Abstract
Background
Lack of awareness of the taxonomic revision from the familiar Streptococcus bovis to the less familiar Streptococcus gallolyticus may be associated with a decrease in recommended colon cancer screening in patients with bacteremia from this organism. This could subsequently lead to a delay in diagnosis or underdiagnosis of colon cancer and other serious underlying gastrointestinal diseases. The aim of this study was to determine whether the nomenclature change of S. bovis to S. gallolyticus resulted in decreased colon cancer screening.
Methods
This study was a retrospective, observational, nationwide analysis of patients who had positive blood cultures for S. bovis/S. gallolyticus from any Veterans Affairs Medical Center (VAMC) between January 1, 2002, and December 31, 2017.
Results
There was no difference in the primary end point of intent for colonoscopy between the S. gallolyticus and S. bovis groups (66.5% [117/176] vs 62.1% [624/1005], respectively; P = .26). The overall mortality rate was 33.8% among 1181 patients included in the study, with a significantly lower mortality in patients with evidence of intent for colonoscopy (29.6% vs 42.5%; P ≤ .001), gastroenterology (GI) consultation (29.8% vs 41.4%; P < .001), infectious diseases (ID) consultation (29.4% vs 39.0%; P = .001), or either consultation (31.9% vs 40.7%; P = .013), compared to those that did not.
Conclusions
There was no difference in colon cancer screening rates between patients with episodes of bacteremia reported as S. bovis and those reported as S. gallolyticus. Overall mortality was lower in patients who had ID consultation, GI consultation, or evidence of colonoscopy.
Keywords: bacteremia, colon cancer, colonoscopy, Streptococcus bovis, Streptococcus gallolyticus
Klein and colleagues demonstrated a strong association linking Streptococcus bovis bacteremia with the presence of colorectal cancer in 1977 following several case reports that described episodes of S. bovis bacteremia associated with colorectal carcinoma and other gastrointestinal diseases [1, 2]. Since then, several reports have supported the relationship between isolation of S. bovis in the bloodstream and colorectal malignancy. Many have also shown an association with a number of other gastrointestinal conditions including inflammatory bowel disease, diverticular disease, and gastrointestinal bleeding, as well as hepatobiliary abnormalities [3, 4]. Due to these associations of S. bovis with colorectal malignancy and other gastrointestinal abnormalities, the Infectious Diseases Society of America (IDSA) guidelines recommend that patients found to have bacteremia from this organism be evaluated with a colonoscopy [5].
Several hypotheses about the mechanisms that underlie the association between S. bovis and malignancy have been proposed. Most theories favor that the organism itself leads to cellular changes that can cause premalignant lesions to develop into malignancy. More specifically, these mechanisms include proinflammatory changes causing cytokine release and the induction of mutations in tumor suppressor genes or oncogenes. Other contributing mechanisms include carcinogenesis due to destabilization of normal colonic flora and the induction of uncontrolled cellular proliferation [6]. In 2003, several authors proposed reclassification of S. bovis biotypes I, II/1, and II/2 based on genotypic studies and phylogenetic data. Consequently S. bovis biotype I and II/2, the biotypes most strongly associated with colorectal malignancy, were renamed Streptococcus gallolyticus [7]. Shortly thereafter, van’t Wout and Bijlmer noted that the taxonomic changes could have deleterious effects on the evaluation and management of S. bovis/S. gallolyticus bacteremias due to lack of awareness, which could lead to the underdiagnosis of colon cancer and other serious underlying gastrointestinal diseases. The authors proposed that the old name for the bacteria be reported along with the new name to prevent confusion [8]. Additional authors have continued to express the concern that the new name for S. bovis biotypes may not be familiar to providers [9, 10]. To the best of our knowledge, no studies have been undertaken to assess whether this taxonomic change influenced patient management, specifically compliance with the recommendation for colon cancer screening in bacteremic patients. The aim of this study was to determine whether the nomenclature change of S. bovis to S. gallolyticus led to a decrease in recommended colon cancer screening in these patients, utilizing a nationwide clinical database in the Veterans Health Administration.
METHODS
Eligible patients ≥18 years of age were included in the study with data collected through the Veterans Affairs Informatics and Computing Infrastructure (VINCI) database across all Veterans Affairs Medical Centers (VAMC) in the United States. Patients were assigned a de-identified patient identification number (“PatientSID”) within VINCI, making them un-identifiable by the investigators. Investigators accessed VINCI from a secure, password-protected computer intranet at the Oklahoma City VAMC. Baseline demographic data, diagnosis codes, admission, discharge, and microbiological data were collected. An order for a colonoscopy and/or a gastroenterology (GI) consultation was a surrogate marker for acknowledgement of the need for colon cancer workup and was referred to as “intent for colonoscopy.” For this retrospective study, our Institutional Review Board approved waiver of patient consent.
Data Collection and Definitions
This study was a retrospective, observational, nationwide analysis of patients who had positive blood cultures for S. bovis/S. gallolyticus from any VAMC between January 1, 2002, and December 31, 2017. We excluded patients who had S. bovis/S. gallolyticus isolated from sites that were not associated with concomitant bacteremia. Microbiology records were examined to determine whether the organism was identified as S. bovis or S. gallolyticus in the report. If any attempt (such as both names presented in the organism’s name field) was made to inform the clinician that S. gallolyticus was formerly called S. bovis, the patient was placed into the S. bovis group. Identifications were performed on various platforms including BioMerieux Vitek2, BD Phoenix, and matrix-assisted laser desorption ionization time of flight (MALDI-ToF) mass spectrometers. The S. gallolyticus group included organisms identified and reported as S. gallolyticus and S. gallolyticus subspecies (subsp. pasteurianus, subsp. gallolyticus), S. infantarius and S. infantarius subspecies (subsp. infantarius, subsp. coli, subsp. lutetiensis), S. pasteurianus, and S. lutetiensis. Further reference to “S. gallolyticus” includes these specific species and subspecies. Records were searched for any evidence that a colonoscopy or GI consult was requested from the date of the positive blood culture up to 1 year from that date by searching for a specific Current Procedural Terminology (CPT) code for a colonoscopy or a GI consultation request. The first date of such evidence was recorded. Patient disposition (ie, mortality) up to 1 year from the date of the positive blood culture was recorded.
The primary outcome was evidence of colonic evaluation or GI consultation within 90 days of a positive blood culture. Secondary outcomes included request for infectious diseases (ID) consultation, request for GI consultation, and all-cause mortality within 1 year. The primary and secondary outcomes were also delineated by age (≥75 years vs <75 years), and were further delineated by excluding early death (defined as death within 14 days from the date of first positive blood cultures and presumed to be infection-related or due to other complications).
Statistical Analysis
The Wilcoxon/Kruskal-Wallis test was used for continuous variables. Chi-square likelihood ratios were reported for categorical data. A P value of ≤.05 was considered statistically significant. Univariate variables associated with the intent to perform colonoscopy were identified. Those variables with a P value of ≤.1 were entered into nominal logistic multivariate analysis to determine the independent variables associated with the intent to perform colonoscopy.
RESULTS
After exclusion of Streptococcus species other than S. bovis or S. gallolyticus, 1181 unique cases of bacteremia due to either S. bovis (n = 1005) or S. gallolyticus (n = 176) were included from 102 Veterans Affairs (VA) sites. Out of the 1005 episodes included in the S. bovis group, 53 positive blood cultures (5.3%) from 7 VA sites were reported as S. gallolyticus with mention of the former name of S. bovis in the report. The 2 groups were largely comparable, except that patients with S. gallolyticus bacteremia were slightly older (Table 1).
Table 1.
Patient Characteristics of S. bovis and S. gallolyticus Groups
| S. bovis | S. gallolyticus | Total | P Value | |
|---|---|---|---|---|
| n = 1005 | n = 176 | n = 1181 | ||
| Male gender, % (No.) | 98.5 (990) | 98.30 (173) | 98.48 (1163) | .83 |
| Race/ethnicity, % (No.) | .27 | |||
| White | 65.77 (661) | 67.61 (119) | 66.05 (780) | |
| Black | 13.83 (139) | 11.93 (21) | 13.55 (160) | |
| Hispanic or Latino | 7.96 (80) | 11.36 (20) | 8.47 (100) | |
| Othera | 12.44 (125) | 9.09 (16) | 11.94 (141) | |
| Age, y | 71.8 | 74.0 | 72.1 | .033 |
aAmerican Indian or Alaskan Native, Native Hawaiian or Pacific Islander, Asian, unknown.
Primary Outcome
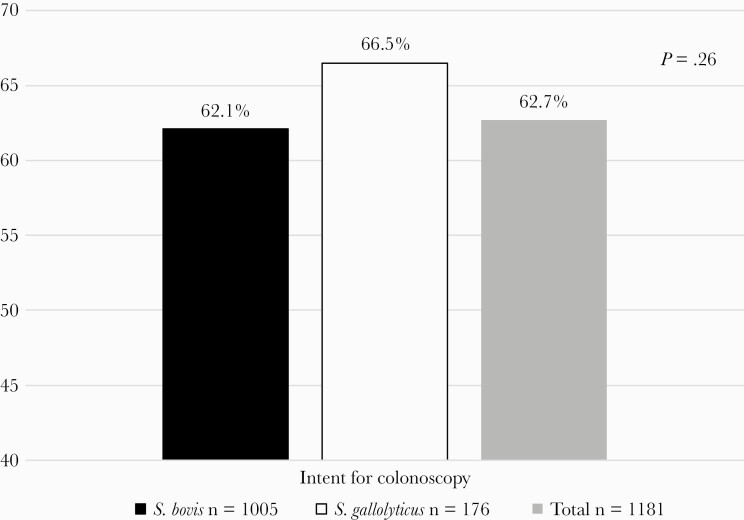
Evidence of intent for colonoscopy was present in 62.7% (741/1181) of patients. There was no statistically significant difference in the rate of intent for colonoscopy between the S. gallolyticus group and the S. bovis group (66.5% [117/176] vs 62.1% [624/1005], respectively; P = .26) (Figure 1). Similarly, no difference between groups was found in patients age <75 years (69.8% [67/96] vs 61.9% [336/543]; P = .13) or patients age ≥75 years (62.5% [50/80] vs 62.3% [288/462]; P = .98). One hundred twenty-one patients died within 14 days of diagnosed bacteremia; after excluding these patients, there was still no difference in the intent for colonoscopy between the S. gallolyticus group and the S. bovis group (69.3% [115/166] vs 67.6% [604/894], respectively; P = .66).
Figure 1.
Primary end point of colonoscopy in S. bovis and S. gallolyticus groups.
Secondary End Points
There was no statistically significant difference in the rate of GI consults within 90 days between the S. gallolyticus group (65.3% [115/176]) and the S. bovis group (60.2% [605/1005]; P = .19). After excluding those patients who died within the first 14 days of bacteremia, there was still no difference in the rate of GI consultation (68.1% [113/166]) in the S. gallolyticus group vs the S. bovis group (65.4% [585/894]; P = .51). The rate of GI consultation did not differ between the S. gallolyticus group and the S. bovis group in patients aged ≥75 years (62.5% [50/80] vs 61.7% [285/462]; P = .89) and in patients <75 years of age (67.7% [65/96] vs 58.9% [320/543]; P = .10).
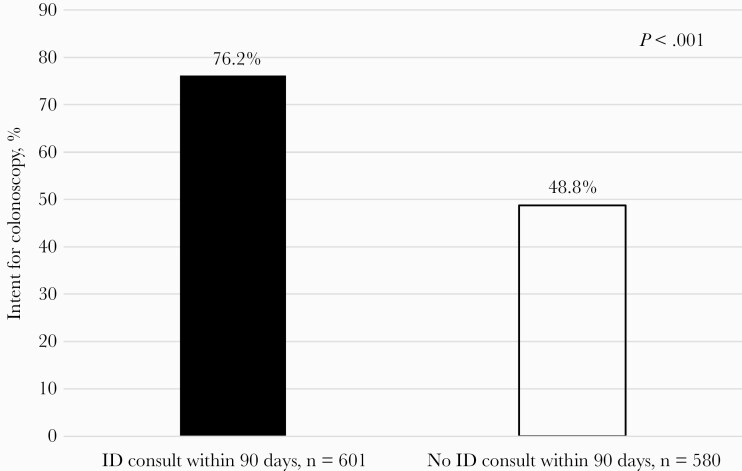
Infectious Diseases consultation occurred in 601 (50.9%) patients. Patients who had an ID consult had a higher rate of evidence of intent for colonoscopy (76.2% [458/601]) vs patients who did not have an ID consult (48.8% [283/580]; P < .001), regardless of reported name of bacteria (Figure 2). In those patients who were still alive at 15 days after bacteremia diagnosis, there was a higher number of ID consults in the S. gallolyticus group compared with the S. bovis group (65.7% [109/166] vs 52.8% [472/894]; P = .002).
Figure 2.
Infectious diseases consultation and intent for colonoscopy in combined S. gallolyticus and S. bovis groups. Abbreviation: ID, infectious diseases.
There was a significantly higher rate of ID consultations in the S. gallolyticus group compared with the S. bovis group in patients age ≥75 years (61.2% [49/80] vs 48.7% [225/462]; P = .037) and those <75 years of age (65.6% [63/96] vs 48.6% [264/543]; P = .019). There was an overall higher consult rate (GI or ID) in the S. gallolyticus group vs the S. bovis group (84.9% [141/166] vs 77.5% [693/894]; P = .027).
In patients who did not have an ID consult, there was no difference in the rate of GI consults between groups in the S. gallolyticus and S. bovis groups (50% [35/70] and 44.7% [195/436], respectively; P = .41). Bacteremias reported as S. gallolyticus prompted more ID consults than those reported as S. bovis (63.6% [112/176] vs 48.7% [489/1005]; P < .001). The S. gallolyticus group had a higher number of combined GI and ID consults (83.0% [146/176]) than the S. bovis group (72.1% [725/1005]; P = .002).
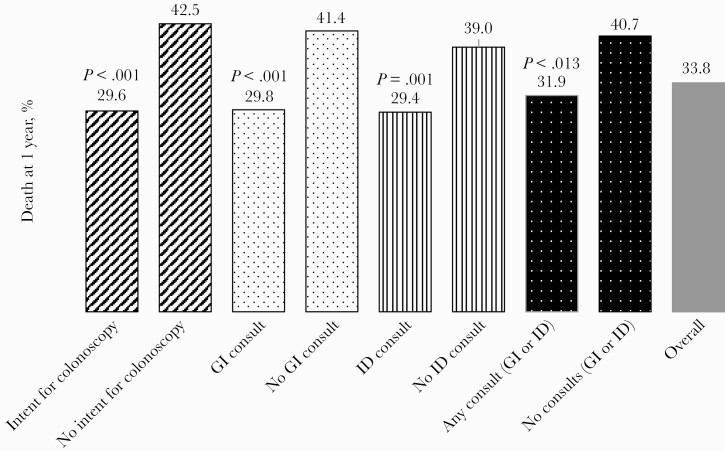
There was no difference in mortality between the S. gallolyticus (38.1% [67/176]) and S. bovis (41.0% [412/1005]) groups (P = .47). There was no difference in mortality between the S. gallolyticus and S. bovis groups in those age ≥75 years (51.2% [41/80] vs 47.2% [218/462]; P = .50) and those age <75 years (27.1% [26/96] vs 35.7% [195/543]; P = .095). In the first 14 days after the first positive blood culture for S. bovis/S. gallolyticus, 121 patients died. After exclusion of the 121 patients, there was an overall mortality of 33.8% (358/1060), with a significant lower mortality in those patients who had evidence of intent for colonoscopy (29.6% [213/719]) vs those who did not (42.5% [145/341]; P ≤ .001) GI consult (29.8% [208/698]) vs no GI consult (41.4% [150/362]; P < .001), ID consult (29.4% [171/581]) vs no ID consult (39.0% [187/479]; P = .001), or either GI or ID consult (31.9% [266/834]) vs no consult (40.7% [92/226]; P = .013) (Figure 3).
Figure 3.
All-cause mortality at 1 year in patients surviving the first 14 days of bacteremia. Abbreviations: GI, gastrointestinal; ID, infectious diseases.
There was no increase in the level of compliance to order a colonoscopy in the years following the nomenclature change compared with years prior (P = .61). There was no significant delay in ordering of a GI consult or colonoscopy based on organism name. The median number of days from diagnosis of bacteremia to date of colonoscopy order was 9.11 days in the S. gallolyticus group and 8.74 days in the S. bovis group (P = .96).
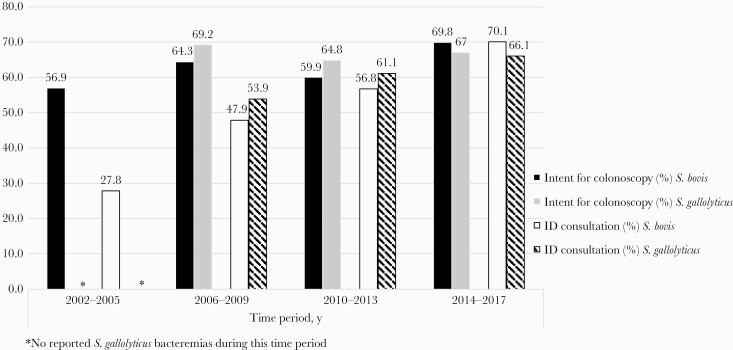
Univariate analysis revealed that the presence of an ID consult, Hispanic or Latino ethnicity, and the time period of bacteremia diagnosis (Table 2, Figure 4) were associated with intent for colonoscopy. Multivariate analysis showed that patients who received an ID consult or who were Hispanic or Latino were independently associated with intent for colonoscopy (Table 3). Intent for colonoscopy and ID consultation were significantly higher in the years after 2005 as compared with the time period of 2002–2005 (Figure 4).
Table 2.
Univariate Variables Associated With Intent for Colonoscopy
| Variable | No. (%) With Evidence for Intent for Colonoscopy | P Value |
|---|---|---|
| Gender | .27 | |
| Male | 732/1163 (62.9) | |
| Female | 9/18 (50.0) | |
| Age | .80 | |
| ≥75 y | 338/542 (62.4) | |
| <75 y | 403/639 (63.1) | |
| Hispanic or Latino race/ethnicity | .003 | |
| Yes | 76/100 (76.0) | |
| No | 665/1081 (61.5) | |
| White race | .18 | |
| Yes | 500/780 (64.1) | |
| No | 241/401 (60.1) | |
| Black race | .55 | |
| Yes | 97/160 (60.6) | |
| No | 644/1021 (63.1) | |
| Organism nomenclature | .26 | |
| Streptococcus bovis | 624/1005 (62.1) | |
| Streptococcus gallolyticus | 117/176 (66.5) | |
| Period of bacteremic episode | .028 | |
| 2002–2005 | 145/255 (56.9) | |
| 2006–2009 | 198/307 (64.5) | |
| 2010–2013 | 205/338 (60.6) | |
| 2014–2017 | 193/281 (68.7) | |
| Infectious diseases consult | <.001 | |
| Yes | 458/601 (76.2) | |
| No | 283/580 (48.8) |
Figure 4.
Increase in intent for colonoscopy and ID consultation in S. bovis and S. gallolyticus groups over time. Abbreviation: ID, infectious diseases.
Table 3.
Independent Variables Associated with Intent of Colonoscopy
| Variable | Relative Risk (95% CI) | P Value |
|---|---|---|
| Infectious diseases consult | 1.57 (1.46–1.66) | <.001 |
| Hispanic or Latino race/ethnicity | 1.21 (1.04–1.34) | .016 |
DISCUSSION
Colonoscopy rates for patients who are diagnosed with S. bovis/S. gallolyticus bacteremia range widely from 33% to 77% [9, 11, 12]. Even in cases where the more familiar species name of S. bovis is reported, thorough workup for gastrointestinal malignancy may not be performed, which could lead to detrimental and potentially preventable outcomes [10]. Based on concern that providers may not be as familiar with the name change of S. bovis biotypes to S. gallolyticus initially described by van’t Wout and Bijlmer [8], we hypothesized that patients who had bacteremias reported as S. gallolyticus may be less likely to have a colonoscopy compared with when the bacteremia was reported as S. bovis. However, we found no difference in the rate of intent for colonoscopy between the S. gallolyticus and S. bovis groups. Interestingly, the S. gallolyticus group had significantly more ID consults than the S. bovis group, and multivariate analysis showed that patients who received an ID consult were independently associated with intent for colonoscopy, with an odds ratio of 3.4. It is possible that the primary provider’s unfamiliarity with the S. gallolyticus nomenclature could have prompted more ID consults. Infectious diseases providers are more likely to be aware of changes in microbiology nomenclature, which could have led to appropriate colon cancer screening in the S. gallolyticus group despite the relatively unfamiliar name. Conversely the fact that orders for colonoscopies increased over time, could also be an indication that primary providers may have become more aware of the need for GI evaluation over time. In addition, we saw an overall increase in ID consultation and GI consultation, as well as an increase in colonoscopy orders over the years (2002–2017), which could have contributed to the increase in colonoscopies in the S. gallolyticus group. Overall, there was no difference in rate of GI consultation between the 2 groups. Again, this may be due to the fact that there were more ID consults in the S. gallolyticus group, possibly leading to more GI consults and subsequent colonoscopies in the S. gallolyticus group and resulting in no difference between groups. In patients who had an ID consult, there was a higher intent for colonoscopy than in those without an ID consult, regardless of the reported name of the bacteria.
Total all-cause mortality was high at 40.6% (479/1181), but there was no difference in mortality between the S. bovis and S. gallolyticus groups. After exclusion of 121 patients who had died in the first 14 days, there was a significant decrease in overall mortality of the 1060 remaining patients if they had evidence of intent for colonoscopy, GI consultation, ID consultation, or any consultation compared with those patients who did not, suggesting that ID and GI consultations in patients with S. bovis/S. gallolyticus bacteremia are associated with lower mortality. ID consultation has been illustrated to decrease mortality in patients suffering from a number of infections such as those caused by multidrug-resistant organisms [13] and Staphylococcus aureus [14] and in enterococcal bacteremias [15]. Though we did not investigate specific causes of mortality, based on these studies, appropriate antimicrobial agent use, duration of therapy, and identification and control of the source of bacteremia may explain this finding.
There are several limitations to this study. First and foremost, the organisms assigned to the S. bovis group and classification of S. bovis biotypes and S. bovis subspecies are very inconsistent in the literature. Several different streptococcal species such as Streptococcus equinis have been included in the S. bovis group by some authors but not all. In addition, when an organism such as S. bovis/S. gallolyticus is reclassified and subsequently renamed, there is no specific document where this information is published; thus there is no specific time or date that an organism is “renamed.” As a result, different laboratories adopt the revised name at different times. Furthermore, for the information to disseminate to health care providers, it requires that they read educational materials or published literature that uses the new name of the organism or rely on laboratories or other providers to educate them. Another limitation was the inability to gather certain data within our VINCI clinical administrative database that could have affected results. For instance, we were unable to see if a referral was made to gastroenterologists outside the VA for further gastrointestinal workup after a result of S. bovis/S. gallolyticus was acknowledged. We were also unaware of any “curbside” consults regarding the clinical significance of S. bovis/S. gallolyticus to either the infectious diseases service or gastroenterology service, which may have triggered further workup. Of note, 18 out 102 sites did not have any of their bacteremic cases result in ID consultation; however, 12 of these sites had only 1 or 2 bacteremic episodes. It is likely that many of these 18 sites did not have ID consultation available. Lastly, there may be alternative mechanisms that microbiology laboratories use to communicate nomenclature updates in their reports that may have been missed by our methods of data collection. For instance, we were unable to see the text portion of blood culture reports, which may have contained the former and more familiar name of S. bovis. These factors could have contributed to a lack of difference in the screening rates between the 2 groups.
Although a difference in screening rates between both the S. bovis and S. gallolyticus groups was not seen in the current study, the proposal to include both the old and revised names of S. bovis/ S. gallolyticus by all laboratories in United States, including the VA Healthcare Network, with a statement or other form of communication to the provider recommending workup for colorectal malignancy would appear beneficial. Further clarification of the role and importance of distinguishing S. bovis biotypes to fully understand their relationships with different gastrointestinal and other associated pathologies is needed, as well as appropriate education to providers on the recommendations to pursue screening for individuals with S. bovis/S. gallolyticus bacteremia. Notably, colon cancer screening guidelines by the American Cancer Society, American College of Gastroenterology, and United States Preventative Task Force do not recognize S. bovis/S. gallolyticus as a risk factor for colon cancer despite the abundance of evidence illustrating the relationship. We suggest guidelines to incorporate this pathogen as risk factor for colon cancer. In addition, we hope that this study will educate providers on the nomenclature revision of S. bovis/S. gallolyticus and encourage providers to be aware of new evidence and recommendations in the medical literature, particularly when they lead to a change in management that directly impacts patient morbidity and mortality.
CONCLUSIONS
No statistically significant difference in colon cancer screening rates between patients with bacteremias reported as S. bovis vs S. gallolyticus was found. There was a decrease in overall mortality in all S. bovis/S. gallolyticus bacteremic patients who had an ID consult, GI consult, or evidence of colonoscopy.
Acknowledgments
This material is the result of work supported with the resources and use of facilities at the Veterans Affairs Health Care System (Oklahoma City, OK, USA) and the VHA Corporate Data Warehouse.
Author contributions. S.T. and C.G. contributed to the study design and data analysis. S.T. and C.G. contributed to the drafting of the manuscript. S.T., C.G., and D.S. participated in editing and finalizing the manuscript. All authors read and approved the final manuscript.
Patient consent. For this retrospective study, our Institutional Review Board approved waiver of patient consent. The “Methods” section has been updated to incorporate this information.
Financial support. No external funding was received for this study.
Potential conflicts of interest. The authors declare that they have no conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Klein RS, Recco RA, Catalano MT, et al. Association of Streptococcus bovis with carcinoma of the colon. N Engl J Med 1977; 297:800–2. [DOI] [PubMed] [Google Scholar]
- 2.Hoppes WL, Lerner PI. Nonenterococcal group-D streptococcal endocarditis caused by Streptococcus bovis. Ann Intern Med 1974; 81:588–93. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Frodl R, Funke G. Comprehensive study of strains previously designated Streptococcus bovis consecutively isolated from human blood cultures and emended description of Streptococcus gallolyticus and Streptococcus infantarius subsp. coli. J Clin Microbiol 2008; 46:2966–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boleij A, van Gelder MM, Swinkels DW, Tjalsma H. Clinical importance of Streptococcus gallolyticus infection among colorectal cancer patients: systematic review and meta-analysis. Clin Infect Dis 2011; 53:870–8. [DOI] [PubMed] [Google Scholar]
- 5.Baddour LM, Wilson WR, Bayer AS, et al. ; American Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young, Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Stroke Council. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015; 132:1435–86. [DOI] [PubMed] [Google Scholar]
- 6.Abdulamir AS, Hafidh RR, Abu Bakar F. The association of Streptococcus bovis/gallolyticus with colorectal tumors: the nature and the underlying mechanisms of its etiological role. J Exp Clin Cancer Res 2011; 30:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schlegel L, Grimont F, Ageron E, et al. Reappraisal of the taxonomy of the Streptococcus bovis/Streptococcus equinus complex and related species: description of Streptococcus gallolyticus subsp. gallolyticus subsp. nov., S. gallolyticus subsp. macedonicus subsp. nov. and S. gallolyticus subsp. pasteurianus subsp. nov. Int J Syst Evol Microbiol 2003; 53:631–45. [DOI] [PubMed] [Google Scholar]
- 8.van’t Wout JW, Bijlmer HA. Bacteremia due to Streptococcus gallolyticus, or the perils of revised nomenclature in bacteriology. Clin Infect Dis 2005; 40:1070–1. [DOI] [PubMed] [Google Scholar]
- 9.Fernández-Ruiz M, Villar-Silva J, Llenas-García J, et al. Streptococcus bovis bacteraemia revisited: clinical and microbiological correlates in a contemporary series of 59 patients. J Infect 2010; 61:307–13. [DOI] [PubMed] [Google Scholar]
- 10.Ferrari A, Botrugno I, Bombelli E, et al. Colonoscopy is mandatory after Streptococcus bovis endocarditis: a lesson still not learned. Case report. World J Surg Oncol 2008; 6:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarovitch T, Shango M, Levine M, et al. The relationship between the new taxonomy of Streptococcus bovis and its clonality to colon cancer, endocarditis, and biliary disease. Infection 2013; 41:329–37. [DOI] [PubMed] [Google Scholar]
- 12.Corredoira JC, Alonso MP, García-País MJ, et al. Is colonoscopy necessary in cases of infection by Streptococcus bovis biotype II? Eur J Clin Microbiol Infect Dis 2014; 33:171–7. [DOI] [PubMed] [Google Scholar]
- 13.Burnham JP, Olsen MA, Stwalley D, et al. Infectious diseases consultation reduces 30-day and 1-year all-cause mortality for multidrug-resistant organism infections. Open Forum Infect Dis 2018; 5:XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson JO, Pozzi-Langhi S, Phillips M, et al. Formal infectious diseases consultation is associated with decreased mortality in Staphylococcus aureus bacteraemia. Eur J Clin Microbiol Infect Dis 2012; 31:2421–8. [DOI] [PubMed] [Google Scholar]
- 15.Lee RA, Vo DT, Zurko JC, et al. Infectious diseases consultation is associated with decreased mortality in enterococcal bloodstream infections. Open Forum Infect Dis 2020; 7:XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]