Abstract
Study objectives
COVID-19 brought unique challenges; however, it remains unclear what effect the pandemic had on violence in healthcare. The objective of this study was to identify the impact of the pandemic on workplace violence at an academic emergency department (ED).
Methods
This mixed-methods study involved a prospective descriptive survey study and electronic medical record review. Within our hospital referral region (HRR), the first COVID-19 case was documented on 3/11/2020 and cases peaked in mid-November 2020. We compared the monthly HRR COVID-19 case rate per 100,000 people to the rate of violent incidents per 1000 ED visits. Multidisciplinary ED staff were surveyed both pre/early-pandemic (April 2020) and mid/late-pandemic (December 2020) regarding workplace violence experienced over the prior 6-months. The study was deemed exempt by the Mayo Clinic Institutional Review Board.
Results
There was a positive association between the monthly HRR COVID-19 case rate and rate of violent ED incidents (r = 0.24). Violent incidents increased overall during the pandemic (2.53 incidents per 1000 visits) compared to the 3 months prior (1.13 incidents per 1000 visits, p < .001), as well as compared to the previous year (1.24 incidents per 1000 patient visits, p < .001). Survey respondents indicated a higher incidence of assault during the pandemic, compared to before (p = .019).
Discussion
Incidents of workplace violence at our ED increased during the pandemic and there was a positive association of these incidents with the COVID-19 case rate. Our findings indicate health systems should prioritize employee safety during future pandemics.
Keywords: Workplace violence, COVID-19, Pandemic, Staff safety
Abbreviations: CTA, Care Team Assistant(s); ECG, electrocardiogram; ED, Emergency Department; EMR, electronic medical record; EMT, emergency medical technician; HRR, Hospital referral region; PCA, Patient Care Assistant(s)
1. Introduction
Violence in the emergency department (ED) is a common and longstanding threat to staff [1,2]. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic with coronavirus disease 2019 (COVID-19) resulted in unprecedented isolation and stress to individuals and brought unique challenges to healthcare institutions and employees. The impact of the pandemic on mental health and home life has been previously documented [[3], [4], [5], [6]]; however, it remains unclear what effect the pandemic had on violence in healthcare. The objective of this study was to identify the impact of the pandemic on workplace violence at our academic emergency department in the Midwestern United States.
2. Methods
2.1. Study design and setting
This mixed-methods study involved a prospective descriptive survey study and electronic medical record (EMR) review. The study took place within the ED of a large, academic, Level 1 trauma center in a small urban city in the Midwest. The ED has 24/7 security presence available and had an average patient volume of 78,000 annually prior to COVID-19, with 65,500 patients seen in 2020. The hospital referral region (HRR) refers to the catchment area of patients referred to our institution. Within our HRR, the first COVID-19 case was documented on 3/11/2020 (n = 1) and the peak of documented cases occurred in mid-November 2020 with an average of 109.9 new positive COVID-19 cases per day (range: 0–498). The average monthly HRR COVID-19 case rate per 100,000 people was obtained from 3/11/2020 through 12/31/2020. Monthly incidents of ED violence were obtained from the institution's Office of Security from January 2019 to December 2020 and included both physical assault and verbal threats where security officers were notified to respond. These incidents were combined with monthly reports of violent events from the electronic medical record during the same time period. Overlapping data from both sources were counted only once. Monthly ED patient volume was obtained to calculate a rate of violent incidents per 1000 ED visits.
2.2. Survey study
We compared anonymous responses from a prior survey that was sent to all multidisciplinary ED staff pre/early-pandemic (April 2020) as previously described in McGuire et al. [7] to responses received from a similar second survey mid/late-pandemic (December 2020). Both questionnaires surveyed respondents regarding the incidence of verbal abuse and physical assault experienced over the prior 6-months (November 2019–April 2020 and July 2020–December 2020) and perception of safety in the workplace.
2.3. Selection of participants for surveys
The survey study target population consisted of all multidisciplinary staff that work within the ED, including non-ED staff assigned to other departments that perform services for ED patients. This population included clinicians [attending and resident physicians and advanced practice providers (APPs)], nursing staff [nurses and Patient Care Assistants (PCA)], Care Team Assistants (CTA) who provide clerical support and limited patient interaction, ancillary testing services [electrocardiogram (ECG) and radiology technicians and phlebotomists], registration/finance staff, and security officers. After Institutional Review Board review, the survey (described below and previously in McGuire et al. [7]) was distributed broadly by department and job type to anyone who might work in the ED even occasionally, via email distribution lists for the abovementioned target population with a cover letter describing the study purpose, directions for participation, and information regarding informed consent. In total, the survey was sent electronically to approximately 960 staff members. The questionnaire included a statement of informed consent at the beginning and completion indicated participant consent for inclusion in the study. Three reminder notices were sent through the same method prior to the close of the survey. The Institutional Review Board reviewed this study and materials and deemed it exempt from approval requirement.
2.4. Survey measurements
The initial pre/early-pandemic survey was developed in REDCap and the mid/late-pandemic survey was developed in Qualtrics. Both surveys were anonymous and included single-choice, multiple-choice and Likert-scale response questions. Participants were asked to indicate whether they had experienced any of the following forms of verbal abuse in the prior 6 months while working in the ED: threatening tone of voice; abusive language/statement; harassment (eg, racial, gender, sexual); or personal verbal threats (eg, threat of physical or sexual violence, threat of physical assault to occur outside the workplace). Participants were asked to indicate whether they had experienced any of the following forms of physical assault in the prior six months while working in the ED: physical assault with weapons (including hospital equipment); physical assault with bodily fluids (eg, saliva, urine, feces, wound exudate, blood, or spit); or physical assault in the form of punching, biting, rough handling, scratching, kicking, shoving/pushing, or hitting. Likert scales were used to measure participants' perception of safety and estimated frequency of verbal abuse. Standard demographic measures were collected.
2.5. Outcomes
The primary outcome was the correlation between the monthly HRR COVID-19 case rate per 100,000 people with the monthly rate of ED violent incidents per 1000 ED visits. The secondary outcome was the incidence of verbal abuse and physical assault experienced by multidisciplinary ED staff in a six-month time period, pre/early-pandemic versus mid/late-pandemic, as indicated by survey responses.
2.6. Data analysis
Survey responses were summarized with frequency counts and percentages. Subgroup comparisons of survey responses were performed using Chi-squared tests. For questions with multiple choice responses, if only one choice is allowed then a global Chi-squared test was performed. Alternatively, if multiple options are allowed within a single question, subgroups were compared for each option using pairwise Chi-squared tests. The Pearson Correlation Coefficient was calculated to determine association between the incidence of violence per 1000 patients in ED volume compared to average monthly HRR rate. P-values less than 0.05 were considered significant. Analysis was performed using R version 3.6.2.
3. Results
3.1. Survey study
A total of 480 responses were included for the survey study comparison- 259 responses from the pre/early-pandemic survey and 221 responses from the mid/late-pandemic survey, for an estimated survey response rate of 27.0% and 23.0%, respectively. A summary of respondent demographics is given in Table 1 .
Table 1.
Survey respondent demographics
| Pre/Early-COVID (N = 259) |
Mid/Late-COVID (N = 221) |
|
|---|---|---|
| Gender Male Female Transgender Prefer Not to Answer |
102 (39.4%) 154 (59.5%) 0 (0%) 3 (1.2%) |
72 (32.6%) 141 (63.8%) 1 (0.4%) 7 (3.2%) |
| Worked in ED for 6 Months Yes |
242 (93.4%) |
200 (90.5%) |
| Primary Role in ED Clinician Nursing Staff Testing Services Unit Secretary Registration/Finance Security |
50 (19.3%) 108 (41.7%) 55 (21.2%) 0 (0%) 4 (1.5%) 42 (16.2%) |
49 (22.2%) 99 (44.8%) 38 (17.2%) 10 (4.5%) 4 (1.8%) 21 (9.5%) |
| Primary Shift Day Evening Night Rotating |
70 (27.0%) 44 (17.0%) 52 (20.1%) 93 (35.9%) |
61 (27.6%) 24 (10.9%) 39 (17.6%) 97 (43.9%) |
| Years of Experience 0–4 Years 5–10 Years 11–20 Years ≥21 Years |
85 (32.8%) 57 (22.0%) 74 (28.6%) 43 (16.6%) |
70 (31.7%) 62 (28.1%) 49 (22.2%) 40 (18.1%) |
Overall, 208 (80.3%) of respondents indicated they had been verbally abused in the preceding six months pre/early-pandemic, compared to 188 (85.1%) mid/late-pandemic (Table 2 ). Although there was no significant difference in the overall incidence of verbal abuse experienced by staff during the pandemic, the frequency of verbal abuse did increase, with 6.2% of respondents pre/early-pandemic indicating verbal abuse by patients or their visitors every day or two, compared to 12.7% mid/late-pandemic (p = .017).
Table 2.
Violence in the ED by survey period.
| Pre/Early-COVID (N = 259) |
Mid/Late-COVID (N = 221) |
P-Value | |
|---|---|---|---|
| How safe do you feel in the ED? Extremely safe Very safe Moderately safe Slightly safe Not safe at all |
30 (11.6%) 128 (49.4%) 90 (34.7%) 11 (4.2%) 0 (0%) |
22 (10.0%) 96 (43.4%) 85 (38.5%) 16 (7.2%) 2 (0.9%) |
0.214 |
| In the last 6 months, have you experienced… | |||
| Any Verbal Abuse | 208 (80.3%) | 188 (85.1%) | 0.212 |
| Threatening Tone of Voice Abusive Language Harassment Threats of Violence |
202 (78.0%) 201 (77.6%) 102 (39.4%) 98 (37.8%) |
184 (83.3%) 179 (81.0%) 100 (45.2%) 95 (43.0%) |
0.1820 .4250 .2280 .292 |
| Any Physical Assault | 90 (34.7%) | 101 (45.7%) | 0.019 |
| Assault with Weapons Assault with Bodily Fluids Physical Attack (Punching, Biting, Scratching) |
8 (3.1%) 44 (17.0%) 81 (31.3%) |
6 (2.7%) 58 (26.2%) 88 (39.8%) |
>0.990 .0180 .063 |
| How often were you verbally abused by patients or visitors in the past 6 months? | 0.017 | ||
| Less Than Once a Month Every Month Every Week Every Day or Two |
116 (44.8%) 81 (31.3%) 46 (17.8%) 16 (6.2%) |
87 (39.4%) 54 (24.4%) 52 (23.5%) 28 (12.7%) |
|
| How often have you reported incidents of violence in the past 6 months? | 0.144 | ||
| Always Often Sometimes Rarely Never Not Applicable/Did Not Respond |
19 (7.3%) 13 (5.0%) 17 (6.6%) 32 (12.4%) 159 (61.4%) 19 (7.3%) |
11 (5.0%) 15 (6.8%) 20 (9.0%) 44 (19.9%) 127 (57.5%) 4 (1.8%) |
|
More respondents indicated experiencing physical assault within a six-month period mid/late-pandemic (n = 101; 45.7%), compared to 90 (34.7%) respondents pre/early-pandemic (p = .019). Staff indicated an increase in assault with bodily fluids during mid/late-pandemic (26.2%), compared to pre/early-pandemic (17.0%; p = .018). Nursing staff (p = .004) and security officers (p = .037) experienced higher rates of assault with bodily fluids during the pandemic compared to other job specialties (Table 3 ). Survey respondents indicated no significant difference in the reporting of violent incidents during the pandemic. The reported level of safety perceived by staff remained the same during the pandemic.
Table 3.
Comparison of Verbal abuse and physical assault by respondent position.
| Clinician | Nursing Staff | Security | Testing Services | |
|---|---|---|---|---|
| Total Responses Pre/Early-COVID Mid/Late-COVID |
50 49 |
108 99 |
42 21 |
55 38 |
| Threatening Tone Pre/Early-COVID Mid/Late-COVID P-Value |
42 (84.0%) 41 (83.7%) > 0.99 |
94 (87.0%) 91 (91.9%)0 .361 |
40 (95.2%) 20 (95.2%) > 0.99 |
24 (43.6%) 24 (63.2%)0 .101 |
| Abusive Language Pre/Early-COVID Mid/Late-COVID P-Value |
38 (76.0%) 40 (81.6%)0 .660 |
93 (86.1%) 91 (91.9%)0 .268 |
40 (95.2%) 20 (95.2%) > 0.99 |
29 (52.7%) 21 (55.3%)0 .976 |
| Harassment Pre/Early-COVID Mid/Late-COVID P-Value |
19 (38.0%) 13 (26.5%)0 .315 |
46 (42.6%) 43 (43.4%) > 0.99 |
28 (66.6%) 16 (76.2%)0 .628 |
9 (16.4%) 13 (34.2%)0 .081 |
| Threats of Violence Pre/Early-COVID Mid/Late-COVID P-Value |
17 (34.0%) 15 (30.6%)0 .884 |
51 (47.2%) 55 (55.6%)0 .290 |
27 (64.3%) 18 (85.7%)0 .139 |
3 (5.5%) 5 (13.2%)0 .265 |
| Assault – Weapons Pre/Early-COVID Mid/Late-COVID P-Value |
1 (2.0%) 0 (0%) > 0.99 |
5 (4.6%) 4 (4.0% > 0.99 |
2 (4.8%) 2 (9.5%)0 .595 |
0 (0%) 0 (0%) > 0.99 |
| Assault – Fluids Pre/Early-COVID Mid/Late-COVID P-Value |
8 (16.0%) 9 (18.4%)0 .964 |
15 (13.9%) 31 (31.3%)0 .004 |
18 (42.9%) 15 (71.4%)0 .037 |
3 (5.5%) 3 (7.9%)0 .686 |
| Assault – Attack Pre/Early-COVID Mid/Late-COVID P-Value |
8 (16.0%) 11 (22.4%)0 .576 |
39 (36.1%) 48 (48.5%)0 .097 |
28 (66.6%) 19 (90.5%)0 .064 |
6 (10.9%) 10 (26.3%)0 .091 |
3.2. EMR review
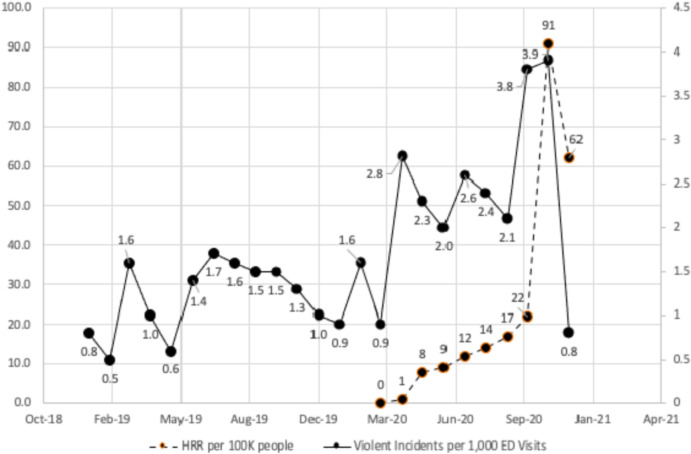
There was a positive association between the monthly HRR COVID-19 case rate and rate of violent ED incidents (r = 0.24; Fig. 1 ). There was an increase in overall violent workplace incidents during the pandemic (2.53 incidents per 1000 patient visits) compared to the 3 months prior (1.13 incidents per 1000 patient visits, p < .001), as well as compared to the previous year (1.24 incidents per 1000 patient visits, p < .001).
Fig. 1.
Data from EMR: Incidence of violence per 1000 patients ED volume compared to average monthly HRR COVID-19 case rate (r = 0.24) and overall, in the months leading up to the pandemic.
4. Discussion
Despite healthcare workers being hailed as heroes during the pandemic [[8], [9], [10]], we found a positive association between the local COVID-19 case rate and the rate of patient violence incidents in our ED through EMR review. We also found an increase in violent incidents in our ED overall during the pandemic, compared to before. These findings mirror prior data that has demonstrated an increase in interpersonal violence and child abuse during COVID-19 [3,6,11]. Proposed factors for this increase in home violence have included significant fear; stress; financial or food insecurity; and exposure to media hype, as well as worsening substance abuse and mental health during the pandemic [4,5]. These factors are all likely contributory to the increased incidence of violence seen within the healthcare workplace as well.
Similar to trends across the nation, our ED experienced a decrease in patient volume during the pandemic of approximately 12,500 patient visits from the year prior [12]. This decreased patient volume, coupled with our finding of an increased incidence of violence, would lead us to believe that workplace violence was felt to be a significant stressor to our ED staff during the pandemic; however, staff perception of workplace safety remained unchanged between the pre/early-pandemic and mid/late-pandemic periods. This may be attributable to staff prioritizing other personal safety concerns throughout the pandemic, or it may be due, in part, to staff empathizing with their perpetrator during an unprecedented period of significant stress, changes in day-to-day life, and uncertainty for everyone.
Our survey respondents indicated an increase in incidents of physical assault; specifically, assault with bodily fluids. This may be explained by generalized perception during the pandemic that spitting and coughing directly on others served to cause them significant harm [13]. Violent patients may have used this method of assault to their advantage and ED staff may have perceived this behavior to be more threatening during COVID-19. We found no significant difference in survey respondents' workplace violence reporting behaviors during the pandemic; however, due to protection of employee anonymity, this was not corroborated with actual employee incident reports.
This study has several important limitations. To preserve anonymity of employees, the surveys were sent to email distribution lists (DL) and included some DLs with employees working in other departments other than the ED (eg, phlebotomy, and ECG and radiology technicians), or who also worked at additional sites elsewhere in our health system (eg, clinicians). Thus, it is not possible to know the actual number of employees from different disciplines who work in the ED to obtain an exact response rate for our survey. Our estimated response rate of 23–27% may represent an unintended selection bias with individuals who have experienced workplace violence being more likely to respond regarding their experience. Additionally, to further preserve anonymity, we did not ask in-depth demographic questions. Without knowing full-time vs part-time status of respondents, it is possible that some responses came from employees working part time and this may have skewed our incidence of violence. The definition of “verbal abuse” is highly subjective to individual respondents and survey inclusion of “threatening tone of voice’” may have contributed to over-reporting of verbal abuse in general by respondents. The study was also subject to recall and reporting bias in terms of violence experienced over a six-month time period, as well as the reporting of incidents. Recall bias may have been even more significant during the pandemic. Likewise, reporting bias is possible if staff were more likely to report during the pandemic or during periods of increased COVID-19 patient volume than they were prior to the pandemic. We acknowledge that because this was a single-center study some aspects may not be generalizable to all institutions or geographic regions. However, the finding of an increased incidence of workplace violence during the COVID-19 pandemic is important and not likely related to local factors.
Our findings indicate that health systems should additionally prioritize employee safety during future pandemics.
Declarations of interest
None.
Meetings
An abstract with limited data from this study has been accepted for presentation at the ACEP 2021 Virtual Research Forum- Special Edition: COVID.
Financial support
No financial support was received for this research.
Conflict of interest disclosure
All authors report no conflicts of interest.
Credit author statement
S.M. conceived the study concept. All authors collected the data. S.M. and A.M. analyzed the data. S.M. wrote the first draft, and all authors read and approved the final manuscript.
References
- 1.U.S. Bureau of Labor Statistics Workplace violence in healthcare. 2018. https://www.bls.gov/iif/oshwc/cfoi/workplace-violence-healthcare-2018.htm Accessed July 4, 2021.
- 2.Philips J.P. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374:1661–1669. doi: 10.1056/NEJMra1501998. [DOI] [PubMed] [Google Scholar]
- 3.UN News . UN News; 2020. Chief calls for domestic violence ‘ceasefire’ amid ‘horrifying global surge.’.https://news.un.org/en/story/2020/04/1061052 Accessed July 4, 2021. [Google Scholar]
- 4.Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 5.Mazza M., Marano G., Lai C., Janiri L., Sani G. Danger in danger: interpersonal violence during COVID-19 quarantine. Psychiatry Res. 2020;289:113046. doi: 10.1016/j.psychres.2020.113046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taub A. The New York Times; 2020. A new Covid-19 crisis: domestic abuse rises worldwide.https://www.nytimes.com/2020/04/06/world/coronavirus-domestic-violence.html Accessed July 4, 2021. [Google Scholar]
- 7.McGuire S.S., Mullan A.F., Clements C.M. Unheard victims: a prospective descriptive study of multidisciplinary incidence of violence among emergency department staff at an Academic Medical Center. WestJEM. 2021 doi: 10.5811/westjem.2021.2.50046. [DOI] [Google Scholar]
- 8.Hurst L. Euronews; 2020. Coronavirus: health workers clapped across the world for battling on the COVID-19 frontline.https://www.euronews.com/2020/03/24/coronavirus-health-workers-clapped-across-the-world-for-battling-on-the-covid-19-frontline March 24, 2020. Accessed July 5, 2021. [Google Scholar]
- 9.O’Kane C. CBS News; 2020. Mattel releases new toys to honor workers on the front lines of the coronavirus battle.https://www.cbsnews.com/news/mattel-thank-you-heroes-frontline-workers-action-figures/ April 30 2020. Accessed July 5, 2021. [Google Scholar]
- 10.Lake T. CNN; 2020. The real heroes in the fight against coronavirus.https://edition.cnn.com/2020/04/02/opinions/nurses-doctors-volunteers-covid19-coronavirus-lake/index.html updated April 2, 2020. Accessed July 5, 2021. [Google Scholar]
- 11.Cluver L., Lachman J.M., Sherr L., et al. Parenting in a time of COVID-19. Lancet. 2020 doi: 10.1016/s0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeffery M.M., D’Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Porterfield C. Why Spitters could be charged as terrorists because of the coronavirus. 2020. https://www.forbes.com/sites/carlieporterfield/2020/03/31/coronavirus-spitters-could-be-charged-as-terrorists---heres-why/?sh=1dd6669779c2