With interest, we read the commentary by Zhong et al. entitled, “How can we best use COVID-19 vaccines in adolescents?” discussing the risk and benefits of vaccination for the adolescent age group and concluding that the risk-benefit ratio for vaccinating healthy adolescents was equivocal [1]. The authors noted in the first sentence of the article, “Mass vaccination of the world population is our ticket out of the COVID-19 pandemic”. We posit that the adolescent age group, a significant proportion of the “world population”, is an important group to vaccinate to curb the spread of COVID-19 disease and to directly protect children and adolescents at risk of disease and disease complications.
Adolescent children have social behaviors that may lead to increased exposure to COVID-19 including congregating with friends, participating in extramural or intramural sports, having a sense of teenage invincibility, and importantly attending school each day. Vaccination for this age group is clearly very important, not only to protect each teenager but especially to reduce viral spread to unvaccinated peers. Although schools with mitigation measures in place were mostly successful at preventing high rates of transmission in the 2020–2021 school year, it remains to be seen how the highly contagious delta variant will impact the 2021–2022 school year. As Zhong et al. have pointed out, we all want to assist our adolescents in the return to ‘normal life’, and vaccination would move us forward toward that end.
COVID-19 containment has also been complicated by the emergence of multiple variant strains of SARS-CoV-2 [2]. The data on which Zhong et al. base much of their commentary pertained to the alpha variant strain of Sars-CoV-2 (B.1.1.7). Currently, the dominant circulating strain is B.1.617.2 or the delta variant. The virus has changed substantially in its ability to infect and transmit between people and is thought to be roughly 50% more contagious than the alpha variant, which itself was roughly 50% more contagious than the ancestral strain [2]. Data on age and demographics from the delta surge are still emerging, but as hospitalizations have increased, a clear theme has arisen across the country: patients with COVID-19 are younger and mostly unvaccinated, and hospitalizations in children are up dramatically, primarily in places with low community vaccination coverage [3]. It is unknown whether future variant strains of the virus will eventually elude the protection afforded by the vaccine, but this is a concern. This adds urgency to the goal of vaccinating enough people to stop the spread of disease; it will be essentially impossible to interrupt transmission without vaccinating children and adolescents. The immunization of adolescents is not just an indirect way of protecting adults; rather, it is a way (1) to help interrupt transmission, (2) to prevent the development of future variants, (3) to protect children and adolescents themselves, and (4) to support a return to a more normal life.
During the week ending August 14, 2021, while the proportion of COVID-19 patients aged 0–17 years who were admitted to the intensive care unit in August was similar to that seen during the circulation of the alpha variant [4], the hospitalization rate per 100,000 children and adolescents was nearly five times the rate during the week ending June 26, 2021, thus significantly changing the impact on our child/adolescent population. The hospitalization rate among unvaccinated adolescents aged 12–17 years was 10.1 times higher than among those who were not vaccinated [3]. Clearly, with the evolution of the virus, the effects on each age group—including our adolescent population—may change quickly and with unknown consequences, including changes in mortality, multisystem inflammatory syndrome in children, or ‘long COVID’ rates. Vaccination will help us avoid these unknowns.
Zhong et al. further argued that the mortality rate among the adolescent group was low with COVID-19, approximately 1–2 per million, comparing COVID-19 with seasonal influenza due to similar mortality indices. COVID-19 may be comparable by mortality with influenza in this group, but most humans have an epigenetic history with seasonal influenza, whereas humans have no prior immune history with Sars-CoV-2 [5]. The transmissibility of seasonal influenza (R0 ∼ .9–2.1) and many other viruses, including the alpha variant of Sars-CoV-2 (R0 ∼ 1.5–3.5), is substantially less than the currently circulating delta variant of Sars-CoV-2 (R0 estimated to be ∼ 5–9) [[6], [7], [8]]. One could argue against making comparisons between a novel highly infectious pandemic-creating virus and more established viruses, but a more reasonable comparison than influenza may be poliovirus. Poliovirus is nearly as transmissible as the delta strain of Sars-CoV-2, and 90%–95% of poliovirus infections are asymptomatic in children. Before the polio vaccine was available, the devastating consequences of poliovirus infection, including paralytic polio, affected approximately 1% of children, and, of that 1%, the mortality rate was between 5% and 15% [9]. Through vaccination, we no longer see poliovirus outbreaks in the United States as it has nearly been eradicated from the globe, with notable exceptions. COVID-19, like poliovirus, results in large numbers of mild and asymptomatic infections in adolescents but severe morbidity and mortality in some. Recently, the increase in cases as a result of the delta variant has resulted in increased hospitalizations in this age group [10,11]. Multiple deaths in the adolescent age group have now been reported [12]. Just as we recommend routine vaccination against poliovirus for every child, it is our strong opinion that it is also appropriate for us to vaccinate children, including adolescents, against COVID-19.
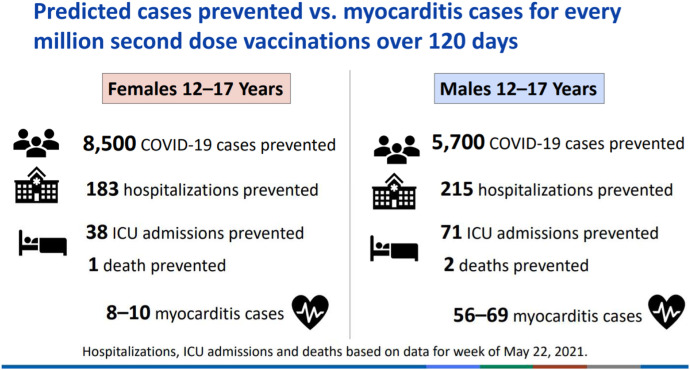
There are some safety concerns described by Zhong et al. related to the development of pericarditis and myocarditis in younger persons after receiving mRNA COVID-19 vaccines. A summary of the data from the June 23, 2021 Advisory Committee on Immunization Practices Meeting at the Centers for Disease Control and Prevention indicated a higher rate of observed over-expected cases of myocarditis/pericarditis among 12- to 39-year-olds who received an mRNA vaccine, and the risk was greater after the second dose of the vaccine [13]. Importantly, post-vaccine myocarditis is mild, typically with quick clinical recovery rates [14]. These cases clustered approximately one week after the vaccine dose and were more common among males than females [13]. However, when looking at the number of cases and hospitalizations prevented among this age group versus the number of mild cases of myocarditis/pericarditis associated with mRNA vaccination, the benefits of vaccination significantly outweigh the risks (Figure 1 ) [12]. A study published in September 2021 showed 15.7 times the risk of myocarditis from March 2020 to January 2021 among patients with COVID-19 disease versus those without the disease [15]. More data are needed, but the risk of myocarditis/pericarditis rises significantly with COVID-19 disease, making vaccination of greater benefit.
Figure 1.
Risk versus benefit of the mRNA vaccine: Predicated cases prevented versus myocarditis cases, Wallace M OS. COVID-19 mRNA vaccines in adolescents and young adults: Benefit-risk discussion. Presented at ACIP, June 23, 2021. CDC, Atlanta, GA. In:2021.
The vaccination of adolescents in the United States is not likely to have a direct effect on the ability of the rest of the world to receive COVID-19 vaccines. It is critical that the entire world be vaccinated, but the number of doses needed to vaccinate adolescents is a tiny percentage of the number of doses needed for the global vaccine supply. In addition, the United States has been among the hardest hit countries in the world; therefore, working to interrupt transmission in the United States by all possible means is reasonable. The health disparities for COVID-19 morbidity and mortality by race/ethnicity that have occurred during the pandemic in this country have been of great concern; mitigating these inequalities through mass vaccination that includes the adolescent population is a worthy goal.
Zhong et al. make some interesting and valid points regarding vaccination after prior infection and the potential efficacy of a single dose of an mRNA vaccine in adolescents who have been infected previously. Specifically, because the rare risk of peri-myocarditis typically occurs after the second dose of mRNA vaccines, could this dose be avoided for adolescents previously infected with COVID-19? We agree that further study of clinical outcomes regarding vaccination after natural infection is appropriate, especially due to high immunogenicity in this age group [16]. The question remains, does an adolescent person need both vaccine doses after natural infection or would a single dose offer sufficient protection without potential risk? Perhaps a lower dose of the vaccine is appropriate for younger children. Research is needed to answer these questions.
Finally, physicians and scientists need to focus attention on a major challenge preventing us from putting an end to this pandemic: vaccine hesitancy [17]. Although it may not be the case throughout the world, vaccines are in ample supply in the United States, and we need to remain vigilant in our unified public health message of risk mitigation focused on reducing Sars-CoV-2 transmission by encouraging vaccination of all eligible persons. In addition, we must continue efforts to encourage the use of other mitigation measures such as appropriate mask use, continued handwashing, and social distancing. Choosing not to utilize a safe and effective vaccine among specific age groups because of lower mortality risk in the midst of an evolving and ongoing pandemic is not justifiable. That choice will keep Sars-CoV-2 circulating, allowing for the development of further mutations which will ultimately hurt us all.
Footnotes
Conflicts of interest: D.L.T. and S.T.O.L. declare that they have no conflicts of interest. OUHSC entered into a service agreement for 2020 with Pfizer, Inc. for educational research for which A.B.M served as a principal investigator.
References
- 1.Zhong Y., Lee L.Y., Tambyah P.A., et al. How can we best use COVID-19 vaccines in adolescents? – an International Prespective. J Adolesce Health. 2021;69:1. doi: 10.1016/j.jadohealth.2021.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Immunization and Respiratory Diseases (NCIRD) DoVD . 2021. What You need to Know about variants.https://www.cdc.gov/coronavirus/2019-ncov/variants/variant.html Available at: [Google Scholar]
- 3.Delahoy M.J., Ujamaa D., Whitaker M., et al. Hospitalizations associated with COVID-19 among children and adolescents — COVID-NET, 14 States, March 1, 2020–August 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1255–1260. doi: 10.15585/mmwr.mm7036e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegel D.A., Reses H.E., Cool A.J., et al. Trends in COVID-19 cases, emergency Department Visits, and hospital Admissions among children and adolescents aged 0–17 Years — United States, August 2020–August 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1249–1254. doi: 10.15585/mmwr.mm7036e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menachery V.D., Schäfer A., Burnum-Johnson K.E., et al. MERS-CoV and H5N1 influenza virus antagonize antigen presentation by altering the epigenetic landscape. Proc Natl Acad Sci United States America. 2018;115:E1012–E1021. doi: 10.1073/pnas.1706928115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luo C.H., Morris C.P., Sachithanandham J., et al. medRxiv; Cold Spring Harbor, NY: 2021. Infection with the SARS-CoV-2 Delta Variant is Associated with Higher Infectious Virus Loads Compared to the Alpha Variant in both Unvaccinated and Vaccinated Individuals. [DOI] [Google Scholar]
- 7.Chowell G., Miller M.A., Viboud C. Seasonal influenza in the United States, France, and Australia: Transmission and prospects for control. Epidemiol Infect. 2008;136:852–864. doi: 10.1017/S0950268807009144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dagpunar J. medRxiV; Cold Spring Harbor, NY: 2021. Interim estimates of increased transmissibility, growth rate, and reproduction number of the Covid-19 B.1.617.2 variant of concern in the United Kingdom. [DOI] [Google Scholar]
- 9.European Centre for Disease Prevention and Control . 2018. Disease factsheet about poliomyelitis.https://www.ecdc.europa.eu/en/poliomyelitis/facts#:∼:text=The%20mortality%20rate%20for%20acute,of%20patients%20with%20paralytic%20poliomyelitis Available at: [Google Scholar]
- 10.American Academy of Pediatrics Cdc: Delta variant causing increase in pediatric COVID-19 cases, not severity. 2021. https://www.aappublications.org/news/2021/09/03/covid-delta-variant-children-hospitalizations-090321 Available at:
- 11.Pediatrics AAo . 2021. Children and COVID-19: State-Level data Report.https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ Available at: [Google Scholar]
- 12.Wallace M OS . CDC; Atlanta, GA: 2021. COVID-19 mRNA vaccines in adolescents and young adults: Benefit-risk discussion. Presented at ACIP, June 23, 2021. [Google Scholar]
- 13.T S . CDC; Atlanta, GA: 2021. Vaccine safety updates. Presented at ACIP, June 23,2021. [Google Scholar]
- 14.Jain S.S., Steele J.M., Fonseca B., et al. COVID-19 vaccination-associated myocarditis in adolescents. Pediatrics. 2021 doi: 10.1542/peds.2021-053427. [DOI] [PubMed] [Google Scholar]
- 15.Boehmer T.K., Kompaniyets L., Lavery A.M., et al. Association between COVID-19 and myocarditis using hospital-based administrative data – United States, March 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1228–1232. doi: 10.15585/mmwr.mm7035e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frenck R.W., Jr., Klein N.P., Kitchin N., et al. Safety, immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents. N Engl J Med. 2021;385:239–250. doi: 10.1056/NEJMoa2107456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dror A.A., Eisenbach N., Taiber S., et al. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]