Abstract
There is an increasing evidence that meteorological (temperature, relative humidity, dew) and air quality indicators (PM2.5, PM10, NO2, SO2, CO) are affecting the COVID-19 transmission rate and the number of deaths in many countries around the globe. However, there are contradictory results due to limited observations of these parameters and absence of conclusive evidence on such relationships in cold or hot arid tropical and subtropical desert climate of Gulf region. This is the first study exploring the relationships of the meteorological (temperature, relative humidity, and dew) and air quality indicators (PM10,CO, and SO2) with daily COVID-19 infections and death cases for a period of six months (1st March to August 31, 2020) in six selected cities of the Kingdom of Saudi Arabia by using generalized additive model. The Akaike information criterion (AIC) was used to assess factors affecting the infections rate and deaths through the selection of best model whereas overfitting of multivariate model was avoided by using cross-validation. Spearman correlation indicated that exponentially weighted moving average (EWMA) temperature and relative humidity (R > 0.5, P < 0.0001) are the main variables affecting the daily COVID-19 infections and deaths. EWMA temperature and relative humidity showed non linear relationships with the number of COVID-19 infections and deaths (DF > 1, P < 0.0001). Daily COVID-19 infections showed a positive relationship at temperature between 23 and 34.5 °C and relative humidity ranging from 30 to 60%; a negative relationship was found below and/or above these ranges. Similarly, the number of deaths had a positive relationship at temperature ˃28.7 °C and with relative humidity ˂40%, showing higher number of deaths above this temperature and below this relative humidity rate. All air quality indicators had linear relationships with the number of COVID-19 infections and deaths (P < 0.0001). Hence, variation in temperature, relative humidity and air pollution indicators could be important factors influencing the COVID-19 spread and mortality. Under the current scenario with rising temperature and relative humidity, the number of cases is increasing, hence it justifies an active government policy to lessen COVID-19 infection rate.
Keywords: Air pollution, Arid tropical and subtropical desert climate, COVID-19, Generalized additive model, Gulf
1. Introduction
The novel virus, severe acute respiratory syndrome corona 2 (SARS-CoV-2), had initiated an outbreak of corona virus disease (COVID-19) around the globe (WHO, 2020). Immediately after its discovery in December 2019, this virus had increased the number of pneumonia patients in Wuhan China (Huang et al., 2020; Zhou et al., 2020). From the reports, it appeared that the seafood market was responsible for spreading the majority of the early cases in China, but laterally the disease spread around the globe through its transmission by human-to-human contact (Zhou et al., 2020). Therefore, its “community spread” nature made this a high frequency spreading virus in humans within short time (Kraemer et al., 2020). Because of its high spreading nature, the number of infected persons reached over 925,000 with 46000 mortalities in a very short interval of time (until April 1, 2020) globally (Worldometers, 2021). The forceful counteractive measures and travel restrictions (Ahmadi et al., 2021) proved effective in reducing the number of daily new cases, but herd immunity absence against COVID-19 advocated that the infection counts would resurge when the life return to normalcy (Aleta et al., 2020). Many studies already warned about its second wave when severe restrictions around the globe such as social-distancing measures, would be lifted (Aleta et al., 2020; Xu and Li, 2020). Currently, most of the continents are facing a third wave of COVID-19, where it spread in 221 countries with the number of infected people reached to 119, 728,651 and 2,653, 822 mortalities until March 13, 2021 (Worldometers, 2021).
The SARS-CoV-2 enters the human body through different routes. These include the inhalation of aerosols, respiratory droplets produced after coughing or sneezing activity of the infected persons (Fang et al., 2020), and close contact with virus contaminated surfaces. Recent reports showed that the COVID-19 virus can make a cluster with air particulate matter (PM) (Setti et al., 2020) and therefore this virus can potentially spread to people with aerosol (Liu et al., 2020b). Moreover, increasing PM2.5 concentration in the atmosphere can increase the infection and mortality rates in COVID-19 patients (Salim and Raza, 2020; Wu et al., 2020a). The respiratory droplets can stay for long time in humid air and therefore influenced the daily infections and mortality rate associated with COVID-19 pneumonia (Biktasheva, 2020). Consequently, it is important to understand how environmental variables such as air humidity and temperature can play a role in the spread, transmission and preventing COVID-19 infection. Such information will not only be helpful for policy maker to make guidelines about the viral spread but also beneficial for the public.
Seasonal cyclicity is a ubiquitous feature of any acute infectious disease (Martinez, 2018). Such phenomenon is generally found in most viral respiratory diseases (Martinez, 2018). The common example is influenza which displayed a strong seasonal cyclicity and spread during winter in the temperate regions (Tamerius et al., 2013). Therefore, a strong robust association was observed between environmental parameters (temperature and humidity) and influenza incidence in these regions (Lowen and Steel, 2014). Similarly, the activity and transmission efficacy of SARS-CoV-2 in people were also strongly influenced by meteorological factors such as temperature and humidity (Lin et al., 2020). In mainland China, the COVID-19 transmission was negatively associated with temperature and humidity (Qi et al., 2020). Accordingly, Wu et al. (2020c) observed an inverse relationship of COVID-19 daily infections and death rates with daily atmospheric temperature and humidity in 166 countries. However, in another very recent study, the transmission of this virus was negatively and exponentially linked with temperature (Lin et al., 2020). Similarly, Prata et al. (2020) observed a negative linear relationship between temperature and COVID-19 daily infections in Brazil when temperature ranged from 16.8 to 27.4 °C, with each 1 °C increase in temperature resulted in a −4.9% decrement in daily infections. However, this curve was flattened at a threshold temperature of 25.8 °C indicating no further decline in infection rate was observed above this temperature. Interestingly, Qi et al. (2020) showed a significant interaction among humidity, temperature, and COVID-19 daily infection rate in Hubei, China. They found that at a humidity range of 67–85.5%, an increase in 1 °C temperature resulted in a decrease of 36–57% daily infections. On the other hand, each 1% increase in relative humidity decreased the daily infections by 11–22% when temperature ranged between 5.0 and 8.2 °C. The maximum temperature during this study was 2.5–9.9 °C (Qi et al., 2020) and in the case of Prata et al. (2020) this was 16.8–27.4 °C. However, Prata et al. (2020) did not observe the influence of humidity and its interaction with temperature on the, spread, transmission and mortality caused by COVID-19. On the other hand, Ma et al. (2020) observed a negative relationship among daily COVID-19 deaths, diurnal temperature range and relative humidity in Wuhan, China. Therefore, the role of meteorological conditions on the spread, transmission, and mortality is still controversial. The studies published so far did not able to conclusively figure out whether temperature and humidity are the key factors regulating COVID-19 transmission and mortality (Pani et al., 2020). Other weather/meteorological conditions such as rainfall, wind speed, solar activity and radiation also influenced the COVID-19 spread rate (Ahmadi et al., 2020; Nasirpour et al., 2021). However, their influence on the number of daily cases is much less than temperature and humidity (Srivastava, 2021). For instance, Ahmadi et al. (2020) did not find a correlation between number of COVID-19 infections and rainfall however they observed higher number of cases in the area with lower solar radiation. Bashir et al. (2020) observed insignificant role of wind speed in the spread of COVID-19. The dew is also an important factor influencing the respiratory syncytial virus, influenza and other viruses activity (Price et al., 2019). However, its influence on COVID-19 has not been investigated in any study.
Air quality parameters are also important in influencing the COVID-19 spread rate and mortalities in COVID-patients. In a recent literature review, Srivastava (2021) concluded that low air quality (PM and gaseous pollutants) caused more COVID-19 infections and mortalities. The air pollutants (PM10, PM2.5 and NO2) significantly increased the number of COVID-19 infections. An increment in per interquartile range of PM2.5, PM10 and NO2 in air was responsible for 6, 7, and 19% increase in daily COVID infections in China (Zhang et al., 2021b). Travaglio et al. (2021) observed that increasing levels of PM and NO2 raised the number of COVID-19 cases in England. They ranked PM2.5 as the main contributor to COVID-19 infections and NO2 to COVID-19 mortality rate. They further found that an increment in 1 m3 long-term average PM2.5 in air was linked to a 12% increase in COVID-19 related infections. Moreover, in their study, 1 μg m−3 increase in NO and NO2 in air increased 1.5 and 2.5% COVID-19 related mortalities in England. In another study, an increase in air per interquartile NO2 (4.6 ppb) was associated with 16.2% COVID-19 moralities in USA (Liang et al., 2020). The SO2, NO2, O3 and CO in the air also influenced the number of infections and daily mortality cases in China (Zhu et al., 2020). It is observed that 10 μg m−3 increment in NO2 and O3 in the air resulted in 6.94 and 4.76% increase in daily number of COVID-19 infections in China. Moreover, a 1 μg m−3 increase of CO in the air resulted in a 15.11% increase in daily infection cases. However, 1 μg m−3 increment in air SO2 decreased the COVID-19 infections by 7.79% (Zhu et al., 2020). Therefore, the contradictory relationships of air quality (particulate matter and gaseous pollutants) and COVID-19 related mortalities and infections warrant further investigation on these relationships (Srivastava, 2021).
The influence of air pollution and meteorological factors on the number of COVID-19 cases and mortalities was also investigated in few recent studies (Bolaño-Ortiz et al., 2020; Hassan et al., 2021; Mehmood et al., 2021). Both climatic and air pollution parameters significantly influenced the number of COVID-19 cases in selected cities of Pakistan (Mehmood et al., 2021). In this study, PM2.5 was the most dominant factor influenced the COVID-19 cases especially in highly affected city i.e. Lahore, Pakistan. Bolaño-Ortiz et al. (2020) observed that air pollution parameters (PM10, PM2.5, and NO2) were positively associated with the daily number of COVID-19 infections in Latin America and the Caribbean region. However, in their study, only wind speed among the studied meteorological factors might be responsible for airborne transmission of COVID-19 among people from the observed correlations. In a recent study carried out in Dhaka, Bangladesh, it was observed that both air pollution (PM2.5, water vapor, CO, and O3) and meteorological factors (wind pressure, rainfall and wind speed) were significantly correlated with number of daily COVID-19 cases (Hassan et al., 2021). Therefore, in a literature review, Paraskevis et al. (2021) concluded that the effect of climate/meteorological factors and air pollution on COVID-19 infections is highly contradictory. Only in the urban environment, air pollution influenced COVID-19 transmission (Paraskevis et al., 2021). In another literature review, Srivastava (2021) concluded that high air pollution was linked to increased number of mortalities in COVID-19 patients. Such contradiction in observed relationships among air pollution and/or meteorological parameters and COVID-19 infections or deaths indicated that differences in local climatic and air pollution conditions and immunological variables may vary among regions and also play a role in determining these relationships (Paraskevis et al., 2021).
Despite of the above discussed efforts on the role of meteorological factors and air quality parameters on COVID-19 spread, transmission, and associated deaths, still, the data is insufficient and lacking from the arid region of the world, where maximum temperature (especially in Saudi Arabia during the summer) sometimes exceeded 50 °C and humidity 90% (Almazroui et al., 2014). However, the studies to date on such relations were in the temperature range of 2.5–27.4 °C and humidity between 37 and 85% (Prata et al., 2020; Qi et al., 2020). On the other hand, due to the desert nature, the severe dust storm might lead the air quality of the region to a hazardous level which could be prone to COVID-19 related deaths. According to WHO, the detailed and updated studies on the association of air quality and meteorological parameters with COVID-19 infections and deaths are necessary to mend current pandemic forecasting models in order to adopt better public health measures. Therefore, to better understand the COVID-19 spread and transmission in the people, meteorological and air quality factor dependency of COVID-19 is imperative to investigate at local, regional and global scale (Pani et al., 2020; Srivastava, 2021). Moreover, no such study is performed in the Gulf region, where meteorological conditions are much different from other regions in both summer and winter.
Most of the studies exploring the relationship of air quality and meteorological factors with the COVID-19 infections and deaths cases used normal daily data of these variables (Lin et al., 2020; Prata et al., 2020; Qi et al., 2020; Wu et al., 2020a, 2020c). However, the COVID-19 incubation period among different ages of the people varied between 8 and 17 days (Kong, 2020). Qin et al. (2020) observed that this incubation duration among the 90th percentile of the people was 14.28 days. Therefore, one cannot find better fit of the daily environmental variables data with the number of COVID-19 infected cases without taking into consideration of COVID-19 incubation period. Hence, in order to find better fit of the model, the exponentially weighted moving average (EWMA) of the environmental variable data of at least 14 days should be taken. However, upon best of our knowledge, no studies used EWMA of environmental or air quality variables data to figure out their relationship with number of COVID-19 infected cases.
Therefore, the objective of this study was to investigate the role of daily and EWMA meteorological factors (temperature, humidity, and dew) and air quality (PM10, CO, and SO2) variables on the COVID-19 spread, and daily mortalities in major cities of Saudi Arabia. These relationships are explored using generalized additive model where contribution of the main variables influencing COVID-19 daily cases and deaths were identified using Spearman correlation coefficients. Further Akaike information criteria score was used to select the most appropriate model with best set of variables.
2. Methods
2.1. Study area
We selected six cities of the Kingdom of Saudi Arabia with variable meteorological conditions. These included Abha, Buraydah, Dammam, Jeddah, Mecca, and Riyadh. Köppen-Geiger classified “BWk” subtype for the climate of Abha, which is close to arid tropical and subtropical desert climate with the average coolest temperature 13.3 °C in January and the mean warmest temperature 23.3 °C. January and September are the most and least humid months with maximum relative humidity reached to 70% and minimum to 30% in Abha. The other selected cities were located in the subtype “BWh” hot arid tropical and subtropical desert climate. In these cities, the temperature ranged −1.1 to 50 °C, during the year, with the minimum temperature observed in January and maximum in July. The average minimum temperature ranged from 9.6 to 23.3, and the maximum temperature varies from 30.1 to 36.1 C in these cities. The mean humidity of these cities ranged between 10 and 95%.
2.2. Data collection
The data on the number of COVID-19 daily infections and deaths in infected people was collected from the above mentioned main cities from the ministry of health, the kingdom of Saudi Arabia (https://covid19.moh.gov.sa). This data was collected from the detection of the first case in these cities till August 30, 2020 for the analysis. The weather conditions (daily temperature, relative humidity and dew point) and air quality factors (PM10, CO, and SO2) data of these cities during the aforesaid period was collected from The World Air Quality Index project website (https://aqicn.org/map/saudi-arabia/). The missing data in some variables was calculated using the mean imputation.
2.3. Statistical analysis of the data
The SAS (SAS Institute inclusive) analytical software provided more than one information criteria, including Akaike's information (AIC), Akaike's bias-corrected information (AICC), and Schwarz Bayesian information (BIC) to compare between different models. The software used all these criteria to select the most appropriate model with best set of variables. However, the AIC is most widely used in the literature when working with a generalized additive model. The following formulae are used to calculate the information criteria:
| (1) |
| (2) |
| (3) |
Where DF shows degrees of freedom, f indicates frequencies number used in the model, and denotes the log likelihood which is calculated in the model at converged estimates.
We performed descriptive analysis on the data of daily COVID-19 infections and deaths, with temperature and humidity as main variables and air quality factors (PM10, CO, and SO2) and dew point as confounding variables. This analysis includes numerical variables that were described by means, and their standard deviations. From the daily data of the meteorological and air quality variables, the exponentially weighted moving average (EWMA) for 14 days was calculated. The EWMA data for their relationship with COVID-19 infected cases and deaths from 1st March to August 31, 2020 was used for the analysis. The generalized additive models (GAM) were used to find the predictor-response relationships. The model consisted of the Poisson dependent variable (infected (count)/death (count)) and the continuous independent variables (not normally distributed). Therefore, we used a nonparametric analysis procedure for exploring the relationships. First, we tested the correlation between the variables. Since, all the variables did not follow the normal distribution; therefore, Spearman correlation was used because the data is nonparametric and does not depend on the assumption of normality.
The GAM was used to study the relationship among EWMA temperature, EWMA relative humidity, and dew and air quality parameter (PM10, CO, and SO2) as confounding variables and the number of COVID-19 cumulative infections and deaths (lgN) for fitting the equations and splines. Thin-plate regression splines were used as smoothing splines function (Wood, 2003) and restricted maximum likelihood was selected for estimating the smoothing parameter. The GAM can be used for determining the parametric and non-parametric regression and smoothing function of this relationship (Liu et al., 2020a), as well as exploring the linear and nonlinear air quality effects on the number of COVID-19 pneumonia infections (Prata et al., 2020; Zhu et al., 2020) and associated deaths. The model is described in equation (4) as follow:
| (4) |
Where is the number of confirmed infected/death cases. β1 (EWMA temp), β1 (EWMA Humidity) are the parametric part of the model. PM10, CO, dew and SO2 are confounding variables. is the intercept and denotes a spline function to elude overfitting (Liu et al., 2020a).
The Degrees of Freedom (DF) for spline function can be calculated based on Wood (2006).
This software procedure is based on two DF for spline functions:
-
1)
The non-integer or effective degrees of freedom (EDF) for the model fit
The EDF represents statistic summary of GAM and it reflects the degree of non-linearity of a curve. a) An EDF = 1 shows a linear relationship. b) EDF >1 and ≤ 2 depicts a medium non-linear relationship, and (c) an EDF >2 signifies a high non-linear relationship (Zuur et al., 2009).
-
2)
EDF for the test examines the presence of a contribution for each smoothing component
If W is the adjustment in weighted matrix at a given convergence and if is the roughness in the penalty matrix in selected smoothing parameters.
According to Wood (2006) degree of freedom matrix will be:
| (5) |
The model DF is given as
| (6) |
The model DF for the error can be calculated as
| (7) |
The DF for the spline term component is the trace of sub-matrix
| (8) |
Therefore, the smoothing component test DF for term is calculated as
| (9) |
3. Results
3.1. Pre-analysis
The Shapiro-Wilk test of selected variables was significant at 5% probability level. This showed that the data did not meet the basic requirement of normal distribution. Consequently, the data was log transformed as the link function (Guisan et al., 2002). According to the test, it is observed that most of the explanatory variables were significant (P˂0.01; Table 1 ) however, most of the correlation coefficient were ˂0.30 except exponentially weighted moving average (EWMA) temperature and humidity (Table 1). This indicates that correlations were low among the air quality variables and one of the studied meteorological factor (i.e., dew point). The largest values of R were observed between temperature and number of infected (R = 0.55) and deaths cases (R = 0.50), respectively (Table 1). The second largest R values were observed between humidity and number of infected (R = −0.40) and deaths cases (R = −0.38) indicating medium negative correlations. However, the R values were ˂0.1 for the correlation of air quality parameters and the COVID-19 infections or deaths. Therefore, meteorological factors (EWMA temperature and humidity) were selected as main variables and dew point and air quality parameters (PM10, CO, and SO2) were selected as confounding variables in the generalized additive model.
Table 1.
Spearman correlation coefficients (R) of the response and explanatory variables. ***Designates significant differences at P˂0.0001. **Specifies significant differences at P˂0.001. *Shows significant differences at P˂0.01 or P ≤ 0.05.
| Variable | Infected | Death | Temp | Humidity | PM10 | CO | dew | SO2 |
|---|---|---|---|---|---|---|---|---|
| Infected | 1 | |||||||
| Death | 0.225*** | 1 | ||||||
| Temp | 0.551*** | 0.501*** | 1 | |||||
| Humidity | −0.395*** | −0.377*** | −0.644*** | 1 | ||||
| PM10 | 0.038 | 0.232*** | 0.096** | −0.277*** | 1 | |||
| CO | 0.058* | −0.015 | 0.168*** | −0.232*** | 0.198*** | 1 | ||
| Dew | 0.040 | 0.046 | 0.106 *** | 0.456*** | −0.173*** | −0.114*** | 1 | |
| SO2 | 0.007 | −0.030 | −0.235*** | 0.239*** | 0.070* | −0.201*** | 0.077* | 1 |
3.2. Descriptive analysis
The descriptive statistics of the daily COVID-19 infected cases, the number of deaths, EWMA temperature, relative humidity, dew and air quality variables (PM10, CO, and SO2) data is summarized in Table 2 . The total number of observations of these variables were ∼1100 (1st March to August 31, 2020). The mean number of daily infected cases, deaths, EWMA temperature, relative humidity, dew, PM10, CO and SO2 were 131.7, 7.5, 28.7 °C, 36.7%, 10.7 g m−3, 26 μg m−3, 8.4 mg m−3, and 2.7 mg m−3 respectively in all selected cities of the kingdom during 1st March to August 31, 2020. The maximum daily number of infected people during this period were 2371 and the deaths were 41, whereas the minimum value of both of the aforesaid parameters was 0. The daily temperature and relative humidity ranged between 12 and 42 °C and 6–94%, respectively. The EWMA temperature ranged between 14 and 39 °C and humidity was 10.8–79.3% during this period (Table 2). The dew point was ranged between -8-28 g m−3. The air quality parameters such as PM10, CO, and SO2 were in the range of 1–290 μg m−3, 1–26, and 1–17 mg m−3, respectively during March to August 2020 (Table 2).
Table 2.
Descriptive statistics of COVID-19 infected cases, number of deaths and environmental (temperature, humidity, and dew) and air quality (PM10, CO, and SO2) parameters since the start of the outbreak in six cities of Saudi Arabia.
| Variable | N | Mean | Std Dev | Median | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Infected | 1104 | 131.74366 | 208.97744 | 56.00000 | 0 | 2371 |
| Death | 1104 | 7.50589 | 11.63360 | 1.00000 | 0 | 41.00000 |
| EWMA Temperature | 1104 | 28.74289 | 6.12128 | 29.14000 | 14.00000 | 39.00000 |
| EWMA Humidity | 1104 | 36.73019 | 15.47045 | 36.25000 | 10.79000 | 79.36000 |
| Dew | 1104 | 10.70053 | 6.56459 | 10.00000 | −8.00000 | 28.00000 |
| PM10 | 1103 | 25.99469 | 22.81056 | 20.50000 | 1.00000 | 290.00000 |
| CO | 1099 | 8.44538 | 4.11055 | 7.00000 | 1.00000 | 26.00000 |
| SO2 | 1103 | 2.66053 | 1.86333 | 2.00000 | 1.00000 | 17.00000 |
3.3. Model selection
Akaike information criterion (AIC) score indicated the better fitness of the selected model. Our results indicated that AIC score was the lowest (119565) for the number of daily COVID-19 infected cases when EWMA data of the environmental (main factors) and air quality parameters (confounding variables) were used in the generalized additive model (GAM; Table 3 ). On the other hand, the AIC score was the highest (155007) when original daily environmental variables data without confounding variables was used. In case of number of daily deaths, the same trend in AIC score was observed with the lowest score (12239) when EWMA environmental variables and air quality parameters as confounding variables were used in the model. Moreover, the highest AIC value (14996) was observed when model used only original environmental i.e., daily temperature, humidity and dew, and air quality variable data (Table 3).
Table 3.
Akaike information criterion (AIC: smaller AIC value indicates better fit) for comparing the different generalized additive models of original and exponentially weighted moving average (EWMA) data of environmental (temperature, humidity, and dew) and air quality variables (PM10, CO, and SO2) and number of COVID-19 infected cases and deaths.
| COVID-19 Infected cases |
|||||
|---|---|---|---|---|---|
| Original |
EWMA |
||||
| Criteria | Effective DF for test | No confounding | Confounding | No confounding | Confounding |
| AIC |
9.9 |
155007 |
152094 |
123817 |
119565 |
|
COVID-19 Deaths | |||||
| AIC | 13.9 | 14996 | 13547 | 13697 | 12239 |
3.4. Influence of environmental and air quality parameters on number of COVID-19 infected and death cases
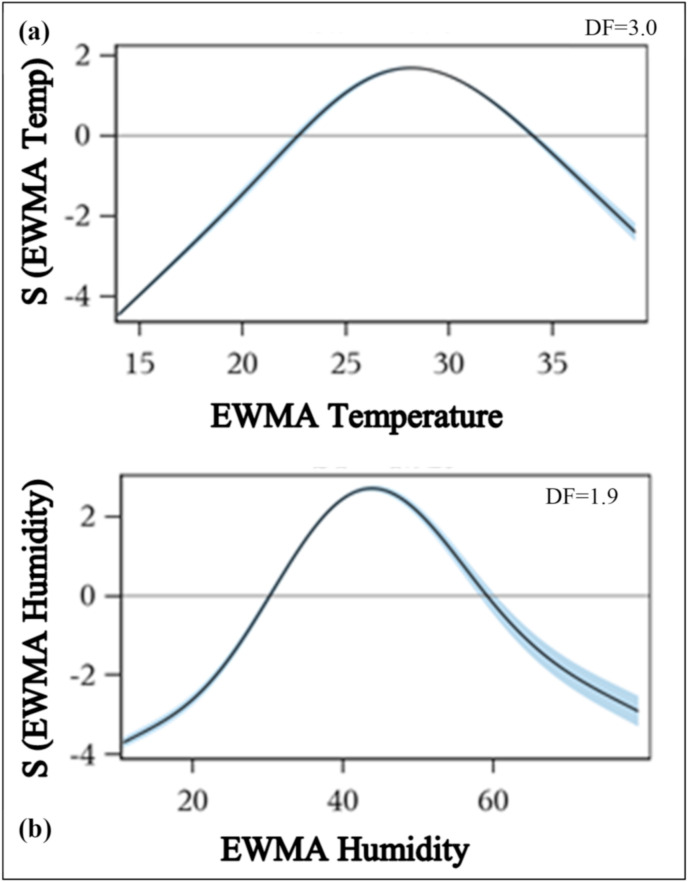
The predictor response-relationship using GAM model was established among the environmental and air quality parameters with the number of COVID-19 infected and death cases (Fig. 1, Fig. 2 ). This relation is the combination of linear and non-linear trends of GAM model. A bell shaped curvilinear relationship among number of COVID-19 infected cases and exponentially weighted moving average (EWMA) data of temperature and humidity was observed when accounting for air quality parameters of all the cities as confounding variables (Fig. 1). In case of number of COVID-19 infections, the linear part of the relationship was significant (P˂0.0001) for the main EWMA data of meteorological (temperature, humidity & dew) and air quality parameters (PM10, CO, and SO2) as confounding variables (Table 3). Fig. 1a shows the estimated smoothing spline function without the linear effect. The EWMA temperature appear to have the largest effect on the number of infection when it ranged from 23 to 34.5 °C, and the maximum increase in the number of infections was observed at 28.5 °C. In case of EWMA humidity and number of COVID-19 infected cases, Fig. 1b visualizes the estimated spline function for EWMA humidity. This relationship indicated that EWMA humidity had significant effect on number of infections when it varied from 30 to 60% with the highest effect on a humidity level of 45% (Fig. 1b). The linear part of the relationship showed that for each 1 °C rise in temperature there was 13% increase in the number of COVID-19 infections (P < 0.0001; Table 3). In contradiction to temperature, each 1% rise in air humidity, decreased the number of COVID-19 patients by 5% (Table 3).
Fig. 1.
The relationships of exponentially weighted moving average (EWMA) temperature (a) and EWMA humidity (b) with number of COVID-19 confirmed cases. The values on x-axis specify the average temperature compensation and y-axis shows the smoothing components for infected cases to the fitted values. The confidence bands of smoothing components was 95%.
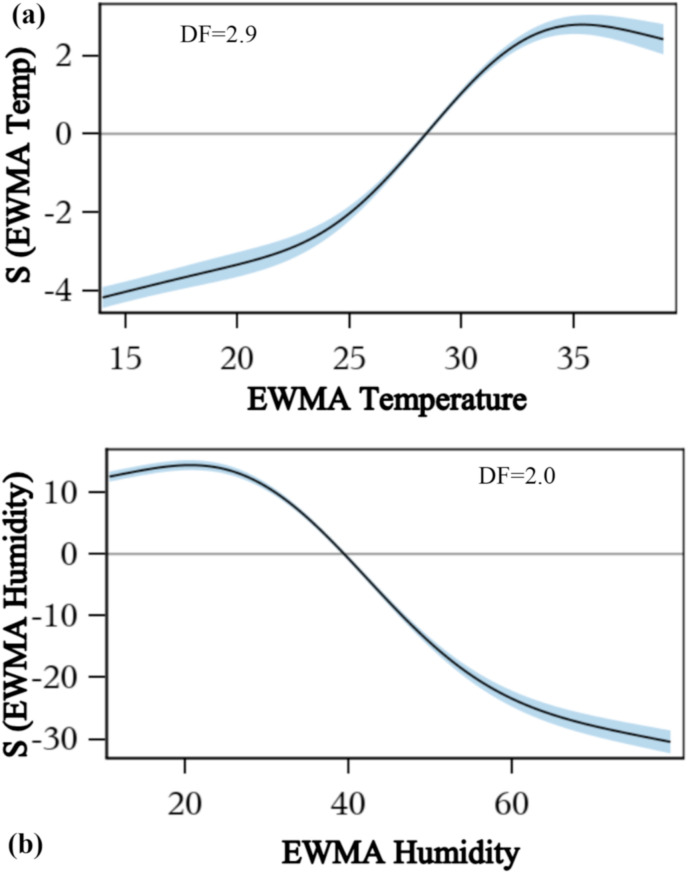
Fig. 2.
The relationships of exponentially weighted moving average (EWMA) temperature (a), EWMA humidity (b) with number of COVID-19 deaths. The values on x-axis specify the average temperature compensation and y-axis shows the smoothing components for number of deaths to the fitted values. The confidence bands of smoothing components was 95%.
The relationships of EWMA temperature and humidity with number of COVID-19 deaths were different than what were observed for number of infected cases. Fig. 2a shows the estimated smoothing spline function for the EWMA temperature which appeared to have the largest effect on the number of deaths when it crossed 28.7 °C with the highest influence when it reached to 35 °C. The linear relationship indicates that each 1 °C rise in EWMA temperature resulted 19.6% decrease in number of deaths (Table 4 ). In case of EWMA humidity, there is positive relationship between number of deaths and humidity where the linear relationship coefficient showed an increase in number of deaths by 33.7% with each 1% increase in humidity (Table 3). Fig. 2b shows the estimated spline function which indicated nonlinear relationship between EWMA humidity and death rate with the highest influence when the EWMA humidity below 40%.
Table 4.
Parameter estimates of linear part of the generalized additive model comparing the relationships among different environmental (temperature, humidity, and dew) and air quality variables (PM10, CO, and SO2) and number of COVID-19 infected cases and deaths.
| COVID-19 Infected cases | |||||
|---|---|---|---|---|---|
| Parameter | DF | Estimate | Std Error | Chi-Square | Pr > ChiSq |
| Intercept | 1 | 1.800386 | 0.366437 | 24.1398 | <.0001 |
| EWMA Temperature | 1 | 0.129529 | 0.011394 | 129.2402 | <.0001 |
| EWMA Humidity | 1 | −0.047913 | 0.003344 | 205.3080 | <.0001 |
| Dew | 1 | 0.003322 | 0.000584 | 32.3571 | <.0001 |
| PM10 | 1 | −0.001137 | 0.000125 | 82.9433 | <.0001 |
| CO | 1 | 0.022512 | 0.000762 | 872.2004 | <.0001 |
| SO2 |
1 |
0.083384 |
0.001344 |
3848.2284 |
<.0001 |
|
COVID-19 Deaths | |||||
| Intercept | 1 | −5.041431 | 0.857154 | 34.5931 | <.0001 |
| EWMA Temperature | 1 | −0.195671 | 0.016950 | 133.2640 | <.0001 |
| EWMA Humidity | 1 | 0.336855 | 0.018297 | 338.9497 | <.0001 |
| dew | 1 | 0.018721 | 0.002706 | 47.8697 | <.0001 |
| PM10 | 1 | 0.009594 | 0.000363 | 699.9910 | <.0001 |
| CO | 1 | −0.069266 | 0.003134 | 488.5453 | <.0001 |
| SO2 | 1 | −0.161722 | 0.009200 | 309.0070 | <.0001 |
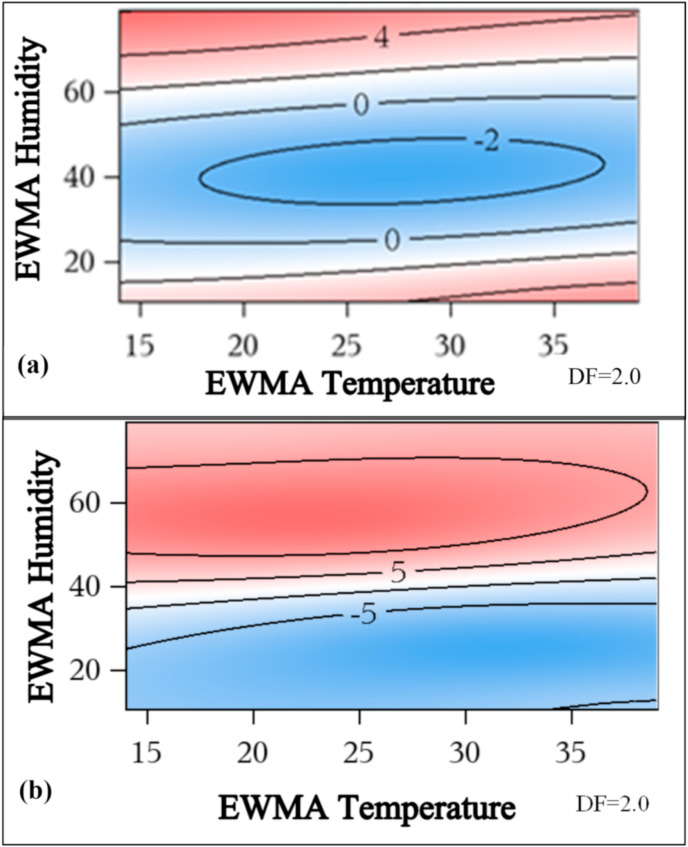
The interaction of EWMA temperature and humidity on the number of COVID-19 infections and death cases is a three-dimensional relationship presented in Fig. 3 . The plots indicate a significant nonlinear relationships between the number of infected or death cases with EWMA temperature and humidity. The relationship of Fig. 3a indicates that humidity above 64% at the temperature range of 15–35 °C and below 15% at temperature between 30–39 °C resulted in lower influence on the number of COVID-19 infections. Moreover, EWMA humidity between 25 and 42% at all temperatures resulted in higher number of infections (Fig. 3a). On the other hand, humidity below 30% resulted in higher nonlinear effects on the number of deaths at all temperatures under investigation and this parameter above 42% resulted in low effect on the number of deaths at all temperatures (Fig. 3b).
Fig. 3.
Three-dimensional relationships between exponentially weighted moving average (EWMA) temperature and EWMA humidity with number of COVID-19 infected cases (a) and deaths (b). The confidence bands of smoothing components was 95%.
The critical part of these relationships is the Tests for Smoothing Components (Table 5 ). For each smoothing effect in the model, there existed a contribution of each smoothing component i.e. EWMA temperature, humidity or their interaction (Table 5). The chi-square values in the table indicates that the three smoothing terms i.e., EWMA temperature, humidity and their interaction are highly significant (P < 0.0001). Moreover, all the splines (smoothing component) showed a significant contribution to the model (Table 3). The degrees of freedom values DF > 1 demonstrated the amount of nonlinearity of this relationship. This shows that there are higher-order relationships between the number of COVID-19 infected persons or deaths with EWMA temperature, humidity and their interaction (Table 5). From the Chi-Square values, it is apparent that EWMA temperature played a major role in the smoothing effect followed by EWMA humidity and their interaction for both number of infections and deaths caused by COVID-19 (Table 5).
Table 5.
Tests for smoothing components of major environmental variables (temperature, humidity and their interaction) effect on number of COVID-19 infected cases and deaths. The effective degrees of freedom (EDF) is a summary statistic of GAM and it reflects the degree of non-linearity of a curve. a) An EDF equal to 1 is equivalent to a linear relationship. b) EDF >1 and ≤ 2 is a medium non-linear relationship, and (c) an EDF >2 indicates a highly non-linear relationship. The EDF for test examines the existence of a contribution for each smoothing component.
| COVID-19 Infected cases | ||||
|---|---|---|---|---|
| Component | Effective DF | Effective DF for Test | Chi-Square | Pr > ChiSq |
| Spline (EWMA Temp) | 2.99841 | 3 | 25817.2395 | <.0001 |
| Spline (EWMA Humidity) | 1.92461 | 2 | 5868.3845 | <.0001 |
| Spline (EWMA Temp × EWMA Humidity) |
2.00000 |
2 |
3450.6865 |
<.0001 |
|
COVID-19 Deaths | ||||
| Spline (EWMA Temp) | 2.94716 | 3 | 1439.4696 | <.0001 |
| Spline (EWMA Humidity) | 2.00000 | 2 | 1349.6326 | <.0001 |
| Spline (EWMA Temp × EWMA Humidity) | 2 | 2 | 1298.1032 | <.0001 |
4. Discussion
Our strong motivation for this study was the discussion that geographical scope and differences in climatic (temperature and humidity) and air quality variables may play an important role in the spread of COVID-19 infections and the number of mortalities caused by this virus in different countries (Ali et al., 2021; Liang et al., 2020; Marquès et al., 2021; Prata et al., 2020; Qi et al., 2020; Sobral et al., 2020). To our best of the knowledge such studies are lacking in arid tropical and subtropical desert climate of gulf region where windstorm and deserted climate further deteriorated the air quality with higher dust containing PM2.5 and PM10 in the air (Elsayed et al., 2021; Khodeir et al., 2012). Therefore, to understand the role of environmental and air quality parameters in spreading or causing the mortalities in COVID-19 patients, we used a generalized additive model to study these relationships. In our study, we observed the curvilinear bell shaped relationship of temperature and humidity on the number of COVID-19 infected cases (Fig. 1). This indicated that temperature and humidity dependent influence on the number of infections is nonlinear.
Remarkably, we observed both positive and negative correlations of temperature with number of infections (Fig. 1a). The infections increased with increasing temperature between 23 and 34.5 °C and decreased with temperature between 14-23 and 34.5–39 °C. In line with our results, Prata et al. (2020) also observed nonlinear relationship of temperature and number of COVID-19 infections. However, in their study, the linear relationship was negative indicating that with rising temperature between 16.8 °C and 27.4 °C there was a decrease in number of infections by −5% and no effect on the number of infections was observed at temperature above 27.4 °C. Qi et al. (2020) found negative relation between temperature and number of infections however in their study, the max temperature was 10 °C. According to Iqbal et al. (2020), local weather condition played an important role in altering the transmission of virus. This observation is in line with many other reports on other contagious viruses such as influenza (Lowen and Steel, 2014), MERS (Altamimi and Ahmed, 2020), SARS (Chan et al., 2011) and Zika virus (Yang and Sarfaty, 2016). The transmission rate of influenza virus is much higher at lower temperature (Lowen and Steel, 2014), since cold temperature weaken the human immunity so enhanced the susceptibility of the host to virus infection (Kudo et al., 2019). Similarly, lower temperature and humidity most likely favored the COVID-19 transmission, therefore it was argued that pandemic may ease during the rising temperature in summer (Liu et al., 2020a). In line with this argument Prata et al. (2020) observed 5% decrease in number of COVID-19 infections with each 1 °C rise in temperature until 27.4 °C but after this temperature no effect on number of infections was observed. However, in our study, we observed nonlinear relationship indicating that we could not observe 1:1 relationship of temperature, humidity and number of COVID-19 infection or deaths cases (Fig. 1, Fig. 2, Fig. 3). This could be explained by the fact that temperature (14–39 °C) and humidity (10.8–79.3%) ranges in our study are much different than the above reported studies (Prata et al., 2020; Qi et al., 2020).
The relationship of meteorological factor i.e. temperature with COVID-19 transmission rate (Prata et al., 2020; Qi et al., 2020) is not only dependent on temperature but also on other meteorological (humidity, dew etc.) and outdoor air quality parameters i.e. PM2.5, PM10, NO2, CO and SO2 etc. (Kraemer et al., 2020; Liu et al., 2020a; Marquès et al., 2021; Pani et al., 2020; Sobral et al., 2020; Wu et al., 2020a; Zhu et al., 2020). For instance, other viruses such as MERS infection increased with high temperature and low humidity in the kingdom of Saudi Arabia (Altamimi and Ahmed, 2020). The humidity was negatively associated with number of COVID-19 infections in Iran (Ahmadi et al., 2020). Accordingly, Zhang et al. (2021a) investigated the role of climatic conditions on the number of COVID-19 infections in 1236 regions of the world and observed that both the temperature and humidity were negatively associated with COVID-19 transmissions in the people. In line with these findings, Wu et al. (2020c) observed the negative relationships of temperature and humidity with number of infections and death cases in 166 countries of the world. Biryukov et al. (2020) also observed in a laboratory study that increase in temperature and/or relative humidity decreased the half-life of the COVID-19 virus on two hard surfaces. They found that increase in temperature from 24 to 35 °C resulted in faster viral decay and shorter half-life at a relative humidity of 20, 40 and 60% on these surfaces (Biryukov et al., 2020). In contradiction to their study, we observed higher number of infections at this temperature range (Fig. 1a), however the humidity above 62% resulted in lower number of infections (Fig. 1b) at temperature range of 14–35 °C (Fig. 3a). The difference in our results with the above reported studies could be explained by air quality indicators and many other socioeconomic factors and mobility restriction of the people that influenced the spread of COVID-19 infections (Fang et al., 2020; Rahman et al., 2021; Zhu et al., 2020).
Air quality parameters might also influence COVID-19 infections. For instance, Zhu et al. (2020) observed positive relationships with PM2.5, PM10, CO, NO2 and O3 and negative relationship with SO2 and number of COVID-19 cases in China. Similarly, Rahman et al. (2021) also observed that both meteorological (i.e. temperature and humidity etc.) and air quality parameters had a very good coherence with number of COVID-19 infections in Dhaka city of Bangladesh. In line with their findings, we also observed the relationships of air quality and meteorological factors with number of COVID-19 infections (Table 1, Table 4). However, in our study the strong correlations were observed between the meteorological parameters i.e. EWMA temperature and humidity. Moreover, PM10 was negatively and CO, and SO2 were positively correlated with number of daily COVID-19 infections (Table 4). Hence, the results of our study highlighted the new research domain on the potential relationships of air quality parameter with number of COVID-19 daily cases. Therefore, as suggested by Rahman et al. (2021) and our study, it is essential to identify the importance of meteorological and air quality indicators to draw a line between imposing restriction policy and these factors for the reduction of daily COVID-19 infections. The Spearman correlations and GAM model depicted that EWMA temperature and humidity were the major variables linked with number of daily COVID-19 cases in selected six cities of the Saudi Arabia followed by air quality indicators (Table 1, Table 2, Table 4).
The relationships among the meteorological parameters, air quality indicators and number of deaths were in contradictory to the number of COVID-19 infections (Fig. 1, Fig. 2). We observed negative association between EWMA temperature and number of mortalities caused by COVID-19 until 28.7 °C and after this temperature, the relationship was positive indicated that increasing temperature above 28.7 resulted in higher number of deaths (Fig. 2a). On the other hand, despite of non-linear relationships, we observed positive relationship of number of COVID-19 deaths below 40% of the humidity and the relationship was negative above this humidity level. In line with us, Biktasheva (2020) observed that relative humidity was negatively correlated with number of COVID-19 mortalities in German federal states. Ma et al. (2020) observed a negative association of COVID-19 deaths with temperature and relative humidity. In line with these, many other studies found that mortality due to respiratory diseases increased with declining temperature (Ghalhari and Mayvaneh, 2016) and strongly linked with cold temperature (Dadbakhsh et al., 2017). In contradictory to these findings, Li et al. (2019) observed that extreme temperature (hot and cold) increased the mortality rate in respiratory patients in China. The explained that exposure to prolonged low temperature may cause congestion in airways and could lead to bronchoconstriction. Therefore, low temperature played a role in reducing ciliary activity. Such effects could lead to enhance the proneness of respiratory tract infections (Hayes et al., 2012). On the other hand, exposure to high temperature could trigger the inflammation that could influence the condition of the patients with existing respiratory disease (Bunker et al., 2016). Similar phenomena could have been occurred in COVID-19 associated deaths where meteorological conditions influenced the vulnerability of the patient to mortality (Ma et al., 2020).
Humidity is also an important parameter influenced the mortality of respiratory disease patient, lower humidity levels could potentially increase the mortality rate in influenza patients (Barreca, 2012). Inhalation of dry air could potentially damage the epithelial cells and/or reduce the clearance of mucociliary which enhanced the susceptibility of the host to respiratory viral infections (Lowen et al., 2007). In line with the aforementioned observations, Biktasheva (2020) hypothesized that dry air resulted in over-dried respiratory mucosa in the vulnerable patients and therefore increased the COVID-19 related deaths. Virus usually transmitted through droplet nuclei but under humid climate the exhaled droplet rapidly settled in the environment and it is less likely that such settled respiratory droplet could contribute to the viral (influenza) spread (Lowen et al., 2007). Therefore, as observed in previous studies (Biktasheva, 2020; Ma et al., 2020), in present study the COVID-19 mortalities may related to lower humidity (Fig. 1b).
The air pollution also significantly affecting the COVID-19 related mortalities in number of previous studies (Conticini et al., 2020; Liang et al., 2020; Wu et al., 2020a). Particulate matter, NO2, SO2 and O3 played a prominent role in inducement of systematic and respiratory inflammations (Kurai et al., 2018; Perret et al., 2017). Long term exposure to particulate matter (PM10, PM2.5) increased the cardiovascular and respiratory morbidity and mortality (Liu et al., 2019). This is in line with Wu et al. (2020b) who observed that an increase of PM2.5 concentration (1 mg m−3) in the air resulted in 8% increase in COVID-19 associated mortalities. Pozzer et al. (2020) observed that particulate air pollution 15% increased the number of COVID-19 mortalities worldwide. Similarly, an increase in per interquartile range of PM2.5, PM10 and NO2 in the air increased the daily COVID infections in China by 6, 7, and 19%, respectively (Zhang et al., 2021b). Travaglio et al. (2021) ranked PM2.5 as the main contributor to COVID-19 infections and NO2 to COVID-19 mortality rate. In their study, an increase of 1 μg m−3 of NO and NO2 in the air increased 1.5 and 2.5% COVID-19 related mortalities in England. However, in our study the most important factor influencing the COVID-19 infections/deaths were the meteorological factors (temperature and humidity), air pollution indicators also influenced this relationship but their contribution was much less (Table 1, Table 3).
There are number of limitations of the present study that could not be ignored. Government intervention in the form of lockdown, reduction in mobility of people may also affect the number of COVID-19 infections as well. Moreover, the availability of medical resources and trained staff can also affect the COVID-19 mortality and may influence their relationships with meteorological and air pollution indicators. However, the effect of government policies and measures on the transmission rate and deaths caused by COVID-19 were not investigated in this study. In this study, we investigated the longer duration (i.e. 6 months) than any study so far according to the best of our knowledge to explore the relationships among meteorological and air quality indicators with number of COVID-19 infection or death cases. The future studies can use yearly data and other factors such as population density, use of sanitizers and masks, intercity movement etc. in the analysis to give the clear picture on such relationships and give recommendation to avoid/slow down the current and future pandemics. In the same direction future studies can explore these relationships at country, or world level analysis to offer useful insights on the factors affecting the COVID-19 spread and deaths.
5. Conclusion
The Coronavirus (COVID-19) pandemic is still uncontrollable and rapidly spreading infections in human population around most of the countries globally. The rapid death caused by COVID-19 is still a major challenge for the scientist, policy makers and the researchers. Therefore, this is the first study to explore the relationship of meteorological parameters (i.e. temperature, relative humidity, and dew) and air quality indicators (PM10, CO, and SO2) on the daily COVID-19 infections and number of death cases using generalized additive model in the selected six cities of the Kingdom of Saudi Arabia. Our findings highlighted that meteorological and air quality indicators are important factors influencing the COVID-19 spread and deaths cases. This study unveils that temperature, relative humidity, dew, PM10, CO, and SO2 are significantly correlated with both number of infections and deaths caused by COVID-19 in Saudi Arabia. Among all studied factors, temperature and relative humidity are the main parameters influencing the COVID-19 infections and deaths. In contradictory to number of studies, we observed nonlinear relationships among temperature, relative humidity and COVID-19 infections and death cases. Remarkably, the temperature between 23 and 34.5 °C and relative humidity between 30 and 60% is positively associated with daily COVID-19 infections and below and/or above these ranges, a negative correlation was observed. This is indicating that number of COVID-19 cases decreased at temperature below 23 and above 34.5 °C and humidity below 30 and above 60%. The number of deaths were positively associated at temperature ˃28.7 °C and relative humidity ˂40% showing higher number of deaths above this temperature and below this humidity. Although air quality indicators were significantly correlated but their effects were much less than major meteorological parameters. Hence, the present study suggested that variation in temperature, relative humidity and air pollution indicators could be important factors influencing the COVID-19 spread and mortality. Consequently, it is important to take this into account especially at current scenario when the temperature and relative humidity are rising and again the number of infections is increasing in the kingdom, therefore, like before, it justifies an active government policy to lessen COVID-19 infection rate.
Credit author statement
Conceptualization: Iqbal M.I. Ismail, Muhammad Imtiaz Rashid, Methodology, Nadeem Ali, Bothinah Abdullah Saeed Altaf, Muhammad Imtiaz Rashid, Statistics: Bothinah Abdullah Saeed Altaf, Muhammad Imtiaz Rashid, Data curation, Muhammad Imtiaz Rashid, Nadeem Ali, Writing – original draft preparation. Muhammad Imtiaz Rashid Reviewing and Editing, Iqbal M.I. Ismail, Muhammad Imtiaz Rashid, Nadeem Ali, Bothinah Abdullah Saeed Altaf, Muhammad Munir.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, Sauid Arabia under grant no. GCV19-17-1441. The authors therefore, acknowledge with thanks to DSR for technical and financial support.
References
- Ahmadi M., et al. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M., et al. Presentation of a developed sub-epidemic model for estimation of the COVID-19 pandemic and assessment of travel-related risks in Iran. Environ. Sci. Pollut. Control Ser. 2021;28:14521–14529. doi: 10.1007/s11356-020-11644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleta A., et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nature Human Behaviour. 2020;4:964–971. doi: 10.1038/s41562-020-0931-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S.M., et al. Exploring the linkage between PM2.5 levels and COVID-19 spread and its implications for socio-economic circles. Environ. Res. 2021;193:110421. doi: 10.1016/j.envres.2020.110421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almazroui M., et al. Trends of temperature extremes in Saudi Arabia. Int. J. Climatol. 2014;34:808–826. [Google Scholar]
- Altamimi A., Ahmed A.E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. Journal of Infection and Public Health. 2020;13:704–708. doi: 10.1016/j.jiph.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreca A.I. Climate change, humidity, and mortality in the United States. J. Environ. Econ. Manag. 2012;63:19–34. doi: 10.1016/j.jeem.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., et al. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biktasheva I.V. Role of a habitat's air humidity in Covid-19 mortality. Sci. Total Environ. 2020:138763. doi: 10.1016/j.scitotenv.2020.138763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biryukov J., et al. Increasing temperature and relative humidity accelerates inactivation of SARS-CoV-2 on surfaces. mSphere. 2020;5 doi: 10.1128/mSphere.00441-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolaño-Ortiz T.R., et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: a look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020;191:109938. doi: 10.1016/j.envres.2020.109938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunker A., et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.M., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011(734690):1–7. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., et al. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadbakhsh M., et al. Death from respiratory diseases and temperature in Shiraz, Iran (2006–2011) Int. J. Biometeorol. 2017;61:239–246. doi: 10.1007/s00484-016-1206-z. [DOI] [PubMed] [Google Scholar]
- Elsayed Y., et al. Meteorological patterns, technical validation, and chemical comparison of atmospheric dust depositions and bulk sand in the Arabian Gulf region. Environ. Pollut. 2021;269:116190. doi: 10.1016/j.envpol.2020.116190. [DOI] [PubMed] [Google Scholar]
- Fang H., Wang L., Yang Y. Human mobility restrictions and the spread of the Novel Coronavirus (2019-nCoV) in China. J. Publ. Econ. 2020;191:104272. doi: 10.1016/j.jpubeco.2020.104272. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghalhari G.F., Mayvaneh F. Effect of air temperature and universal thermal climate index on respiratory diseases mortality in Mashhad, Iran. Arch. Iran. Med. 2016;19 0-0. [PubMed] [Google Scholar]
- Guisan A., et al. Generalized linear and generalized additive models in studies of species distributions: setting the scene. Ecol. Model. 2002;157:89–100. [Google Scholar]
- Hassan M.S., et al. Relationship between COVID-19 infection rates and air pollution, geo-meteorological, and social parameters. Environ. Monit. Assess. 2021;193:29. doi: 10.1007/s10661-020-08810-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes D., Jr., et al. Bronchoconstriction triggered by breathing hot humid air in patients with asthma: role of cholinergic reflex. Am. J. Respir. Crit. Care Med. 2012;185:1190–1196. doi: 10.1164/rccm.201201-0088OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal M.M., et al. The effects of regional climatic condition on the spread of COVID-19 at global scale. Sci. Total Environ. 2020;739:140101. doi: 10.1016/j.scitotenv.2020.140101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khodeir M., et al. Source apportionment and elemental composition of PM2.5 and PM10 in Jeddah city, Saudi Arabia. Atmospheric Pollution Research. 2012;3:331–340. doi: 10.5094/apr.2012.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong T.-k. Longer incubation period of coronavirus disease 2019 (COVID-19) in older adults. AGING MEDICINE. 2020;3:102–109. doi: 10.1002/agm2.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U., et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo E., et al. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc. Natl. Acad. Sci. Unit. States Am. 2019;116:10905–10910. doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurai J., et al. Ozone augments interleukin-8 production induced by ambient particulate matter. Gene Environ. 2018;40:1–8. doi: 10.1186/s41021-018-0102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M., et al. Temperature, temperature extremes, and cause-specific respiratory mortality in China: a multi-city time series analysis. Air Quality, Atmosphere & Health. 2019;12:539–548. [Google Scholar]
- Liang D., et al. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. Innovation. 2020;1:100047. doi: 10.1016/j.xinn.2020.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C., et al. A mechanism-based parameterisation scheme to investigate the association between transmission rate of COVID-19 and meteorological factors on plains in China. Sci. Total Environ. 2020;737:140348. doi: 10.1016/j.scitotenv.2020.140348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., et al. Ambient particulate air pollution and daily mortality in 652 cities. N. Engl. J. Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Lowen A.C., et al. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:e151. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., et al. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquès M., et al. Effects of air pollution on the potential transmission and mortality of COVID-19: a preliminary case-study in Tarragona Province (Catalonia, Spain) Environ. Res. 2021;192:110315. doi: 10.1016/j.envres.2020.110315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez M.E. The calendar of epidemics: seasonal cycles of infectious diseases. PLoS Pathog. 2018;14 doi: 10.1371/journal.ppat.1007327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmood K., et al. Spatiotemporal variability of COVID-19 pandemic in relation to air pollution, climate and socioeconomic factors in Pakistan. Chemosphere. 2021;271:129584. doi: 10.1016/j.chemosphere.2021.129584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasirpour M.H., Sharifi A., Ahmadi M., Ghoushchi S.J. Revealing the relationship between solar activity and COVID-19 and forecasting of possible future viruses using multi-step autoregression (MSAR) Environ. Sci. Pollut. Res. Int. 2021;28:38074–38084. doi: 10.1007/s11356-021-13249-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani S.K., Lin N.H., RavindraBabu S. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020;740:140112. doi: 10.1016/j.scitotenv.2020.140112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paraskevis D., et al. A review of the impact of weather and climate variables to COVID-19: in the absence of public health measures high temperatures cannot probably mitigate outbreaks. Sci. Total Environ. 2021;768:144578. doi: 10.1016/j.scitotenv.2020.144578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perret J.L., et al. The dose–response association between nitrogen dioxide exposure and serum interleukin-6 concentrations. Int. J. Mol. Sci. 2017;18:1015. doi: 10.3390/ijms18051015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pozzer A., et al. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc. Res. 2020;116:2247–2253. doi: 10.1093/cvr/cvaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., et al. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price R.H.M., et al. Association between viral seasonality and meteorological factors. Sci. Rep. 2019;9:929. doi: 10.1038/s41598-018-37481-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J., et al. Estimation of incubation period distribution of COVID-19 using disease onset forward time: a novel cross-sectional and forward follow-up study. Science Advances. 2020;6 doi: 10.1126/sciadv.abc1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M.S., et al. How air quality and COVID-19 transmission change under different lockdown scenarios? A case from Dhaka city, Bangladesh. Sci. Total Environ. 2021;762:143161. doi: 10.1016/j.scitotenv.2020.143161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salim N., Raza A. Nutrient use efficiency (NUE) for sustainable wheat production: a review. J. Plant Nutr. 2020;43:297–315. [Google Scholar]
- Setti L., et al. SARS-Cov-2RNA found on particulate matter of bergamo in northern Italy: first evidence. Environ. Res. 2020:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobral M.F.F., et al. Association between climate variables and global transmission oF SARS-CoV-2. Sci. Total Environ. 2020;729:138997. doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava A. COVID-19 and air pollution and meteorology-an intricate relationship: a review. Chemosphere. 2021;263:128297. doi: 10.1016/j.chemosphere.2020.128297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamerius J.D., et al. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9 doi: 10.1371/journal.ppat.1003194. e1003194-e1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M., et al. Links between air pollution and COVID-19 in England. Environ. Pollut. 2021;268:115859. doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . vol. 2020. 2020. (Naming the Coronavirus Disease (COVID-19) and the Virus that Causes it). [Google Scholar]
- Wood S.N. Thin plate regression splines. J. Roy. Stat. Soc. B. 2003;65:95–114. [Google Scholar]
- Wood S.N. Chapman & Hall/CRC; Boca Raton, FL, USA: 2006. Generalized Additive Models. [Google Scholar]
- Worldometers . vol. 2020. 2021. (COVID-19 Coronavirus Pandemic). [Google Scholar]
- Wu X., et al. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Science advances. 2020;6 doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., et al. MedRxiv; 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S., Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395:1321–1322. doi: 10.1016/S0140-6736(20)30845-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y.T., Sarfaty M. Zika virus: a call to action for physicians in the era of climate change. Preventive Medicine Reports. 2016;4:444–446. doi: 10.1016/j.pmedr.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., et al. The role of weather conditions in COVID-19 transmission: a study of a global panel of 1236 regions. J. Clean. Prod. 2021;292:125987. doi: 10.1016/j.jclepro.2021.125987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., et al. Associations between air pollution and COVID-19 epidemic during quarantine period in China. Environ. Pollut. 2021;268:115897. doi: 10.1016/j.envpol.2020.115897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., et al. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuur A., et al. Springer Science & Business Media; 2009. Mixed Effects Models and Extensions in Ecology with R. [Google Scholar]