Abstract
Purpose
The impact of the COVID-19 pandemic on adolescent mental health is a global concern; however, most research is cross-sectional or started after the pandemic response began and thus unable to evaluate within-individual change. The purpose of this prospective study was to evaluate the effect of the initial COVID-19 response on adolescent mental health and ill-health as a natural experiment.
Methods
We used 3-year linked data from the COMPASS study, including 7,653 Canadian (Quebec, Ontario) adolescents from which 2,099 completed surveys in all three waves (pre-COVID-19 [2018 and 2019] and online [May–July 2020], 2–3 months into the pandemic). A structural equation modeling approach to fixed effects and a difference-in-differences design were used to estimate pre-COVID-19–to–early lockdown change in mental health (psychosocial well-being [flourishing—reverse scored]) and ill-health (depression and anxiety symptoms), compared with 2018-to-2019 change. Models were adjusted for self-selection, age of entry into the cohort, and sociodemographics.
Results
Depression, anxiety, and reverse-flourishing scores increased across all waves; however, the mental health changes from the pre-COVID-19 wave (2019) to 2020 were not greater relative to the changes seen across the 2018-to-2019 waves.
Conclusions
Our results do not support a detrimental effect of the initial stages of the COVID-19 lockdown measures on adolescent mental health. The deterioration in mental health in the early COVID-19 response was less than the decline found over a prepandemic period. Further prospective research is needed to explore the impact of the prolonged pandemic and related measures on adolescents and inequitable effects in population subgroups.
Keywords: COVID-19, Pandemic, Youth, Mental health, Adolescents, Longitudinal, Prospective, Cohort
Implications and Contribution.
This impact analysis does not support the hypothesized deterioration in the mental health of Canadian adolescents during the initial COVID-19 response. Multi-year linked data from a longitudinal cohort starting pre-COVID-19 lockdown allowed for the robust evaluation of the extent to which adolescents were affected by the early pandemic response.
There is an urgent need to understand the mental health effects of the COVID-19 pandemic and lockdown measures to inform future policy and practice to mitigate harms [[1], [2], [3], [4]]. Adolescents are believed to be at particular risk [5,6], as a critical period of psychosocial development and when most mental disorders emerge [7]. Lockdown measures such as stay-at-home orders and limits on social gatherings are at odds with adolescents' developmental propensity to prioritize peer relationships and seek greater autonomy from their parents [[8], [9], [10], [11]]. Previous school closures had adverse associations with mental well-being and more pronounced effects are expected with COVID-19 [11,12]. The youth were also restricted from engaging in many activities (e.g., recreation, sport) shown to help regulate emotions and promote mental health, whereas potentially detrimental exposures may have increased (e.g., family/home environment stress). Inequitable impacts by sex and gender have been hypothesized, with some evidence suggesting girls and females are at greater risk of adverse effects than boys and males [[13], [14], [15]].
In response, several cross-sectional web surveys have been rapidly developed and reveal a high prevalence of psychological distress and anxiety and depression symptoms among adolescents since the onset of the pandemic and related measures [[16], [17], [18]]. Similarly, Canadian adolescents and young adults reported perceived deterioration in their mental health from 3 months before COVID-19 to 3 weeks into the pandemic, particularly in mood and anxiety [19]. However, these studies rely on comparisons with previous population estimates or individuals' retrospective recollections of how they felt before the pandemic. Prospective designs with prepandemic data are necessary to establish the within-individual impact of ongoing pandemic-related changes [[2], [3], [4]]. This study is among the first to examine mental health changes from pre-COVID-19 to the early pandemic response among a prospective cohort of Canadian adolescents.
Existing prospective studies with prepandemic data are limited by small sample sizes and have mixed results, at times conflicting with cross-sectional or retrospective accounts. In a sample of 451 U.S. adolescents and young adults, increases in generalized and social anxiety symptoms in all participants, and increased depression and panic/somatic symptoms in females only, were found based on surveys conducted between 2014 and 2019 and again in March–May 2020 [14]. Similarly, an Australian study reported increased anxiety and depressive symptoms, and declines in life satisfaction, among 248 adolescents surveyed in the 12 months before the pandemic and two months after implementation of government restrictions and online learning [15]. Greater mental health declines were found among females than males [15]. However, modest effect sizes led the authors to conclude that most adolescents are coping well and showing minimal negative impact in the early stages of the pandemic [19]. Contrary to expectations, in a primarily Hispanic/Latinx sample of 322 early adolescents in a Southwestern U.S. city, internalizing symptoms declined from assessments conducted pre-COVID-19 to three time points during the pandemic [20]. Inconsistencies across prospective studies may reflect differences in sample demographics, timing of assessments, regional COVID-19 prevalence and lockdown measures, and social support systems available. Furthermore, adjustment for age-related changes over time is necessary, given evidence of increases in anxiety and depressive symptoms and reduced life satisfaction across adolescence [21,22].
The purpose of this study is to leverage prepandemic and early-pandemic data from an ongoing Canadian prospective cohort study to evaluate the effect of COVID-19 on youth mental health as a natural experiment. Specifically, we tested the hypothesis that mental health among adolescents would deteriorate from pre-COVID-19 to the early enactment of pandemic-related measures, to a greater extent than expected to occur over this time period, based on changes seen across prepandemic waves. Sex- and age-specific changes were also examined.
Methods
Design
The Cannabis use, Obesity, Mental health, Physical activity, Alcohol use, Smoking, and Sedentary behavior (COMPASS) Study is an ongoing prospective study designed to collect hierarchical health data once annually from a rolling cohort of students in grades 9 through 12 (secondary I–V in Quebec) and the secondary schools they attend [23]. School boards and schools were purposefully selected based on whether they permitted active-information passive-consent parental permission protocols, which are critical for collecting robust youth data [24]. All students attending participating schools and not withdrawn by their parents were eligible to participate. All participating students provided assent. Surveys include a set of questions to create unique student codes, maintaining anonymity while enabling individual student data to be linked across participation waves [23]. School data collections are typically scheduled between October and June; each school's date is kept similar across waves. All procedures received ethics approval from the University of Waterloo (ORE#30118), Brock University (REB#18–099), CIUSSS de la Capitale-Nationale–Université Laval (#MP-13-2017-1264), and participating school boards. Additional details regarding the COMPASS study methods can be found online (www.compass.uwaterloo.ca) or in print [23].
To evaluate the effect of COVID-19 and related measures as a natural experiment, we used 3-year linked survey data collected from students who attended 43 schools in Ontario (N = 20) and Quebec (N = 23) and participated in the spring of the 2017/18 (81.8% response rate) and 2018/19 (84.2% response rate) school years and in May–July 2020 (29.2% response rate). In 2018 and 2019, student data were collected using a paper-based survey completed during one classroom period by whole school samples. In 2020, as the 43 schools were closed for in-person learning due to the COVID-19 pandemic response, surveys were conducted online using Qualtrics XM online survey software (Qualtrics, Provo, UT, USA). A survey link was emailed to all students by their schools, followed by a reminder email one week after [25]. Most initial emails were sent out on May 12, 2020; the earliest school email was sent on May 1, 2020 [25]. Ontario and B.C. surveys were left open for two weeks after the initial email, and Quebec surveys, for 4 weeks [25]; the last survey closed on July 6, 2020.
Measures
Depression symptoms
Depressive symptoms were measured using the 10-item Center for Epidemiologic Studies Depression Scale Revised [[26], [27], [28]]. Students were asked how often they experienced each symptom within the last 7 days. Sum scores had a plausible range of 0–30, with higher scores indicative of greater depressive symptoms.
Anxiety symptoms
Anxiety symptoms were measured using the 7-item Generalized Anxiety Disorder scale [29,30]. Students were asked how often they experienced each symptom in the last 2 weeks. Sum scores had a possible range of 0–21, with higher scores indicating greater anxiety symptoms.
Flourishing
Diener's 8-item Flourishing Scale [31,32] was used to assess how the youth perceived their relationships, life purpose and satisfaction, engagement and interest with daily activities, optimism, and self-esteem and competence, to provide a total score that reflects overall psychosocial well-being. The original 7-point Likert scale was simplified to 5 points, omitting the “slightly agree” and “slightly disagree”, to be suitable for a large school-based survey [32]. Scores were reversed to be consistent in direction with the other mental health scales, meaning possible scores ranged from 0–32, with lower scores indicating higher flourishing.
Statistical analysis
Consistent with the approach used in a previous study [33], in the absence of a possible control group, we used an evaluation design to compare annual variations in the cohort respondents' mental health between the two pre-COVID-19 study waves (2018, 2019) and the two waves straddling the early COVID-19 era (2019, 2020). First, mean potential outcomes (i.e., estimated average adjusted predictions) and average treatment effects were obtained using Stata 15 structural equation modeling (SEM) and generalized SEM routines (StataCorp, 2017). We used a lagged dependent variable, where mental health in the prior year predicted mental health in following wave. We used a fixed effect method using SEM as recommended by Allison [34], given the advantages of simultaneously controlling for time-invariant unobserved confounders and producing final estimates for time-invariant predictors (sex and age at entry into the 2018 cohort). A structural model was assessed for each of the three outcomes; each model included three equations (one for each year). Following Allison's [334] approach, each set of equations included a vector of invariant predictors (sex, age at entry into the cohort) as well as a latent term (alpha) representing all other unobserved stable differences between individuals. The full information maximum likelihood method was used to control for missing data. Robust estimators accounted for school clustering.
An additional complication resides in the self-selection process encountered in the 2020 online survey. To account for self-selection in 2020, the initial models (type 1 model) were supplemented by Heckman-type sample selection models (models 2 and 3) [35]. A selection equation was first estimated (probit equation) using a set of individual and family predictors of self-selection (i.e., factors associated with participation in 2020: age of entry into the cohort, sex, weekly spending money, province, and school connectedness). The inverse Mills ratio was generated and introduced as an additional explanatory variable into the 2020 equation of each SEM model to correct for selection bias.
We assume that without the effect of COVID-19 and related measures, annual changes in mental health among students would be the same between the pre-COVID-19 waves (2018–2019) and the early phases of the COVID-19 response (2019–2020). The hypothesis of a different progression in mental health outcomes in each of the two periods was tested using a difference-in-differences design [[36], [37], [38]], which provides an estimation of the average effect of the COVID-19 pandemic and early lockdown response on participant mental health. Difference-in-differences calculations were performed in three steps. First, the mean predicted values are obtained under the counterfactual scenarios. Second, simple differences are computed by subtracting the mean potential outcomes across the two periods (i.e., pre-COVID-19 period [2019 minus 2018] and the early COVID-19 period [2020 minus 2019]). Third, the causal effect is estimated using difference-in-differences, by subtracting the difference in the early COVID-19 period (2020 minus 2019) from the difference in the pre-COVID-19 period (2019 minus 2018). The 95% confidence intervals were estimated based on robust Huber-White standard errors.
Results
Survey data from 7,653 eligible participants who completed the survey in the 2018 and 2019 waves were considered for analysis. Of them, 2,099 also participated in the 2020 online wave, completing all three waves of data collection. Participants entered the cohort in 2018 with a mean age of 14.1 (standard deviation 1.0) years old with just over half (53%) identifying themselves as females and 83% as white.
See Table 1 for observed mean scores of the mental health scales among eligible secondary school students across the three waves.
Table 1.
Observed mental health scores among students attending 43 secondary schools with linked survey data across three waves of the COMPASS study
| Wave | Depression |
Anxiety |
Flourishing—reversed |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean (SD) | α | N | Mean (SD) | α | N | Mean (SD) | α | |
| 2018 | 7,317 | 7.64 (5.65) | .80 | 7,061 | 5.27 (5.15) | .89 | 6,500 | 6.99 (5.71) | .90 |
| 2019 | 7,354 | 8.61 (5.97) | .82 | 7,106 | 6.06 (5.51) | .90 | 6,554 | 7.65 (5.92) | .90 |
| 2020 | 1,880 | 8.88 (5.96) | .81 | 1,863 | 6.23 (5.44) | .90 | 1,678 | 7.29 (5.74) | .90 |
Depression: CESD-10, range 0–30; Anxiety: GAD-7, range 0–21; Flourishing—reversed: Diener's 8-item Flourishing Scale, range 0–32 with lower numbers depicting higher flourishing. α = Cronbach's alpha.
COMPASS = Cannabis use, Obesity, Mental health, Physical activity, Alcohol use, Smoking, and Sedentary behavior; SD = standard deviation.
Potential outcome means (i.e., estimated average adjusted predictions) for depression, anxiety, and flourishing over study waves can be found in Table 2 . For all three mental health measures, for all three models, potential outcome means increased between each wave. Consequently, the highest scores are found during the last wave (2020). Average discrete change between years decreased between periods, indicating that deterioration of estimated mental health scores within the second period (2019–2020), crossing the early COVID-19 pandemic and the enactment of preventive measures, was lower than that in the pre-COVID-19 period (2018–2019). For all mental health measures, and all models performed, even after accounting for predictors of self-selection (model 3), the negative estimated causal effects do not support the hypothesis of a deterioration in the mental health of Canadian adolescents related to the initial COVID-19 response.
Table 2.
Potential outcome means, discrete change of mental health over survey waves, and estimated causal effect among students attending 43 secondary schools with linked survey data across three waves of the COMPASS study
| Depression |
Anxiety |
Flourishing—reversed |
||||||
|---|---|---|---|---|---|---|---|---|
| Model 2 | Model 3 | Model 2 | Model 3 | Model 2 | Model 3 | |||
| Potential outcome mean | 2018 | Mean [95% CI] | 7.64 [7.36, 7.92] | 7.65 [7.37, 7.94] | 5.28 [5.02, 5.55] | 5.29 [5.03, 5.55] | 7.01 [6.61, 7.40] | 6.99 [6.61, 7.37] |
| 2019 | 8.61 [8.40, 8.83] | 8.62 [8.42, 8.82] | 6.05 [5.82, 6.28] | 6.06 [5.84, 6.28] | 7.61 [7.30, 7.93] | 7.59 [7.30, 7.89] | ||
| 2020 | 9.09 [8.66, 9.53] | 9.09 [8.66, 9.52] | 6.36 [6.04, 6.68] | 6.32 [5.97, 6.66] | 7.70 [7.27, 8.13] | 7.61 [7.14, 8.08] | ||
| Average discrete change | 2019–18 (Pre) | Dif. Mean [95% CI] | .97 [.81, 1.14] | .97 [.79, 1.14] | .77 [.62, .91] | .77 [.62, .92] | .61 [.42, .79] | .61 [.42, .80] |
| 2020–19 (Per) | .48 [.10, .87] | .47 [.10, .83] | .30 [.07, .53] | .26 [.02, .50] | .09 [−.24, .41] | .01 [−.35, .38] | ||
| Estimated causal effect | Per - Pre | Dif.-In-Dif. [95% CI] | −.49 [−.93, −.05] | −.50 [−.94, −.05] | −.47 [−.74, −.19] | −.51 [−.83, −.20] | −.52 [−.92, −.13] | −.59 [−1.05, −.14] |
Model 1 (Not shown): Base model. Fixed effect model controlling for time-invariant unobservables; the lagged variable is the outcome; covariates used: sex interaction with age at entry.
Model 2: Model 1 but constraining sex/age effects on outcomes to be fixed across time and sample selection correction with predictors of selection: age, sex, and weekly spending money.
Model 3: Model 2 with predictors of selection: age, sex, weekly spending money, province, and school connectedness (predictor IMR).
Depression: CESD-10, range 0–30; Anxiety: GAD-7, range 0–21; Flourishing—reversed: Diener's 8-item Flourishing Scale, range 0–32 with lower numbers depicting higher flourishing.
CI = confidence interval; COMPASS = Cannabis use, Obesity, Mental health, Physical activity, Alcohol use, Smoking, and Sedentary behavior.
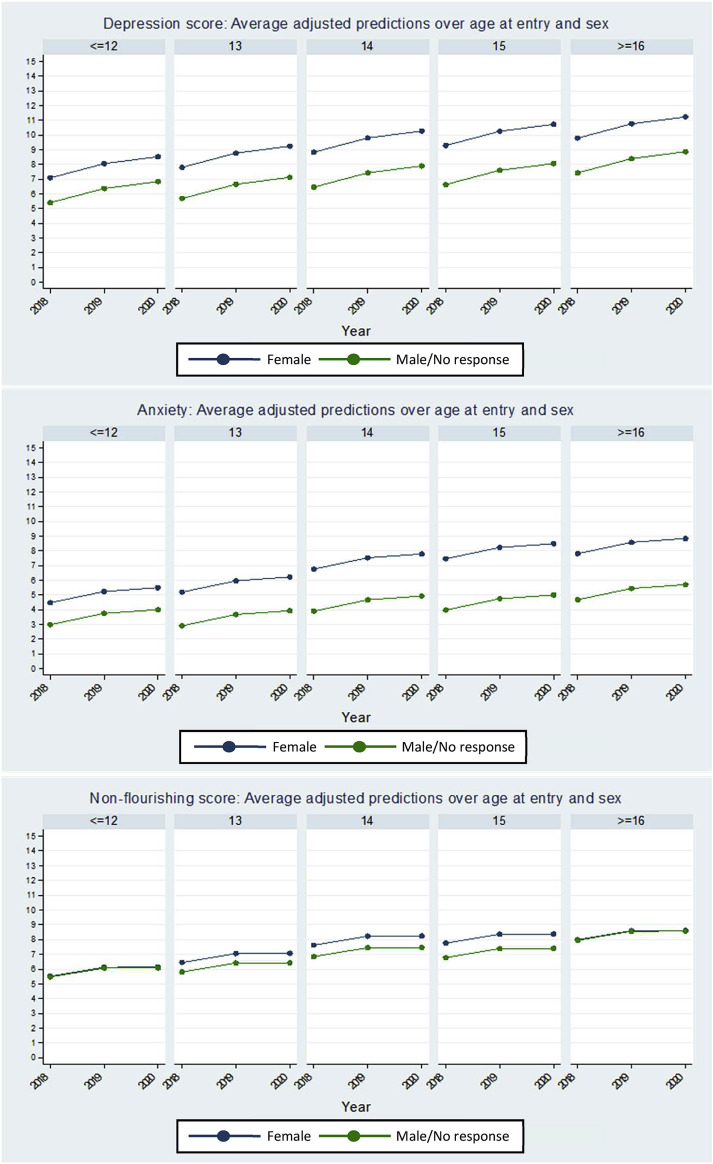
To ascertain the possible differential impact of the early COVID-19 pandemic measures based on sex and age at entry into the cohort, stratified potential outcome means, discrete changes in predictions, and estimated causal effects are presented in Table 3 and Figure 1 . Based on model 3, females and older adolescents reported greater scores on all mental health measures across all waves, yet neither sex nor age at entry appeared to lead to a greater deterioration between the first and the second period. Accordingly, all estimated causal effects were negative.
Table 3.
Average discrete change over survey wave and estimated causal effects for mental health scores, stratified by sex, among students attending 43 secondary schools with linked survey data across three waves of the COMPASS study
| Depression |
Anxiety |
Flourishing—reversed |
||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male/No response | Female | Male/No response | Female | Male/No response | |||
| Average discrete change | 2019–18 (Pre) | Dif. Mean [95% CI] | 1.14 [.93, 1.36] | .76 [.60, .92] | .96 [.77, 1.15] | .55 [.40, .70] | .00 [−.34, .35] | .54 [.36, .73] |
| 2020–19 (Per) | .33 [−.09, .74] | .64 [.24, 1.04] | .25 [−.02, .52] | .26 [−.07, .59] | −.52 [−1.10, .07] | .66 [.47, .85] | ||
| Estimated causal effect | Per - Pre | Dif.-In-Dif. [95% CI] | −.82 [−1.33, −.31] | −.11 [−.59, .36] | −.71 [−1.05, −.36] | −.29 [−.67, .09] | −.66 [−1.07, −.24] | .03 [−.46, .51] |
Based on model 3: Fixed effect model controlling for time-invariant unobservables; the lagged variable is the outcome; constraining age effects on outcomes to be fixed across time and sample selection correction with predictors of selection: age, sex, weekly spending money, province, and school connectedness (predictor IMR).
Depression: CESD-10, range 0–30; Anxiety: GAD-7, range 0–21; Flourishing—reversed: Diener's 8-item Flourishing Scale, range 0–32 with lower numbers depicting higher flourishing.
CI = confidence interval; COMPASS = Cannabis use, Obesity, Mental health, Physical activity, Alcohol use, Smoking, and Sedentary behavior.
Figure 1.
Average adjusted predictions across waves for mental health scores by age at entry and sex among students attending 43 secondary schools with 3-year linked survey data.
Discussion
The potential mental health impact of the COVID-19 pandemic and related preventative measures has raised global concern, with adolescence believed to be a particularly vulnerable period. This natural experiment study is among the first to evaluate the effect of the early pandemic response on the mental health of Canadian adolescents in a prospective cohort with prepandemic data. Using survey data linked across three study waves and adjusting for self-selection bias, there was no evidence of an adverse effect of the COVID-19 initial lockdown on the mental health of adolescents in Ontario and Quebec, Canada. Although mental health generally deteriorated from 2019 to 2020, the decline was less than would have typically been expected over this time period based on changes found over pre-COVID-19 waves. In fact, the increase in depression and anxiety symptoms from 2019 to spring 2020 was about half of the change found over the same time period a year prior, and flourishing declined by approximately 90% less than the 2018-to-2019 change. Neither sex nor age at entry into the cohort appeared to be risk factors for greater deterioration of mental health between the two periods. Although females had higher internalizing symptoms and poorer psychosocial well-being across all three waves, the effect of the early COVID-19 pandemic response appears largely parallel across sex. Continued prospective analysis is needed over the prolonged and fluctuating course of the pandemic, with schools reopening and closing again in the subsequent waves.
Contrary to our findings, a systematic review of early studies on adolescent psychiatric disorders during the COVID-19 outbreak found support for increased risk of depressive and anxiety symptoms [21]; however, most studies have used cross-sectional designs, and new COVID-19 studies lack prepandemic data and therefore are unable to determine within-individual effects [[2], [3], [4]]. Results of the few extant prospective studies with prepandemic data have been mixed [14,15,20]. Magson et al. [15] found modest increases in depression and anxiety symptoms and decreased life satisfaction in Australian adolescents. Similarly, in a U.S. adolescent and young adult sample, Hawes et al. [14] reported increased anxiety in all participants and increased depression in females only. In contrast, Penner et al. [20] found decreased internalizing symptoms in a primarily Latinx/Hispanic U.S. sample of adolescents. Our study provides prospective evidence in a Canadian sample and builds on the existing literature using a relatively larger sample and robust impact analysis, in which we built counterfactuals and adjusted for self-selection by leveraging linked data across prepandemic waves.
As we look toward lifting pandemic measures, our results underline calls for not returning to “normal” but establishing a “new normal”. We found continued declines in mental health across all three waves, albeit to a lesser extent in the early pandemic response period than in the pre-COVID-19 period. Essentially, pandemic measures put a pause on many adolescents' day-to-day lives, with schools closed to in-person learning, canceled extracurricular activities (sports, recreation, etc.), and limits to face-to-face social interactions outside of household members. School closures may have also allowed more family time and respite for the youth with adverse school experiences [1]. This interruption appears to have blunted age-related deterioration in mental health during adolescence [22,39]. However, although some causal or risk factors in the pre-COVID-19 period may have been temporarily abated, it remains plausible that new concerns introduced by the pandemic response contributed to continued increases in depression and anxiety symptoms. It is important to note that our analysis only allows comparison of the relative magnitude of changes; we are unable to determine the mechanisms responsible for mental health changes in either the pre-COVID-19 or the early pandemic response period. In a Swiss study, the approximately one in five young adults who reported feeling better than before the pandemic had an appreciation for the opportunity to slow down, relax and rest, spend more time with family and close friends, engage in hobbies, and sleep and the removal of educational pressures [40]. The authors note the importance of considering findings in the context of secular trends of increasing reports of psychological distress and internalizing symptoms among the Western youth [40]. More attention is needed to explore contributing factors in the school context or other aspects of adolescents' lives that were disrupted (e.g., academic-related stress, bullying, school schedules) or new influences that were introduced (e.g., greater family and/or sleep time) that explain these findings.
Since the initial lockdown in spring 2020, the portrait of mental health depicted here may have changed for the worst, as suspected by many researchers [4]. The pandemic was under relative control in spring 2020 in most areas in Canada, albeit with inequitable impacts. Ongoing prospective research is needed to examine the impact of prolonged and continually changing pandemic measures, disparate effects in marginalized and socially disadvantaged populations, and whether effects are sustained over time. Wade et al. [4] proposed five developmentally informed potential effect pathways: cumulative (exposure to multiple risk factors depletes the ability to overcome future stressors), sleeper (consequences surface later), sensitizing (pandemic-related stress lowers tolerance thresholds for later challenges), mechanistic (mediation of effect pathways), and resilience (process in which resources foster adaptation to challenges). All potential pathways necessitate ongoing and comprehensive prospective research to robustly evaluate the unpredictable course of the pandemic.
The overall consistency of results across three mental health scales adds further confidence in the legitimacy of our findings. To reflect Keyes' model of complete mental health [41], where mental health and illness exist on separate continua, our outcomes assessed positive mental health (flourishing-languishing) and two of the most common mental illnesses among adolescents [42]. Results were generally equivalent for depression and anxiety; however, the early pandemic response appears to have diminished increases in internalizing symptoms to a lesser degree than the declines in psychosocial well-being. Flourishing scores were generally comparable across 2019 and spring 2020, unlike the decline found between 2018 and 2019. Factors contributing to pre-COVID-19 trends in depression and anxiety symptoms over time may have been less disrupted by the lockdown than those responsible for declines in psychosocial well-being. For instance, depression and anxiety have a large biological susceptibility [43], with most mental disorders having their onset in adolescence [7]. The dual continuum model highlights potential to promote mental health among all and the need for targeted prevention of mental illness among higher-risk populations. Further research is needed to examine differential impacts in adolescents with pre-existing mental ill-health.
Strengths and limitations
The key strengths of this study include the use of well-validated mental health measures, examination of both psychopathology and mental well-being, and the prospective cohort design with early lockdown data linked to two years of pre-COVID-19 data from adolescents in two Canadian provinces, allowing evaluation of within-individual effects and adjustment for age-related changes and self-selection. Several limitations require mention. Although self-report data are prone to recall and social desirability bias, COMPASS uses passive consent protocols which are shown to better reach students at risk of depression [24] and does not require student names, helping to preserve perceptions of anonymity for honest reporting. In terms of the statistical models, we built counterfactuals in the absence of a possible comparison group, but difference-in-differences designs are limited by assuming parallel trends; therefore, there is no control for within-individual variations over time related to time-varying unobserved characteristics (e.g., changes in socioeconomic status). Future studies are needed to examine modifying effects of socioeconomic status, which require a different analytic approach. The change from school-based paper-and-pencil questionnaires to online assessment may have influenced reports. The lower online response rates may bias the results; students not responding may be at higher risk of adverse mental health impacts. We corrected for self-selection by adjusting for factors that predicted participation in the 2020 wave (age, sex, weekly spending money, province, school connectedness). However, the consistency of estimates may be affected if there are departures from the statistical assumptions of sample selection models (e.g., assuming error terms that are jointly normally distributed). Finally, as COMPASS was not designed to be representative, results may not be generalizable to all Canadian adolescents.
Conclusions
This evaluation study adds to the growing evidence base on the impact of COVID-19 on adolescent mental health and ill-health. In a three-year cohort of Canadian adolescents, we found no evidence of an adverse effect of the early pandemic response on mental health. Although mental health deteriorated across all waves, the decline in the early COVID-19 period was relatively less than expected based on the pre-COVID-19 period. The lockdown interruptions appear to have diminished anticipated deteriorations in mental health. These deteriorations seen over time have implications as we move toward lifting pandemic measures and highlight the importance of considering opportunities to establish a “new normal” that is more supportive of mental health and the prevention of mental illness among the youth. Further prospective research is needed to explore changes over the prolonged and unpredictable course of the pandemic and inequitable impacts among subgroups at greater risk.
Acknowledgments
The authors would like to thank the schools, school boards, and students that have participated in the COMPASS study and all COMPASS staff and team members.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Funding Sources
The COMPASS study has been supported by a bridge grant from the CIHR Institute of Nutrition, Metabolism and Diabetes (INMD) through the “Obesity – Interventions to Prevent or Treat” priority funding awards (OOP-110788; awarded to S.T.L.), an operating grant from the CIHR Institute of Population and Public Health (IPPH) (MOP-114875; awarded to S.T.L.), CIHR Project Grants (PJT-148562 awarded to S.T.L.; PJT-159693 awarded to K.A.P.), and a research funding arrangement with Health Canada (#1617-HQ-000012; awarded to S.T.L.). The COMPASS-Quebec data benefit from funding from the Ministère de la Santé et des Services sociaux of the province of Québec and the Direction régionale de santé publique du CIUSSS de la Capitale-Nationale (awarded to S.H. and R.E.B.). A SickKids Foundation New Investigator Grant, in partnership with CIHR Institute of Human Development, Child and Youth Health (IHDCYH) (Grant No. NI21-1193; awarded to K.A.P.), funds a mixed-methods study examining the impact of the COVID-19 pandemic on youth mental health, leveraging COMPASS study data.
References
- 1.Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holmes E.A., O’Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwong A.S.F., Pearson R.M., Adams M.J., et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. The Br J Psychiatry. 2021:1–10. doi: 10.1192/bjp.2020.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wade M., Prime H., Browne D. Letter to the Editor: Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatry Res. 2020;290:113143. doi: 10.1016/j.psychres.2020.113143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 6.Zhou S.J., Zhang L.G., Wang L.L., et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler R.C., Amminger G.P., Aguilar-Gaxiola S., et al. Age of onset of mental disorders: A review of recent literature. Curr Opin Psychiatry. 2007;20:359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee J. Mental health effects of school closures during COVID-19. Lancet. 2020;395:912–920. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loades M.E., Chatburn E., Higson-Sweeney N., et al. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orben A., Tomova L., Blakemore S.-J. The effects of social deprivation on adolescent development and mental health. Lancet. 2020;4:634–640. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ontario Agency for Health Protection and Promotion (Public Health Ontario) Queen’s Printer for Ontario; Toronto, ON: 2020. Rapid Review: Negative impacts of community-based public health measures during a pandemic (e.g., COVID-19) on children and families. [Google Scholar]
- 12.UNESCO Framework for reopening schools. April 2020. https://unesdoc.unesco.org/ark:/48223/pf0000373348 Available at:
- 13.Canadian Institutes of Health Research Why sex and gender need to be considered in COVID-19 research: A guide for applicants and peer reviewers. 2020. https://cihr-irsc.gc.ca/e/51939.html Available at:
- 14.Hawes M.T., Szenczy A.K., Klein D.N., et al. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2021:1–9. doi: 10.1017/S0033291720005358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magson N.R., Freeman J.Y., Rapee R.M., et al. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mental Health Commission of Canada, Conference Board of Canada How has COVID-19 impacted Canadians’ mental health? https://www.conferenceboard.ca/focus-areas/health/how-has-covid-19-impacted-canadians-mental-health Available at:
- 17.Ispos, CMHO, AMHO CMHO/AMHO mental health Week Poll. May 2020. https://amho.ca/mhw-poll/ Available at:
- 18.Statistics Canada Canadians’ mental Health during the COVID-19 pandemic. https://www150.statcan.gc.ca/n1/daily-quotidien/200527/dq200527b-eng.htm Available at:
- 19.Hawke L.D., Barbic S.P., Voineskos A., et al. Impacts of COVID-19 on youth mental health, Substance Use, and well-being: A Rapid survey of clinical and Community samples. Can J Psychiatry. 2020;65:701–709. doi: 10.1177/0706743720940562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Penner F., Ortiz J.H., Sharp C. Change in youth mental health during the COVID-19 pandemic in a majority Hispanic/Latinx US sample. J Am Acad Child Adolesc Psychiatry. 2020;S0890-8567:32212–32217. doi: 10.1016/j.jaac.2020.12.027. [DOI] [PubMed] [Google Scholar]
- 21.Guessoum S.B., Lachal J., Radjack R., et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldbeck L., Schmitz T.G., Besier T., et al. Life satisfaction decreases during adolescence. Qual Life Res. 2007;16:969–979. doi: 10.1007/s11136-007-9205-5. [DOI] [PubMed] [Google Scholar]
- 23.Leatherdale S.T., Brown K.S., Carson V., et al. The COMPASS study: A longitudinal hierarchical research platform for evaluating natural experiments related to changes in school-level programs, policies and built environment resources. BMC Public Health. 2014;14:331. doi: 10.1186/1471-2458-14-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chartier M., Vander Stoep A., McCauley E., et al. Passive versus active parental consent: Implications for the ability of school-based depression screening to reach youth at risk. J Sch Health. 2008;78:157–186. doi: 10.1111/j.1746-1561.2007.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reel B., Battista K., Leatherdale S.T. COMPASS protocol changes and recruitment for online survey implementation during the Covid-19 pandemic. Vol. 7. University of Waterloo; Waterloo, Ontario: 2020. (Technical Report Series). [Google Scholar]
- 26.Andresen E.M., Malmgren J.A., Carter W.B., Patrick D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 27.Zhang W., O’Brien N., Forrest J.I., et al. Validating a shorted depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7:e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haroz E.E., Ybarra M., Eaton W.W. Psychometric evaluation of a self-report scale to measure adolescent depression: The CESDR-10 in two national adolescent samples in the United States. J Affect Disord. 2014;158:154–160. doi: 10.1016/j.jad.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 30.Tiirikainen K., Haravuori H., Ranta K., et al. Psychometric properties of the 7-item Generalized Anxiety Disorder Scale (GAD-7) in a large representative sample of Finnish adolescents. Psychiatry Res. 2019;272:30–35. doi: 10.1016/j.psychres.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Diener E., Wirtz D., Tov W., et al. New measures of well-being: Flourishing and positive and negative feelings. Soc Indic Res. 2010;97:143–156. [Google Scholar]
- 32.Romano I., Ferro M.A., Patte K.A., et al. Measurement invariance of the flourishing scale among a large sample of Canadian adolescents. IJERPH. 2020;17:7800. doi: 10.3390/ijerph17217800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leatherdale S.T., Bélanger R.E., Gansaonré R.J., et al. Examining the impact of the early stages of the COVID-19 pandemic response on youth cannabis use: Adjusted annual changes between the pre-COVID and initial COVID-lockdown waves of the COMPASS study. BMC Public Health. 2021;21:1181. doi: 10.1186/s12889-021-11241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Allison P.D. Sage Publications; Thousand Oaks, CA: 2009. Fixed effects Regression models. [Google Scholar]
- 35.Wooldridge J. Simple solutions to the initial conditions problem in dynamic, nonlinear panel data models with unobserved heterogeneity. J Appl Econom. 2005;20:39–54. [Google Scholar]
- 36.Lechner M. The estimation of causal effects by difference-in-difference methods. Foundations Trends® Econom. 2011;4:165–224. [Google Scholar]
- 37.Gertler P.J., Martinez S., Premand P., et al. Inter-American Development Bank and World Bank. © World Bank; Washington DC: 2016. Impact evaluation in practice. [Google Scholar]
- 38.Wing C., Simon K., Bello-Gomez R.A. Designing difference in difference studies: Best practices for public health policy research. Annu Rev Public Health. 2018;39:453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- 39.Rapee R.M., Oar E.L., Johnco C.J., et al. Adolescent development and risk for the onset of social-emotional disorders: A review and conceptual model. Behav Res Ther. 2019;123:103501. doi: 10.1016/j.brat.2019.103501. [DOI] [PubMed] [Google Scholar]
- 40.Shanahan L., Steinhoff A., Bechtiger L., et al. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychol Med. 2020;23:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Westerhof G.J., Keyes C.L. Mental illness and mental health: The two continua model across the lifespan. J Adult Dev. 2010;17:110–119. doi: 10.1007/s10804-009-9082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Merikangas K.R., He J.P., Burstein M., et al. Lifetime prevalence of mental disorders in U.S. Adolescents: Results from the national Comorbidity survey Replication--adolescent supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hettema J.M. What is the genetic relationship between anxiety and depression? Am J Med Genet C Semin Med Genet. 2008;148C:140–147. doi: 10.1002/ajmg.c.30171. [DOI] [PubMed] [Google Scholar]