Abstract
Objective
Lipotoxic hepatocyte injury is a primary event in non-alcoholic steatohepatitis (NASH), but the mechanisms of lipotoxicity are not fully defined. Sphingolipids and free cholesterol (FC) mediate hepatocyte injury, but their link in NASH has not been explored. We examined the role of free cholesterol and sphingomyelin synthases (SMSs) that generate sphingomyelin (SM) and diacylglycerol (DAG) in hepatocyte pyroptosis, a specific form of programmed cell death associated with inflammasome activation, and NASH.
Design
Wild-type C57BL/6J mice were fed a high fat and high cholesterol diet (HFHCD) to induce NASH. Hepatic SMS1 and SMS2 expressions were examined in various mouse models including HFHCD-fed mice and patients with NASH. Pyroptosis was estimated by the generation of the gasdermin-D N-terminal fragment. NASH susceptibility and pyroptosis were examined following knockdown of SMS1, protein kinase Cδ (PKCδ), or the NLR family CARD domain-containing protein 4 (NLRC4).
Results
HFHCD increased the hepatic levels of SM and DAG while decreasing the level of phosphatidylcholine. Hepatic expression of Sms1 but not Sms2 was higher in mouse models and patients with NASH. FC in hepatocytes induced Sms1 expression, and Sms1 knockdown prevented HFHCD-induced NASH. DAG produced by SMS1 activated PKCδ and NLRC4 inflammasome to induce hepatocyte pyroptosis. Depletion of Nlrc4 prevented hepatocyte pyroptosis and the development of NASH. Conditioned media from pyroptotic hepatocytes activated the NOD-like receptor family pyrin domain containing 3 inflammasome (NLRP3) in Kupffer cells, but Nlrp3 knockout mice were not protected against HFHCD-induced hepatocyte pyroptosis.
Conclusion
SMS1 mediates hepatocyte pyroptosis through a novel DAG-PKCδ-NLRC4 axis and holds promise as a therapeutic target for NASH.
Keywords: hepatocyte, immunology in hepatology, nonalcoholic steatohepatitis, lipid mediators
Significance of this study.
What is already known on this subject?
Lipotoxic injury of hepatocytes may be a primary lesion that triggers the development of non-alcoholic steatohepatitis (NASH).
Gasdermin D-driven pyroptosis is found in mouse models of NASH and patients with NASH.
What are the new findings?
Expression of sphingomyelin synthase 1 (SMS1), an enzyme that generates sphingomyelin (SM) and diacylglycerol (DAG) from de novo-synthesised ceramide, was increased in the liver of multiple murine models of NASH and patients with NASH.
Free cholesterol induced SMS1 expression in hepatocytes. DAG produced by SMS1 activated protein kinase Cδ (PKCδ) and NLR family CARD domain-containing protein 4 (NLRC4) inflammasome to induce hepatocyte pyroptosis.
How might it impact on clinical practice in the foreseeable future?
Our findings underscore a novel SMS1-DAG-PKCδ-NLRC4 axis that may be of potential relevance for the treatment of NASH.
Introduction
Non-alcoholic steatohepatitis (NASH), an advanced stage of non-alcoholic fatty liver disease, is an important cause of morbidity and mortality worldwide and a leading cause of end-stage liver disease.1 Despite recent progress, the mechanisms involved in the transition from hepatic steatosis to NASH remain elusive.2 3 Lipotoxic injury of hepatocytes may be a primary event in the development of NASH and can contribute to inflammation, leading to hepatic fibrosis.4 However, the nature and mechanisms of lipotoxicity in NASH are not fully understood.
Apoptosis is a non-lytic form of death mediated by caspases and confers minimal effects on nearby cells. In contrast, programmed necrotic cell death (ie, necroptosis and pyroptosis) releases immunostimulatory intracellular components due to the rupture of cell membranes and induce inflammation.5 Necroptosis is activated by the necrosome, which consists of the kinases receptor-interacting serine/threonine-protein kinase (RIPK) 1 and RIPK3 and the pseudokinase mixed linkage kinase domain-like protein (MLKL), and is known to occur in human and experimental NASH.6 Pyroptosis occurs predominantly in professional phagocytes—macrophages, monocytes and dendritic cells—and plays a major role in the clearance of bacteria from these cells. Moreover, pyroptosis has also been described in hepatocytes.7 Gasdermin-D and its N-terminal fragment (GSDMD-N) is a key player in pyroptotic cell death, whose levels increase in human and experimental NASH.8 Pyroptosis is initiated by either caspase-1 or caspase-11.9 Caspase-1 is activated by several inflammasomes, including the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome, which results in pyroptosis and the maturation and secretion of proinflammatory cytokines such as interleukin-1β (IL-1β) and IL-18.10 In the liver, NLRP3 inflammasome is prominently expressed in hepatic macrophages (Kupffer cells) with moderate expression in hepatic stellate cells (HSCs), and IL-1β produced by NLRP3 inflammasome promotes the proliferation and transdifferentiation of HSCs to induce liver fibrosis.11 Interestingly, knock-in mice with global or myeloid-specific Nlrp3 overexpression underwent caspase-1-dependent hepatocyte pyroptosis, liver inflammation and fibrosis.7 However, the role of NLRP3 inflammasome activation in hepatocyte pyroptosis is yet to be elucidated. NLR family CARD domain-containing protein 4 (NLRC4) inflammasome, which senses bacterial flagellin and the components of bacterial secretion, has been shown to cause macrophage pyroptosis and is activated by protein kinase C (PKC) δ.12 13 Moreover, NLRC4 inflammasome activation has also been described in obesity-associated breast cancer progression and diabetic nephropathy.14 15 Yet, the specific role of NLRC4 inflammasome in NASH remains largely unknown.
Sphingolipids are ubiquitous building blocks of eukaryotic cell membranes that regulate a wide range of cellular processes including immunity, inflammation and metabolic diseases.16 In the liver, increased intracellular ceramide, the prototype sphingolipid and the precursor of complex sphingolipids, induces lipotoxic hepatocellular cell death by multiple mechanisms.17 18 Although ceramide can be generated by de novo synthesis in the endoplasmic reticulum from palmitoyl-CoA and serine or sphingomyelin (SM) hydrolysis by sphingomyelinases (SMases), ceramide can also be converted to SM and diacylglycerol (DAG) by sphingomyelin synthases (SMSs). DAG produced by SMSs can activate PKC,19 which in turn phosphorylates and activates a wide range of targets.
In this study, we investigated the role of SMS1, an enzyme that links de novo-synthesised ceramide to SM synthesis and DAG generation,20 in hepatocyte pyroptosis and the pathogenesis of NASH. Our study identifies SMS1 as a novel player in the hepatocyte pyroptosis in NASH via the DAG-PKCδ-NLRC4 axis and delineates a previously unrecognised role of NLRC4 inflammasome in metabolic liver disease.
Experimental procedures
The detailed methods are provided in online supplemental data.
gutjnl-2020-322509supp001.pdf (918.9KB, pdf)
Results
SMS1 expression is increased in the livers of HFHCD-fed mice
Cholesterol has emerged as the key player in NASH development through multiple pathological mechanisms, including the trafficking of free cholesterol (FC) to mitochondria.21 Moreover, hepatic FC has been shown to accumulate in obese diabetic mice22 and patients with NASH,23 24 and pharmacological lowering of cholesterol reversed NASH in obese, diabetic mice with metabolic syndrome.25 However, the link between cholesterol and sphingolipid metabolism in NASH has not been explored. Thus, we tested this possibility using a dietary cholesterol-driven murine model of NASH.
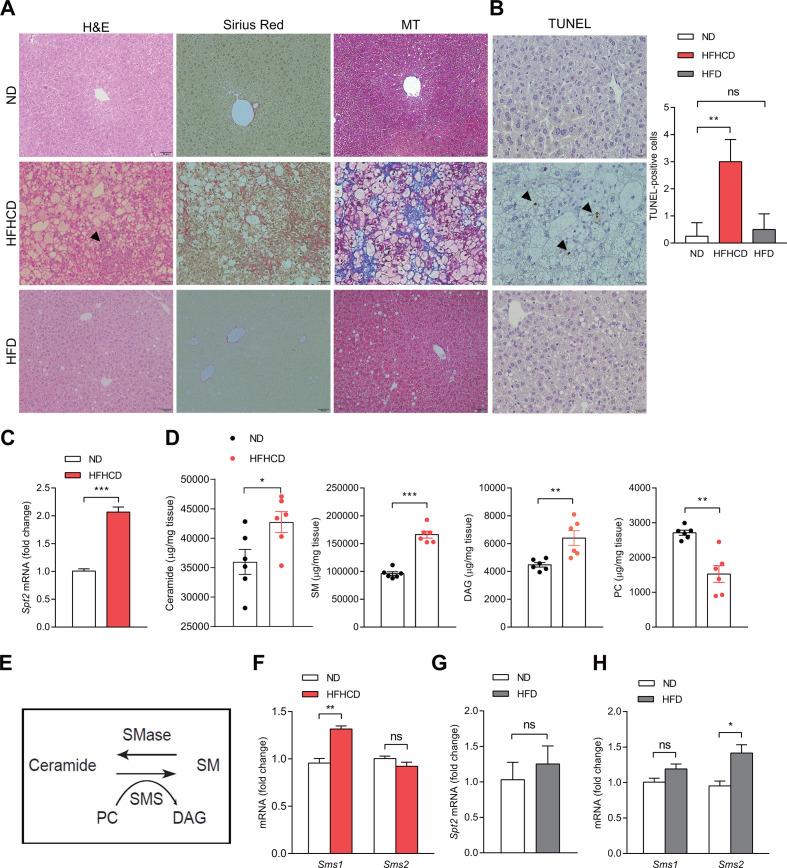
Feeding male C57BL/6J mice with high fat, high cholesterol (2.5%) diet (HFHCD) for 12 weeks induced NASH, whereas mice fed a high fat diet (HFD) developed simple steatosis without significant inflammation and fibrosis (figure 1A).26 Terminal deoxynucleotidyl transferase-mediated dUTP nick‐end labelling (TUNEL) staining showed that apoptosis is evident in HFHCD-fed mice but not in HFD-fed mice (figure 1B). HFHCD significantly increased the expression of serine palmitoyltransferase subunit 2 (Spt2), a key player in sphingolipid biosynthesis (figure 1C).20 HFHCD feeding significantly increased the levels of ceramide, SM and DAG and decreased the level of phosphatidylcholine (PC) (figure 1D and online supplemental figure S1).
Figure 1.
Hepatic Sms1 expression in murine NASH models. Liver tissues from mice fed control diet (ND), HFHCD or HFD for 12 weeks showing representative H&E, Sirius Red and MT staining. Scale bar, 50 µM. Arrowhead indicates inflammatory foci (A) and TUNEL staining. TUNEL staining positivity was observed in hepatocytes (arrowhead). Scale bar, 20 µm. The graph represents the percentage of TUNEL-positive cells in each group (B). (C) Relative mRNA expression of Spt2 in ND-fed or HFHCD-fed mice. (D) Levels of hepatic ceramide, SM, DAG and PC. (E) Schematic figure depicting the action of the SMSs. (F) Relative mRNA expression of Sms1 and Sms2. (G, H) Relative mRNA expression of Spt2, Sms1 and Sms2 in mice fed ND or HFD. Data are presented as mean±SEM (n=6). *p<0.05, **p<0.01 and ***p<0.001 vs control mice. DAG, diacylglycerol; HFD, high fat diet; HFHCD, high fat, high cholesterol diet; ns, not significant; PC, phosphatidylcholine; SM, sphingomyelin; TUNEL, terminal deoxynucleotidyl transferase-mediated dUTP nick‐end labelling.
As SMSs use ceramide and PC as substrates to produce SM and DAG (figure 1E), we hypothesised that increased SM and DAG levels with a concomitant decrease in PC may reflect an increased expression in the SMSs. Feeding mice HFHCD significantly increased the hepatic expression of SMS1 but not Sms2 (figure 1F and online supplemental figure S2A). In contrast, HFD feeding increased the hepatic expression of Sms2, but had no effect on the expression of Spt2 and SMS1 (figure 1G, H and online supplemental figure S2B). Collectively, these findings show that HFHCD feeding upregulates the expression of SMS1.
FC induces SMS1 expression
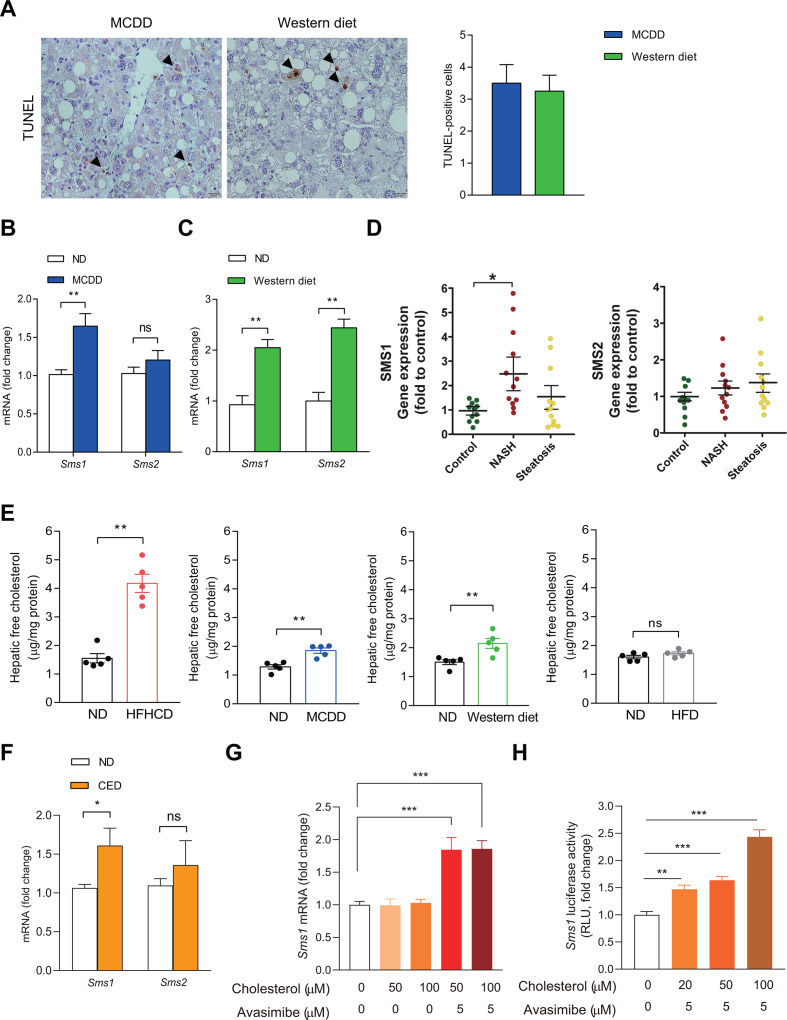
We next examined the expression of hepatic SMSs in other models of NASH induced by the methionine and choline-deficient diet (MCDD) and Western diet (enriched with fat, cholesterol and fructose).27 TUNEL staining showed increased hepatocellular apoptosis in MCDD and Western diet-fed mice (figure 2A).
Figure 2.
FC induces Sms1 expression in hepatocytes. (A) TUNEL staining in the liver sections following MCDD (8 weeks) or Western diet (16 weeks). Arrowheads show TUNEL positive hepatocytes, which are quantitated in the graph. Scale bar, 20 µm. (B, C) mRNA expression of Sms1 and Sms2 in the livers of mice fed MCDD (B) or Western diet (C) (n=7). (D) Hepatic mRNA expression of SMS1 and SMS2 in liver samples of patients with NASH/cirrhosis and subjects with steatosis (n=12). Surgical specimens of donor livers were used as controls (n=11). (E) Hepatic FC levels of mice fed ND, HFHCD, MCDD, Western diet or HFD (n=5). (F) mRNA expression of Sms1 and Sms2 in the livers of mice fed ND or CED for 2 days (n=7). (G) AML12 cells were treated with cholesterol with Avasimibe for 2 hours at the indicated dose to determine Sms1 mRNA expression (n=4). (H) AML12 cells were transfected with mouse Sms1 promoter-Luc to determine Sms1 transcriptional activity. After 48 hours of transfection, cells were treated with vehicle or cholesterol with Avasimibe for 3 hours (n=6). Data are presented as mean±SEM *p< 0.05, **p<0.01 and ***p<0.001 vs control. CED, cholesterol-enriched diet; FC, free cholesterol; HFD, high fat diet; HFHCD, high fat, high cholesterol diet; MCDD, methionine and choline-deficient diet; ns, not significant; TUNEL, terminal deoxynucleotidyl transferase-mediated dUTP nick‐end labelling.
Administration of MCDD and Western diet significantly increased the expression of SMS1, similar to HFHCD feeding (figure 2B, C and online supplemental figure S2C, D), suggesting that SMS1 induction is a characteristic feature of NASH independent of obesity. Intriguingly, Western diet also increased the expression of Sms2 (figure 2C). In addition, samples from patients with NASH/cirrhosis undergoing liver transplantation exhibited a higher expression of SMS1 but not of SMS2 (figure 2D), and this result was also reflected at the protein level (online supplemental figure S2E). There was a trend for a relationship between SMS1 expression and the hepatic FC levels in the NASH/cirrhosis group, with a weaker correlation with body mass index (data not shown). Moreover, the expression of SMS1 did not change in liver specimens from subjects with steatosis (figure 2D). Thus, these findings suggest that higher hepatic SMS1 expression may be a common feature of NASH. Although previous studies28 29 and our findings in mice fed HFD (figure 1H) showed that Sms2 is associated with hepatic steatosis, SMS2 expression did not significantly change in the subjects with steatosis (figure 2D). Its relevance in human steatosis should be confirmed by using a larger cohort of subjects.
Cholesterol and SM are coenriched in the same membrane domains, and their molar ratio is tightly regulated to maintain membrane properties and signalling pathways.30 31 We thus examined whether increased FC levels induce the expression of SMS1. As seen, the levels of hepatic FC were increased in mice fed HFHCD, MCDD or Western diet, but not in those fed HFD (figure 2E). To further test the direct link between hepatic FC and SMS1 expression, we used two different approaches. First, we fed mice a cholesterol-enriched diet (CED) supplemented with sodium cholate to sustain hepatic FC,32 which increased hepatic Sms1 expression but not Sms2 (figure 2F). In addition, treatment of AML12 hepatocytes with water-soluble cholesterol and Avasimibe, an acyl-CoA cholesterol acyltransferase inhibitor that maintains cholesterol in its unesterified form,33 significantly increased Sms1 expression (figure 2G). Moreover, Sms1 promoter activity significantly increased by cholesterol and Avasimibe, suggesting that FC induces the upregulation of Sms1 at the transcriptional level (figure 2H). Taken together, these results suggest that the accumulation of FC stimulates the transcriptional expression of Sms1 in NASH.
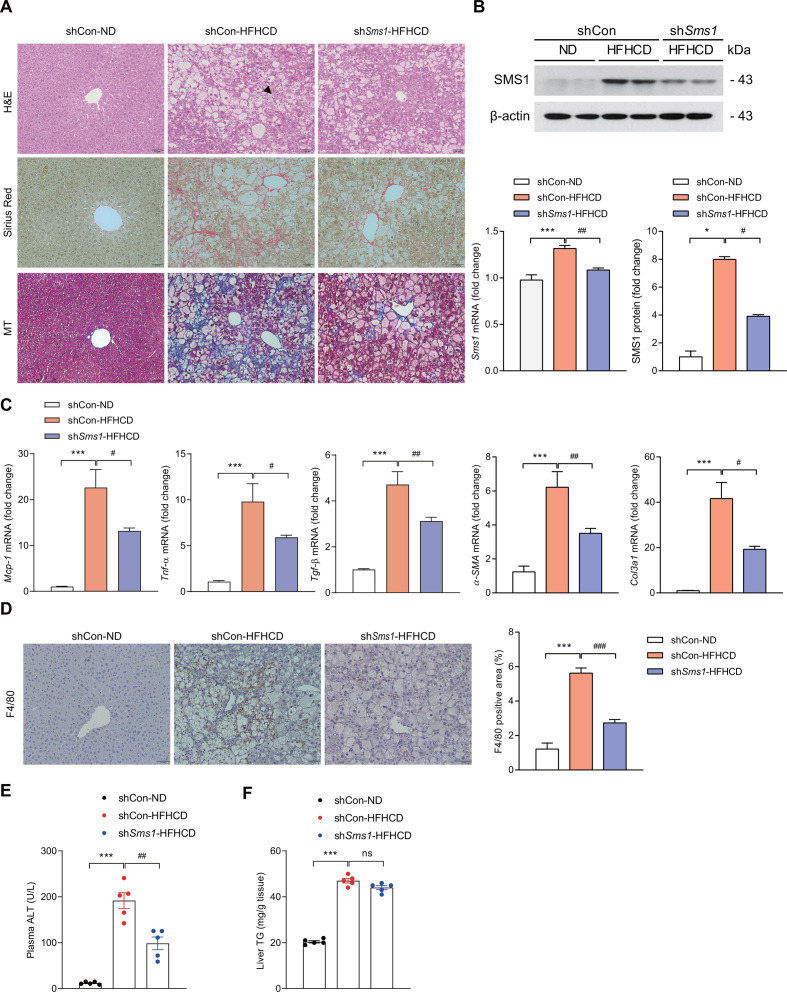
SMS1 knockdown prevents NASH development
To further elucidate the role of SMS1 in NASH, we examined the effect of shRNA-mediated knockdown of Sms1 in HFHCD-fed mice. Sms1 knockdown ameliorated HFHCD-induced liver inflammation and fibrosis (figure 3A, B), lowered expression of monocyte chemoattractant protein-1 (Mcp-1), tumour necrosis factor-α (Tnf-α), transforming growth factor-β1 (Tgf-β1), α-smooth muscle actin (α-Sma) and collagen type III α1 (Col3a1) (figure 3C and online supplemental figure S3A). Furthermore, HFHCD-induced increase in α-SMA immunoreactivity was decreased following Sms1 knockdown (online supplemental figure S3A), with similar findings observed for F4/80 immunohistochemistry (figure 3D). Knockdown of Sms1 also decreased the level of serum alanine aminotransferase (ALT) (figure 3E), but did not significantly change the hepatic triglyceride levels in HFHCD-fed mice (figure 3F). Hence, SMS1 mediates diet-induced liver injury, inflammation and fibrosis, but not steatosis.
Figure 3.
Depletion of SMS1 prevents NASH development. Mice were injected with AAV carrying control shRNA (shCon) or Sms1-specific shRNA (shSms1) and then fed ND or HFHCD for 12 weeks. (A) Representative H&E, Sirius Red and MT liver staining. Scale bar, 50 µM. Arrowhead indicates inflammatory foci. (B) Relative mRNA expression, and Western blot of SMS1. (C) mRNA expression of Mcp-1, Tnf-α, Tgf-β1, α-Sma and Col3a1. (D) Immunohistochemical staining and quantitative analysis of F4/80-positive area in the liver. (E) Plasma ALT level. (F) Liver TG contents. Data are presented as mean±SEM of mice (n=5). *p<0.05 and ***p<0.001 vs control mice. #p<0.05, ##p<0.01, ###p<0.001 vs shCon-HFHCD mice.HFHCD, high fat, high cholesterol diet; ns, not significant; SMS, sphingomyelin synthase; TG, triglyceride.
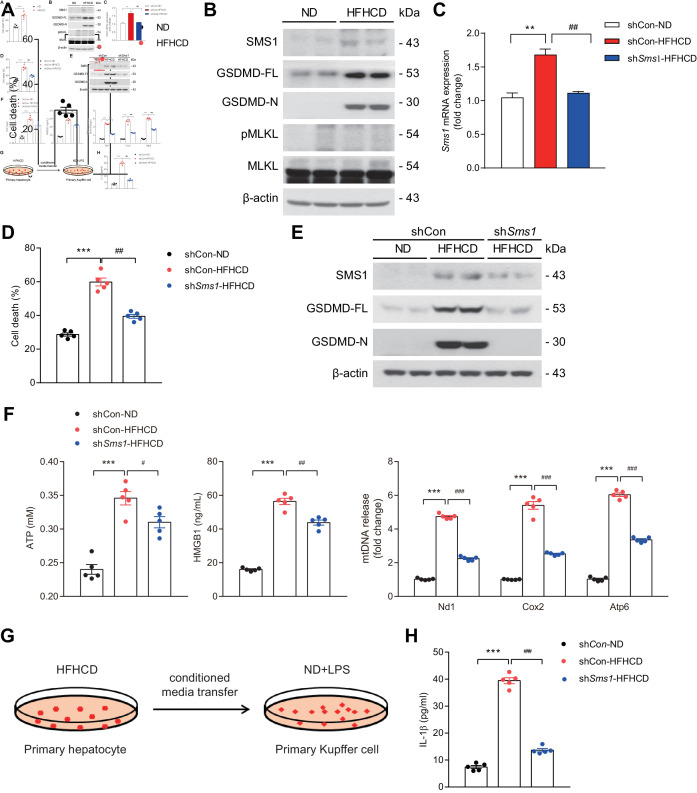
SMS1 mediates diet-induced hepatocyte pyroptosis
We next examined whether SMS1 mediates hepatocyte pyroptosis. Hepatocytes isolated from HFHCD-fed mice (HFHCD hepatocytes) exhibited increased SMS1 protein levels and enhanced release of lactate dehydrogenase (LDH) in the supernatant (figure 4A, B). Moreover, HFHCD hepatocytes had increased levels of GSDMD-N, a key player in pyroptotic cell death in NASH;34 however, the level of phosphorylation of MLKL, a marker of necroptosis,5 did not change (figure 4B). These data collectively indicate that pyroptosis specifically occurs in HFHCD hepatocytes. Importantly, knockdown of Sms1 significantly decreased cell death as reflected by lower LDH release in the supernatant (figure 4C, D) and the generation of GSDMD-N in HFHCD hepatocytes (figure 4E). These findings support a causal link between SMS1 and HFHCD-induced hepatocyte pyroptosis.
Figure 4.
SMS1 causes hepatocyte pyroptosis. (A) Cell death measured by LDH level in the media of primary hepatocytes isolated from mice fed HFHCD (4 weeks). (B) Representative Western blots of SMS1, GSDMD-FL, GSDMD-N and MLKL. (C–E) Mice were infected with AAV carrying control shRNA (shCon) or Sms1-specific shRNA (shSms1) and then fed with ND or HFHCD (4 weeks) to determine mRNA expression of Sms1 in the hepatocyte (C), cell death by LDH release (D) and Western blots of SMS1, GSDMD-FL and -N (E). (F–H) DAMPs released from pyroptotic hepatocytes activate NLRP3 inflammasome in Kupffer cells. (F) Levels of ATP, HMGB1 and mtDNA in the supernatant. (G, H) Primary hepatocyte-conditioned media was transferred to primary Kupffer cells primed with 10 ng/ml of LPS for 4 hours (G) to determine IL-1β in the culture supernatants of primary hepatocytes (H). Data are presented as mean±SEM (n=5). **p< 0.01 and ***p<0.001 vs control mice. #p<0.05, ##p<0.01 and ###p<0.001 vs shCon-HFHCD mice. DAMPs, damage-associated molecular pattern molecules; GSDMD-FL, full-length gasdermin D; GSDMD-N, N-terminal fragment of gasdermin-D; HFHCD, high fat, high cholesterol diet; HMGB1, high mobility group protein box 1; LDH, lactate dehydrogenase; LPS, lipopolysaccharides; MLKL, mixed linkage kinase domain-like protein; NLRC4, NLR family CARD domain-containing protein 4; NLRP3, NOD-like receptor family pyrin domain containing 3; SMS, sphingomyelin synthase.
DAMPs released from pyroptotic hepatocytes activate NLRP3 inflammasome in Kupffer cells in a SMS1-dependent manner
As damage-associated molecular pattern molecules (DAMPs) activate NLRP3 inflammasome,35 we examined the levels of DAMPs in HFHCD hepatocytes. The levels of ATP, high mobility group protein box 1 (HMGB1), and mitochondrial DNA (mtDNA) in the supernatants of pyroptotic HFHCD hepatocytes were significantly higher than those of control hepatocytes, and this effect was decreased on Sms1 knockdown (figure 4F). We then examined whether the DAMPs released from pyroptotic HFHCD hepatocytes activated NLRP3 inflammasome in Kupffer cells isolated from control mice pretreated with lipopolysaccharides (LPS) (figure 4G). As seen, the conditioned media from pyroptotic hepatocytes activated NLRP3 inflammasome in LPS-primed Kupffer cells, as evidenced by the increase in IL-1β levels (figure 4H) and this effect was suppressed on hepatic Sms1 depletion by shRNA treatment (figure 4H).
Plasma from mice and patients with NASH has been reported to contain high levels of extracellular vesicles (EVs) containing mtDNA and damaged organelles (ie, mitochondria) released from hepatocytes.36 37 Thus, we examined the presence of EVs from hepatocytes of HFHCD fed mice. As seen, the amount of mtDNA in the EVs was significantly increased in the supernatants of HFHCD hepatocytes and was significantly decreased by Sms1 depletion (online supplemental figure S4). These findings suggest that SMS1 plays a key role in the release of DAMPs that include mtDNA in the EVs from dying hepatocytes.
NLRC4-dependent pyroptosis in hepatocytes from NASH animals
The basal expression level of NLCR4 in hepatocytes is negligible compared with those in non-parenchymal cells and is minimally induced in cholestatic liver disease;38 therefore, we first examined the expression of NLRC4 in hepatocytes from HFHCD-fed mice. As seen, the mRNA levels of NLRC4 were significantly higher in both isolated hepatocytes and liver extracts from HFHCD-fed mice, with similar findings observed for NLRP3 (online supplemental figure S5). The increased expression of both NLRP3 and NLRC4 in HFHCD-hepatocytes was also reflected at the protein level and in the phosphorylation of NLRC4 (figure 5A). Interestingly, Sms1 knockdown did not affect NLRP3 expression but abrogated the HFHCD-mediated NLRC4 phosphorylation (figure 5A). Moreover, knockdown of Nlrc4 did not significantly affect hepatic steatosis but prevented NASH (figure 5B, C and online supplemental figures S3B and S6) and significantly decreased gasdermin-D activation reflected by the lower level of the GSDMD-N fragment and hepatocyte death (figure 5D, E). Furthermore, supernatant from hepatocytes of HFHCD-fed mice following Nlrc4 knockdown induced significantly lower production of IL-1β from LPS-pretreated Kupffer cells compared with hepatocytes from HFHCD-fed mice treated with control shRNA (figure 5F). As DAG is generated from SMS and is known to activate PKCδ, we explored the putative link between SMS1 and PKCδ activation. PKCδ phosphorylation was higher in hepatocytes from HFHCD-fed mice, but not in HFHCD-fed mice with Sms1 knockdown (figure 5G). Furthermore, knockdown of Pkcδ in HFHCD-fed mice by shRNA prevented NASH (online supplemental figure S3C) and significantly decreased the phosphorylation of NLRC4 (figure 5H, I). These findings underscore a causal link between SMS1 and NLRC4 in inducing hepatocyte pyroptosis through PKCδ activation.
Figure 5.
NLRC4-dependent pyroptosis in hepatocytes from HFHCD-fed mice through PKCδ. (A–F) Hepatocytes from mice infected with AAV carrying control shRNA (shCon), Sms1-specific shRNA (shSms1) (A) or Nlrc4-specific shRNA (shNlrc4) (B–F) and fed ND or HFHCD for 12 weeks (B, C) or 4 weeks (A, D–G) to determine Western blots for NLRC4 and NLRP3 (A). (B) Representative H&E and MT staining. Scale bar, 50 µM. Arrowhead indicates inflammatory foci. (C) Liver TG. (D) Representative Western blots of GSDMD-FL and GSDMD-N. (E) Cell death by LDH level. (F) IL-1β from hepatocyte-conditioned media transferred to Kupffer cells primed with 10 ng/ml of LPS for 4 hours. (G, H) Representative Western blots of PKCδ (G) and NLRC4 (H) of hepatocytes from mice infected with AAV carrying control shRNA (shCon), Sms1-specific shRNA (shSms1) (G) or Pkcδ-specific shRNA (shPkcδ) (H). (I) mRNA expression and protein levels of PKCδ. Data are presented as mean±SEM (n=5). *p<0.05, **p<0.01 and ***p<0.001 vs control mice. #p<0.05, ##p<0.01 vs shCon-HFHCD mice. GSDMD-FL, full-length gasdermin D; GSDMD-N, N-terminal fragment of gasdermin-D; HFHCD, high fat, high cholesterol diet; LDH, lactate dehydrogenase; NLRC4, NLR family CARD domain-containing protein 4; NLRP3, NOD-like receptor family pyrin domain containing 3; ns, not significant; PKC, protein kinase C; TG, triglyceride.
SMS1 overexpression induces hepatocyte pyroptosis
To further demonstrate that SMS1 contributes to NLRC4-mediated hepatocyte pyroptosis, we explored the role of SMS1 overexpression in hepatocyte pyroptosis. SMS1 overexpression into AML12 hepatocytes using lentiviral vectors induced phosphorylation of NLRC4 and activation of gasdermin-D (online supplemental figure S7).
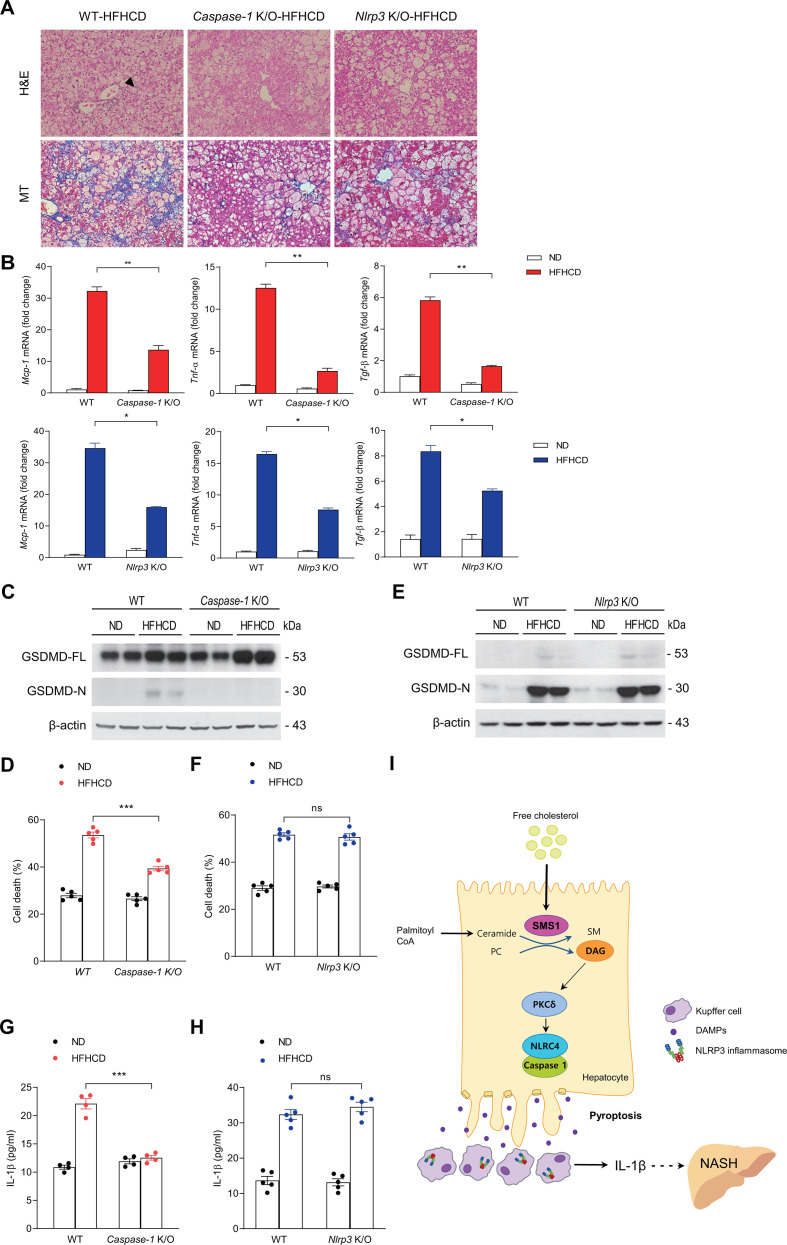
Caspase-1 but not Nlrp3 knockout mice are protected against hepatocyte pyroptosis
Considering the link between NLRP3 inflammasome and caspase-1 in liver inflammation and fibrosis,7 we investigated the role of the NLRP3-caspase-1 axis in HFHCD-induced NASH and hepatocyte pyroptosis by examining the susceptibility of Caspase-1 K/O or Nlrp3 K/O male mice (generated by the TALEN method in C57BL/6N mice).39 In line with previous findings,40 41 both Caspase-1 and Nlrp3 K/O mice were protected from HFHCD-induced hepatic inflammation and fibrosis (figure 6A, B). Moreover, hepatocytes obtained from HFHCD-fed Caspase-1 K/O mice were protected from pyroptosis (figure 6C, D). Interestingly, however, hepatocytes from HFHCD-fed Nlrp3 K/O mice showed an increased level of GSDMD activation (GSDMD-N fragment) and increased cell death, indicating that NLRP3 does not directly mediate hepatocyte pyroptosis (figure 6E, F). In line with these findings, conditioned media of hepatocytes from HFHCD-fed Caspase-1 K/O mice failed to induce IL-1β production in LPS-primed Kupffer cells from control mice (figure 6G). In contrast, conditioned media of hepatocytes from HFHCD-fed Nlrp3 K/O mice induced significant IL-1β production in LPS-primed Kupffer cells from control mice (figure 6H). These results suggest that caspase-1, but not NLRP3, is necessary for hepatocyte pyroptosis induced by HFHCD feeding.
Figure 6.
Genetic ablation of caspase-1 but not NLRP3 protects against hepatocyte pyroptosis. Caspase-1 K/O mice and Nlrp3 K/O mice were fed HFHCD for 12 weeks (A, B) or 4 weeks (C–H) to determine (A) H&E and MT staining. Scale bar, 50 µm. Arrowhead indicates inflammatory foci. (B) mRNA expression of Mcp-1, Tnf-α and Tgf-β1. Representative Western blots of GSDMD (C) and cell death (D) of hepatocytes from WT and Caspase-1 K/O mice. Representative Western blots of GSDMD-FL and GSDMD-N (E) and cell death (F) in hepatocytes of WT and Nlrp3 K/O mice. IL-1β from Caspase-1 K/O (G) or Nlrp3 K/O (H) hepatocyte-conditioned media transferred to primary Kupffer cells primed with 10 ng/ml of LPS for 4 hours. (I) Conceptual model depicting the role of SMS1, PKCδ and NLRC4 inflammasome in causing hepatocyte pyroptosis and NLRP3 inflammasome activation in Kupffer cells in the pathogenesis of NASH. Data are presented as mean±SEM (n=4-5). *p<0.05, **p<0.01 and ***p<0.001 vs WT-HFHCD mice. GSDMD-FL, full-length gasdermin D; GSDMD-N, N-terminal fragment of gasdermin-D; HFHCD, high fat, high cholesterol diet; LPS, lipopolysaccharides; NLRC4, NLR family CARD domain-containing protein 4; NLRP3, NOD-like receptor family pyrin domain containing 3; ns, not significant; SMSs, sphingomyelin synthases; WT, wild type.
Caspase-11 deletion fails to protect against hepatocyte pyroptosis or NASH development
In addition to caspase-1, caspase-11 can also induce pyroptosis by sensing cytoplasmic LPS.42 In contrast to Caspase-1 K/O mice, however, Caspase-11 K/O mice were not protected from HFHCD-induced NASH and hepatocyte pyroptosis (online supplemental figure S8), indicating that caspase-11 does not play a significant role in diet-induced NASH and hepatocyte pyroptosis. This outcome is in contrast with a recent finding that caspase-11 activated gasdermin-D in alcoholic hepatitis,43 but is consistent with the notion that caspase-1 but not caspase-11 is required for NLRC4-mediated pyroptosis in macrophages.44
Discussion
Whereas apoptosis is a non-lytic form of cell death that confers minimal effects on nearby cells, it is recognised to play a role in the NASH. It was suggested that apoptotic cells can nonetheless release selective and low levels of DAMPs, thereby triggering inflammation in specific settings.45 Accordingly, we found that apoptosis was prominent in different models of diet-induced NASH but not in mice fed HFD, which induces steatosis but not NASH. In addition, we uncover a previously unrecognised DAG-PKCδ-NLRC4 axis in NASH, which is initiated by the induction of SMS1, in both experimental and human NASH and causes hepatocyte pyroptosis.
Our study shows for the first time that NLRC4 inflammasome is activated in NASH independently of bacterial components, and that this phenomenon is downstream of PKCδ activation through SMS1 induction in hepatocytes. Previous studies showed that PKCδ was activated in the liver of MCDD-fed mice,46 but the responsible mechanism remained unknown. Our results suggest that DAG produced by SMS1 is responsible for the activation of PKCδ, as treatment with shRNA against Sms1 in HFHCD-fed mice significantly decreased the phosphorylation of PKCδ. In addition, treatment with shRNA against Pkcδ and Nlrc4 decreased the phosphorylation of NLRC4 and hepatocyte pyroptosis, respectively, indicating that the SMS1-PKCδ-NLRC4 axis is pivotal in hepatocyte pyroptosis during NASH. Importantly, Nlrp3 K/O mice were protected from NASH development, but hepatocytes from Nlrp3 K/O mice were still sensitive to diet-induced pyroptosis. These results show that NLRP3 does not have a significant role in hepatocyte pyroptosis, even though NLRP3 in Kupffer cells plays a crucial role in the progression of hepatic inflammation and fibrosis (figure 6I).41
It should be noted that the content of cholesterol in the diet used to induce NASH in mice is higher than the recommended dose in humans. Since mice are resistant to maintaining FC levels, we fed mice with this specific HFHCD for 3 months to keep cholesterol in the free form. This outcome is similar to recent findings in mice fed with a lower cholesterol-enriched HFHCD (0.2%) for 12–14 months.47 Thus, these findings indicate that feeding mice with a high CED for a short time (present study) is equivalent to feeding a moderate CED for longer periods, achieving with either approach a high level of FC in the liver. Of potential relevance, the increase in SMS1 expression in different NASH models in mice, including feeding the HFHCD for 12 weeks, was observed in patients with NASH but not steatosis.
We found that SMS1, which is present in the Golgi and is involved in SM and DAG synthesis from de novo synthesised ceramide,20 plays an important role in the pathogenesis of NASH in HFHCD-fed mice. We also show that higher FC in hepatocytes is responsible for Sms1 induction at the transcriptional level. DAG was shown to induce insulin resistance in skeletal muscle and liver,48 and hepatic DAG activation of PKCε was suggested as a key mechanism of hepatic insulin resistance, NAFLD and type 2 diabetes.49 We show that DAG produced by SMS1 induces hepatocyte pyroptosis and NASH by sequentially activating the PKCδ-NLRC4 axis. Thus, DAG produced by different pathways may activate different isoforms of PKC that can induce either hepatic steatosis/insulin resistance (PKCε) or hepatocyte pyroptosis/NASH (PKCδ).
Based on the present findings, it could be speculated that inhibition of SMS1 may be of potential relevance to prevent or slow down NASH progression. Unfortunately, there are not characterised SMS1 inhibitors, whose identification would require extensive research. Alternatively, rather than inhibiting SMS1, which would be expected to result in decreased SM levels with potential adverse effects, it may be less problematic to antagonise SMS1 downstream targets. Further research is warranted in the future to identify potential targets of this new SMS1-DAG-PKCδ-NLRC4 axis in NASH.
Acknowledgments
We thank the core facilities of the Metabolomics Core and the GEAR Core at the Convergence medicine research center (CREDIT), Asan Medical Center for the use of their shared equipment, services and expertise. We want to express our gratitude to Drs Josep Fuster, Juan Carlos Garcia-Valdecasas and Joanna Ferrer for the supply of liver samples from NASH patients undergoing liver transplantation.
Footnotes
EHK, JEY and MSK contributed equally.
Correction notice: This article has been corrected since it published Online First. The author Laura Conde de la Rosa's name has been corrected.
Contributors: EHK conceptualised the study, designed the study and wrote the manuscript. JEY designed the study, performed in vivo and in vitro experiments and wrote the manuscript. MSK designed the study, performed in vitro and molecular experiments and wrote the manuscript. J-YY and CHH performed in vivo experiments. YKC, JEJ, SEL, JYB and JSL analysed the data and participated in writing of the manuscript. COS provided critical review of liver histology. HJY and SJK measured lipid metabolite levels. ST, ESV, LCR and CG-R performed and analysed in vivo studies in mice and examined the human samples. W-IJ, SHB, AF and JCF-C critically reviewed the manuscript, provided suggestions and contributed to the discussion. I-JB generated the Nlrp3 K/O mice. K-UL and JCF-C conceptualised the study, wrote the manuscript and are responsible for the integrity of this work. All authors discussed the results and commented on the manuscript.
Funding: This study was supported by grants from the National Research Foundation of Korea (NRF), funded by the Ministry of Education, Science, and Technology, Korea (2017R1E1A1A01073206: KUL, 2017R1E1A1A01074207: EHK) and Asan Institute for Life Sciences, Korea (2018IP0557-1). We acknowledge the support from NIH grants R01 DK113592, R01 AA024206 to AEF; grants SAF2017-85877R and PID2019-1116691RB from Plan Nacional de I+D, Spain and by the CIBEREHD, Instituto de Salud Carlos III, Spain; the center grant P50AA011999 Southern California Research Center for ALPD and Cirrhosis funded by NIAAA/NIH; support from AGAUR of the Generalitat de Catalunya SGR-2017–1112 and the 'ER stress-mitochondrial cholesterol axis in obesity-associated insulin resistance and comorbidities'-Ayudas Fundación BBVA (35_2018) a Equipos de Investigación Científica 2017, the Red Nacional 2018–1 02 799 T 'Enfermedades metabólicas y cáncer' and the Fundació Marató TV3 201916-30-31.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. All data used in the manuscript are available from the corresponding author (kulee@amc.seoul.kr) on reasonable request in either raw or deidentified format, as appropriate. Reuse of the data is not permitted under normal circumstances. Detailed information on experimental protocols may also be shared on reasonable request.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Friedman SL, Neuschwander-Tetri BA, Rinella M, et al. Mechanisms of NAFLD development and therapeutic strategies. Nat Med 2018;24:908–22. 10.1038/s41591-018-0104-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology 2010;52:1836–46. 10.1002/hep.24001 [DOI] [PubMed] [Google Scholar]
- 3.Ratziu V, Goodman Z, Sanyal A. Current efforts and trends in the treatment of NASH. J Hepatol 2015;62:S65–75. 10.1016/j.jhep.2015.02.041 [DOI] [PubMed] [Google Scholar]
- 4.Machado MV, Diehl AM. Pathogenesis of nonalcoholic steatohepatitis. Gastroenterology 2016;150:1769–77. 10.1053/j.gastro.2016.02.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wallach D, Kang T-B, Dillon CP, et al. Programmed necrosis in inflammation: toward identification of the effector molecules. Science 2016;352:aaf2154. 10.1126/science.aaf2154 [DOI] [PubMed] [Google Scholar]
- 6.Afonso MB, Rodrigues PM, Carvalho T, et al. Necroptosis is a key pathogenic event in human and experimental murine models of non-alcoholic steatohepatitis. Clin Sci 2015;129:721–39. 10.1042/CS20140732 [DOI] [PubMed] [Google Scholar]
- 7.Wree A, Eguchi A, McGeough MD, et al. NLRP3 inflammasome activation results in hepatocyte pyroptosis, liver inflammation, and fibrosis in mice. Hepatology 2014;59:898–910. 10.1002/hep.26592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu B, Jiang M, Chu Y, et al. Gasdermin D plays a key role as a pyroptosis executor of non-alcoholic steatohepatitis in humans and mice. J Hepatol 2018;68:773–82. 10.1016/j.jhep.2017.11.040 [DOI] [PubMed] [Google Scholar]
- 9.Jorgensen I, Rayamajhi M, Miao EA. Programmed cell death as a defence against infection. Nat Rev Immunol 2017;17:151–64. 10.1038/nri.2016.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strowig T, Henao-Mejia J, Elinav E, et al. Inflammasomes in health and disease. Nature 2012;481:278–86. 10.1038/nature10759 [DOI] [PubMed] [Google Scholar]
- 11.Alegre F, Pelegrin P, Feldstein AE. Inflammasomes in liver fibrosis. Semin Liver Dis 2017;37:119–27. 10.1055/s-0037-1601350 [DOI] [PubMed] [Google Scholar]
- 12.Zhao Y, Yang J, Shi J, et al. The NLRC4 inflammasome receptors for bacterial flagellin and type III secretion apparatus. Nature 2011;477:596–600. 10.1038/nature10510 [DOI] [PubMed] [Google Scholar]
- 13.Qu Y, Misaghi S, Izrael-Tomasevic A, et al. Phosphorylation of NLRC4 is critical for inflammasome activation. Nature 2012;490:539–42. 10.1038/nature11429 [DOI] [PubMed] [Google Scholar]
- 14.Kolb R, Phan L, Borcherding N, et al. Obesity-associated NLRC4 inflammasome activation drives breast cancer progression. Nat Commun 2016;7:13007. 10.1038/ncomms13007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan F, Kolb R, Pandey G, et al. Involvement of the NLRC4-Inflammasome in diabetic nephropathy. PLoS One 2016;11:e0164135. 10.1371/journal.pone.0164135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maceyka M, Spiegel S. Sphingolipid metabolites in inflammatory disease. Nature 2014;510:58–67. 10.1038/nature13475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pagadala M, Kasumov T, McCullough AJ, et al. Role of ceramides in nonalcoholic fatty liver disease. Trends Endocrinol Metab 2012;23:365–71. 10.1016/j.tem.2012.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia-Ruiz C, Mato JM, Vance D, et al. Acid sphingomyelinase-ceramide system in steatohepatitis: a novel target regulating multiple pathways. J Hepatol 2015;62:219–33. 10.1016/j.jhep.2014.09.023 [DOI] [PubMed] [Google Scholar]
- 19.Hampton RY, Morand OH. Sphingomyelin synthase and PKC activation. Science 1989;246:1050. 10.1126/science.2555921 [DOI] [PubMed] [Google Scholar]
- 20.Slotte JP. Biological functions of sphingomyelins. Prog Lipid Res 2013;52:424–37. 10.1016/j.plipres.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 21.Marí M, Caballero F, Colell A, et al. Mitochondrial free cholesterol loading sensitizes to TNF- and Fas-mediated steatohepatitis. Cell Metab 2006;4:185–98. 10.1016/j.cmet.2006.07.006 [DOI] [PubMed] [Google Scholar]
- 22.Van Rooyen DM, Larter CZ, Haigh WG, et al. Hepatic free cholesterol accumulates in obese, diabetic mice and causes nonalcoholic steatohepatitis. Gastroenterology 2011;141:1393–403. 403 e1-5. 10.1053/j.gastro.2011.06.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caballero F, Fernández A, De Lacy AM, et al. Enhanced free cholesterol, SREBP-2 and StAR expression in human NASH. J Hepatol 2009;50:789–96. 10.1016/j.jhep.2008.12.016 [DOI] [PubMed] [Google Scholar]
- 24.Min H-K, Kapoor A, Fuchs M, et al. Increased hepatic synthesis and dysregulation of cholesterol metabolism is associated with the severity of nonalcoholic fatty liver disease. Cell Metab 2012;15:665–74. 10.1016/j.cmet.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Rooyen DM, Gan LT, Yeh MM, et al. Pharmacological cholesterol lowering reverses fibrotic NASH in obese, diabetic mice with metabolic syndrome. J Hepatol 2013;59:144–52. 10.1016/j.jhep.2013.02.024 [DOI] [PubMed] [Google Scholar]
- 26.Jang JE, Park H-S, Yoo HJ, et al. Protective role of endogenous plasmalogens against hepatic steatosis and steatohepatitis in mice. Hepatology 2017;66:416–31. 10.1002/hep.29039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Santhekadur PK, Kumar DP, Sanyal AJ. Preclinical models of non-alcoholic fatty liver disease. J Hepatol 2018;68:230–7. 10.1016/j.jhep.2017.10.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitsutake S, Zama K, Yokota H, et al. Dynamic modification of sphingomyelin in lipid microdomains controls development of obesity, fatty liver, and type 2 diabetes. J Biol Chem 2011;286:28544–55. 10.1074/jbc.M111.255646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Y, Dong J, Ding T, et al. Sphingomyelin synthase 2 activity and liver steatosis: an effect of ceramide-mediated peroxisome proliferator-activated receptor γ2 suppression. Arterioscler Thromb Vasc Biol 2013;33:1513–20. 10.1161/ATVBAHA.113.301498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yan N, Ding T, Dong J, et al. Sphingomyelin synthase overexpression increases cholesterol accumulation and decreases cholesterol secretion in liver cells. Lipids Health Dis 2011;10:46. 10.1186/1476-511X-10-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang S, Robinet P, Smith JD, et al. Free-cholesterol-mediated autophagy of ORMDL1 stimulates sphingomyelin biosynthesis. Autophagy 2015;11:1207–8. 10.1080/15548627.2015.1052209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solsona-Vilarrasa E, Fucho R, Torres S, et al. Cholesterol enrichment in liver mitochondria impairs oxidative phosphorylation and disrupts the assembly of respiratory supercomplexes. Redox Biol 2019;24:101214. 10.1016/j.redox.2019.101214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Llaverías G, Laguna JC, Alegret M. Pharmacology of the ACAT inhibitor avasimibe (CI-1011). Cardiovasc Drug Rev 2003;21:33–50. 10.1111/j.1527-3466.2003.tb00104.x [DOI] [PubMed] [Google Scholar]
- 34.Shi J, Zhao Y, Wang K, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 2015;526:660–5. 10.1038/nature15514 [DOI] [PubMed] [Google Scholar]
- 35.Garcia-Martinez I, Shaker ME, Mehal WZ. Therapeutic opportunities in damage-associated molecular Pattern-Driven metabolic diseases. Antioxid Redox Signal 2015;23:1305–15. 10.1089/ars.2015.6383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia-Martinez I, Santoro N, Chen Y, et al. Hepatocyte mitochondrial DNA drives nonalcoholic steatohepatitis by activation of TLR9. J Clin Invest 2016;126:859–64. 10.1172/JCI83885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eguchi A, Yan R, Pan SQ, et al. Comprehensive characterization of hepatocyte-derived extracellular vesicles identifies direct miRNA-based regulation of hepatic stellate cells and DAMP-based hepatic macrophage IL-1β and IL-17 upregulation in alcoholic hepatitis mice. J Mol Med 2020;98:1021–34. 10.1007/s00109-020-01926-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boaru SG, Borkham-Kamphorst E, Tihaa L, et al. Expression analysis of inflammasomes in experimental models of inflammatory and fibrotic liver disease. J Inflamm 2012;9:49. 10.1186/1476-9255-9-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sung YH, Baek I-J, Kim DH, et al. Knockout mice created by TALEN-mediated gene targeting. Nat Biotechnol 2013;31:23–4. 10.1038/nbt.2477 [DOI] [PubMed] [Google Scholar]
- 40.Dixon LJ, Berk M, Thapaliya S, et al. Caspase-1-mediated regulation of fibrogenesis in diet-induced steatohepatitis. Lab Invest 2012;92:713–23. 10.1038/labinvest.2012.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mridha AR, Wree A, Robertson AAB, et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol 2017;66:1037–46. 10.1016/j.jhep.2017.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kayagaki N, Warming S, Lamkanfi M, et al. Non-canonical inflammasome activation targets caspase-11. Nature 2011;479:117–21. 10.1038/nature10558 [DOI] [PubMed] [Google Scholar]
- 43.Khanova E, Wu R, Wang W, et al. Pyroptosis by caspase11/4-gasdermin-D pathway in alcoholic hepatitis in mice and patients. Hepatology 2018;67:1737–53. 10.1002/hep.29645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cerqueira DM, Pereira MSF, Silva ALN, et al. Caspase-1 but not caspase-11 is required for NLRC4-Mediated pyroptosis and restriction of infection by flagellated Legionella species in mouse macrophages and in vivo. J Immunol 2015;195:2303–11. 10.4049/jimmunol.1501223 [DOI] [PubMed] [Google Scholar]
- 45.Schwabe RF, Luedde T. Apoptosis and necroptosis in the liver: a matter of life and death. Nat Rev Gastroenterol Hepatol 2018;15:738–52. 10.1038/s41575-018-0065-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greene MW, Burrington CM, Ruhoff MS, et al. PKC{delta} is activated in a dietary model of steatohepatitis and regulates endoplasmic reticulum stress and cell death. J Biol Chem 2010;285:42115–29. 10.1074/jbc.M110.168575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang X, Coker OO, Chu ES, et al. Dietary cholesterol drives fatty liver-associated liver cancer by modulating gut microbiota and metabolites. Gut 2021;70:761–74. 10.1136/gutjnl-2019-319664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Birkenfeld AL, Shulman GI. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology 2014;59:713–23. 10.1002/hep.26672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Perry RJ, Samuel VT, Petersen KF, et al. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature 2014;510:84–91. 10.1038/nature13478 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gutjnl-2020-322509supp001.pdf (918.9KB, pdf)
Data Availability Statement
Data are available on reasonable request. All data used in the manuscript are available from the corresponding author (kulee@amc.seoul.kr) on reasonable request in either raw or deidentified format, as appropriate. Reuse of the data is not permitted under normal circumstances. Detailed information on experimental protocols may also be shared on reasonable request.