Abstract
Aims:
Investigate the relationship between food insecurity and glycemic control in adults with diagnosed and undiagnosed diabetes.
Methods:
Using National Health and Nutrition Examination Survey (NHANES) between 2003–2016, food insecurity was measured using the household food insecurity scale. Glycemic control was measured using glycated hemoglobin (HbA1c) collected during the NHANES examination. Individuals were categorized into undiagnosed diabetes or diagnosed diabetes based on their measured HbA1c and response to whether they were told by a doctor or other health professional they have diabetes or were taking medications for diabetes. Sampling weights and survey procedures were used when conducting univariate and multivariable models using SAS version 9.4.
Results:
Approximately 13.7% of the population sample (35,216 adults representing 207,271,917 US adults) reported food insecurity. Reporting food insecurity was associated with 0.37 higher HbA1c for diagnosed (95%CI 0.15–0.60) and 0.45 higher HbA1c for undiagnosed diabetes (95%CI 0.05–0.85). In the undiagnosed diabetes population, those reporting food insecurity had 80% higher likelihood of HbA1c above 7% (OR=1.80, 95%CI 1.06–3.06).
Conclusions:
Food insecurity had a stronger relationship with HbA1c for those with undiagnosed diabetes. Results suggest the importance of screening for individuals with food insecurity that may be at high risk for having undiagnosed diabetes.
Keywords: food insecurity, diabetes, undiagnosed diabetes, glycemic control, social determinants of health
INTRODUCTION
Diabetes is a major public health concern, being the seventh leading cause of death in the United States and the number one cause of kidney failure, limb amputation and blindness in adults (1–3). The prevalence of diagnosed type 2 diabetes in adults has risen dramatically, from 4.5% in 1995 to 10.2% in 2020 (1,3). Undiagnosed diabetes as remained relatively stable over that time frame, though 7.3 million adults are still living with undiagnosed diabetes. (1) Socioeconomic inequities exist in both diagnosed and undiagnosed diabetes, however, there is evidence to suggest diagnosis can improve risk factor modification through awareness to begin lifestyle interventions or preventative methods (4,5). Given the cost and physical burden of diabetes, it is important to investigate modifiable risk factors, such as food insecurity, to address underlying drivers of poor health (4,6–7).
Food security is an important social determinant of health associated with poor outcomes, especially in adults with chronic disease (2,8). There is ample evidence that supports a relationship between food security and the physical, mental and social health of individuals (9–11). Food insecurity is defined as “limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways” (12). Rates have been rising since the late 1990’s and have doubled from 9% of the US population in 2005–2006 to 18% in 2011–2012, with some plateau recently to 15% (4). A substantial amount of research describes the relationship between food insecurity and poor dietary quality, which in turn can influence diabetes and poor diabetes control (7,13–16). Studies suggests food insecurity may influence following a diabetes diet, as inexpensive foods tend to be more calorie dense, with high fats and sugars, and refined carbohydrates (14).
Based on the American Diabetes Association Diabetes Care Guidelines, one of the primary ways to maintain good glucose control is with exercise and good eating habits, however, additional biological, behavioral, and psychosocial factors influence glycemic control, such as age, duration of diabetes, number of medications, stress, and insulin sensitivity (17–21). Addressing glycemic control is necessary to decrease the risk of complications of diabetes (17). Glycemic targets are recommended to be individualized depending on a patient’s current health status, their goals, and their life expectancy (19,22). Food insecurity may reduce self-efficacy and or increase emotional distress regarding diabetes management (7,8). However, for undiagnosed individuals this becomes particularly difficult, as they have neither the awareness of the need to address them, nor the training to conduct self-care behaviors. (2). In addition, given the socioeconomic disparities noted in individuals with undiagnosed diabetes, factors such as food insecurity, may have a greater influence on glycemic control with the additional lack of awareness of self-management goals. (23–25)
Given the impact of poor glycemic control on quality of health and future complications, and the significant number of individuals with both diagnosed and undiagnosed diabetes, it is important to understand the relationship between food insecurity and glycemic control. Currently, the evidence focuses on diagnosed diabetes, and as such, may underestimate the need to address this risk factor. Therefore, the aim of this study was to investigate the relationship between food insecurity and glycemic control in adults with diagnosed and undiagnosed diabetes.
METHODS
Data Source and Study Population
The National Health and Nutrition Examination Survey (NHANES) is a nationally representative survey conducted by the National Center for Health Statistics (NCHS) and released in two-year intervals. NHANES is used to estimate health and nutritional status of adults in the United States and includes both a self-reported questionnaire and physical examination. (26,27) Findings from NHANES help dictate the widespread presence of disease and risk factors, such as food insecurity and nutrition, helping determine which risk factors increase the prevalence of the disease(s).
This study used seven cycles of NHANES data covering the years 2003– 2016. Participants included in the analysis were ages 20 years and older, and completed both the survey interview and physical examination. In total, 35,216 participants were analyzed, after removing participants that did not answer questions related to food insecurity (578 participants), or have HbA1c information (1,916 participants).
Food Insecurity Measures
The Food Security Survey Module includes ten questions asked of households without children and eighteen questions asked of households with children to measure the level of household food insecurity. (12) The same questions were used throughout all cycles. Questions include frequency of being worried food would run out before more money was available to buy more food, frequency of food that was bought not lasting, frequency of not being able to afford to eat balanced meals, and whether respondent cut the size of meals, was hungry, lost weight or ate less because of money. Food security was defined as either full or marginal food security (0–2 affirmative responses). Food insecurity was defined as low or very low food security (3 or more affirmative responses).
Glycemic Control and Diabetes Status
The main outcome was blood glycated hemoglobin (HbA1c) as collected by the NHANES examination. Individuals were categorized into three mutually exclusive groups by diabetes status (no diabetes, undiagnosed diabetes, and diagnosed diabetes) based on their measured HbA1c and response to diabetes related questions. Participants were considered to have diagnosed diabetes if they answered “yes” to any of the following three questions: “Have you ever been told by a doctor or other health professional that you have diabetes or sugar diabetes?”, “Are you now taking insulin?”, or “Are you now taking diabetic pills to lower your blood sugar?”. Participants were classified as having undiagnosed diabetes if they answered “no” to all three questions, but had a measured HbA1c ≥ 6.5%. If participants answered “no” to all three questions and had a measured HbA1c <6.5%, they were categorized as no diabetes, based on ADA guidelines for diagnosis (18).
Demographic Variables
Demographic variables included sex, age (grouped as 20–39 years; 40–54 years; 55–69 years; and 70 + years), race/ethnicity (grouped as non-Hispanic White; non-Hispanic Black; Hispanic; and other minority), education (grouped as no degree; high school diploma/GED; some college; and college graduate), marital status (grouped as married/partnered; widowed, divorced/separated; and never married), ratio of family income to poverty, and access to health care based on the question “Is there a place that you usually go when you are sick or you need advice about health?” (dichotomized as yes and no).
Statistical Analysis
Statistical analysis was performed with SAS version 9.4 (SAS Institute) in April 2020. As NHANES data were collected using a complex multistage design, SAS procedures for survey sampling were used to calculate correct standard errors (SEs) and p-values. To correct unequal probability sampling bias and nonresponse bias, exam sample weights were used in all analyses. To account for the missing of HbA1c and food insecurity information, we created a domain – valid, all those with information of both variables are included as valid. We completed a subpopulation analysis using the entire selected sample in all analyses, and only took the sample size of the created domain into account. In this way, we accounted for the random variability introduced by domain sample sizes unrelated to sample design.
The SURVEYFREQ, SURVEYMEANS, SURVEYREG, and SURVEYLOGISTIC procedures were used to account for the complex survey design. Survey general linear regression models were used to assess the relationship between food insecurity and continuous HbA1c level. Univariate models and multivariable models adjusted by demographics and survey cycles were developed to test the unadjusted and adjusted mean difference between food security and food insecurity. We also performed subpopulation analyses by diabetes status to further test if there were any differences by diabetes status. Survey logistic regression models were performed to assess the relationship between food insecurity and HbA1c control level dichotomized by 7% for diagnosed and undiagnosed individuals. All p values were 2-sided and p<.05 was considered statistically significant.
RESULTS
The population sample included 35,216 adults 20 years and older, which represented 207,271,917 US adults 20 years and older. Table 1 provides weighted sample demographics. 13.7% of the population reported food insecurity. Among those reporting food insecurity, 53.9% were female, median ratio of family income to poverty was 1.15, 34.6% had no degree and 26.7% had high school diploma/GED, 18.7% were NHB and 28.0% were Hispanic. Comparatively, among individuals that were food secure, median ratio of family income to poverty was 3.40, 63.2% had college or above education, and 72.3% were non-Hispanic white.
Table 1:
Sample demographics of adults by food security status (% and means weighted, unweighted n)
| Food Secure | Food Insecure | p-value | |
|---|---|---|---|
| Unweighted sample | n = 28,660 | n = 6,556 | |
| Weighted sample | N = 178,885,416 | N = 28,386,500 | |
| Sex | 0.0024 | ||
| Male | 48.29% (13,990) | 46.10% (3,012) | |
| Female | 51.71% (14,670) | 53.90% (3,544) | |
| Age group | <.0001 | ||
| 20–39 | 34.62% (9,236) | 48.52% (2,768) | |
| 40–54 | 29.77% (7,101) | 30.60% (1,915) | |
| 55–69 | 22.28% (6,726) | 15.44% (1,324) | |
| 70 + | 13.33% (5,597) | 5.43% (549) | |
| Race/Ethnicity | <.0001 | ||
| Non-Hispanic White | 72.26% (13,822) | 46.93% (1,987) | |
| Non-Hispanic Black | 9.63% (5,598) | 18.66% (1,629) | |
| Hispanic | 11.03% (6,401) | 27.99% (2,512) | |
| Other Minority | 7.08% (2,839) | 6.42% (428) | |
| Education level | <.0001 | ||
| No degree | 14.34% (6,474) | 34.63% (2,770) | |
| High school diploma/GED | 22.51% (6,466) | 26.68% (1,636) | |
| Some college | 31.50% (8,364) | 30.95% (1,723) | |
| College graduate | 31.65% (7,326) | 7.74% (419) | |
| Marital status | <.0001 | ||
| Married/Partnered | 65.92% (17,780) | 51.96% (3,382) | |
| Widowed | 6.20% (2,545) | 5.10% (455) | |
| Divorced/Separated | 11.51% (3,605) | 19.40% (1,255) | |
| Never married | 16.36% (4,717) | 23.54% (1,460) | |
| Ratio of family income to poverty | <.0001 | ||
| Median (interquartile range) | 3.40 (1.82–4.99) | 1.15 (0.73–1.85) | |
| Access to health care | <.0001 | ||
| No | 13.34% (3,914) | 24.17% (1,531) | |
| Yes | 86.66% (24,746) | 75.83% (5,025) | |
| Diabetes status | <.0001 | ||
| No diabetes | 88.95% (24,322) | 85.77% (5,387) | |
| Diagnosed diabetes | 9.25% (3,587) | 11.57% (971) | |
| Undiagnosed diabetes | 1.80% (751) | 2.66% (198) | |
| HbA1c, mean (95% CI) | |||
| No Diabetes | 5.36 (5.35 – 5.37) | 5.39 (5.37 – 5.40) | 0.0056 |
| Diagnosed Diabetes | 7.16 (7.09 – 7.23) | 7.74 (7.56 – 7.91) | <.0001 |
| Undiagnosed Diabetes | 7.40 (7.27 – 7.52) | 8.07 (7.74 – 8.40) | 0.0006 |
| Body Mass, mean (95% CI) | |||
| BMI | 28.62 (28.46 – 28.78) | 29.97 (29.67 – 30.26) | <.0001 |
| Waist Circumference, cm | 98.40 (97.99 – 98.81) | 100.15 (99.47 – 100.83) | <.0001 |
Table 1 also provides information on the weighted means of HbA1c by diabetes status. Those with reported food insecurity had significantly higher HbA1c levels – for those with no diabetes 5.36 compared to 5.39 (p=0.0056), for those with diagnosed diabetes 7.16 compared to 7.74 (p<.0001), and for those with undiagnosed diabetes 7.40 compared to 8.07 (p=0.0006). The difference in weighted mean HbA1c was clinically significant for those with diagnosed (difference in HbA1c=0.58) and undiagnosed diabetes (difference in HbA1c=0.67). Figure 1 shows the weighted A1c level distribution by household food security status.
Figure 1.
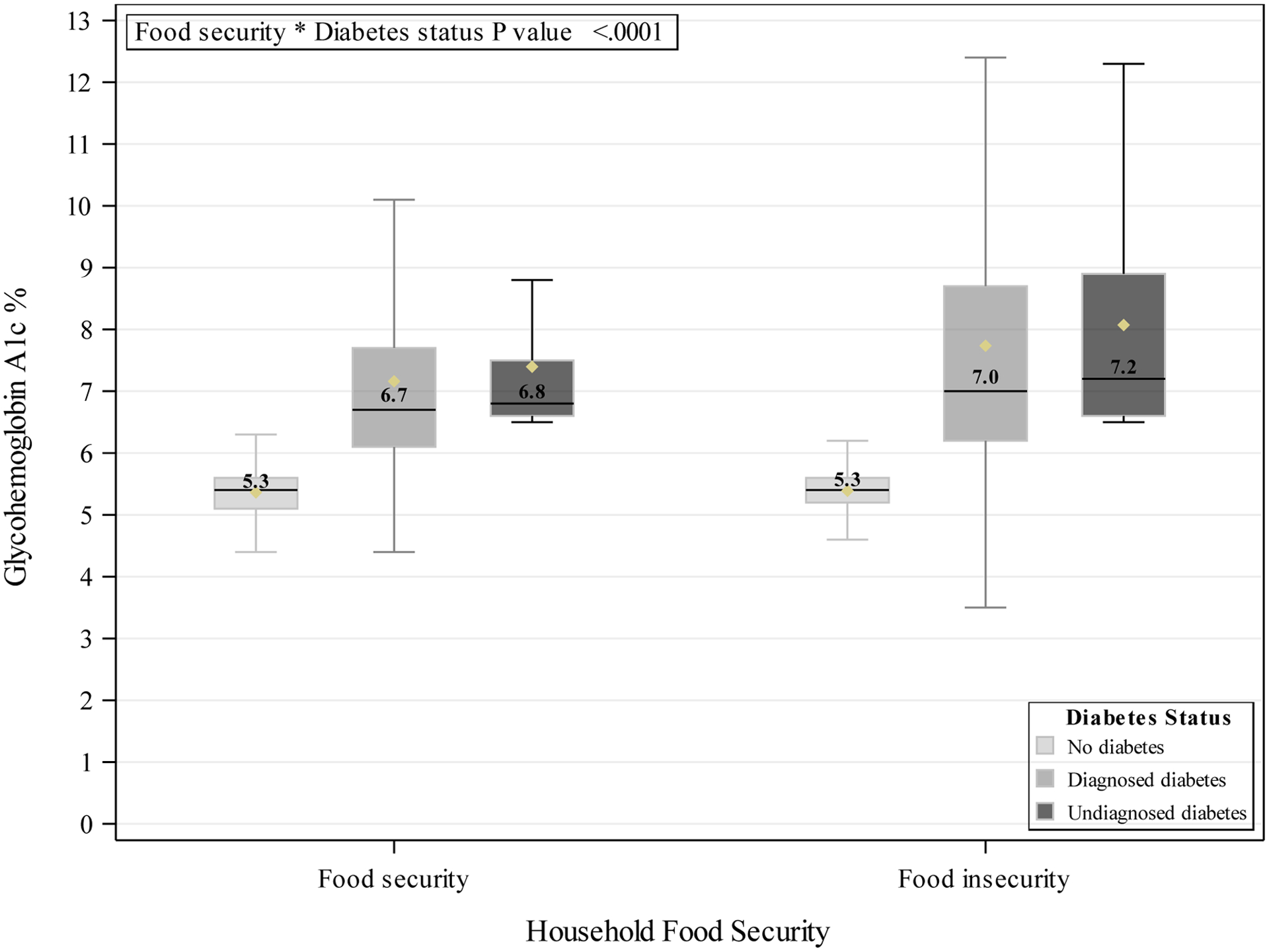
Weighted A1c level distribution by household food security
Table 2 presents the adjusted linear analyses by diabetes status - no diabetes, diagnosed diabetes, and undiagnosed diabetes. For those with no diabetes, reporting food insecurity was associated with 0.03 higher HbA1c level (β=0.03, 95% CI 0.01–0.04). For those with diagnosed diabetes, reporting food insecurity was associated with 0.37 higher HbA1c level (β=0.37, 95% CI 0.15–0.60). For those with undiagnosed diabetes, reporting food insecurity was associated with 0.45 higher HbA1c level (β=0.45, 95% CI 0.05–0.85).
Table 2:
Weighted Adjusted Linear Regression for the Relationship between Food Insecurity and Glycemic Control
| No Diabetes | Diagnosed Diabetes | Undiagnosed Diabetes | ||||
|---|---|---|---|---|---|---|
| Adjusted Estimate | P Value | Adjusted Estimate | P Value | Adjusted Estimate | P Value | |
| Household food security | 0.0003 | 0.0015 | 0.0284 | |||
| Food security | Ref | Ref | Ref | |||
| Food insecurity | 0.03(0.01 – 0.04) | 0.37(0.15 – 0.60) | 0.45(0.05 – 0.85) | |||
| Sex | <.0001 | 0.0003 | 0.0004 | |||
| Male | Ref | Ref | Ref | |||
| Female | −0.03(−0.04 – −0.02) | −0.24(−0.37 – −0.11) | −0.36(−0.55 – −0.16) | |||
| Age group | <.0001 | <.0001 | 0.0041 | |||
| 20–39 | Ref | Ref | Ref | |||
| 40–54 | 0.19(0.18 – 0.20) | 0.16(−0.17 – 0.49) | −0.26(−0.74 – 0.21) | |||
| 55–69 | 0.35(0.34 – 0.37) | −0.09(−0.42 – 0.24) | −0.38(−0.83 – 0.08) | |||
| 70 + | 0.40(0.39 – 0.42) | −0.35(−0.67 – −0.04) | −0.74(−1.23 – −0.25) | |||
| Race | <.0001 | <.0001 | 0.0183 | |||
| Non-Hispanic White | Ref | Ref | Ref | |||
| Non-Hispanic Black | 0.16(0.14 – 0.18) | 0.44(0.27 – 0.61) | −0.10(−0.41 – 0.20) | |||
| Hispanic | 0.09(0.07 – 0.10) | 0.58(0.37 – 0.79) | 0.45(0.10 – 0.80) | |||
| Other Minority | 0.11(0.09 – 0.13) | 0.13(−0.16 – 0.41) | 0.22(−0.24 – 0.68) | |||
| Education level | <.0001 | 0.0509 | 0.9903 | |||
| No degree | Ref | Ref | Ref | |||
| High school diploma/GED | −0.02(−0.03 – −0.002) | 0.05(−0.13 – 0.24) | 0.04(−0.32 – 0.40) | |||
| Some college | −0.04(−0.06 – −0.03) | −0.04(−0.24 – 0.16) | −0.02(−0.38 – 0.35) | |||
| College graduate | −0.08(−0.10 – −0.07) | −0.20(−0.42 – 0.01) | 0.01(−0.44 – 0.45) | |||
| Marital status | <.0001 | 0.9395 | 0.0606 | |||
| Married/Partnered | Ref | Ref | Ref | |||
| Widowed | 0.03(0.002 – 0.05) | 0.03(−0.11 – 0.17) | 0.20(−0.15 – 0.56) | |||
| Divorced/Separated | 0.002(−0.01 – 0.02) | −0.01(−0.18 – 0.16) | −0.05(−0.40 – 0.30) | |||
| Never married | −0.04(−0.05 – −0.02) | 0.06(−0.24 – 0.36) | 0.51(0.09 – 0.93) | |||
| Ratio of family income to poverty | 0.5026 | 0.7215 | 0.3397 | |||
| Ratio increase of 1 | −0.001(−0.01 – 0.003) | 0.01 (−0.04 – 0.06) | −0.05(−0.15 – 0.05) | |||
| Access to health care | 0.6427 | 0.0029 | 0.0057 | |||
| No | Ref | Ref | Ref | |||
| Yes | −0.003(−0.02 – 0.01) | −0.69(−1.15 – −0.24) | −0.56(−0.96 – −0.17) | |||
| Data release cycle | <.0001 | 0.2170 | 0.6862 | |||
| NHANES 2003–2004 | Ref | Ref | Ref | |||
| NHANES 2005–2006 | −0.05(−0.08 – −0.03) | −0.07(−0.34 – 0.20) | 0.38(−0.12 – 0.89) | |||
| NHANES 2007–2008 | 0.06(0.03 – 0.09) | −0.08(−0.32 – 0.16) | 0.03(−0.37 – 0.44) | |||
| NHANES 2009–2010 | 0.10(0.08 – 0.13) | −0.09(−0.35 – 0.16) | −0.04(−0.40 – 0.32) | |||
| NHANES 2011–2012 | 0.09(0.06 – 0.12) | 0.11(−0.14 – 0.36) | −0.02(−0.47 – 0.44) | |||
| NHANES 2013–2014 | 0.04(0.02 – 0.07) | 0.13(−0.09 – 0.35) | 0.10(−0.33 – 0.53) | |||
| NHANES 2015–2016 | 0.08(0.05 – 0.10) | 0.01(−0.24 – 0.26) | −0.01(−0.41 – 0.39) | |||
Table 3 presents adjusted logistic analyses those with diagnosed and undiagnosed diabetes. In a population with diagnosed diabetes, those with food insecurity were 25% more likely to have an A1c above 7%, and the relationship was statistically significant (OR=1.25, 95% CI 1.01–1.55). In an undiagnosed diabetes population, those reporting food insecurity are 80% more likely to be in above 7%, and the relationship was statistically significant (OR=1.80, 95% CI 1.06–3.06).
Table 3.
Weighted Adjusted Logistic Regression for the Relationship between Food Insecurity and Glycemic Control (above 7% vs 7% or less)
| Diagnosed Diabetes | Undiagnosed Diabetes | |||
|---|---|---|---|---|
| Odds Ratio | P Value | Odds Ratio | P Value | |
| Household food security | 0.0437 | 0.0289 | ||
| Food security | Ref | Ref | ||
| Food insecurity | 1.25(1.01 – 1.55) | 1.80(1.06 – 3.06) | ||
| Sex | 0.0006 | 0.0090 | ||
| Male | Ref | Ref | ||
| Female | 0.76(0.65 – 0.89) | 0.61(0.43 – 0.88) | ||
| Age group | 0.0053 | 0.1331 | ||
| 20–39 | Ref | Ref | ||
| 40–54 | 1.34(0.96 – 1.88) | 0.97(0.50 – 1.89) | ||
| 55–69 | 1.15(0.82 – 1.62) | 0.62(0.33 – 1.17) | ||
| 70 + | 0.87(0.60 – 1.26) | 0.58(0.28 – 1.23) | ||
| Race | 0.0006 | 0.0190 | ||
| Non-Hispanic White | Ref | Ref | ||
| Non-Hispanic Black | 1.32(1.10 – 1.60) | 0.76(0.45 – 1.29) | ||
| Hispanic | 1.61(1.29 – 2.02) | 1.56(0.90 – 2.70) | ||
| Other Minority | 1.16(0.85 – 1.59) | 1.64(0.81 – 3.30) | ||
| Education level | 0.0870 | 0.5093 | ||
| No degree | Ref | Ref | ||
| High school diploma/GED | 1.02(0.82 – 1.27) | 0.80(0.44 – 1.43) | ||
| Some college | 0.91(0.72 – 1.16) | 1.15(0.69 – 1.93) | ||
| College graduate | 0.72(0.55 – 0.93) | 0.87(0.43 – 1.77) | ||
| Marital status | 0.8076 | 0.2747 | ||
| Married/Partnered | Ref | Ref | ||
| Widowed | 0.92(0.74 – 1.15) | 1.25(0.60 – 2.63) | ||
| Divorced/Separated | 0.93(0.77 – 1.13) | 0.89(0.47 – 1.69) | ||
| Never married | 0.97(0.72 – 1.31) | 1.71(0.94 – 3.13) | ||
| Ratio of family income to poverty | 0.5634 | 0.6019 | ||
| Ratio increase of 1 | 1.02(0.95 – 1.09) | 0.96(0.81 – 1.13) | ||
| Access to health care | 0.1148 | 0.0210 | ||
| No | Ref | Ref | ||
| Yes | 0.70(0.45 – 1.09) | 0.53(0.31 – 0.91) | ||
| Data release cycle | 0.9769 | 0.8503 | ||
| NHANES 2003–2004 | Ref | Ref | ||
| NHANES 2005–2006 | 0.88(0.60 – 1.30) | 1.69(0.81 – 3.52) | ||
| NHANES 2007–2008 | 0.92(0.63 – 1.36) | 1.17(0.60 – 2.26) | ||
| NHANES 2009–2010 | 0.90(0.60 – 1.35) | 0.99(0.52 – 1.88) | ||
| NHANES 2011–2012 | 0.98(0.69 – 1.39) | 1.24(0.57 – 2.68) | ||
| NHANES 2013–2014 | 1.02(0.71 – 1.47) | 1.18(0.65 – 2.14) | ||
| NHANES 2015–2016 | 0.97(0.67 – 1.42) | 1.08(0.53 – 2.19) | ||
DISCUSSION
This analysis provides important insights to guide primary care efforts, finding that food insecurity is associated with glycemic control in individuals with diagnosed and undiagnosed diabetes. Results in adults with diagnosed diabetes align with previous studies indicating food insecurity is associated with higher A1c. This association, however, appears stronger for those with undiagnosed diabetes. Weighted mean A1c was 0.45% higher for food insecure individuals with undiagnosed diabetes, and they were 80% more likely to have A1c above 7%. Since those with a diagnosis may have more regular access to healthcare, and may have received more self-management training, these results suggest an important target population for future interventions should be individuals with food insecurity who may be at high risk for having undiagnosed diabetes.
This analysis offers novel information for public health professionals and healthcare providers. A recent analysis by Dwyer-Lindgren et al. found that substantial geographic disparities in rates of diagnosis of diabetes and rates of effective diabetes treatment in the US population, and suggested targeting high-burden areas with the right mix of public health strategies (24). Public health strategies should be informed by the social determinants of health influencing populations at the local level to be most effective. (28) This analysis provides information to inform development of public health interventions by investigating a specific social determinant of health, food insecurity, and showing its influence on those not diagnosed is stronger than on those diagnosed with diabetes. The interplay between food security, diabetes prevention and management, is also one healthcare providers should be aware of as it increases the difficulty of compliance with the necessary diet due to availability of food. (17,29). Lack of awareness of diabetes diagnosis can explain the worse glycemic control observed among adults with undiagnosed diabetes compared with adults with diagnosed diabetes. Healthcare provider awareness and recognition of the potential challenges posed by food insecurity with its associated impact on glycemic control is essential for 1) the patient-provider encounter, 2) managing patient expectations, 3) patient outcomes and 4) provision of available and necessary resources (within the healthcare organization and in the communities) to the patient. Identifying food insecurity may improve clinical care, and linking patients to reliable food access and support will help improve outcomes over time (7).
Finally, this study highlights the importance of early screening and diagnosis of diabetes, for individuals with increased risk either due to biological, behavioral, or social determinants. Diabetes screening in high-risk populations, such as food insecure individuals, is necessary to increase the capacity of individuals to understand their health risks and develop self-management goals with their socioeconomic realities taken into account. Raising awareness of the symptoms and risk factors of diabetes may also lead to earlier diagnosis and treatment, resulting in overall better health (18). Historically, screening is focused on individuals who are overweight and obese, however, recent studies are finding a large proportion of individuals with diabetes are going un-screened and thus undiagnosed (18,30). Individuals that go unscreened and undiagnosed are those with healthy weights, this has been referred to as “normal weight obesity” where they have high body fat, and low lean muscle mass yet still falling within the parameters of a “healthy” weight (31). In order to understand the burden of undiagnosed diabetes, it is critical for public health efforts to focus on evaluation and monitoring, specifically in regard to screening and diagnosis (32).
Limitations
This analysis provides nationally representative information on the relationship between an important social determinant of health, food insecurity, and a health outcome, glycemic control, both in diagnosed and undiagnosed individuals. Limitations include the cross-sectional nature of the data, which precludes discussion of causality. Secondly, variables not accounted for in the analysis, such as details surrounding diet, medication adherence, and neighborhood factors may further explain the relationship and should be considered in local level analysis. Finally, NHANES does not allow separation of type 1 and type 2 diabetes, and our analysis relies on self-report of diabetes. Prior studies have shown participant recall for chronic illness, such as diabetes, is high and therefore a valid measure of diagnosis. (33,34) Given approximately 5–10% of people with diabetes have type 1 diabetes, results are likely to generalize most to type 2 diabetes, and future work should investigate if differences in the relationship exist by type 1 and type 2 diagnosis.
CONCLUSION
In conclusion, this analysis found reported food insecurity was associated with significantly higher HbA1c levels, with a stronger relationship for those with undiagnosed diabetes. These results suggest the need to consider increasing screening for individuals with food insecurity. Diabetes screening in high risk populations, such as food insecure individuals, is necessary to increase the capacity of individuals to understand their health risks and develop self-management goals with the context of their socioeconomic realities.
Highlights:
Food insecurity had a stronger relationship with HbA1c for undiagnosed diabetes.
Adults with food insecurity may be at high risk for having undiagnosed diabetes.
Screening for diabetes should be considered in food insecure adults.
Funding:
Effort for this study was partially supported by the National Institute of Diabetes and Digestive Kidney Disease (K24DK093699, R01DK118038, R01DK120861, PI: Egede), the National Institute for Minority Health and Health Disparities (R01MD013826, PI: Egede/Walker), and the American Diabetes Association (1-19-JDF-075, PI: Walker).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests: The authors declare that they have no competing interests.
Financial Disclosures: No financial disclosures are reported by the authors of this paper.
Ethical approval: No ethics approval was required for this study as it used nationally available data.
References:
- 1.Centers for Disease Control and Prevention. (2020) National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services. [Google Scholar]
- 2.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, & Wee CC (2013). Food Insecurity and Metabolic Control Among U.S. Adults With Diabetes. Diabetes Care, 36(10), 3093–3099. 10.2337/dc13-0570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murillo R, Reesor LM, Scott CW, & Hernandez DC (2017). Food Insecurity and Pre-diabetes in Adults: Race/Ethnic and Sex Differences. American Journal of Health Behavior, 41(4), 428–436. 10.5993/ajhb.41.4.7 [DOI] [PubMed] [Google Scholar]
- 4.Walker RJ, Grusnick J Garacci E, Mendez C, Egede LE (2019). Trends in food insecurity in the USA for individuals with prediabetes, undiagnosed diabetes, and diagnosed diabetes. JGIM, 34:33–35. 10.1007/s11606-018-4651-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moody A, Cowley G, Fat LN, & Mindell JS (2016). Social inequalities in prevalence of diagnosed and undiagnosed diabetes and impaired glucose regulation in participants in the Health Surveys for England series. BMJ Open, 6(2). 10.1136/bmjopen-2015-010155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkowitz SA, Gao X, & Tucker KL (2014). Food-Insecure Dietary Patterns Are Associated With Poor Longitudinal Glycemic Control in Diabetes: Results From the Boston Puerto Rican Health Study. Diabetes Care, 37(9), 2587–2592. 10.2337/dc14-0753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seligman HK, Jacobs EA, Lopez A, Tschann J, & Fernandez A (2012). Food Insecurity and Glycemic Control Among Low-Income Patients With Type 2 Diabetes. Diabetes Care, 35(2), 233–238. 10.2337/dc11-1627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gucciardi E, Vahabi M, Norris N, Monte JP, & Farnum C (2014). The Intersection between Food Insecurity and Diabetes: A Review. Current Nutrition Reports, 3(4), 324–332. 10.1007/s13668-014-0104-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirkpatrick S (2008). Food Insecurity is Associated with Nutrient Inadequacies Among Canadian Adults and Adolescents. J Nutri, 138(3), 604–612. [DOI] [PubMed] [Google Scholar]
- 10.Martin KS, Rogers BL, Cook JT, & Joseph HM (2004). Social capital is associated with decreased risk of hunger. Social Science & Medicine, 58(12), 2645–2654. 10.1016/j.socscimed.2003.09.026 [DOI] [PubMed] [Google Scholar]
- 11.Essien UR, Shahid NN, & Berkowitz SA (2016). Food Insecurity and Diabetes in Developed Societies. Current Diabetes Reports, 16(9). 10.1007/s11892-016-0774-y [DOI] [PubMed] [Google Scholar]
- 12.Bickel G (n.d.). Guide to Measuring Household Food Security (Revised 2000). Retrieved September 29, 2017, from https://www.fns.usda.gov/guide-measuring-household-food-security-revised-2000
- 13.Drenowski A (2005). Food Choices and Diet Costs: An Economic Analysis. J Nutri, 135, 900–904. [DOI] [PubMed] [Google Scholar]
- 14.Nord M, Andrews M, & Carlson S (2005). Household Food Security in the United States, 2004. SSRN Electronic Journal. 10.2139/ssrn.878333 [DOI] [Google Scholar]
- 15.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, & Kushel MB (2007). Food Insecurity is Associated with Diabetes Mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. Journal of General Internal Medicine, 22(7), 1018–1023. 10.1007/s11606-007-0192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berkowitz SA, Berkowitz TS, Meigs JB, & Wexler DJ (2017). Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005–2012. Plos One, 12(6). 10.1371/journal.pone.0179172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Diabetes Association. Standards of Medical Care 2017. Diabetes Care. 2017; 40(Supplement 1): 1–142. [Google Scholar]
- 18.Beckles GL, Chou C. Diabetes – United States, 2006 and 2010. Morbidity and Mortality Weekly Report. 2013; 62(3): 99–104. [PubMed] [Google Scholar]
- 19.Perlmuter LC, Flanagan BP, Shah PH, & Singh SP (2009). Glycemic Control and Hypoglycemia: Is the Loser the Winner?: Response to Clark. Diabetes Care, 32(3). 10.2337/dc08-2199 [DOI] [PubMed] [Google Scholar]
- 20.Feldman J, Barshi I: The Effects of Blood Glucose Levels on Cognitive Performance: a Review of Literature. Moffett Field, California, NASA Ames Research Center, 2007(NASA/TM-2007–214555) [Google Scholar]
- 21.Hartz A, Kent S, James P, Xu Y, Kelly M, & Daly J (2006). Factors that influence improvement for patients with poorly controlled type 2 diabetes. Diabetes Research and Clinical Practice, 74(3), 227–232. 10.1016/j.diabres.2006.03.023 [DOI] [PubMed] [Google Scholar]
- 22.Palta P, Huang E, Kalyani R, Golden S. Hemoglobin A1c and Mortality in Older Adults With and Without Diabetes: Results From the National Health and Nutrition Examination Surveys (1988–2011). Diabetes Care 2017April; 40(4): 453–460. 10.2337/dci16-0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher-Hoch SP, Vatcheva KP, Rahbar MH, McCormick JB. Undiagnosed diabetes and pre-diabetes in health disparities. PLoS One. 2015July17; 10(7): e0133135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dwyer-Lindgren L, Mackenbach JP, van Lenthe FJ, Flaxman AD, Mokdad AH. Diagnosed and undiagnosed diabetes prevalence by county in the US, 1999–2012. Diabetes Care. 2016; 39: 1556–1562 [DOI] [PubMed] [Google Scholar]
- 25.Flint KL, Davis GM, Umpierrez GE (2019) Emerging trends and the clinical impact of food insecurity in patients with diabetes. J Diabetes. 12(3): 187–196. 10.1111/1753-0407. [DOI] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey. Accessible at: https://www.cdc.gov/nchs/nhanes/index.htm Accessed onNov 3, 2017.
- 27.National Center for Health Statistics (NCHS). National Health and Nutrition Examination Datasets. Accessible at: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx Accessed onNov 3, 2017
- 28.Shi L, Tsai J, Kao S. Public health, social determinants of health, and public policy. J Med Sci. 2009; 29(2): 43–59. [Google Scholar]
- 29.Seligman H (2010). Hunger and Socioeconomic Disparities in Chronic Disease — NEJM. Retrieved September 29, 2017, from http://www.nejm.org/doi/full/10.1056/NEJMp1000072 [DOI] [PubMed]
- 30.Mainous AG 3rd, Tanner RJ, Anton SD, Jo A, Luetke MC. Physical Activity and Abnormal Blood Glucose Among Healthy Weight Adults. Am J Prev Med. 2017July;53(1):42–47. 10.1016/j.amepre.2016.11.027.Epub 2017 Jan 19. [DOI] [PubMed] [Google Scholar]
- 31.Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Normal weight obesity: a risk factor for cardio-metabolic dysregulation and cardiovascular mortality. Eur Heart J. 2010; 31: 737–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Selvin E, Wang D, Lee AK, Bergenstal RM, Coresh J. Identifying Trends in Undiagnosed Diabetes in U.S. Adults by Using a Confirmatory Definition: A Cross-sectional Study. Ann Intern Med. [Epub ahead of print24October2017]:. 10.7326/M17-1272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edwards WS, Winn DM, Kurlantzick V, Sheridan S, et al. Vital health statistics 2: evaluation of National Health Interview Survey diagnostic reporting. Retrieved from National Center for Health Statistics, 1994. [Google Scholar]
- 34.Bowlin SJ, Morrill BD, Nafziger AN, Lewis C, & Pearson TA. Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: The behavioral risk factor survey. J Clin Epidemiol 1996;49:511–517. [DOI] [PubMed] [Google Scholar]


