroscopic, ultrasonographic, or computed tomography guidance. Although these procedures are not effective for every patient, they usually provide some degree of analgesia, from partial to complete, that lasts from days to several months and reduces the opioid requirement.55-57
Neurolysis of the superior hypogastric plexus is the most common block for pelvic cancer pain. The superior hypogastric plexus lies anterior to the L5/S1 disk and innervates the cervix, uterus, bladder, and rectum. Complications such as neural injury, bowel perforation, retroperitoneal bleeding, bowel and bladder dysfunction, infection, and diarrhea are rare.30,55-57
Ganglion impar block is a safe and relatively easy procedure to treat visceral pelvic, perineal, and anal pain. The ganglion impar lies in the presacral space near the sacrococcygeal ligament and provides innervation to the perineum, distal rectum, distal urethra, vagina, and vulva. Image-guided neurolysis of the ganglion impar appears to be a generally safe and effective procedure.58-60
Intrathecal drug delivery systems infuse analgesics directly into the spinal fluid at the appropriate spinal level via a subcutaneous catheter connected to an implanted, refillable drug pump. This method of analgesia can be very effective but is expensive, requires specialized equipment and well-trained staff members, and should not be initiated during an infection.61-63 Because of the risk of permanent neurologic injury, intrathecal saddle neurolysis of the sacral nerve roots should be considered only as a last resort for severe refractory pain in a patient near the end of life.64-66
Neurosurgical Procedures
Where a skilled spine surgeon and the necessary support staff and facilities are available, transmission of pain impulses from pelvis to brain can also be interrupted by surgical intervention in the spine or brain.67 Chemical rhizotomy (severing of spinal nerve roots) by injecting alcohol into the lumbar subarachnoid space can be combined with percutaneous cordotomy,68 but skill and expertise are necessary to minimize risk of injury to other nerves. Another surgical option is to open the lumbar dura and cut the dorsal roots to the pelvis.69 For pelvic pain mainly on one side, the spinothalamic tract on the contralateral side of the spinal cord can be interrupted by an open surgical or percutaneous cordotomy. Cordotomy usually is performed only unilaterally because bilateral cordotomy has a high risk of permanent motor weakness.70-72
A visceral afferent nociceptive pathway is located between the dorsal columns of the spinal cord and can be interrupted by surgical laminectomy and midline myelotomy.73,74 This requires opening the spinal dura, usually at the T10 level, direct incision into the dorsal midline of the spinal cord between the dorsal columns over 1-2 cm in length, and extending within the spinal cord to the level of the central canal—about 5 mm deep. An operating surgical microscope is required to guide the incision and minimize damage to the dorsal columns, which are essential for balance and ambulation.75-78 There is some risk of meningitis with this procedure, and it should be performed only by well-trained and experienced neurosurgeons.
The neural pathways that interpret pain in the brain can also be interrupted by performing a stereotactic cingulotomy.79 This procedure requires access to a stereotactic frame and imaging to target the appropriate region of the brain. Good pain relief at three months has been reported in 64% of patients. Spinal cord stimulation, used primarily for non-cancer pain, can also be used for cancer pain. However, stimulators require surgical implantation and are expensive, and the wire leads tend to break.53,80
Palliative Surgical Procedures
Women with locally advanced or recurrent invasive cervical cancer may benefit from surgical procedures to palliate physical symptoms and emotional distress related to compromise of the urinary tract, intestinal tract, or vasculature. However, when deciding whether to intervene surgically, the potential benefits of the surgery must be weighed carefully against the risks and potential discomforts of the procedure itself in the context of the patient's values and likely prognosis. Women who are medically fragile or are late in the course of their illness may be better served by non- or less-invasive interventions.
Ureteral obstruction often causes pain and acute kidney injury and can lead rapidly to destruction of function of one or both kidneys. If possible, this should be treated with placement of ureteral stents or, if necessary, percutaneous nephrostomy tubes. Fistulae of the distal urinary tract to the vagina or rectum may develop either because of direct tumor infiltration or as a complication of radiotherapy. Placement of flexible percutaneous nephrostomy tubes, ideally with simultaneous placement of coils in the ureters, can decrease or eliminate leakage of urine via a fistula from the vagina or rectum. However, provision must be made for urostomy bags.
The sigmoid colon or rectum can also become obstructed because of infiltration or compression by tumor, and fistulae can develop to the vagina or bladder. Colostomy can relieve large bowel obstruction and may decrease or eliminate fecal incontinence because of leakage via a fistula. It also may help prevent abscess formation or enable an existing abscess to heal after drainage and antibiotic treatment. In addition, some women may experience ulceration of the rectum as a complication of radiotherapy, and colostomy may bring relief from any resulting pain, fecal frequency, or incontinence. Access to training in colostomy care and to an adequate supply of colostomy bags should be assured if colostomy is offered.
Local progression of cervical cancer may lead to catastrophic hemorrhage from compromise of major vessels or from tumor neovasculature. If the goal of care is not solely comfort but (also) to sustain life to some extent, emergent selective pelvic vessel embolization should be considered if experienced operators and adequate equipment are available.14 If this is not an option, emergent palliative radiotherapy should be arranged, if possible. If neither embolization nor radiotherapy are available, tranexamic acid can be given, and the vagina can be tightly packed with simple roller gauge in a lithotomy position, with or without sedation or short general anesthesia depending on expected pain. A bladder catheter is needed while the pack is in place.81 If the only goal of care is comfort and the patient appears to be exsanguinating, pain, dyspnea, anxiety, or any other symptoms should be treated aggressively, even to the point of sedation if necessary to assure comfort.
Psycho-Oncology
Any doctor with basic palliative care training should be able to diagnose and treat uncomplicated anxiety or depressed mood with medicines in the EPPCCC, described elsewhere,3 and in LMICS, nurses, psychologists, social workers, and community health workers can be trained to provide simple, culturally appropriate supportive counseling and psychotherapy for uncomplicated depression.82-84 However, psychiatric or psycho-oncologic consultation is recommended for severe or refractory symptoms, for patients taking multiple psychoactive medicines, and for more complex psychiatric disorders such as bipolar disorder and psychotic disorders.85,86
Psycho-oncology, a subspecialty of psychiatry and psychology, addresses the psychological, social, behavioral, and cognitive problems related to cancer and cancer treatment. Psycho-oncologists collaborate with oncologists and palliative care providers to assess severe, complex, or refractory psychological and social suffering of patients with cancer and their family members and to plan and implement efforts to relieve this suffering.87,88 Specific competencies include diagnosis of psychological distress and comorbidities such as anxiety disorders, post-traumatic stress disorder, major depression, and sexual dysfunction; recognition of drug interactions and adverse psychological effects such as delirium; planning and implementing evidence-based psychopharmacologic and nonpharmacologic interventions; assistance with difficult discussions with patients or family members; and identification of optimum goals of care.85-87
Standard open-access measures used by psycho-oncologists to identify and diagnose psychosocial distress include the Distress Thermometer,89 the Patient Health Questionnaire Anxiety and Depression Scale,90 and the PROMIS emotional distress scales for cervical cancer.91 Treatment is tailored to the specific clinical situation. Evidence-based nonpharmacologic interventions for anxiety and depression include cognitive behavioral therapy, acceptance and commitment therapy, psychoeducation, and mindfulness and relaxation.87,92 Some patients benefit from existential interventions, such as dignity therapy, that promote meaning making, foster hope, and support expression of feelings at the end of life.93 Psycho-oncologists who are psychiatrists (medical doctors) can provide advice on the best pharmacologic interventions in a specific situation. Specialized psycho-oncologic consultation can be made accessible in LMICs via mobile phone or internet either as needed or as part of regular virtual tumor board conferences.
In conclusion, cervical cancer and its treatment sometimes result in suffering that is refractory to basic palliative care with the EPPCC. Therefore, we propose an augmented package of palliative care for cervical cancer that can prevent or alleviate even refractory suffering. Some elements require special training or experience, and some medicines or equipment are expensive and will not be widely available in low-income settings. However, we propose that each element should be implemented as soon as possible by at least one referral center in a region, province, or state, in a manner that makes relief of refractory suffering accessible by all.
ACKNOWLEDGMENT
We are grateful to the following for helpful comments on drafts of the paper: Sally Agallo Kwenda, Esther Cege-Munyoro, Liliana de Lima, Lailatul Ferdous, Rei Haruyama, Kim Hulscher, Elizabeth Mattfeld, Diana Nevzorova, MR Rajagopal, Julie Torode, and Linda Van Le.
Eric L. Krakauer
Employment: (I) My wife is employed by Inform Diagnostics and Foundation Medicine
Xiaoxiao Kwete
Employment: Yaozhi Co Ltd
Stock and Other Ownership Interests: Expat Inc
Research Funding: Roche
Patents, Royalties, Other Intellectual Property: My husband Patrick Kwete has a granted patent called “Personalized Medical Treatment Provision Software” (https://patents.google.com/patent/US20130080425A1/en)
Travel, Accommodations, Expenses: Expat Inc
Shekinah N. Elmore
Stock and Other Ownership Interests: Teladoc
Consulting or Advisory Role: Best Doctors Inc, Wildtype
Annette Hasenburg
Honoraria: AstraZeneca, Med Update, Pfizer, Roche, Streamedup!, Tesaro, MedConcept, LEO Pharma
Consulting or Advisory Role: PharmaMar, Tesaro, Roche, AstraZeneca, LEO Pharma, GlaxoSmithKline/MSD
Travel, Accommodations, Expenses: AstraZeneca, MedConcept, Roche, Streamedup!, Tesaro, MedUpdate, Pfizer
Mihir Kamdar
Leadership: Amorsa Therapeutics
Stock and Other Ownership Interests: Amorsa Therapeutics
Consulting or Advisory Role: Medtronic, Fern Health
Cristiana Sessa
Consulting or Advisory Role: Basilea
Ted Trimble
Consulting or Advisory Role: Merck, GlaxoSmithKline, Inovio Pharmaceuticals
Research Funding: Frantz Viral Therapeutics
No other potential conflicts of interest were reported.
DISCLAIMER
E.F., C.V. and E.L.K. are staff members or consultants of the WHO. The authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policy, or views of the WHO.
SUPPORT
Funding for this study was provided by WHO and Unitaid.
AUTHOR CONTRIBUTIONS
Conception and design: Eric L. Krakauer, Khadidjatou Kane, Xiaoxiao Kwete, Gauhar Afshan, Danta Dona Ruthnie Bien-Aimé, Lawrence F. Borges, Raimundo Correa, Cristiana Sessa, Cherian Varghese, Elena Fidarova
Collection and assembly of data: Eric L. Krakauer, Xiaoxiao Kwete, Nahla Gafer, Annekathryn Goodman, Kelly Irwin, Annette Hasenburg, Mihir Kamdar, Lawrence F. Borges, Shekinah N. Elmore, Quynh Xuan Nguyen Truong, Suresh Kumar, Maryam Rassouli, Elena Fidarova
Data analysis and interpretation: Eric L. Krakauer, Xiaoxiao Kwete, Lisa Bazzett-Matabele, Sarah Byrne-Martelli, Stephen Connor, C. R. Beena Devi, Mamadou Diop, Shekinah N. Elmore, Nahla Gafer, Annekathryn Goodman, Surbhi Grover, Annette Hasenburg, Kelly Irwin, Mihir Kamdar, Quynh Xuan Nguyen Truong, Tom Randall, Cristiana Sessa, Dingle Spence, Ted Trimble, Elena Fidarova
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Eric L. Krakauer
Employment: (I) My wife is employed by Inform Diagnostics and Foundation Medicine
Xiaoxiao Kwete
Employment: Yaozhi Co Ltd
Stock and Other Ownership Interests: Expat Inc
Research Funding: Roche
Patents, Royalties, Other Intellectual Property: My husband Patrick Kwete has a granted patent called “Personalized Medical Treatment Provision Software” (https://patents.google.com/patent/US20130080425A1/en)
Travel, Accommodations, Expenses: Expat Inc
Shekinah N. Elmore
Stock and Other Ownership Interests: Teladoc
Consulting or Advisory Role: Best Doctors Inc, Wildtype
Annette Hasenburg
Honoraria: AstraZeneca, Med Update, Pfizer, Roche, Streamedup!, Tesaro, MedConcept, LEO Pharma
Consulting or Advisory Role: PharmaMar, Tesaro, Roche, AstraZeneca, LEO Pharma, GlaxoSmithKline/MSD
Travel, Accommodations, Expenses: AstraZeneca, MedConcept, Roche, Streamedup!, Tesaro, MedUpdate, Pfizer
Mihir Kamdar
Leadership: Amorsa Therapeutics
Stock and Other Ownership Interests: Amorsa Therapeutics
Consulting or Advisory Role: Medtronic, Fern Health
Cristiana Sessa
Consulting or Advisory Role: Basilea
Ted Trimble
Consulting or Advisory Role: Merck, GlaxoSmithKline, Inovio Pharmaceuticals
Research Funding: Frantz Viral Therapeutics
No other potential conflicts of interest were reported.
REFERENCES
- 1.Arbyn M Weiderpass E Bruni L, et al. : Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob Health 8:e191-e203, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krakauer EL Kwete X Kane K, et al. : Cervical Cancer-Associated Suffering: Estimating the Palliative Care Needs of a Highly Vulnerable Population. JCO Glob Oncol 7:862-872, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krakauer EL Kane K Kwete X, et al. : An Essential Package of Palliative Care for Women with Cervical Cancer: Responding to the Suffering of a Highly Vulnerable Population. JCO Glob Oncol 7:873-885, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) : Integrating Palliative Care and Symptom Relief into Primary Health Care: A WHO Guide for Planners, Implementers and Managers. Geneva, World Health Organization, 2018. https://apps.who.int/iris/handle/10665/274559 [Google Scholar]
- 5.Knaul FM Farmer PE Krakauer EL, et al. : Alleviating the access abyss in palliative care and pain relief: An imperative of universal health coverage. Lancet 391:1391-1454, 2018 [DOI] [PubMed] [Google Scholar]
- 6.Krakauer EL Kwete X Verguet S, et al. : Palliative care and pain control, in: Jamison DT Gelband H Horton S, et al. (eds): Disease Control Priorities: Improving Health and Reducing Poverty, Volume 9 (ed 3). Washington, DC, World Bank, 2018, pp 235-246. https://openknowledge.worldbank.org/bitstream/handle/10986/28877/9781464805271.pdf?sequence=2&isAllowed=y [Google Scholar]
- 7.World Health Organization (WHO) : WHO Model List of Essential Medicines—21st List, 2019. Geneva, Switzerland, World Health Organization, 2019. https://www.who.int/publications/i/item/WHOMVPEMPIAU2019.06 [Google Scholar]
- 8.Palat G, Rajagopal MR: Pain management in cancer cervix. Indian J Palliat Care 11:64-73, 2005 [Google Scholar]
- 9.Pilkey J Demiers C Chochinov H, et al. : Does gynecologic malignancy predict likelihood of a tertiary palliative care unit hospital admission? A comparison of local, provincial and national death rates. Palliat Support Care 10:249-254, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Spoozak L Seow H Liu Y, et al. : Performance status and symptom scores of women with gynecologic cancer at the end of life. Int J Gynecol Cancer 23:971-978, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Lefkowits C Rabow MW Sherman AE, et al. : Predictors of high symptom burden in gynecologic oncology outpatients: Who should be referred to outpatient palliative care? Gynecolog Oncol 132:698-702, 2014 [DOI] [PubMed] [Google Scholar]
- 12.Rayment C Hjermstad MJ Aass N, et al. : Neuropathic cancer pain: Prevalence, severity, analgesics and impact from the European Palliative Care Research Collaborative–Computerised symptom assessment study. Palliat Med 27:714-721, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Fowler JM Carpenter KM Gupta P, et al. : The Gynecologic oncology consult: Symptom presentation and concurrent symptoms of depression and anxiety. Obstet Gynecol 103:1211-1217, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alméciga A Rodriguez J Beltrán J, et al. : Emergency embolization of pelvic vessels in patients with locally advanced cervical cancer and massive vaginal bleeding: A case series in a Latin American oncological center. JCO Glob Oncol 6:1376-1383, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allende-Perez S Dominguez-Ocadio G Velez-Salas V, et al. : Snapshot of symptoms of advanced cervical cancer patients referred to the palliative care service in a cancer center in Mexico. Int J Gynaecol Obstet 153:335-339, 2020 [DOI] [PubMed] [Google Scholar]
- 16.Bates MJ, Mijoya A: A review of patients with advanced cervical cancer presenting to palliative care services at Queen Elizabeth Central Hospital in Blantyre, Malawi. Malawi Med J 27:93-95, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miner TJ: Palliative surgery for advanced cancer: Lessons learned in patient selection and outcome assessment. Am J Clin Oncol 28:411-414, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Noor-Mahomed SB, Schlebusch L, Bosch BA: Suicidal behavior in patients diagnosed with cancer of the cervix. Crisis 24:168-172, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Maree JE, Holtslander L, Maree JE: The experiences of women living with cervical cancer in Africa: A metasynthesis of qualitative studies. Cancer Nurs, 2020. doi: 10.1097/NCC.0000000000000812 [epub ahead of print on March 24, 2020] [DOI] [PubMed] [Google Scholar]
- 20.Bray F Ferlay J Soerjomataram I, et al. : Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394-424, 2018 [DOI] [PubMed] [Google Scholar]
- 21.Torre LA Bray F Siegel RL, et al. : Global cancer statistics, 2012. CA Cancer J Clin 65:87-108, 2015 [DOI] [PubMed] [Google Scholar]
- 22.van Lonkhuijzen L, Thomas G: Palliative radiotherapy for cervical carcinoma, a systematic review. Radiother Oncol 98:287-291, 2011 [DOI] [PubMed] [Google Scholar]
- 23.Elmore SN Grover S Bourque JM, et al. : Global palliative radiotherapy: A framework to improve access in resource-constrained settings. Ann Palliat Med 8:274-284, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spanos W Guse C Perez C, et al. : Phase II study of multiple daily fractionations in the palliation of advanced pelvic malignancies: Preliminary report of RTOG 8502. Int J Radiat Oncol Biol Phys 17:659-661, 1989 [DOI] [PubMed] [Google Scholar]
- 25.Spanos WJ Perez CA Marcus S, et al. : Effect of rest interval on tumor and normal tissue response—A report of phase III study of accelerated split course palliative radiation for advanced pelvic malignancies (RTOG-8502). Int J Radiat Oncol Biol Phys 25:399-403, 1993 [DOI] [PubMed] [Google Scholar]
- 26.Kim DH Lee JH Ki YK, et al. : Short-course palliative radiotherapy for uterine cervical cancer. Radiat Oncol J 31:216-221, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caravatta L Padula GD Macchia G, et al. : Short-course accelerated radiotherapy in palliative treatment of advanced pelvic malignancies: a phase I study. Int J Radiat Oncol Biol Phys 83:e627-e631, 2012 [DOI] [PubMed] [Google Scholar]
- 28.Farina E Macchia G Siepe G, et al. : Palliative short-course radiotherapy in advanced pelvic cancer: A phase II study (SHARON project). Anticancer Res 39:4237-4242, 2019 [DOI] [PubMed] [Google Scholar]
- 29.Choan E Quon M Gallant V, et al. : Effective palliative radiotherapy for symptomatic recurrent or residual ovarian cancer. Gynecol Oncol 102:204-209, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Mishra S Bhatnagar S Rana SP, et al. : Efficacy of the anterior ultrasound-guided superior hypogastric plexus neurolysis in pelvic cancer pain in advanced gynecological cancer patients. Pain Med 14:837-842, 2013 [DOI] [PubMed] [Google Scholar]
- 31.Spanos WJ Wasserman T Meoz R, et al. : Palliation of advanced pelvic malignant disease with large fraction pelvic radiation and misonidazole: Final report of RTOG phase I/II study. Int J Radiat Oncol Biol Phys 13:1479-1482, 1987 [DOI] [PubMed] [Google Scholar]
- 32.Krishnan MS, Racsa M, Yu H-HM: Handbook of Supportive and Palliative Radiation Oncology. Cambridge, MA, Academic Press, 2016 [Google Scholar]
- 33.Mishra SK Laskar S Muckaden MA, et al. : Monthly palliative pelvic radiotherapy in advanced carcinoma of uterine cervix. J Cancer Res Ther 1:208-212, 2005 [DOI] [PubMed] [Google Scholar]
- 34.Dennis K Linden K Balboni T, et al. : Rapid access palliative radiation therapy programs: An efficient model of care. Future Oncol 11:2417-2426, 2015 [DOI] [PubMed] [Google Scholar]
- 35.Fairchild A Pituskin E Rose B, et al. : The rapid access palliative radiotherapy program: Blueprint for initiation of a one-stop multidisciplinary bone metastases clinic. Support Care Cancer 17:163-170, 2009 [DOI] [PubMed] [Google Scholar]
- 36.Atun R Jaffray D Barton M, et al. : Expanding global access to radiotherapy. Lancet Oncol 16:1153-1186, 2015 [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization (WHO) : Planning and Implementing Palliative Care Services: A Guide for Programme Managers. Geneva, Switzerland, World Health Organization, 2016. https://apps.who.int/iris/handle/10665/250584 [Google Scholar]
- 38.Olson RA Lengoc S Tyldesley S, et al. : Relationships between family physicians' referral for palliative radiotherapy, knowledge of indications for radiotherapy, and prior training: A survey of rural and urban family physicians. Radiat Oncol 7:73, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodin D Burger EA Atun R, et al. : Scale-up of radiotherapy for cervical cancer in the era of human papillomavirus vaccination in low-income and middle-income countries: A model-based analysis of need and economic impact. Lancet Oncol 20:915-923, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pallium India, International Association for Hospice and Palliative Care, and the Pain & Policy Studies Group : A morphine manifesto. J Pain Palliat Care Pharmacother 26:144-145, 2012 [DOI] [PubMed] [Google Scholar]
- 41.Sharma S Rajagopal MR Gayatri Palat G, et al. : A phase II pilot study to evaluate use of intravenous lidocaine for opioid-refractory pain in cancer patients. J Pain Symptom Manage 37:85-93, 2009 [DOI] [PubMed] [Google Scholar]
- 42.Thomas J Kronenberg R Cox MC, et al. : Intravenous lidocaine relieves severe pain: Results of an inpatient hospice chart review. J Palliat Med 7:660-667, 2004 [DOI] [PubMed] [Google Scholar]
- 43.Clark JL, Kalan GE: Effective treatment of severe cancer pain of the head using low-dose ketamine in an opioid-tolerant patient. J Pain Symptom Manage 10:310-314, 1995 [DOI] [PubMed] [Google Scholar]
- 44.Kotlińska-Lemieszek A, Jacek Luczak J: Subanesthetic ketamine: An essential adjuvant for intractable cancer pain. J Pain Symptom Manage 28:100-102, 2004 [DOI] [PubMed] [Google Scholar]
- 45.Jackson K, Ashby M, Goodchild C: Subanesthetic ketamine for cancer pain: By insisting on level I/II evidence, do we risk throwing the baby out with the bath water? J Pain Symptom Manage 29:328-330, 2005 [DOI] [PubMed] [Google Scholar]
- 46.Bell RF, Kalso E: Subanesthetic Ketamine for Cancer Pain and Scientific Rigor in Cancer Pain Trials. A Reply to Jackson et al. J Pain Symptom Manage 31:386, 2006 [DOI] [PubMed] [Google Scholar]
- 47.Prommer EE: Ketamine for pain: An update of uses in palliative care. J Palliat Med 15:474-483, 2012 [DOI] [PubMed] [Google Scholar]
- 48.Bredlau AL Thakur R Korones DN, et al. : Ketamine for pain in adults and children with cancer: A systematic review and synthesis of the literature. Pain Med 14:1505-1517, 2013 [DOI] [PubMed] [Google Scholar]
- 49.Watanabe Nemoto M Natsuko Nozaki-Taguchi N Togasaki G, et al. : New approach to relieving pain and distress during high-dose-rate intracavitary irradiation for cervical cancer. Brachytherapy 14:642-647, 2015 [DOI] [PubMed] [Google Scholar]
- 50.Cheung KWA, Chan PC, Lo SH: The use of ketamine in the management of refractory cancer pain in a palliative care unit. Ann Palliat Med 9:4478-4489, 2019 [DOI] [PubMed] [Google Scholar]
- 51.Tofte Gregers MC Mikkelsen S Prier Lindvig K, et al. : Ketamine as an anesthetic for patients with acute brain injury: A systematic review. Neurocrit Care 33:273-282, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rigor BM: Pelvic cancer pain. J Surg Oncol 75:280-300, 2000 [DOI] [PubMed] [Google Scholar]
- 53.Hunter CW Stovall B Chen G, et al. : Anatomy, pathophysiology and interventional therapies for chronic pelvic pain: A review. Pain Physician 21:147-167, 2018 [PubMed] [Google Scholar]
- 54.Eid S Iwanga J Chapman J, et al. : Superior hypo gastric plexus and its surgical implications during spine surgery: A review. World Neurosurg 120:163-167, 2018 [DOI] [PubMed] [Google Scholar]
- 55.de Leon-Casasola OA, Kent E, Lema MJ: Neurolytic superior hypogastric plexus block for chronic pelvic pain associated with cancer. Pain 54:145-151, 1993 [DOI] [PubMed] [Google Scholar]
- 56.Plancarte R de Leon-Casasola OA El-Helaly M, et al. : Neurolytic superior hypogastric plexus block for chronic pelvic pain associated with cancer. Reg Anesth 22:562-568, 1997 [PubMed] [Google Scholar]
- 57.Rocha A Plancarte R Nataren RGR, et al. : Effectiveness of superior hypogastric plexus neurolysis for pelvic cancer pain. Pain Physician 23:203-208, 2020 [PubMed] [Google Scholar]
- 58.Plancarte R Amescua C Patt RB, et al. : Presacral blockade of the ganglion of Walther (ganglion impar). Anesthesiology 73:A751, 1990 [DOI] [PubMed] [Google Scholar]
- 59.Ahmed DG, Mohamed MF, Mohamed SA: Superior hypogastric plexus combined with ganglion impar neurolytic blocks for pelvic and/or perineal cancer pain relief. Pain Physician 18:E49-E56, 2015 [PubMed] [Google Scholar]
- 60.Sousa Correia J Silva M Castro C, et al. : The efficacy of the ganglion impar block in perineal and pelvic cancer pain. Support Care Cancer 27:4327-4330, 2019 [DOI] [PubMed] [Google Scholar]
- 61.Smith TJ Staats PS Deer T, et al. : Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: Impact on pain, drug-related toxicity, and survival. J Clin Oncol 20:4040-4049, 2002 [DOI] [PubMed] [Google Scholar]
- 62.Deer TR Smith HS Burton AW, et al. : Comprehensive consensus based guidelines on intrathecal drug delivery systems in the treatment of pain caused by cancer pain. Pain Physician 14:E283-E312, 2011 [PubMed] [Google Scholar]
- 63.Deer TR Pope JE Hayek SM, et al. : The Polyanalgesic Consensus Conference (PACC): Recommendations on intrathecal drug infusion systems best practices and guidelines. Neuromodulation 20:96-132, 2017[Erratum: Neuromodulation 20:405-406, 2017] [DOI] [PubMed] [Google Scholar]
- 64.Rodriguez-Bigas M Petrelli NJ Herrera L, et al. : Intrathecal phenol rhizotomy for management of pain in recurrent unresectable carcinoma of the rectum. Surg Gynecol Obstet 173:41-44, 1991 [PubMed] [Google Scholar]
- 65.Slatkin NE, Rhiner M: Phenol saddle blocks for intractable pain at end of life: Report of four cases and literature review. Am J Hosp Palliat Care 20:62-66, 2003 [DOI] [PubMed] [Google Scholar]
- 66.Igarashi H, Sato S, Shiraishi Y: Saddle block using 10-20% tetracaine for patients with perineal pain due to recurrent rectal cancer. Anesthesiology 98:781-783, 2003 [DOI] [PubMed] [Google Scholar]
- 67.Raslan AM Ben-Haim S Falowski SM, et al. : Congress of Neurological Surgeons systematic review and evidence-based guideline on neuroablative procedures for patients with cancer pain. Neurosurgery 88:437-442, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ischia S Luzzani A Ischia A, et al. : Subarachnoid neurolytic block (L5-S1) and unilateral percutaneous cervical cordotomy in the treatment of pain secondary to pelvic malignant disease. Pain 20:139-149, 1984 [DOI] [PubMed] [Google Scholar]
- 69.Son BC Yoon JH Kim DR, et al. : Dorsal rhizotomy for pain from neoplastic lumbosacral plexopathy and advanced pelvic cancer. Stereotactic Funct Neurosurg 92:109-116, 2014 [DOI] [PubMed] [Google Scholar]
- 70.Raslan A Cetas JS McCartney S, et al. : Destructive procedures for control of cancer pain: The case for cordotomy, a review. J Neurosurg 114:155-170, 2011 [DOI] [PubMed] [Google Scholar]
- 71.Shepherd TM Hoch MJ Cohen BA, et al. : Palliative CT-guided cordotomy for medically intractable pain in patients with cancer. AJNR Am J Neuroradiol 38:387-390, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hogberg T Rabow L Rosenberg P, et al. : The use of chordotomy to treat pain from gynecologic cancer. Eur J Gynecol Oncol 10:337-340, 1989 [PubMed] [Google Scholar]
- 73.Hirshberg RM Al-Chaer ED Lawand NB, et al. : Is there a pathway in the posterior funiculus that signals visceral pain? Pain 67:291-305, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Willis WD Al-Chaer ED Quast MJ, et al. : A visceral pain pathway in the dorsal column of the spinal cord. Proc Natl Acad Sci USA 96:7675-7679, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hong D, Andren-Sandberg A: Punctate midline myelotomy: A minimally invasive procedure for the treatment of pain in inextirable abdominal and pelvic cancer. J Pain Symptom Manag 33:99-109, 2007 [DOI] [PubMed] [Google Scholar]
- 76.Becker R, Sure U, Bertalanffy H: Punctate midline myelotomy-a new approach in the management of visceral pain. Acta Neurochirurgica (Wien) 141:881-883, 1999 [DOI] [PubMed] [Google Scholar]
- 77.Filho OV Araujo MR Florencio RS, et al. : CT-guided percutaneous punctate midline myelotomy for the treatment of intractable visceral pain: A technical note. Stereotactic Funct Neurosurg 77:177-182, 2001 [DOI] [PubMed] [Google Scholar]
- 78.Viswanathan A Burton AW Rekito A, et al. : Commissural myelotomy in the treatment of intractable visceral pain: Technique and outcomes. Stereotactic Funct Neurosurg 88:374-382, 2010 [DOI] [PubMed] [Google Scholar]
- 79.Berger A Hochberg U Zegerman A, et al. : Neurosurgical ablative procedures for intractable cancer pain. J Neurosurg 133:144-151, 2020 [DOI] [PubMed] [Google Scholar]
- 80.Flagg A, McGreevy K, Williams K: Spinal cord stimulation in the treatment of cancer-related pain: “Back to the origins”. Curr Pain Headache Rep 16:343-349, 2012 [DOI] [PubMed] [Google Scholar]
- 81.Mishra K: Gynaecological malignancies from palliative care perspective. Indian J Palliat Care 17:S45-S51, 2011. (suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Belkin GS Unützer J Kessler RC, et al. : Scaling up for the “bottom billion”; “5×5” implementation of community mental health care in low-income regions. Psychiatr Serv 62:1494-1502, 2011 [DOI] [PubMed] [Google Scholar]
- 83.Patel V: Where There Is No Psychiatrist: A Mental Health Care Manual. London, United Kingdom, Gaskell, 2003 [Google Scholar]
- 84.Weobong B Weiss HA McDaid D, et al. : Sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial. PLoS Med 14:e1002385, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huffman LB Hartenbach EM Carter J, et al. : Maintaining sexual health throughout gynecologic cancer survivorship: A comprehensive review and clinical guide. Gynecol Oncol 140:359-368, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Riba MB Donovan KA Andersen B, et al. : Distress management, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 17:1229-1249, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Andersen BL DeRubeis RJ Berman BS, et al. : Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology guideline adaptation. J Clin Oncol 32:1605-1619, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Weis J, Hasenburg A: Psychological support, in: Ayhan ARN, Gultekin M, Dursun P. (eds): Textbook of Gynaecological Oncology (ed 3). Ankara, Turkey: Gunes Publishing, 2016, pp 1495-1499 [Google Scholar]
- 89.Donovan KA Grassi L McGinty HL, et al. : Validation of the distress thermometer worldwide: State of the science. Psychooncology 23:241-250, 2014 [DOI] [PubMed] [Google Scholar]
- 90.Kroenke K Wu J Yu Z, et al. : The Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS): Initial validation in three clinical trials. Psychosom Med 78:716-727, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wilford J Osann K Hsieh S, et al. : Validation of PROMIS emotional distress short form scales for cervical cancer. Gynecol Oncol 151:111-116, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li M Kennedy EB Byrne N, et al. : Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psychooncology 26:573-587, 2017 [DOI] [PubMed] [Google Scholar]
- 93.Bauereiß N Obermaier S Özünal SE, et al. : Effects of existential interventions on spiritual, psychological, and physical well-being in adult patients with cancer: Systematic review and meta-analysis of randomized controlled trials. Psychooncology 27:2531-2545, 2018 [DOI] [PubMed] [Google Scholar]