Abstract
目的
探讨游离胸肩峰动脉穿支皮瓣修复舌癌术后缺损的疗效。
方法
2010 年 5 月—2015 年 2 月,采用游离胸肩峰动脉穿支皮瓣移植修复 11 例舌癌术后缺损并行舌再造。男 9 例,女 2 例;年龄 33~72 岁,平均 52.6 岁。均为鳞状细胞癌;原发舌缘 7 例,原发舌腹 2 例,口底癌累及舌 2 例。根据国际抗癌联盟(UICC)TNM 分期:T4N0M0 3 例,T4NlM0 3 例,T3N1M0 2 例,T3N2M0 2 例,T3N0M0 1 例。病程 3~28 个月,平均 10.6 个月。肿瘤范围 6 cm×3 cm~10 cm×5 cm。术中穿支皮瓣切取范围为 7.0 cm×4.0 cm~11.0 cm×5.5 cm;厚度 0.6~1.2 cm,平均 0.8 cm;血管蒂长 6.8~9.9 cm,平均 7.2 cm。
结果
术后 11 例皮瓣均顺利成活,创面Ⅰ期愈合;供区切口均Ⅰ期愈合。患者均获随访,随访时间 12~24 个月,平均 17.2 个月。患者再造舌外形良好,吞咽及语言功能满意,随访期间肿瘤局部无复发。供区仅遗留线性瘢痕,胸大肌功能未见明显影响。
结论
胸肩峰动脉穿支皮瓣质地好,再造舌外形及功能良好,供区损伤小,是舌癌术后舌缺损修复与舌再造的理想选择。
Keywords: 胸肩峰动脉穿支皮瓣, 游离皮瓣, 舌肿瘤, 舌再造
Abstract
Objective
To investigate the clinical outcome of free thoracoacromial artery perforator (TAAP) flap in the reconstruction of tongue and mouth floor defects after radical resection of tongue carcinoma.
Methods
Between May 2010 and February 2015, 11 cases of tongue carcinoma underwent radical resection and reconstruction of tongue and mouth floor defects with free TAAP flaps. The locations of tongue carcinoma were the lingual margin in 7 cases, the ventral tongue in 2 cases, and the mouth floor in 2 cases. According to Union for International Cancer Control (UICC) TNM stage, 3 cases were classified as T4N0M0, 3 cases as T4NlM0, 2 cases as T3N1M0, 2 cases as T3N2M0, and 1 case as T3N0M0. The disease duration ranged from 3 to 28 months, 10.6 months on average. The tumor size ranged from 6.0 cm×3 cm to 10 cm×5 cm. The TAAP flap ranged from 7.0 cm×4.0 cm to 11.0 cm×5.5 cm in size, and 0.6-1.2 cm (0.8 cm on average) in thickness, with a pedicle length of 6.8-9.9 cm (7.2 cm on average).
Results
All 11 flaps survived, the donor site was closed directly and healed primarily in all cases. The patients were followed up 12-24 months (17.2 months on average). The reconstructed tongue had satisfactory appearance and good functions of swallowing and language. No local recurrence was observed during follow-up. Only linear scar was left at the donor site, and the function of pectoralis major muscle was normal.
Conclusion
The TAAP flap is an ideal choice in the reconstruction of tongue defect after resection of tongue carcinoma, which has good texture, appearance, and function results.
Keywords: Thoracoacromial artery perforator flap, free flap, tongue carcinoma, tongue reconstruction
舌癌是临床常见口腔恶性肿瘤,手术切除是舌癌综合治疗中最重要一环,肿物切除后导致的舌与口底复合缺损会严重影响患者语言、吞咽、呼吸等功能,因此需要进行修复重建[1-2]。目前,临床已有多种游离组织瓣可用于修复重建舌癌术后缺损,极大地提高了患者生存质量[3-6]。其中最常用的是股前外侧皮瓣[7],但是股前外侧穿支大多是肌皮穿支,肌内分离穿支操作复杂。Ariyan 等[8] 首先提出了于胸大肌设计穿支皮瓣的可能,并将该皮瓣命名为胸肩峰动脉穿支皮瓣。该穿支皮瓣血管解剖恒定,血管体区大,血管蒂分离相对容易,皮瓣质地薄且与受区毗邻。2010 年 5 月–2015 年 2 月,我们采用游离胸肩峰动脉穿支皮瓣移植修复 11 例舌癌术后缺损,获得较好疗效。报告如下。
1. 临床资料
1.1. 一般资料
本组男 9 例,女 2 例;年龄 33~72 岁,平均 52.6 岁。均为鳞状细胞癌;原发舌缘 7 例,原发舌腹2 例,口底癌累及舌 2 例。根据国际抗癌联盟(Union for International Cancer Control, UICC)TNM 分期:T4N0M0 3 例,T4NlM0 3 例,T3N1M0 2 例,T3N2M0 2 例,T3N0M0 1 例。病程 3~28 个月,平均 10.6 个月。肿瘤范围 6 cm×3 cm~10 cm×5 cm。
1.2. 手术方法
气管插管全麻下,患者取仰卧位,并垫肩、固定头部。手术分两组同时进行,肿瘤切除组按无瘤原则行颈淋巴结清扫和原发病灶根治性切除,切除后软组织缺损范围为 7.0 cm×4.0 cm~11.0 cm×5.5 cm;同时进行受区血管解剖显露分离。皮瓣组制备游离胸肩峰动脉穿支皮瓣、血管吻合,穿支皮瓣游离移植修复供区。
1.2.1 穿支皮瓣设计 作肩峰至剑突连线,沿锁骨中点向肩峰剑突连线画一条垂直线,以两线交点为圆心画半径 2 cm 圆形区域。术前彩色超声多普勒血流探测仪探查该区域恒定穿支发出点,以该点为中心点、肩峰剑突连线为轴线设计游离胸肩峰动脉穿支皮瓣,长、宽较舌缺损扩大 0.5~1.0 cm。见图 1。
图 1.
Schematic drawing of free TAAP flap design
游离胸肩峰动脉穿支皮瓣设计示意图
1.2.2 穿支皮瓣切取 首先沿穿支皮瓣内侧设计线切开皮肤、皮下组织,显露胸大肌,进一步分离显露自胸大肌锁骨部和胸肋部间隙发出的胸肩峰动脉穿支。然后切开穿支皮瓣外侧缘,于胸大肌表面完全游离皮瓣,牵开锁骨部和胸肋部肌肉,进一步沿穿支逆行肌内分离至胸肩峰动脉自锁骨下动脉发出平面,获取足够长的血管蒂,本组血管蒂长 6.8~9.9 cm,平均 7.2 cm;分离时注意保留胸肩峰动脉胸大肌支备用,皮瓣断蒂后移植至受区。见图 2。皮瓣切取范围为 7.0 cm×4.0 cm~11.0 cm×5.5 cm;厚度 0.6~1.2 cm,平均 0.8 cm。所有供区直接拉拢缝合。
图 2.
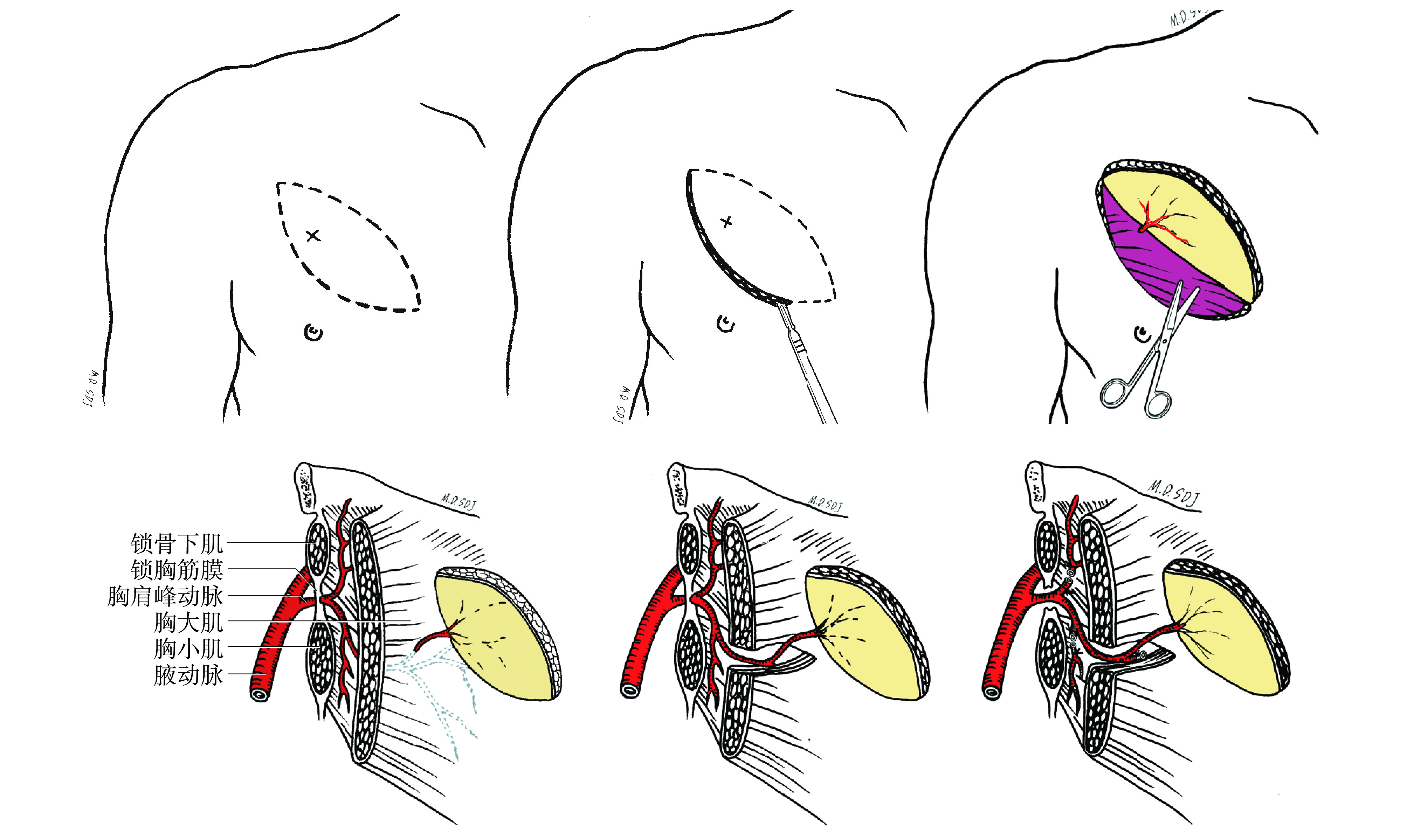
Schematic drawing of free TAAP flap harvesting
游离胸肩峰动脉穿支皮瓣切取示意图
1.2.3 穿支皮瓣修复 先将穿支皮瓣与舌缺损区域缝合固定,皮肤面向外,将胸肩锋动脉穿支与受区甲状腺上动脉吻合,选择较粗的伴行静脉与受区静脉(面总静脉、颈外静脉)吻合,其中 9 例吻合 2 根静脉、2 例吻合 1 根静脉,其中颈内静脉 14 根,均行血管端侧吻合;面总静脉 6 根,均行血管端端吻合。松开血管夹确认皮瓣血运良好、血管通畅。彻底止血,于皮瓣与创面之间、颈清扫创面留置 4 根引流管,注意避开血管吻合区域。
1.3. 术后处理
术后患者卧床休息,头部轻微倾向血管吻合侧。常规抗凝、抗痉挛、抗休克以及全身支持治疗,术后 3 d 内每小时观察皮瓣色泽和指压反应监测皮瓣血运,术后 4~7 d 改为每 3 小时观察皮瓣血运。及时更换敷料及拔除引流管。
2. 结果
术后 11 例皮瓣均顺利成活,未发生切口裂开和肿胀情况,创面Ⅰ期愈合;供区切口均Ⅰ期愈合。患者均获随访,随访时间 12~24 个月,平均 17.2 个月。患者再造舌外形良好,吞咽及语言功能恢复满意,随访期间肿瘤局部无复发。供区仅遗留线性瘢痕,胸大肌功能无明显影响。
3. 典型病例
患者 男,49 岁。因右半舌舌腹鳞状细胞癌 10 个月入院。TNM 分期为 T3N2M0。肿瘤面积 7 cm×4 cm。行颈部淋巴结清扫术联合舌癌根治性切除术后,软组织缺损面积为 8.0 cm×4.5 cm,设计切取左侧游离胸肩峰动脉穿支皮瓣,皮瓣面积为 8.0 cm×4.5 cm,厚度为 0.7 cm,血管蒂长 8.4 cm。皮瓣血管蒂穿支动脉与右侧甲状腺上动脉吻合,两支伴行静脉中 1 支与面静脉端端吻合,另 1 支与颈内静脉端侧吻合。皮瓣供区直接缝合。术后皮瓣成活,创面Ⅰ期愈合;受区切口Ⅰ期愈合。获随访 24 个月,舌外形以及患者吞咽、语言功能均恢复满意,张口度 80°。随访期间肿瘤局部无复发。供区仅遗留线性瘢痕,胸大肌功能无明显影响。见图 3。
图 3.

A typical case a. Preoperative view; b. Intraoperative view of defect; c. Intraoperative free TAAP flap design; d. Intraoperative free TAAP flap harvesting; e. View at immediate after reconstruction; f. Appearance of tongue at 24 months after operation; g, h. Appearance of donor site at 24 months after operation, showing normal function of pectoralis major muscle
典型病例 a. 术前; b. 术中颈部淋巴结清扫和舌癌根治性切除后遗留缺损; c. 术中游离胸肩峰动脉穿支皮瓣设计; d. 术中穿支皮瓣切取; e. 修复术后即刻;f. 术后24个月舌部外观; g、h. 术后24个月皮瓣供区外观,胸大肌功能未见明显影响
4. 讨论
舌癌切除后遗留的舌缺损对患者语言、吞咽等功能及心理均会造成极大影响,一期重建能够极大改善患者术后生存质量,符合现代肿瘤整形外科学的发展方向[9]。临床上常用修复方法有带蒂及游离皮瓣两大类。带蒂皮瓣手术相对简便,易于掌握,不需要显微吻合血管,但由于其供区多位于头颈部,可造成供区继发畸形和功能缺失,而且提供的组织瓣面积有限,影响术后舌功能恢复[10-12]。传统带蒂组织瓣,如胸大肌皮瓣,由于其组织臃肿、修复后外形不满意、供区损伤过大等缺点,已不再作为舌癌术后修复的首选方法[8]。而游离组织瓣可以避免以上问题,临床应用越来越广泛。目前国外报道最多的是游离前臂桡动脉皮瓣,但需牺牲前臂主要供血动脉,供区损伤较大[13-14]。徐达传等[15] 首先报道了股前外侧皮瓣的解剖学研究和临床应用,因其血管蒂长、口径粗、变异少及供区隐蔽等优点成为最常用游离皮瓣;国内外将其广泛用于口腔颌面-头颈肿瘤术后软组织缺损修复[16-17]。但其缺点是血管解剖相对复杂,穿支解剖位置变化较大,肥胖患者皮瓣往往较臃肿,常需一期或多期修薄。
有学者成功采用胸肩峰动脉穿支皮瓣带蒂移位修复头颈部缺损[18-20],我们在此基础上,选择游离胸肩峰动脉穿支皮瓣修复舌癌根治术后继发舌缺损,重建舌外形和结构,取得了满意效果。我们认为游离胸肩峰动脉穿支皮瓣修复舌缺损具有以下优点:① 皮瓣颜色、质地优良,厚度适宜,柔软易塑形;② 胸前区真皮下血管网吻合丰富,穿支血管体区大,切取的皮瓣不仅可以塑形修复舌缺损,还可同时填塞腔隙,满足舌癌术后修复重建需要;③ 穿支血管往往走行于胸大肌锁骨头和胸肋头之间,皮瓣切取分离相对简便;④皮瓣血运可靠,抗感染力强;⑤ 穿支血管蒂部口径粗大,血管蒂长度满意,降低了血管显微吻合难度;⑥ 胸肩峰动脉穿支皮瓣切取宽度不超过 6 cm 时,供区均可直接缝合,创缘张力小,不会造成乳头移位;⑦ 肿瘤切除组和皮瓣切取组可同时手术,缩短了手术时间。另外,与游离股前外侧皮瓣相比,胸肩峰动脉穿支皮瓣制备简便,还能避免二期手术修薄,是舌癌术后软组织缺损修复的理想皮瓣。
Funding Statement
湖南省自然科学基金面上项目(13JJ5012);湖南省科技计划项目(2014SK3002);湖南省卫计委课题项目(B2014-111)
Hunan Provincial Natural Science Foundation (13JJ5012); Hunan Provincial Science and Technology Planning Project (2014SK3002); Hunan Provincial Health and Family Planning Commission Project (B2014-111)
References
- 1.BokhariWA, WangSJ Tongue reconstruction: recent advances. Curr Opin Otolaryngol Head Neck Surg. 2007;15(4):202–207. doi: 10.1097/MOO.0b013e3281fbd406. [DOI] [PubMed] [Google Scholar]
- 2.HanasonoMM, MatrosE, DisaJJ Important aspects of head and neck reconstruction. Plast Reconstr Surg. 2014;134(6):968e–980e. doi: 10.1097/PRS.0000000000000722. [DOI] [PubMed] [Google Scholar]
- 3.BrownJS, RogersSN, LoweD A comparison of tongue and soft palate squamous cell carcinoma treated by primary surgery in terms of survival and quality of life outcomes. Int J Oral Maxillofac Surg. 2006;35(3):208–214. doi: 10.1016/j.ijom.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 4.BroylesJM, AbtNB, ShridharaniSM The fusion of craniofacial reconstruction and microsurgery: a functional and aesthetic approach. Plast Reconstr Surg. 2014;134(4):760–769. doi: 10.1097/PRS.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 5.YuP Reinnervated anterolateral thigh flap for tongue reconstruction. Head Neck. 2004;26(12):1038–1044. doi: 10.1002/hed.20106. [DOI] [PubMed] [Google Scholar]
- 6.KatouF, ShiraiN, KamakuraS Intraoral reconstruction with innervated forearm flap: a comparison of sensibility and reinnervation in innervated versus noninnervated forearm flap. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(6):638–644. doi: 10.1016/s1079-2104(05)80243-4. [DOI] [PubMed] [Google Scholar]
- 7.KoshimaI Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast Reconstr Surg. 2000;105(7):2358–2360. doi: 10.1097/00006534-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 8.AriyanS The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979;63(1):73–81. doi: 10.1097/00006534-197901000-00012. [DOI] [PubMed] [Google Scholar]
- 9.周晓, 胡炳强, 罗以 浅谈肿瘤整形外科形成的必要性. 中国肿瘤. 2001;10(12):694–695. [Google Scholar]
- 10.高银光, 范飞, 尤建军 颏下皮瓣的应用解剖学研究. 中国临床解剖学杂志. 2006;24(1):54–56. [Google Scholar]
- 11.FornerD, PhillipsT, RigbyM Submental island flap reconstruction reduces cost in oral cancer reconstruction compared to radial forearm free flap reconstruction: a case series and cost analysis. J Otolaryngol Head Neck Surg. 2016;45:11. doi: 10.1186/s40463-016-0124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ChaudharyB, GongZ, LingB Application of the submental island flap in the reconstruction of intraoral defects. J Craniofac Surg. 2014;25(4):e309–312. doi: 10.1097/SCS.0000000000000573. [DOI] [PubMed] [Google Scholar]
- 13.KuriakoseMA, LoreeTR, SpiesA Sensate radial forearm free flaps in tongue reconstruction. Arch Otolaryngol Head Neck Surg. 2001;127(12):1463–1466. doi: 10.1001/archotol.127.12.1463. [DOI] [PubMed] [Google Scholar]
- 14.LoewenIJ, BoliekCA, HarrisJ Oral sensation and function: a comparison of patients with innervated radial forearm free flap reconstruction to healthy matched controls. Head Neck. 2010;32(1):85–95. doi: 10.1002/hed.21155. [DOI] [PubMed] [Google Scholar]
- 15.徐达传, 阮默, 张春 股前外侧部皮瓣的进一步解剖学研究——高位皮动脉与皮瓣血供的分型. 中国临床解剖学杂志. 2002;20(6):410–413. [Google Scholar]
- 16.LongoB, PagnoniM, FerriG The mushroom-shaped anterolateral thigh perforator flap for subtotal tongue reconstruction. Plast Reconstr Surg. 2013;132(3):656–665. doi: 10.1097/PRS.0b013e31829acf84. [DOI] [PubMed] [Google Scholar]
- 17.ChengN, ShouB, ZhengM Microneurovascular transfer of the tensor fascia lata musculocutaneous flap for reconstruction of the tongue. Ann Plast Surg. 1994;33(2):136–141. doi: 10.1097/00000637-199408000-00003. [DOI] [PubMed] [Google Scholar]
- 18.ZhangYX, LiZ, GrassettiL A new option with the pedicle thoracoacromial artery perforator flap for hypopharyngeal reconstructions. Laryngoscope. 2016;126(6):1315–1320. doi: 10.1002/lary.25675. [DOI] [PubMed] [Google Scholar]
- 19.LiZ, CuiJ, ZhangYX Versatility of the thoracoacromial artery perforator flap in head and neck reconstruction. J Reconstr Microsurg. 2014;30(7):497–503. doi: 10.1055/s-0034-1370359. [DOI] [PubMed] [Google Scholar]
- 20.ZhangYX, YongjieH, MessmerC Thoracoacromial artery perforator flap: anatomical basis and clinical applications. Plast Reconstr Surg. 2013;131(5):759e–770e. doi: 10.1097/PRS.0b013e3182865bf5. [DOI] [PubMed] [Google Scholar]



