Abstract
The COVID-19 pandemic has had an unprecedented impact on people and healthcare services. The disruption to chronic illnesses, such as epilepsy, may relate to several factors ranging from direct infection to secondary effects from healthcare reorganization and social distancing measures.
Objectives
As part of the COVID-19 and Epilepsy (COV-E) global study, we ascertained the effects of COVID-19 on people with epilepsy in Brazil, based on their perspectives and those of their caregivers. We also evaluated the impact of COVID-19 on the care delivered to people with epilepsy by healthcare workers.
Methods
We designed separate online surveys for people with epilepsy and their caregivers. A further survey for healthcare workers contained additional assessments of changes to working patterns, productivity, and concerns for those with epilepsy under their care. The Brazilian arm of COV-E initially collected data from May to November 2020 during the country's first wave. We also examined national data to identify the Brazilian states with the highest COVID-19 incidence and related mortality. Lastly, we applied this geographic grouping to our data to explore whether local disease burden played a direct role in difficulties faced by people with epilepsy.
Results
Two hundred and forty-one people returned the survey, 20% were individuals with epilepsy (n = 48); 22% were caregivers (n = 53), and 58% were healthcare workers (n = 140). Just under half (43%) of people with epilepsy reported health changes during the pandemic, including worsening seizure control, with specific issues related to stress and impaired mental health. Of respondents prescribed antiseizure medication, 11% reported difficulty taking medication on time due to problems acquiring prescriptions and delayed or canceled medical appointments. Only a small proportion of respondents reported discussing significant epilepsy-related risks in the previous 12 months. Analysis of national COVID-19 data showed a higher disease burden in the states of Sao Paulo and Rio de Janeiro compared to Brazil as a whole. There were, however, no geographic differences observed in survey responses despite variability in the incidence of COVID-19.
Conclusion
Our findings suggest that Brazilians with epilepsy have been adversely affected by COVID-19 by factors beyond infection or mortality. Mental health issues and the importance of optimal communication are critical during these difficult times. Healthcare services need to find nuanced approaches and learn from shared international experiences to provide optimal care for people with epilepsy as the direct burden of COVID-19 improves in some countries. In contrast, others face resurgent waves of the pandemic.
Keywords: Coronavirus, Epilepsy risk, Non-communicable disease, Seizures, SUDEP
1. Introduction
The COVID-19 pandemic has led to a dramatic loss of life and a massive increase in health burden worldwide [1]. While the direct effects of COVID-19 are well documented, the clinical community is still trying to understand the pandemic's indirect impact on specific groups with differential vulnerabilities, particularly in low- and middle-resourced countries [2], [3], [4].
Brazil has been significantly affected by the COVID-19 pandemic [5], [6]. The first wave, in Brazil, lasted until November 2020 and involved more than 6 million cases with about 172,000 attributable deaths (https://covid.saude.gov.br/) [7]. In response, health service provision underwent a significant reorganization to address COVID-19 pressures. The impact on services for people with non-communicable diseases, especially those with associated risk, has been considerable [8], [9], [10].
It is estimated that at least three million people have epilepsy in Brazil [11]. People with epilepsy are, overall, not considered to be at greater risk of COVID-19 infection or of developing a more severe form of the disease [12], [13], [14], [15], [16], [17], [18]. Other factors, including difficulty obtaining antiseizure medications (ASMs) and problems in accessing the health system, may play a role in worsening seizure control and exacerbating comorbidities in this group [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30].
Many epilepsy services were suspended early in the pandemic, including routine electroencephalography (EEG), face-to-face outpatient clinics, and EEG-video-telemetry monitoring. Epilepsy surgery and vagus nerve stimulator (VNS) implantation/adjustments were postponed or canceled [16], [31], [32]. Many neurologists were re-deployed to 'front lines' or Intensive Care Units to manage people with COVID-19, while others moved to remote working as they were in a high-risk group [8], [32], [33], [34]. People with epilepsy and their caregivers stopped attending clinics due to restrictions, and remote consultations were increasingly used [35], [36], [37]. While necessary, such actions may have unintended consequences, including, for example, difficulties in obtaining ASM prescriptions during a lockdown or restrictive social isolation measures.
To understand problems that people with epilepsy faced during the pandemic, the COVID-19 and Epilepsy (COV-E) Study launched online surveys for people with epilepsy, caregivers, and healthcare workers (HCWs). The aim was to assess the impact of the pandemic on health and wellbeing, exploring themes such as health status, interactions with health services, and risk communication. We also asked HCWs about changes in their working patterns, productivity, and concerns for those under their care. Survey responses were compared with national data on virus incidence and mortality along geographic dimensions that measure COVID-19 disease burden. While the complete study has achieved a global reach, here we present the Brazilian data.
2. Methods
2.1. Study design
The study design has been described previously [29]. In brief, we used separate surveys for people with epilepsy, primary caregivers, and HCWs involved in epilepsy care (https://sudep.org/epilepsy-risks-and-covid-19-survey-people-epilepsy?fbclid=IwAR0M5ATaHN9iU1CDlZmkcEntyZH1saE4Y_t1uTuvxxYBF4JF2z9mRmcjJdk) [38]. The surveys were piloted in the United Kingdom (UK). Originally the surveys were in English but have since been translated into eight languages, including Portuguese, for people with epilepsy and caregivers. The HCW survey in Brazil was in English, as there is a broad familiarity with English among health professionals. Surveys are hosted on the Jisc web platform (https://www.onlinesurveys.ac.uk/) [39].
The surveys' focus was on collecting quantitative data, but the option to submit qualitative responses was available through free-text answers. Data entry was anonymous and quantitative responses were analyzed in aggregate. The University of Oxford Ethics Committee approved the study (Ref.: R69353/RE001).
2.2. Measurements
2.2.1. Demographics
People with epilepsy provided background information, including age, sex, ethnic background, and postcode information. Caregivers provided the same information about those for whom they care.
Healthcare workers provided similar demographic information, their primary role, and their specialties.
2.2.2. Epilepsy type/health background
We asked people with epilepsy and caregivers about epilepsy characteristics, including type and frequency of seizures and access to healthcare (planned appointments and emergency settings) in the previous 12 months.
We asked about the possibility of COVID-19 infection and the need to self-isolate due to contact exposure. We asked HCWs about their COVID-19 concerns affecting work, seeing people, and their experience in utilizing online platforms.
2.2.3. Risk factors for epilepsy morbidity and mortality
We probed about changes to seizures, sleep, alcohol and drug consumption, and mental health status. Surveys did not use validated questionnaires, but were instead aimed at obtaining a breadth of representative information.
We explored discussion of risks for epilepsy morbidity and mortality between the participant and their clinician in the previous 12 months, including ASM side effects, rescue medication, alcohol, driving, life changes, employment, mental health, sleep, contraception, pregnancy (when applicable), recreational drugs, safety aids, first aid, stigma, and discussion about Sudden Unexpected Death in Epilepsy (SUDEP).
We asked HCWs about their confidence in diagnosing epilepsy remotely, whether the reduced availability of investigations affected their ability to diagnose and treat seizures and if their approach to ASMs management had changed. We enquired about their views on how the pandemic affected seizure frequency and mental health. HCWs were also asked whether they had discussions about risk, COVID-19 prevention, and whether they were proactively contacting vulnerable groups.
2.2.4. Access to healthcare
We asked people with epilepsy about the impact of the pandemic on healthcare access and if they had been satisfied with these changes or not.
2.2.5. Caregiver survey
The caregiver survey mirrored that for people with epilepsy to ascertain the impact of the COVID-19 pandemic on the individual through a caregiver's perspective.
2.3. Dissemination
SUDEP Action led survey dissemination, and the surveys were shared via social media platforms, individually, and through collaboration with Brazilian Organizations of Epilepsy.
2.4. National data on COVID-19 disease burden
National data on COVID-19 incidence and mortality were obtained from the open-source repository https://cmmid.github.io/visualisations/lacpt using data from Brazil. IO (see links for more information) [40]. This data source with a high temporal and geographic resolution provides updated cumulative numbers of COVID-19 cases and mortality every second day from March 2020 onward for each of the 27 Brazilian states. We used these data for analysis and comparison with the epilepsy survey data.
2.5. Data analysis and statistical testing
We collected data in Brazil from May to November 2020, during the first wave of COVID-19. We categorized the returns and compared qualitative and quantitative data relating to i) demographic; ii) reported health outcomes; iii) awareness of risk; and iv) access to epilepsy care. Data analyses used descriptive statistics and qualitative coding of free-text data. Qualitative analysis on free-text answers was performed by identifying common themes and using terms, such as “anxiety” and “stress”, across different participants.
Each survey was first analyzed individually, utilizing descriptive statistics and cross-tabulation of data using tools provided by Jisc [39]. Data were then exported into Microsoft Excel, and cross-comparisons of individual persons with epilepsy, caregiver, and HCW surveys were made.
We performed comparisons between the national COVID-19 disease burden and epilepsy survey data on Matlab R2019b. We modeled state case incidence and mortality as Gaussian distributions followed by a z-statistic transformation to compare with state averages. A value greater than two standard deviations away from the mean was considered statistically significant based on a two-tailed p-z pairing. Differences in the survey responses between the states of Sao Paulo and Rio de Janeiro were compared to those from the rest of Brazil using Chi-Square (χ2)-testing.
3. Results
We received 241 completed surveys, 20% from those with epilepsy (n = 48), 22% from caregivers (n = 53), and 58% from HCWs (n = 140) (Table 1 ). Caregivers completed the surveys based on their impression of the pandemic’s impact upon the person with epilepsy for whom they cared. Data from surveys completed in Portuguese were converted and amalgamated with data provided in English.
Table 1.
Demographics of the cohort including sex, age, and ethnicity of Brazilian participants. The under-18 years’ responses correspond to caregivers completing the caregiver survey for children with epilepsy.
| People with epilepsy | Caregivers | Healthcare workers | |
| N | 48 | 53 | 140 |
| Sex | |||
| Female (% within group) | 28 (58%) | 30 (57%) | 86 (61%) |
| Age group in years (%) | |||
| <18 | 12 (23%) | ||
| 18–29 | 10 (21%) | 10 (19%) | 27 (19%) |
| 30–39 | 16 (33%) | 8 (15%) | 50 (36%) |
| 40–49 | 7 (15%) | 9 (17%) | 34 (24%) |
| 50–59 | 10 (21%) | 8 (15%) | 21 (15%) |
| >60 | 5 (10%) | 6 (11%) | 8 (6%) |
| Minority ethnic group (%) | |||
| Yes | 4 (8%) | 7 (13%) | |
| 34 (71%) | 28 (53%) | ||
| Not sure | 8 (17%) | 10 (19%) | |
| Prefer not to say | 2 (4%) | 8 (15%) | |
3.1. Population demographics
3.1.1. Geographical distribution
We received responses from 17 states, covering all regions of Brazil (Fig. 1 ). Of all responses, 82% came from Rio de Janeiro and Sao Paulo, the most populous states (comprising about a third of the Brazilian population).
Fig. 1.
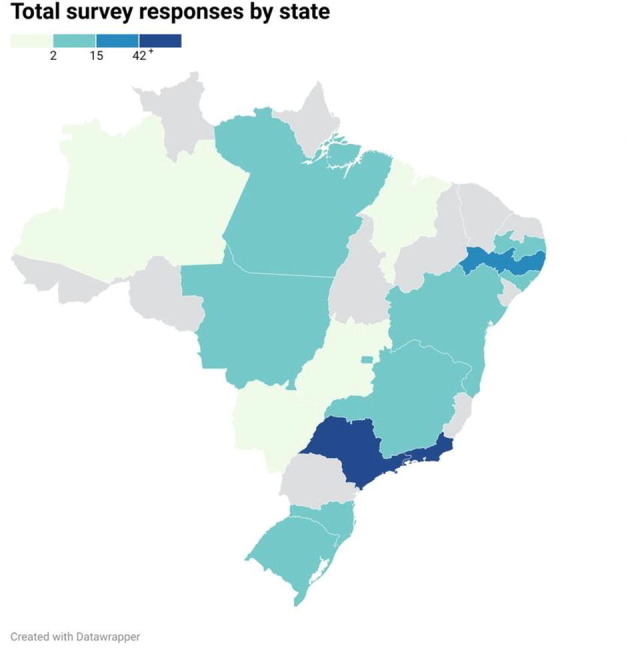
Geographic distribution of survey responses by state in Brazil. The states of Rio de Janeiro and Sao Paulo, both in the southeastern region, represented the majority of the survey responses (65% and 17%, respectively), followed by the state of Pernambuco (6%), located in the northeastern region of the country. Color bar denotes absolute response numbers with dark blue indicating more than 42 responses in that state.
3.1.2. Sex and age
There were more responses from females and those below 60 years of age (see Table 1 for details).
3.1.3. Relationship between the caregiver and the person with epilepsy
Of the 53 caregiver respondents, 49% (n = 26) were one of the parents of the person with epilepsy; 19% (n = 10) a close relative, and 17% (n = 9) a partner or spouse. One carer was a guardian and 13% (n = 7) reported an unspecified caregiver relationship to the person with epilepsy.
3.2. Exposure to risk during the COVID-19 pandemic
3.2.1. Health and wellbeing
Thirty-one percent of respondents from the people with epilepsy and caregiver surveys (31/101) reported changes in their health/the health for the person for whom they care. Qualitative data analysis of free-text responses indicated that worse seizure control was a significant issue with “stress”, “anguish”, and “fear” related to the pandemic restrictions and contracting the virus, acting as contributing factors.
3.2.2. Access to healthcare
3.2.2.1. Prescriptions
Overall, 44/97 (45%) reported problems in obtaining prescriptions during the pandemic. When combining individuals and caregiver responses, of those who take ASMs (97/101), 11% reported difficulties taking medications on time (11/97). Difficulty in obtaining prescriptions and altered or canceled medical appointments were described as contributing factors.
3.2.2.2. First aid
Nine percent of individuals lived alone during lockdown or restrictive measures of social isolation (9/101). Of the 92 who reported living with someone, only three did not live with someone who could provide first aid in case of a seizure.
3.2.2.3. Emergency care
Thirty-three percent of individuals and caregiver surveys reported injuries or a need for emergency care due to epilepsy during the previous 12 months (33/101), including a report of hospitalization due to serial seizures. Twenty-four percent of this group reported head trauma (8/33) and 15% facial trauma (5/33). Trauma to the limbs was reported by 27% (9/33), including fractures, skin lacerations, and burns. One person reported spinal trauma.
3.2.2.4. Epilepsy services
Sixty-one percent of respondents reported changes in scheduled medical appointments (62/101), mainly delayed face-to-face consultation. One person reported difficulty making a new appointment, and one did not receive a VNS adjustment at the scheduled time. Forty-four percent (27/ 62) reported not being satisfied with these changes. Thirty-two percent (32/101) found difficulties in receiving help from healthcare providers (HCPs). Qualitative analysis showed that the most frequent concerns were difficulties with canceled or rescheduled medical appointments and fear of COVID-19 infection when attending hospitals or health units.
3.2.3. Risk awareness
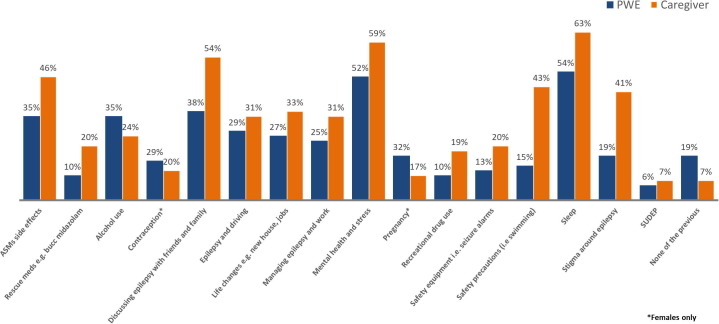
We asked individuals and caregivers about interactions with HCWs and how well epilepsy risk factors were discussed in the previous 12 months. Sixty-one percent of respondents recall discussions on sleep and epilepsy (62/101); 56% had discussed mental health and stress (57/101); and 46% had spoken about the impact of epilepsy on friends and family (46/101). SUDEP was the least considered topic, with only 8% recalling this being discussed (8/101) (Fig. 2 ).
Fig. 2.
Summary of epilepsy-related factors discussed between the healthcare team, patient with epilepsy and caregiver over the last 12 months. Aspects of epilepsy associated risk and epilepsy management, including SUDEP, were not often discussed including in periods prior to the pandemic. Total number of respondents =101. Abbreviations: ASMs- antiseizure medications; PWE- people with epilepsy; SUDEP- Sudden and Unexpected Death in Epilepsy.
3.3. Analysis of special groups
3.3.1. Ethnic minorities
All 11 respondents who considered themselves a minority ethnic group regularly saw epilepsy health professionals. Visit frequency was between two to six or more yearly. All reported living with someone who could assist in case of seizures. Seventy-three % (8/11) reported generalized seizures, and 64% (7/11) seizures during sleep. Two suffered epilepsy-related injuries in the previous 12 months. Thirty-six percent (4/11) reported difficulty getting help from health services. Of this group, only one recalled discussing SUDEP in the previous 12 months.
3.3.2. People with epilepsy aged over 60 years
Eleven responders with epilepsy were over the age of 60 years. The most prevalent comorbidities in this group were hypertension, heart disease, lung disease, intellectual, and memory difficulties. There was one report of nonepileptic seizures. One respondent stated that COVID-19 measures triggered changes in health due to anxiety. None reported problems taking medication on time. All were living with someone aware of their epilepsy and provided first aid. All respondents found it challenging to get help for epilepsy needs during the pandemic, mainly due to modified or canceled appointments and the difficulty of acquiring ASM prescriptions.
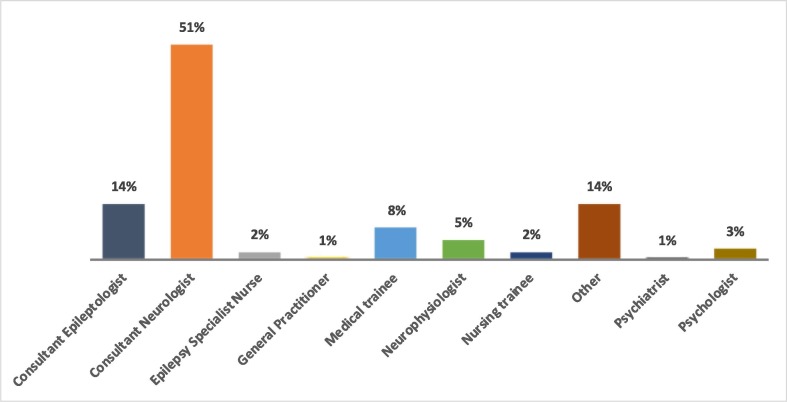
3.4. Healthcare worker survey
Most HCWs were general neurologists (51%, n = 72), followed by neurologists with a special interest in epilepsy (14%, n = 19). Only a small number of non-prescribing HCWs, such as psychologists and nurses, completed the survey (Fig. 3 ). Fifty-seven percent of HCWs (n = 80) saw adults with epilepsy; 28% (n = 39) were involved in the care of both adults and children; 14% (n = 19) only saw children with epilepsy. Two HCWs responded ‘other’ when describing their role, further specifying their answers as ‘adult and elderly’ and ‘adult and teenager’. Fourteen percent (n = 20) had been infected and 18% (n = 25) had possibly been infected by COVID-19. Twenty-one percent (n = 30) had to self-isolate. Overall, 86% (120/140) of HCWs were less confident in diagnosing epilepsy remotely than when seeing people face-to-face. Most HCW responses came from Rio de Janeiro (65%, n = 91), followed by Sao Paulo state (12%, n = 17).
Fig. 3.
Role of healthcare worker respondents. The majority of HCW respondents were consultant neurologists with other respondents comprised of other specialists and non-prescribing participants. (Total number of respondents = 140).
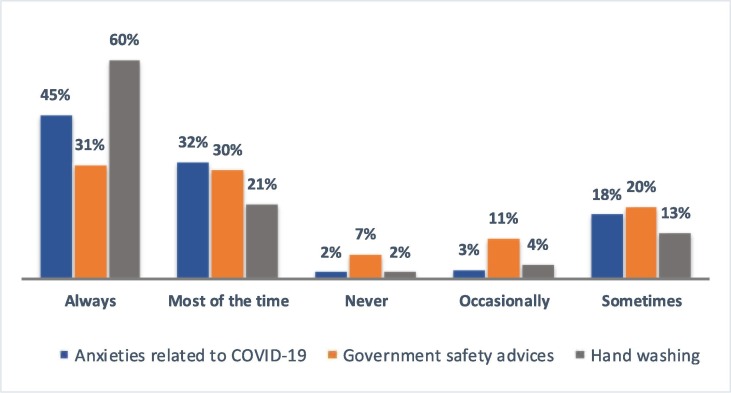
The approach to prescribing ASMs had not changed for 71% (n = 99), while around half had a similar approach to withdrawing ASMs during the pandemic as before (53%, n = 74). Fifty-six percent (79/140) reported that they did not notice changes in people's seizure frequency. Around a third (48/140), however, perceived increased seizures, attributing this to alterations in mental health, difficulty obtaining prescriptions, and reduced access to pre-scheduled consultations. Healthcare workers stated that they also discussed specific COVID-related subjects (e.g., anxieties during the pandemic (45%); governmental advice on prevention (31%); handwashing (60%)) with people with epilepsy and their caregivers (Fig. 4 ).
Fig. 4.
Summary of discussions relating to COVID between healthcare workers (HCWs) and people with epilepsy. HCWs variably discussed aspects related to the pandemic such as anxieties related to COVID-19, government safety advice, and hand washing. Handwashing was, for example, discussed at least most of the time by 81% of HCWs and anxiety related to COVID-19 in 77% of interactions. (Total number of respondents = 140).
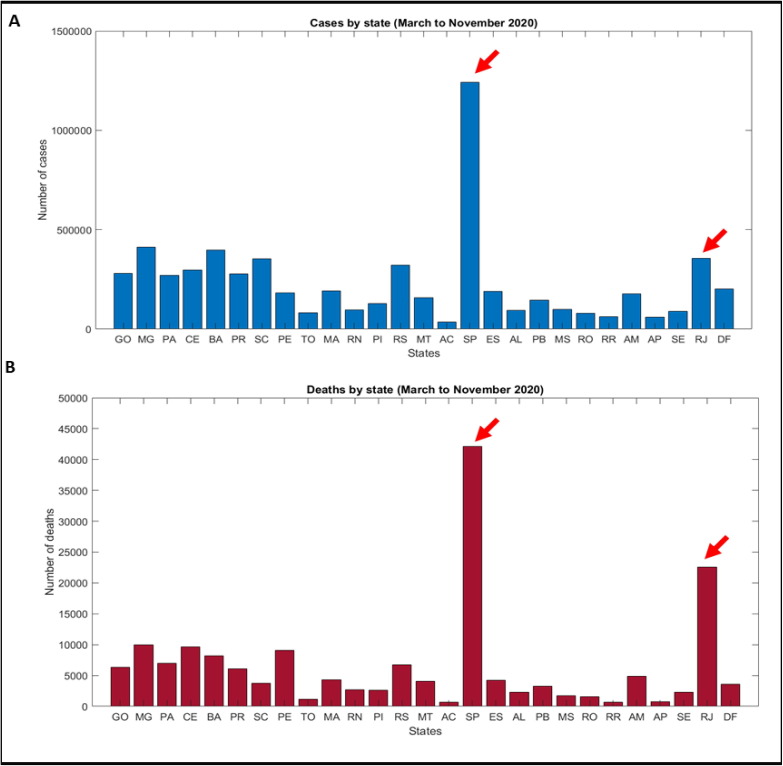
3.5. National COVID-19 disease burden by state
National COVID-19 data on disease burden show a disproportionate distribution of case incidence and mortality among the 27 states. These absolute numbers do not consider relative population density or proportional healthcare resources, but represent a pragmatic, geographic division of disease burden. During the period of survey collection, the state of Sao Paulo had the highest COVID-19 incidence with 1,241,000 cases which was significantly greater (z = 4.20, ***p < 0.001) than the average number of 232,643 cases per state during the time of the study (Fig. 5 A). The states of Sao Paulo and Rio de Janeiro had the highest numbers of COVID-19 deaths (42,110 deaths, z = 4.17, ***p < 0.001 and 22,590 deaths, z = 2.021, *p < 0.05) and were significantly higher than the 6,397 average deaths per state (Fig. 5B).
Fig. 5.
COVID-related incidence and mortality separated by states in Brazil. National data from Brazil showing absolute reported numbers of COVID cases (A) and deaths (B) across 27 states in Brazil during the same time period as the epilepsy survey data collection. Sao Paulo and Rio de Janeiro states are indicated by arrows. The average number of cases per state was 232,643 with Sao Paulo having the highest number with 1,241,000 cases (significantly higher than the state average following z-score transformation, z = 4.20, ***p < 0.001). The average number of deaths per state was 6,397 with Sao Paulo and Rio de Janeiro having the highest two death totals and significantly higher than the state average (42,110 deaths for Sao Paulo, z = 4.17, ***p < 0.001 and 22,590 deaths for Rio de Janeiro, z = 2.021, *p < 0.05). All data were obtained from the open-source repository https://cmmid.github.io/visualisations/lacpt using data from Brasil.IO (municipality level). Abbreviations: GO – Goias, MG - Minas Gerais, PA – Para, CE – Ceara, BA – Bahia, PR – Parana, SC - Santa Catarina, PE – Pernambuco, TO – Tocantins, MA - Maranhao, RN - Rio Grande do Norte, PI - Piaui, RS -Rio Grande do Sul, MT - Mato Grosso, AC – Acre, SP - Sao Paulo, ES - Espirito Santo, AL – Alagoas, PB – Paraiba, MS - Mato Grosso do Sul, RO – Rondonia, RR – Roraima, AM – Amazonas, AP – Amapa, SE – Sergipe, RJ - Rio de Janeiro, DF - Distrito Federal.
3.5.1. Epilepsy survey responses between the states of Sao Paulo and Rio de Janeiro compared to the rest of Brazil
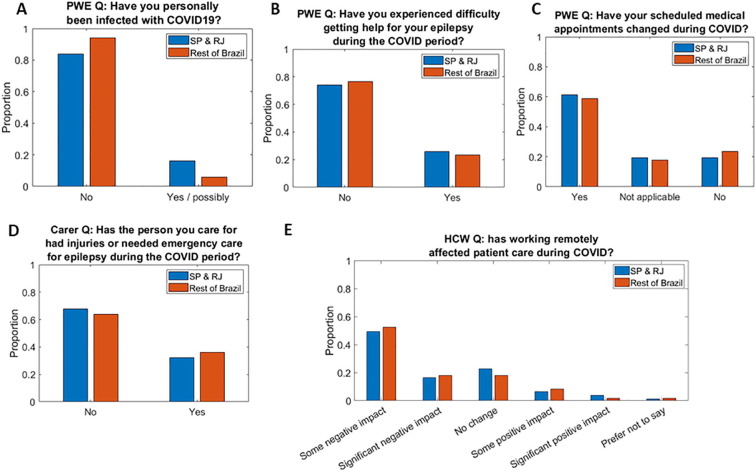
Combining survey data from the states of Sao Paulo and Rio de Janeiro and comparing these to survey responses from the rest of Brazil (where COVID-19 impact was significantly lower), there were no notable differences in responses related to the impact of COVID-19 based on this geographic division. χ2-testing showed no significant difference between individual questions, and further multiple comparison adjustment was not performed for this reason. A representative sample of survey responses is shown in (Fig. 6 ).
Fig. 6.
Survey responses in Sao Paulo and Rio de Janeiro states compared to the rest of Brazil. Representative sample of survey results divided by geographic areas of Sao Paulo & Rio de Janeiro (SP & RJ) compared to the rest of Brazil from people with epilepsy, caregivers, and health care workers (HCW). Sao Paulo (SP) and Rio de Janeiro (RJ) were grouped to reflect areas of high COVID-19 disease burden compared to the rest of the country. Responses from the people with epilepsy survey (A-C), caregivers (D) and HCW (E) show no notable difference in responses between SP & RJ combined compared to the rest of Brazil. Statistically, there was no significant difference between the geographic categories based on χ2-testing (P > 0.05) in each of these survey questions. This suggests the effect of COVID-19 on epilepsy was not directly related to virus incidence and mortality during the time of the survey.
4. Discussion
The COVID-19 pandemic has had an unprecedented public health impact [41], [42]. We assessed views of people with epilepsy, their caregivers, and HCWs in Brazil, one of the countries most adversely affected by the pandemic [5], [43]. Our results provide further evidence that the indirect burden of the virus is considerable, and we have explored specific factors that may have contributed to this effect.
While some people with epilepsy did not report significant changes, a proportion experienced a decline in their health and wellbeing. Increased stress levels due to difficulties in accessing health services, obtaining ASMs, changing or canceling medical appointments, and anxiety around being infected by attending clinical sites were often highlighted. These factors made access to healthcare even more complex and may explain why all people aged 60 or over, even if living with someone capable of caring for them, reported difficulties during the pandemic. Also, these effects had a real impact, resulting in increased seizures and incidents requiring medical attention.
To assess whether the effects of the pandemic seen in the survey responses were related to the number of infections and deaths for COVID-19, we applied a geographic stratification. We combined survey responses from Sao Paulo and Rio de Janeiro, the two states with the highest number of cases and deaths, to the rest of Brazil. Similar to previous studies, our results suggest that the effects of COVID-19 in people with epilepsy and their caregivers are not directly related to infection case number or mortality [16], [17], [21]. Instead, the reported impact on health and wellbeing more likely reflects individual experiences of public health measures and countrywide changes in healthcare such as resource reallocation, change to telemedicine, and alternative arrangements for obtaining ASM prescriptions.
Comparing survey findings from the Brazilian and British arms of the COV-E study yielded valuable insights [29]. Less than ten percent of those with epilepsy lived alone in Brazil compared to over a quarter (n = 112) in the UK, likely reflecting social and cultural constructs. Despite differences in such home support structures and national health provision, similar proportions of people with epilepsy reported health changes, leading to worsening seizure control [29]. Respondents in the UK and Brazil highlighted mental health issues and increased stress levels as the leading causes for a decline in wellbeing [29]. While such factors were perhaps less appreciated in the early stages of the pandemic, optimizing mental health support, particularly for vulnerable people such as those with epilepsy, is crucial.
Healthcare worker data suggested changes to clinical practice resulting from less availability of investigations and face-to-face review. The increased use of telemedicine, also observed in results from the UK, reflects the pandemic's effect on how medicine is practiced. During the pandemic, Brazilian regulators relaxed telemedicine rules, leading to an expanded use. However, these services were not physically or financially accessible to all, particularly for those without private health insurance [35], [36]. Notably, in the UK and Brazil, clinicians felt less confident at diagnosing epilepsy through telemedicine than they did when performing face-to-face reviews [29].
During the pandemic, when risks to people with epilepsy are higher, there is an increased need to discuss key epilepsy-associated risks [29]. Despite this, just over half of respondents reported discussions with HCWs about sleep and mental health and stress. Other aspects of epilepsy-associated risk and management, including SUDEP, were mentioned even less frequently. Reluctance to discuss these issues remotely or in shorter face-to-face consultations due to restriction measures may be attributable to the healthcare professional, the person with epilepsy, or both. As health services reconstitute, a proportion of clinical work will likely continue to be performed by telemedicine. Therefore, it will be essential to ensure that risk communication is not diluted further still through remote consultations.
Brazil is now experiencing a second wave of COVID-19, resulting in over 500,000 deaths. According to the Brazilian Ministry of Health, more than 17 million people have been infected with a case fatality of 2.8% [7]. Brazil has the third-highest number of cases in the world (https://healthmap.org/covid-19/) [44], [45]. Therefore, the importance of identifying and understanding the factors that affect vulnerable groups' health and wellbeing during the pandemic cannot be overstated.
5. Limitations
The overarching COV-E study's limitations have been previously described [29]. A central issue is the survey's self-reported nature. HCWs provided a large proportion of the Brazilian data, and it will be essential to continue ongoing efforts to improve access for people with epilepsy and their caregivers. We also plan to keep the surveys open and enable people to complete them sequentially to understand better how responses may evolve during the pandemic. There may be future opportunities to add more quantitative elements to data capture, for example directing participants to relevant questionnaires on quality of life and mood. An element of socioeconomic bias may also exist as these surveys required access to a computer, and some information was disseminated on platforms such as social media. These factors could have contributed to the disproportionate number of participants from Rio de Janeiro and Sao Paulo.
The survey covered all regions, but Brazil has continental dimensions, and a large proportion of answers came from the southeast region. Concentrated data provided valuable information from the most populous and socio-economically developed parts of the country that could then be compared to other states. Epilepsy centers in public hospitals offered varying degrees of free remote assistance, but the surveys did not involve questions about remuneration for telemedicine consultations from private HCPs. Shortages of physicians and other epilepsy dedicated professionals to more limited access to health services and the internet in socio-economically disadvantaged cities or regions around the country may have masked an even more complex reality of what those with epilepsy have experienced in the current pandemic.
6. Conclusions
Our study offers additional insights on the effect of COVID-19 on those with epilepsy and epilepsy care services beyond factors directly related to viral infection or mortality. We highlight the need to address mental health issues and the importance of maintaining good communication during such times. Comparing responses from the UK and Brazil shows several similarities and some significant differences. Governments and policymakers will need to consider individual nuances to optimizing national healthcare as services reconstitute and learn from shared international experiences.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. PP is supported by the National Health and Medical Research Council (APP1163708), the Epilepsy Foundation, The University of Melbourne, Monash University, and the and the Weary Dunlop Medical Research Foundation. JF has received research support from the Epilepsy Study Consortium, Epilepsy Foundation, GW/FACES and NINDS. DMA is supported by EpLink, Dravet Syndrome Foundation, McLaughlin grants and Biocodex. NJ is the Bludhorn Professor of International Medicine and receives grant funding from NINDS (NIH U24NS107201, NIH IU54NS100064). JHC is supported by the National Institute of Health Research (NIHR) Biomedical Research Centre at Great Ormond Street Hospital, NIHR, Engineering and Physical Sciences Research Council, GOSH Charity, Epilepsy Research UK, and the Waterloo Foundation. JWS is based at UCLH/UCL Comprehensive Biomedical Research Centre, which receives a proportion of funding from the UK Department of Health's NIHR Biomedical Research Centres funding scheme. He receives support from the Dr Marvin Weil Epilepsy Research Fund, the Christelijke Vereniging voor de verpleging van Lijders aan Epilepsie, The Netherlands, and the UK Epilepsy Society. AS is supported by the Oxford NIHR Biomedical Research Centre at the John Radcliffe Hospital, UK.
Acknowledgments
Acknowledgements
This study was led and funded by SUDEP Action (Registered charity 1164250 (England & Wales)) in collaboration with the Oxford NIHR Biomedical Research Centre.
Conflicts of interest: The authors declare no direct conflicts of interest concerning this work.
We are grateful to all of the following organizations and many individuals we cannot name separately for promoting this work through online platforms. We also very much appreciate the valuable input of all the respondents who have completed the surveys.
ASPE Brazil.
BAND Foundation.
Brazilian Association of Epilepsy.
Brazilian Federation of Epilepsy.
Dravet Syndrome UK.
Epilepsy Action.
Epilepsy Connections.
Epilepsy Foundation America.
Epilepsy Research UK.
Epilepsia Sem Crise.
Epilepsy Society.
Epilepsy Sparks.
International Bureau for Epilepsy.
International League Against Epilepsy – Brazilian Branch.
International League Against Epilepsy – British Branch.
Mães da Epilepsia.
Matthew’s Friends.
Neurological Alliance.
SUDEP Action.
References
- 1.Miller W.R., Von Gaudecker J., Tanner A., Buelow J.M. Epilepsy self-management during a pandemic: experiences of people with epilepsy. Epilepsy Behav. 2020;111 doi: 10.1016/j.yebeh.2020.107238. Epub 2020 Jun 25. PMID: 32593874; PMCID: PMC7316066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hughes G.D., Mbamalu O.N., Okonji C.O., Puoane T.R. The impact of health disparities on COVID-19 outcomes: early findings from a high-income country and two middle-income countries. J Racial Ethn Health Disparities. 2021;8:1–8. doi: 10.1007/s40615-021-00999-5. Epub ahead of print. PMID: 33686624; PMCID: PMC7938881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kola L., Kohrt B.A., Hanlon C., Naslund J.A., Sikander S., Balaji M., et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;(21):00025. doi: 10.1016/S2215-0366(21)00025-0. S2215-0366(21)00025-0. Epub ahead of print. Erratum in: Lancet Psychiatry. 2021 Mar 8;: PMID: 33639109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panda P.K., Dawman L., Panda P., Sharawat I.K. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. Epub 2020 Jul 18. PMID: 32712376; PMCID: PMC7368411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Candido D.S., Claro I.M., de Jesus J.G., Souza W.M., Moreira F.R.R., Dellicour S., et al. Evolution and epidemic spread of SARS-CoV-2 in Brazil. Science. 2020;369(6508):1255–1260. doi: 10.1126/science.abd2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreira R.M., Villa Montoya A.C., Silveria Araujo S.L., Trindade R.A., da Cunha Oliveira D., de Oliveira Marinho G. How prepared is Brazil to tackle the COVID-19 disease? J Glob Health. 2020;10(2) doi: 10.7189/jogh.10.020321. PMID: 33110523; PMCID: PMC7561213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.https://covid.saude.gov.br/ [Date accessed: 23 June 2021].
- 8.Araujo O.R., Almeida C.G., Lima-Setta F., Prata-Barbosa A., Colleti Junior J. Brazilian Research Network in Pediatric Intensive Care (BRnet-PIC). The Impact of the Novel Coronavirus on Brazilian PICUs. Pediatr Crit Care Med. 2020;21(12):1059–1063. doi: 10.1097/PCC.0000000000002583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maselli-Schoueri J.H., de Carvalho L.E.W., Rezende L.F.M., Fonseca F.L.A., Ferrari G., Adami F. Hospital admissions associated with noncommunicable diseases during the COVID-19 outbreak in Brazil. JAMA Netw Open. 2021;4(3) doi: 10.1001/jamanetworkopen.2021.0799. PMID: 33683330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leone M., Ciccacci F., Orlando S., Petrolati S., Guidotti G., Majid N.A., et al. Pandemics and burden of stroke and epilepsy in Sub-Saharan Africa: experience from a Longstanding Health Programme. Int J Environ Res Public Health. 2021;18(5):2766. doi: 10.3390/ijerph18052766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandes P.T., Noronha A.L., Sander J.W., Li L.M. National Epilepsy movement in Brazil. Arq Neuropsiquiatr. 2007;65(Suppl 1):55–57. doi: 10.1590/s0004-282x2007001000009. PMID: 17581669. [DOI] [PubMed] [Google Scholar]
- 12.Lu L., Xiong W., Liu D., Liu J., Yang D., Li N., et al. New onset acute symptomatic seizure and risk factors in coronavirus disease 2019: a retrospective multicenter study. Epilepsia. 2020;61(6):e49–e53. doi: 10.1111/epi.16524. Epub 2020 May 2. PMID: 32304092; PMCID: PMC7264627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hogan R.E., Grinspan Z., Axeen E., Marquis B., Day B.K. COVID-19 in patients with seizures and epilepsy: interpretation of relevant knowledge of presenting signs and symptoms. Epilepsy Curr. 2020;20(5):312–315. doi: 10.1177/1535759720948549. Epub 2020 Aug 24. PMID: 32833573; PMCID: PMC7445677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roy D., Ghosh R., Dubey S., Dubey M.J., Benito-León J., Kanti Ray B. Neurological and neuropsychiatric impacts of COVID-19 pandemic. Can J Neurol Sci. 2021;48(1):9–24. doi: 10.1017/cjn.2020.173. Epub 2020 Aug 5. PMID: 32753076; PMCID: PMC7533477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vohora D., Jain S., Tripathi M., Potschka H. COVID-19 and seizures: Is there a link? Epilepsia. 2020;61(9):1840–1853. doi: 10.1111/epi.16656. Epub 2020 Sep 17. PMID: 32944929; PMCID: PMC7537056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reilly C., Muggeridge A., Cross J.H. The perceived impact of COVID-19 and associated restrictions on young people with epilepsy in the UK: young people and caregiver survey. Seizure. 2021;85:111–114. doi: 10.1016/j.seizure.2020.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.French J.A., Brodie M.J., Caraballo R., Devinsky O., Ding D., Jehi L., et al. Keeping people with epilepsy safe during the COVID-19 pandemic. Neurology. 2020;94(23):1032–1037. doi: 10.1212/WNL.0000000000009632. Epub 2020 Apr 23. PMID: 32327490; PMCID: PMC7455365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuroda N. Epilepsy and COVID-19: associations and important considerations. Epilepsy Behav. 2020;108 doi: 10.1016/j.yebeh.2020.107122. Epub 2020 Apr 22. PMID: 32361677; PMCID: PMC7174174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alkhotani A., Siddiqui M.I., Almuntashri F., Baothman R. The effect of COVID-19 pandemic on seizure control and self-reported stress on patient with epilepsy. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107323. Epub 2020 Jul 14. PMID: 32712565; PMCID: PMC7359799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cabezudo-García P., Ciano-Petersen N.L., Mena-Vázquez N., Pons-Pons G., Castro-Sánchez M.V., Serrano-Castro P.J. Incidence and case fatality rate of COVID-19 in patients with active epilepsy. Neurology. 2020;95(10):e1417–e1425. doi: 10.1212/WNL.0000000000010033. Epub 2020 Jun 17. PMID: 32554773. [DOI] [PubMed] [Google Scholar]
- 21.Giordano A., Siciliano M., De Micco R., Sant'Elia V., Russo A., Tedeschi G., Tessitore A. Correlates of psychological distress in epileptic patients during the COVID-19 outbreak. Epilepsy Behav. 2021;115 doi: 10.1016/j.yebeh.2020.107632. Epub 2020 Nov 19. PMID: 33373874; PMCID: PMC7674117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E., Li W., Deng A., Lin M., Yan B. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020;61(6):1166–1173. doi: 10.1111/epi.16544. Epub 2020 May 22. PMID: 32353184; PMCID: PMC7267575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuroda N. Epilepsy and COVID-19: updated evidence and narrative review. Epilepsy Behav. 2021;116 doi: 10.1016/j.yebeh.2021.107785. Epub 2021 Jan 13. PMID: 33515934; PMCID: PMC7805398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuroda N. Mental health considerations for patients with epilepsy during COVID-19 crisis. Epilepsy Behav. 2020;111 doi: 10.1016/j.yebeh.2020.107198. Epub 2020 May 30. PMID: 32531704; PMCID: PMC7260596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Millevert C., Van Hees S., Siewe Fodjo J.N., Wijtvliet V., Faria de Moura Villela E., Rosso B., et al. Impact of COVID-19 on the lives and psychosocial wellbeing of persons with epilepsy during the third trimester of the pandemic: Results from an international, online survey. Epilepsy Behav. 2021;116:107800. doi: 10.1016/j.yebeh.2021.107800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Modi A.C., Patel A.D., Stevens J., Smith G., Huszti H., Guilfoyle S.M., et al. The psychosocial impact of COVID-19 within the first six months of the pandemic on youth with epilepsy and their caregivers. Epilepsy Behav. 2021;117 doi: 10.1016/j.yebeh.2021.107855. Epub ahead of print. PMID: 33636530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salari M., Etemadifar M., Gharagozli K., Etemad K., Ashrafi F., Ashourizadeh H. Incidence of anxiety in epilepsy during coronavirus disease (COVID-19) pandemic. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107442. Epub 2020 Sep 17. PMID: 32949966; PMCID: PMC7494452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tedrus G.M.A.S., Silva J.F.C.P.D., Barros G.S. The impact of COVID-19 on patients with epilepsy. Arq Neuropsiquiatr. 2021 doi: 10.1590/0004-282X-ANP-2020-0517. S0004-282X2021005003201. Epub ahead of print. PMID: 33681882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thorpe J., Ashby S., Hallab A., Ding D., Andraus M., Dugan P., et al. Evaluating risk to people with epilepsy during the COVID-19 pandemic: preliminary findings from the COV-E study. Epilepsy Behav. 2021;115:107658. doi: 10.1016/j.yebeh.2020.107658. Epub 2020 Nov 28. PMID: 33341393; PMCID: PMC7698680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Hees S., Siewe Fodjo J.N., Wijtvliet V., Van den Bergh R., Faria de Moura Villela E., da Silva C.F., Weckhuysen S., Colebunders R. Access to healthcare and prevalence of anxiety and depression in persons with epilepsy during the COVID-19 pandemic: a multicountry online survey. Epilepsy Behav. 2020;112:107350. doi: 10.1016/j.yebeh.2020.107350. Epub 2020 Sep 10. PMID: 32920373; PMCID: PMC7481834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fujimoto A., Sato K., Enoki H. Change in patient flow in the epilepsy care network due to novel coronavirus infection: an opportunity to strengthen local interdisciplinary epilepsy care with general physicians. Front Neurol. 2020;16(11) doi: 10.3389/fneur.2020.591423. PMID: 33304311; PMCID: PMC7701112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adan G.H., Mitchell J.W., Marson T. Epilepsy care in the COVID-19 era. Clin Med (Lond) 2020;20(4):e104–e106. doi: 10.7861/clinmed.2020-0207. Epub 2020 Jun 9. PMID: 32518102; PMCID: PMC7385807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Banks J., Corrigan D., Grogan R., El-Naggar H., White M., Doran E., et al. LoVE in a time of CoVID: clinician and patient experience using telemedicine for chronic epilepsy management. Epilepsy Behav. 2021;115:107675. doi: 10.1016/j.yebeh.2020.107675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trivisano M., Specchio N., Pietrafusa N., Calabrese C., Ferretti A., Ricci R., et al. Impact of COVID-19 pandemic on pediatric patients with epilepsy – the caregiver perspective. Epilepsy Behav. 2020;113 doi: 10.1016/j.yebeh.2020.107527. Epub 2020 Nov 24. PMID: 33242768; PMCID: PMC7683298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Domingues R.B., Mantese C.E., Aquino E.D.S., Fantini F.G.M.M., Prado G.F.D., Nitrini R. Telemedicine in neurology: current evidence. Arq Neuropsiquiatr. 2020 Dec;78(12):818–826. doi: 10.1590/0004-282X20200131. PMID: 33295422. [DOI] [PubMed] [Google Scholar]
- 36.Lima M.C., Sander M., dos Santos Lunardi M., Ribeiro L.C., Rieger D.K., Lin K., et al. Challenges in telemedicine for adult patients with drug-resistant epilepsy undergoing ketogenic diet treatment during the COVID-19 pandemic in the public healthcare system in Brazil. Epilepsy Behav. 2020;113:107529. doi: 10.1016/j.yebeh.2020.107529. [DOI] [PubMed] [Google Scholar]
- 37.Kuchenbuch M., D'Onofrio G., Wirrell E., Jiang Y., Dupont S., Grinspan Z.M., et al. An accelerated shift in the use of remote systems in epilepsy due to the COVID-19 pandemic. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107376. Epub 2020 Aug 31. PMID: 32882627; PMCID: PMC7457939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.https://sudep.org/epilepsy-risks-and-covid-19-survey-people-epilepsy?fbclid=IwAR0M5ATaHN9iU1CDlZmkcEntyZH1saE4Y_t1uTuvxxYBF4JF2z9mRmcjJdk [Date accessed: 10 June 2021].
- 39.https://www.onlinesurveys.ac.uk/ [Date accessed: 10 June 2021].
- 40.https://cmmid.github.io/visualisations/lacpt [Date accessed: 10 June 2021].
- 41.Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat Hum Behav. 2021 doi: 10.1038/s41562-021-01079-8. Epub ahead of print. PMID: 33686204. [DOI] [PubMed] [Google Scholar]
- 42.Bhaskar S., Bradley S., Israeli-Korn S., Menon B., Chattu V.K., Thomas P., et al. Chronic neurology in COVID-19 era: clinical considerations and recommendations from the REPROGRAM Consortium. Front Neurol. 2020;11 doi: 10.3389/fneur.2020.00664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baqui P., Bica I., Marra V., Ercole A., van der Schaar M. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: a cross-sectional observational study. Lancet Glob Health. 2020;8(8):e1018–e1026. doi: 10.1016/S2214-109X(20)30285-0. Epub 2020 Jul 2. PMID: 32622400; PMCID: PMC7332269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cimerman S., Chebabo A., Cunha C.A.D., Rodríguez-Morales A.J. One year after the arrival of COVID-19 in Latin America: what have we learned in Brazil and other countries? Braz J Infect Dis. 2021;25(2) doi: 10.1016/j.bjid.2021.101571. Epub ahead of print. PMID: 33741322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.https://healthmap.org/covid-19/ [Date accessed: 23 June 2021].