Abstract
With 40 million people and substantial county and regional variation in socio-demographics and health services, California is an important setting to study disparities. Its population -- 39.1% Latino, 5.3% Black, and 14.4% Asian -- experienced 54,124 COVID-19 deaths through March 7, 2021, the highest nationally. We analyzed California’s racial/ethnic disparities in COVID-19 exposure risks, testing rates, test positivity, and case rates, through October 2020. We combined data from 15.4 million SARS-CoV-2 tests with sub-county exposure risk estimates from the American Community Survey. Based on accumulated evidence, we defined “high exposure risk” households as those with ≥1 essential workers and fewer rooms than inhabitants. Latino individuals are 8.1 times more likely to live in high exposure risk households than White individuals (23.6% vs. 2.9%); overrepresented in cumulative cases (3,784 vs. 1,112 per 100,000); and underrepresented in cumulative testing (35,635 vs. 48,930 per 100,000). These risks and outcomes were worse for Latinos than for other racial/ethnic groups. Sub-county disparity analyses can inform local targeting of interventions and resources, including community-based testing and vaccine access and uptake measures. Tracking COVID-19 disparities and developing equity-focused public health programming that mitigates effects of systemic racism can help improve health outcomes among California’s populations of color.
Background
The US COVID-19 pandemic has disproportionately impacted people with low socio-economic status and Black, Indigenous, and Latino people,(1–6) who have experienced higher rates of cases,(7, 8) hospitalizations,(1, 9, 10) and deaths.(8, 9, 11) As a state of 40 million people with substantial county and regional variation in terms of demographics, socioeconomic status, and health services, California is an important setting in which to study these disparities. As of March 7, 2021, California’s COVID-19 deaths (54,124) were the highest in the nation, within a statewide population that is 39.1% Latino, 5.3% Black, and 14.4% Asian.(12, 13) Previous analyses of COVID-19 disparities in California have focused on single neighborhoods, specific healthcare systems, a single county, or the state as a whole.(14–16) An examination of disparities at the community scale (sub-county) for the entire state has yet to be undertaken.
Disparities in COVID-19 outcomes can arise from unequal exposure to transmission risks that concentrate in disadvantaged populations, amplified by various economic and social factors both inside and outside of the household including working outside the home as essential workers, hourly wage jobs, living in large, multi-generational households, and limited access to housing and to health care.(6, 17–19) Essential workers are often unable to work from home and therefore are more likely to be in contact with infectious individuals.(20–22) Larger household sizes, especially when in smaller homes, make it more difficult for individuals to quarantine if they have been exposed or isolate if they have been infected.(20, 23) Households with crowded conditions and essential workers are often poor and may not be able to access testing or treatment promptly. Lack of adequate and timely testing and diagnosis that can improve prognosis and break cycles of transmission further increases risks of infection and illness. Heightened risk of exposure at the household level can be magnified in communities within small geographic areas in which household-level risks are concentrated, resulting in substantially higher case rates.(16, 19, 24) Systematic racism in employment markets, financial institutions, and housing access results in larger numbers of essential workers, smaller houses, and more geographically concentrated populations for Black, Latino, Asian, and Indigenous people.(5, 18, 25) While previous studies have highlighted disparities in COVID-19 hospital and death outcomes and their correlations with race/ethnicity(9, 10, 26), we highlight the differences in exposure, geography, testing, and COVID-19 cases over time.
We analyze COVID-19 disparities in terms of structural risk exposures, testing, test positivity, and COVID-19 cases in California at the sub-county level, explicitly considering how these risks and outcomes concentrate geographically and evolve over time.
Methods
We combined weekly surveillance data on SARS-CoV-2 testing volume and diagnosed cases with area-level estimates of risk factors to quantify levels and disparities in risks, testing, and health outcomes, by race/ethnicity and Public Use Microdata Area (PUMA), for all of California. We analyzed cases and tests from March 22 through October 3, 2020. By October 3, total tests were 15,421,862 and cumulative polymerase chain reaction (PCR)-confirmed cases were 817,947.
Demographic and Geographic Units of Analysis
Outcome data are reported weekly, by race/ethnicity, and by Public Use Microdata Area (PUMA). For confidentiality, data included four aggregate categories of self-reported race/ethnicity: Hispanic/Latino of all races (“Latino”), non-Hispanic Black (“Black”), non-Hispanic White (“White”), and non-Hispanic Asian (“Asian”). A fifth category of “Unknown/Other” comprises both missing data and individuals that did not wish to report their race/ethnicity, as well as a small proportion of racial groups (e.g., Native Hawaiian/Pacific Islander, Indigenous, multiracial) not included in the above four categories.
Public Use Microdata Areas are the smallest geographic unit reported in the American Community Survey (ACS) public microdata with a minimum population of 100,000. In California, there are 265 PUMAs within 58 counties. Twenty-seven counties contain more than one PUMA, allowing for sub-county analysis. Eight counties contain a single PUMA, while 23 counties with small populations are grouped together into seven shared PUMAs. The average population in a PUMA in California is 145,000, with the largest being 231,000. To highlight broad geographic patterns, we group PUMAs for some analyses into the five reporting regions used by the California Department of Public Health (Appendix pg. 2).(27)
Data Sources
We analyzed testing and case data provided by the California Department of Public Health from statewide surveillance systems, stratified by PUMA-level after aggregation based on geocodes across our analytic time period. Population and risk exposure data were extracted from the 2014–2018 5-year ACS public use microdata file, downloaded from IPUMS USA.(28)
Exposure and Outcome Definitions
We computed test, case, and test positivity rates by PUMA and race/ethnicity, over the entire time period and month-by-month. Tests were defined as counts of real-time PCR assays performed each week for people residing in each PUMA (and of a given race/ethnicity for stratified analyses). Test positivity was defined as total positive tests divided by total tests, with no de-duplication for repeat testing. Cases were defined as individuals with laboratory-confirmed SARS-CoV-2 by PCR assay within the week of their reported episode date determining when they are counted. Episode date is automatically calculated by the surveillance system as the earliest of the following dates (if the dates exist): date received, date of diagnosis, date of onset, specimen collection date, or date of death. We additionally analyzed state-level COVID-19 deaths and death rates by race/ethnicity.
Based on accumulated evidence on COVID-19 transmission risks (16–18, 20–24), we developed an indicator capturing two key sources of exposure to risk of SARS-CoV-2 transmission using data from the ACS.(29) We analyzed ACS data on 1,800,910 Californians living in households, characterized by race/ethnicity, PUMA in which the household was located, number of rooms the household had, and household members’ employment status. We then characterized PUMA populations (or racial/ethnic subgroups within PUMAs) by the number and percentage of people living in households considered to be “high-risk,” defined as having at least one essential worker and fewer rooms than people (Supplemental Exhibits S1 and S2). [27] We defined essential workers based on the “Essential Critical Infrastructure Workforce” advisory list from the Department of Homeland Security.(30) We used Standard Occupational Classification system codes to identify individuals classified as essential workers.(30) For some individuals, full six-digit occupation codes were unavailable. In these cases, individuals were assigned the average percent of essential workers based on all nested occupation codes within the broader job category.
Analysis
We defined aggregate measures of risk at household, PUMA and race/ethnicity subgroup levels using weights provided with the ACS. We computed rates and rate ratios for all outcome measures, using rates for White populations as the reference. For PUMAs that had very small White populations, we used county-level rates for White populations as the reference when computing rate ratios. We chose the White population as the reference group because it is the largest population at the state-level and provides a consistent baseline comparator for all PUMAs. Finally, we assessed how measures of disparities have evolved over the course of the epidemic.
Some cases and tests were not recorded with residential geocodes (preventing assignment to a PUMA), race/ethnicity, or both. Because negative tests were more likely to be missing one or both dimensions, removing incomplete observations tends to overestimate test positivity. Hence, we redistributed cases and tests with missing PUMA and/or race/ethnicity for the main analysis based on the observed distributions by PUMA and race/ethnicity in data with complete information.
We conducted sensitivity analyses to assess whether our findings were strongly influenced by redistribution strategy for tests and cases with missing PUMA or race/ethnicity, and on our definition of essential worker. Further details on these sensitivity analyses are provided in the appendix.(27)
All analyses were conducted using R version 4.0.2 (R Group, Vienna Austria) and code is accessible at https://github.com/SC-COSMO/ca_covid_disparities. Additional information on methods, results for all counties, and sensitivity analyses are provided in the appendix.(27)
Stanford University’s institutional review board approved this study (Protocol IRB-55671).
Limitations
Our analysis has several limitations. The sub-county data we used does not include all cases and tests, as not all county-level records of tests and cases have geolocation data. A substantial percentage of recorded tests and cases are missing information on race and ethnicity, especially among negative tests. Additionally, we were unable to disaggregate outcomes among Indigenous populations from the “Unknown/Other” category. Although sensitivity analyses showed that our results and conclusions are robust, more complete and more granular race/ethnic reporting will aid future analyses of disparities. Our analysis only links housing and occupation characteristics with test and case data at the PUMA level. The present analysis does not aim to make causal statements about drivers of disparities; nor do we attempt to evaluate the potential effects of interventions like scaling up testing. The relatively small Black population in California may differ in important ways from Black populations in other parts of the country making generalization more challenging. We use historical employment data from the ACS, which does not include the changes in employment rates in 2020. There is almost certainly some dynamic change in occupation and housing over ACS’s five-year period as well as in the post-survey period since 2018. Due to privacy considerations, subcounty, race/ethnic individual-level data were not available for analysis. Since our analysis is linked at the area-level and not at the individual-level, we are unable to directly link an individual’s race/ethnicity and exposure risk to COVID-19 cases and deaths. These changes are unlikely to substantially affect results. Additionally, we assessed annual area-level ACS estimates from 2014–2018 and found that they are quite stable over time, mitigating some of the concern about this potential limitation (Supplemental Exhibits S3 and S4).[27]
Results
Latino populations were overrepresented in California’s 817,947 COVID-19 cases and Latino and Black populations are overrepresented in the 17,815 deaths (March 22 to October 3, 2020), reported in Exhibit 1. Race/ethnicity is known for 64.7% of cases. Among cases with known race/ethnicity, more than half (70.0%) were Latino, compared to their 39.1% population share. White people were underrepresented (19.1% of cases with known race/ethnicity; 37.5% of the population). One of every two people who died (48.5%) was Latino, and death rates in both Latino (59.2 per 100,000) and Black (65.0 per 100,000) populations were more than 1.5 times higher than that of the White population, at 38.3 deaths per 100,000 cases. Observed statewide disparities in these outcomes for Latino populations emerge despite having disproportionately low cumulative testing rates (35,635 per 100,000 vs. 48,930 per 100,000 for White populations). Like the Latino population, the Asian population also had low cumulative testing rates (35,144 per 100,000), but their observed case rates and death rates were not elevated compared to the White population. Test positivity rates were 10.6% for Latino populations compared to 2.3% for White populations in California. Latino individuals in California are 8.1 times more likely to live in crowded households with an essential worker compared to White individuals (23.6% vs. 2.9%); Asian individuals are 3.9 times more likely to live in such households, and Black individuals are 2.2 times more likely. Compared to the county-level data, 4.7% of cases and 29.1% of tests were missing PUMA location information.
Exhibit 1:
California Population and COVID-19 Indicators by Race and Ethnicity
| Total | Latino | Black | White | Asian | Unknown/Other* | |
|---|---|---|---|---|---|---|
| Population | 38,329,281 | 14,978,196 | 2,043,284 | 14,367,727 | 5,537,498 | - |
| Cases | 817,947 | 370,605 | 24,624 | 101,195 | 33,147 | 288,376 |
| Tests | 15,421,862 | 1,934,836 | 391,333 | 2,320,694 | 694,937 | 10,080,062 |
| Deaths | 17,815 | 8,635 | 1,295 | 5,330 | 2,053 | 502 |
| Cases with Location Data | 779,823 | 357,231 | 23,538 | 97,026 | 32,024 | 27,0004 |
| Tests with Location Data | 10,935,196 | 1,300,536 | 288,799 | 1,915,135 | 546,809 | 6,883,917 |
| Estimated Case Rate per 100,000 + | 2,134 | 3,784 | 1,893 | 1112 | 950 | - |
| Estimated Testing Rate per 100,000 people + | 40,235 | 35,635 | 54,236 | 48,930 | 35,144 | - |
|
Estimated Test Positivity
+
(%) |
5.3 | 10.6 | 3.5 | 2.3 | 2.7 | - |
| Estimated Death Rate per 100,000 cases + | 46.5 | 59.2 | 65.0 | 38.3 | 38.2 | - |
| Individuals in households with number of rooms < number of occupants | 6,305,218 | 4,489,962 | 213,685 | 634,091 | 826,271 | - |
| Individuals in households with essential workers | 24,116,506 | 10,805,940 | 1,096,074 | 7,637,099 | 3,720,737 | - |
| Individuals in households with essential workers & number of rooms < number of occupants | 4,817,502 | 3,538,978 | 130,540 | 418,354 | 634,015 | - |
Source/Notes: SOURCE American Community Survey, California Department of Public Health. NOTES Data shown is from March 22 to October 3, 2020, accessed February 26, 2021.
“Unknown/Other” comprises both missing data and individuals that did not wish to report their race/ethnicity (83% of unknown/other tests, 77% of unknown/other cases, and 24% of unknown/other deaths), as well as a small proportion of racial groups (e.g., Native Hawaiian/Pacific Islander, Indigenous, multiracial) not included in Asian, Black, White, and Latino categories. Available racial/ethnic groups were selected as part of a data use agreement to maintain non-identifiability.
Estimated case, test, test positivity, and death rates show values after distributing Other/Unknown outcomes (details on distribution available in Methods). Cells are blank because population data are not available for the Unknown/Other category, which is only applicable for directly reported COVID-19 outcomes.
Household exposure risk, test rates, and case rates vary widely across PUMAs in California. Areas with higher cumulative case rates are more likely to have a high proportion of people living in crowded households with at least one essential worker, as reported in Exhibit 2. These areas also tend to have at least a plurality Latino population. In many parts of California, areas with low cumulative test rates are more likely to have both high case rates and a large proportion of high-risk households. The spatial patterns highlighted in Los Angeles, which indicate strong spatial concentration of risks and poor outcomes among predominantly Latino PUMAs, are also observed in other large-population counties, including Riverside, San Bernardino, Orange, Santa Clara, Alameda, and Contra Costa (Appendix pages 39–52).(27)
Exhibit 2:
Correlation between household exposure risk, case rates, and test rates, by PUMA for California and counties with population exceeding 1.5 million.
| Geography | Exposure vs. Case Rate | Exposure vs. Test Rate | Case Rate vs. Test Rate |
|---|---|---|---|
| California | 0.69*** | 0.20** | 0.19** |
| Los Angeles County | 0.84*** | −0.06 | −0.08 |
| San Diego County | 0.77*** | 0.22 | 0.69*** |
| Orange County | 0.93*** | −0.16 | 0.11 |
| Riverside County | 0.65** | −0.06 | 0.57* |
| San Bernardino County | 0.88*** | 0.56* | 0.77*** |
| Santa Clara County | 0.80*** | 0.26 | 0.40 |
| Alameda County | 0.86** | −0.36 | −0.07 |
Source/Notes: SOURCE American Community Survey, California Department of Public Health. NOTES Data shown is from March 22 to October 3, 2020, accessed February 26, 2021. Correlations reported are the Pearson correlation coefficient. Statistical significance
p<0.05
p<0.01
p<0.001.
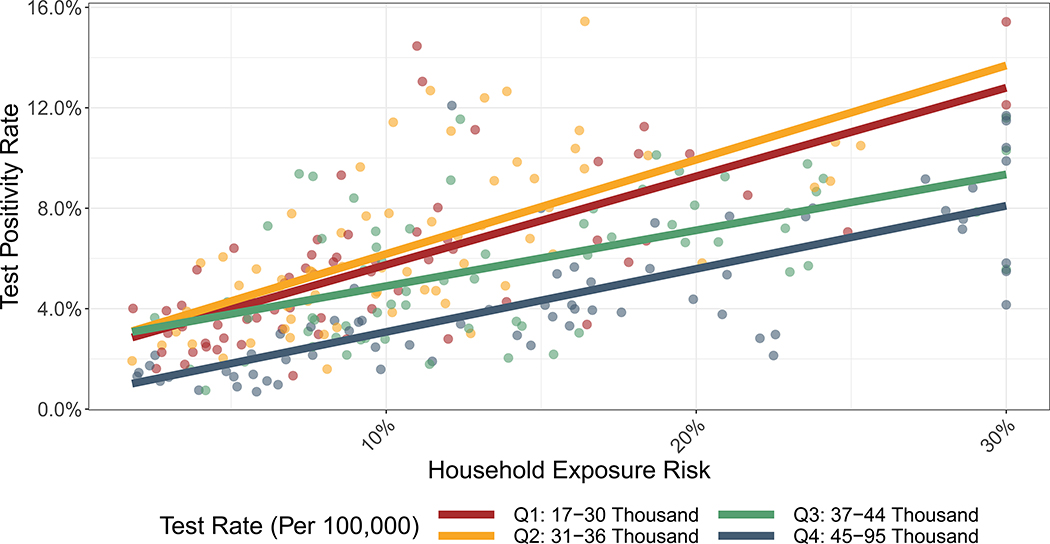
Disparities in case rates in relation to varying household exposure risk are mirrored in persistent disparities in test positivity. Exhibit 3 shows that stratifying by testing rate, PUMAs with larger proportions of people living in households with high exposure risk have higher test positivity rates. Despite substantial increases in testing rates across the state, test positivity has been consistently highest where household exposure risks are high (Supplemental Exhibits S5–S10).(27) Test rates have increased from an average of 3,900 tests per 100,000 population across PUMAs in May to an average of 8,464 tests per 100,000 population in September. Test positivity rates saw particularly large decreases between July and September.
Exhibit 3: Relationship Between Household Exposure Risk, Test Rate, and Test Positivity Rate.
SOURCE Authors’ analysis of data from the American Community Survey and the California Department of Public Health. NOTES Outcomes span March 22 to October 3, 2020. Month–specific results are located in the Appendix. Colors show quartiles of testing rates. Each circle shown represents one of California’s PUMAS. To improve visualization, household exposure risk was capped at 30%.
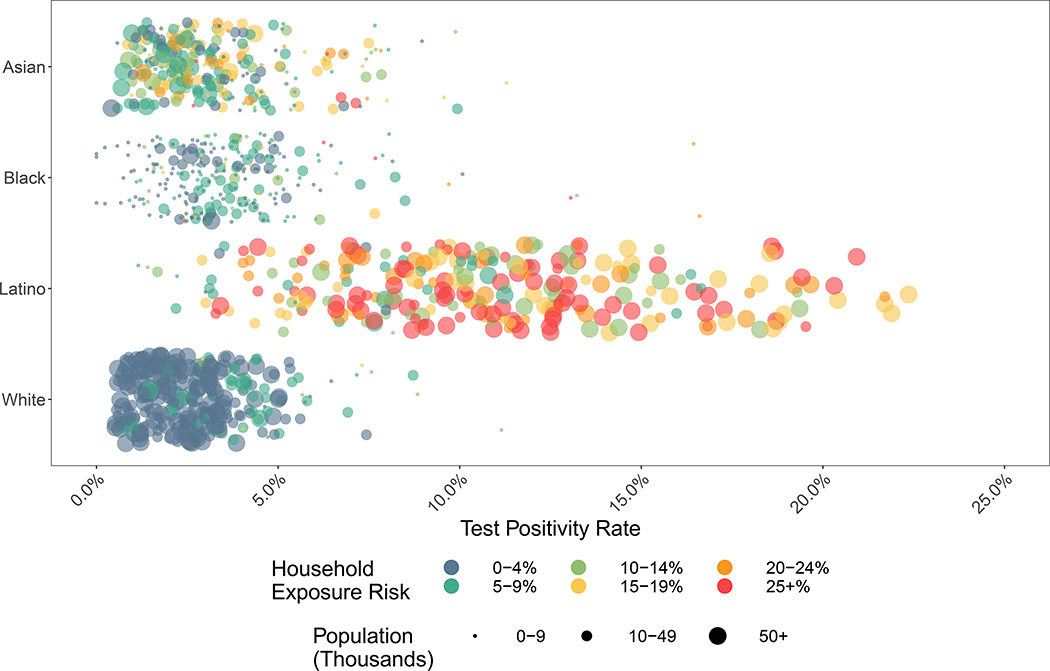
Disaggregating by race/ethnicity in Exhibit 4, Latino populations have seen the smallest improvements in test positivity over time. This is consistent with disparities in household exposure risks given that Latino individuals are more likely to live in overcrowded households with essential workers and in PUMAs with higher proportions of such households. In May, test positivity exceeded 10% among Latino populations in 39% of PUMAs, compared to 3% of PUMAs for all other race/ethnicity groups (Supplemental Exhibit S11).[27] In July, test positivity exceeded 10% among Latino populations in 68% of PUMAs, compared to 5% of PUMAs for all other race/ethnicity groups. In September, test positivity exceeded 10% among Latino populations in 7% of PUMAs, compared to 1% of PUMAs for all other race/ethnicity groups. On average across all PUMAs, test positivity was five times higher among Latino populations than their county’s average for White populations. Exhibit 4 also shows that among Asian populations there is heterogeneity in test positivity rates, with higher positivity rates correlated with household exposure risk.
Exhibit 4: Test Positivity Rate by Race/Ethnicity and Household Exposure Risk.
SOURCE Authors’ analysis of data from the American Community Survey and the California Department of Public Health. NOTES Outcomes span March 22 to October 3, 2020. Each circle shown represents the racial/ethnic-specific subpopulation of one of California’s PUMAs. Month–specific results are located in the Appendix.
The pattern of persistently high test positivity rates among Latinos was observed across all regions of California, across all epidemic months, and even as testing rates have improved (Supplemental Exhibit S12)[27]. Notably, the scale-up in testing was smallest among Latinos in Imperial, Orange, Riverside, San Bernardino, and San Diego counties, and test positivity rates among these populations have remained consistently high. Despite small population sizes, Black populations in all regions tended to have higher test positivity than White populations. In July, Black populations in 73% of California’s PUMAs had higher test positivity rates than their county’s average for White populations.
Our results were robust to sensitivity analyses that varied the definition of essential worker and that used alternative rules for handling tests and cases with missing geolocation data and unknown race/ethnicity. We compared the percentage of cases and tests with residential geolocation information by county and race/ethnicity (Supplemental Exhibits S13 and S14)[27]. Tests with unknown/other race/ethnicity accounted for 63.0% of tests with PUMA-level location data and were less likely to be positive. Various strategies of redistribution of tests with unknown/other race/ethnicity reduced test positivity rates in terms of their levels, but disparities between racial/ethnic groups persisted regardless of strategy (Supplemental Exhibits S15–S19)[27].
Discussion
We analyzed testing and case rates for all of California from March 22 to October 3, 2020 at the sub-county level by race/ethnicity. We assessed household exposure risks, test rates, test positivity rates, and case rates. Latino populations across California have higher household exposure risks, lower testing rates, higher test positivity rates, higher case rates, and higher death rates. Disparities in cases and test positivity rates have persisted throughout the course of the epidemic and across the state, even as testing has been scaled up. We developed a joint measure of risk of exposure and transmission of COVID-19 that considers if individuals live in a household with an essential worker and fewer rooms than people. Areas with higher fractions of individuals living with this exposure risk have higher case rates and test positivity rates; Latinos are more likely to live in households with this risk exposure and in areas where this risk exposure is disproportionately concentrated.
This analysis and others like it are designed to identify the social and structural determinants that contribute to health disparities, and to further demonstrate the associations between those determinants and race/ethnicity. As our analysis illustrates, exposure, testing, and case rates differ across Latino, Black, and Asian populations, suggesting that determinants and barriers may differ across these groups just as their historical experiences of racism and exclusion have differed. Furthermore, race/ethnic categories like “Asian” include multiple diverse groups (e.g., Chinese, Japanese, Vietnamese) whose past experiences, current exposures, and patterns of access and outcomes are likely to be heterogeneous. While analyses like ours provide a powerful tool for understanding the epidemiology of the pandemic and for developing more effective interventions to control it, one limitation of this study and others like it is in understanding the role of racism itself in contributing to disproportionate COVID-19 burden among racial/ethnic groups.(31) Just because we did not analyze a definite indicator of exposure to racism in this study does not mean that such an association does not exist. The analysis we provide could be used to ask questions about racism’s impacts at a sub-county geographic level, which could identify how forms of segregation, divestment, or exclusion from the housing and job markets can put Latino, Asian, and Black communities at unique COVID-19 risk.(8) Further research equipped to measure the effects of racism on COVID-19 outcomes is needed.
As part of California’s reopening plan, counties must achieve and maintain epidemic control as measured by a suite of metrics. One key metric that the California Department of Public Health designed was a disparities metric based on test positivity that must be met by each county in order to progress to the next tier of reopening.(32) Low testing rates and high test positivity rates may be indicative of under-testing in areas of higher risk for transmission and hence prevalence. This could result in an underestimation of disparities in the burden of infections by race/ethnicity, as infections are only counted towards burden when they are detected as cases. Consequently, expanded testing may help to appreciate the magnitude of COVID-19 outcomes disparities but alone may be insufficient to eliminate them. Risks of exposure and poor COVID-19 outcomes are spatially correlated and concentrated. Geographically targeted interventions may be efficient in improving outcomes and reducing disparities.
Nationally, researchers are actively analyzing COVID-19 disparities.(7, 11, 33) John McLaughlin et al. showed the importance of county-level predictors of COVID-19 including housing, pollution, race/ethnicity, income inequality, and mobility out of the home.(19) The present study demonstrates the high value of mapping case rates and test positivity to socio-structural determinants of exposure in California at the sub-county level, though these methods can be implemented in any jurisdiction in the US using ACS data. This analytic approach can inform targeting of interventions such as personal protective equipment provision, rapid testing, income supplementation, and sick pay for those populations at highest risk for poor outcomes, similar to programs being implemented in California now to reduce COVID-19 health disparities.(32)
During COVID-19 shutdowns, essential workers provide many services that allow other people to shelter in place to avoid the epidemic risk, even as they themselves face higher risk of exposure.(20–22) Many essential workers are paid hourly and are not guaranteed paid sick leave.(34) Our results suggest policies to address disparities including targeting testing and transmission risk reduction efforts, facilitating quarantine after exposure, ensuring paid sick leave for essential workers, vaccine allocation to reduce disparities, and expanding the provision of resources in Spanish to effectively promote testing and treatment.(2) California is taking specific steps to implement such policies to address COVID-19 related disparities including ongoing monitoring via an equity metric,(32) quarantine assistance for farmworkers,(35, 36) lists of resources for immigrants,(37) COVID-19 communication materials in many languages including Spanish and Indigenous languages,(38) and increasing testing accessibility in underserved communities.(39)
Our comprehensive examination of small-area racial/ethnic disparities across California highlights that in every region of the state, Latino populations have persistently and disproportionately higher risk exposures, lower testing, and higher test positivity and case rates. Action to address these disparities is required in all parts of the state. Within regions and counties, our study indicates that it may be possible to identify more localized areas in which negative outcomes are particularly concentrated and to prioritize interventions accordingly. Policies specifically designed to address disparities remain an urgent priority for California in the coming months.
Supplementary Material
Acknowledgements
This work was supported in part by a contract with the State of California (SPO No. 184726). The authors’ global work on household crowding, vulnerability, and transmission of SARSCoV- 2 is supported in part by a gift from the Wadhwani Institute for Artificial Intelligence Foundation. Marissa Reitsma is supported by Stanford’s Knight-Hennessy Scholars program. Anneke Claypool is supported by the Stanford Interdisciplinary Graduate Fellowship. Reitsma, Claypool, Joshua Salomon, and Jeremy Goldhaber-Fiebert are supported by theStanford Clinical and Translational Science Award to Spectrum (UL1TR003142). Salomon is supported by funding from the Centers for Disease Control and Prevention though the Council of State and Territorial Epidemiologists (NU38OT000297-02). Salomon and Goldhaber-Fiebert are supported by the National Institute on Drug Abuse (3R37DA01561217S1). This article does not necessarily represent the views of the Centers for Disease Control and Prevention, Council of State and Territorial Epidemiologists, National Institutes of Health, or other funders. The authors acknowledge help from SCCOSMO consortium, whose members include Fernando Alarid-Escudero, Jason Andrews, Jose Manuel Cardona Arias, Liz Chin, Anneke Claypool, Hugo Berumen Covarrubias, Ally Daniels, Mariana Fernandez, Hannah Fung,Zulema Garibo, Jeremy Goldhaber- Fiebert, Valeria Gracia, Alex Holsinger, Erin Holsinger, Radhika Jain, Neesha Joseph, Natalia Kunst, Elizabeth Long, Andrea Luviano, Regina Isabel Medina Rosales, Marcela Pomar Ojeda, Yadira Peralta, Lea Prince, Marissa Reitsma, Neil Rens, Tess Ryckman, Joshua Salomon, David Studdert, and Hirvin Azael Diaz Zepeda. They also acknowledge help from the California Department of Public Health COVID Sciences Branch Epi and Data Teams.
References
- 1.Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The Impact Of The COVID-19 Pandemic On Hospital Admissions In The United States. Health Aff (Millwood). 2020;39(11):2010–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macias Gil R, Marcelin JR, Zuniga-Blanco B, Marquez C, Mathew T, Piggott DA. COVID-19 Pandemic: Disparate Health Impact on the Hispanic/Latinx Population in the United States. J Infect Dis. 2020;222(10):1592–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webb Hooper M, Napoles AM, Perez-Stable EJ. COVID-19 and Racial/Ethnic Disparities. JAMA. 2020;323(24):2466–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVID-19 Racial and Ethnic Health Disparities: Center for Disease Control and Prevention; 2020. [Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/index.html.
- 6.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–2. [DOI] [PubMed] [Google Scholar]
- 7.Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, et al. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J Racial Ethn Health Disparities. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benitez JA, Courtemanche C, Yelowitz A. Racial and Ethnic Disparities in COVID-19: Evidence from Six Large Cities. Journal of Economics, Race, and Policy. 2020;3(4):243–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N Engl J Med. 2020;382(26):2534–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gu T, Mack JA, Salvatore M, Prabhu Sankar S, Valley TS, Singh K, et al. Characteristics Associated With Racial/Ethnic Disparities in COVID-19 Outcomes in an Academic Health Care System. JAMA Network Open. 2020;3(10):e2025197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubin-Miller L, Alban C, Artiga S, Sullivan S. COVID-19 Racial Disparities in Testing, Infection, Hospitalization, and Death: Analysis of Epic Patient Data. Kaiser Family Foundation; 2020September16, 2020. [Google Scholar]
- 12.Coronavirus in the U.S.: Latest Map and Case Count: The New York Times; 2020. [Available from: https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html.
- 13.Tracking COVID-19 in California: Official California State Government Website; 2021. [updated March 7, 2021. Available from: https://covid19.ca.gov/state-dashboard/.
- 14.Azar KMJ, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities In Outcomes Among COVID-19 Patients In A Large Health Care System In California. Health Aff (Millwood). 2020;39(7):1253–62. [DOI] [PubMed] [Google Scholar]
- 15.Chamie G, Marquez C, Crawford E, Peng J, Petersen M, Schwab D, et al. SARS-CoV-2 Community Transmission disproportionately affects Latinx population during Shelter-in-Place in San Francisco. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore JT, Ricaldi JN, Rose CE, Fuld J, Parise M, Kang GJ, et al. Disparities in Incidence of COVID-19 Among Underrepresented Racial/Ethnic Groups in Counties Identified as Hotspots During June 5–18, 2020 – 22 States, February-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1122–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chowkwanyun M, Reed AL Jr. Racial Health Disparities and Covid-19 - Caution and Context. N Engl J Med. 2020;383(3):201–3. [DOI] [PubMed] [Google Scholar]
- 18.Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedon JC. The Structural and Social Determinants of the Racial/Ethnic Disparities in the U.S. COVID-19 Pandemic. What’s Our Role? Am J Respir Crit Care Med. 2020;202(7):943–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McLaughlin JM, Khan F, Pugh S, Angulo FJ, Schmidt HJ, Isturiz RE, et al. County-Level Predictors of COVID-19 Cases and Deaths in the United States: What Happened, and Where Do We Go from Here? Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selden TM, Berdahl TA. COVID-19 And Racial/Ethnic Disparities In Health Risk, Employment, And Household Composition. Health Aff (Millwood). 2020;39(9):1624–32. [DOI] [PubMed] [Google Scholar]
- 21.Chang S, Pierson E, Koh PW, Gerardin J, Redbird B, Grusky D, et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2020. [DOI] [PubMed] [Google Scholar]
- 22.Dingel JI, Neiman B. How Many Jobs Can be Done at Home? [White Paper]. Becker Friedman Institute For Economics at UChicago: University of Chicago; 2020June2020. [Google Scholar]
- 23.Sehgal AR, Himmelstein DU, Woolhandler S. Feasibility of Separate Rooms for Home Isolation and Quarantine for COVID-19 in the United States. Ann Intern Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams DR, Cooper LA. COVID-19 and Health Equity-A New Kind of “Herd Immunity”. JAMA. 2020;323(24):2478–80. [DOI] [PubMed] [Google Scholar]
- 25.Bailey ZD, Feldman JM, Bassett MT. How Structural Racism Works — Racist Policies as a Root Cause of U.S. Racial Health Inequities. New England Journal of Medicine. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ogedegbe G, Ravenell J, Adhikari S, Butler M, Cook T, Francois F, et al. Assessment of Racial/Ethnic Disparities in Hospitalization and Mortalilty in Patients with Covid-19 in New York City. JAMA Network Open. 2020;3(12):e2026881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 28.Ruggles S, Flood S, Goeken R, Grover J, Meyer E, Pacas J, et al. IPUMS USA: Version 10.0 2014–2018 American Community Survey 5-Year Dataset [Available from: 10.18128/D010.V10.0. [DOI] [Google Scholar]
- 29.Reitsma MB, Salomon JA, Goldhaber-Fiebert JD. Mapping Inequality in SARS-CoV-2 Household Exposure and Transmission Risk in the USA. J Gen Intern Med. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Institute L. SOC Codes for CISA Critical Infrastructure Workers [Available from: https://www.lmiontheweb.org/more-than-half-of-u-s-workers-in-critical-occupations-in-the-fight-against-covid-19/.
- 31.Boyd RW, Lindo EG, Weeks LD, McLemore MR. Health Affairs Blog.
- 32.Blueprint for a Safer Economy: Equity Focus: California State Department of Health; [Available from: https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/CaliforniaHealthEquityMetric.aspx.
- 33.Figueroa JF, Wadhera RK, Lee D, Yeh RW, Sommers BD. Community-Level Factors Associated With Racial And Ethnic Disparities In COVID-19 Rates In Massachusetts. Health Aff (Millwood). 2020;39(11):1984–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schneider D, Harknett K. Essential and Vulnerable: Service-Sector Workers and Paid Sick Leave. The Shift Project: Harvard Kennedy School; 2020. [Google Scholar]
- 35.Ross K Planting Seeds: Food & Farming News from CDFA [Internet]: California Department of Food and Agriculture. 2020. Available from: https://plantingseedsblog.cdfa.ca.gov/wordpress/?p=21915. [Google Scholar]
- 36.COVID-19 Information for Agricultural Workers: Labor & Workforce Development Agency; 2020. [Available from: https://www.labor.ca.gov/coronavirus2019/campo/english/.
- 37.COVID-19 Guidance for Immigrant Californians Listos California: Governor’s Office of Emergency Services; 2020. [Available from: https://www.listoscalifornia.org/wp-content/uploads/2020/07/LISTOS_COVID_19_immigrant_guidance_EN_dAf.pdf.
- 38.Communications Toolkits: California Department of Public Health; 2020. [Available from: https://www.cdph.ca.gov/Programs/OPA/Pages/Communications-Toolkits/Communications-Toolkit.aspx.
- 39.Playbook to Stand Up Community-Based Collection Sites. California Department of Public Health Valencia Branch Laboratory; 2020December2, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.