Abstract
Introduction
Children and adolescents with cerebral palsy may be trapped in a vicious circle of low physical fitness, resulting in deconditioning that causes a further decrease in physical activity (PA), a lower quality of life and an increased risk of developing non-communicable diseases. Therefore, establishing a healthy and active lifestyle during childhood is even more important for individuals with a disability. However, the factors that influence habitual PA in children and adolescents with cerebral palsy remain unknown.
The present protocol outlines a prospective cohort study with the aim of investigating potential predictors of habitual PA in children and adolescents with cerebral palsy in order to provide evidence for optimising PA levels and associated overall health.
Methods and analysis
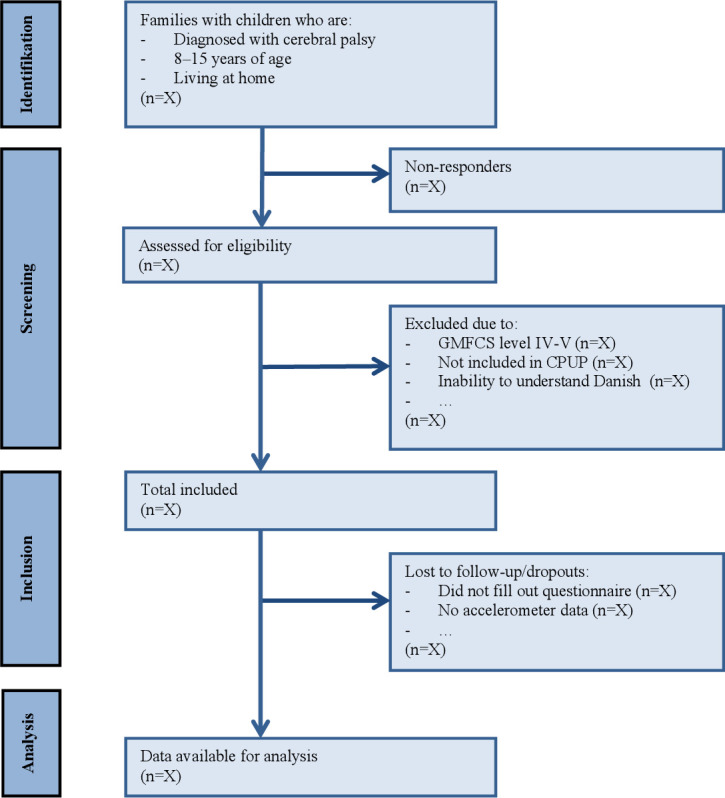
This prospective cohort study will enrol participants with cerebral palsy between the ages of 8 and 15 years at Gross Motor Function Classification System levels I–III. Using a modified version of the International Classification of Functioning, Disability and Health model as a conceptual analytical framework, the analysis will be divided into six components and will provide predictors for habitual PA measured by accelerometry. The potential predictive variables are registry data on physical function (Danish Cerebral Palsy Follow-Up Programme); validated proxy-reported questionnaires on quality of life (Paediatric Quality of Life Inventory), overall health, pain and participation in daily activities (Paediatric Outcomes Data Collection Instrument) and supplementary questions regarding sleep, screen time and socioeconomic status.
Ethics and dissemination
The project is approved by the Danish Data Protection Agency (19/16396) and has been declared not notifiable by the Regional Committee on Health Research Ethics, cf. Committee Act Art. 14, paragraph 1 (S-20192000-23). The study results will be published in international peer-reviewed journals, presented at international conferences, and published in a PhD dissertation.
Trial registration number
Keywords: musculoskeletal disorders, developmental neurology & neurodisability, epidemiology
Strengths and limitations of this study.
The study will provide novel evidence that will aid identification of physical activity (PA) levels and patterns in children and adolescents with cerebral palsy for early intervention.
The findings may be implemented in evidence-based PA guidelines, which currently are lacking for children and adolescents with cerebral palsy.
Bootstrap validation will be performed to increase internal validation. Optimally, external validity of the findings should be verified in the future using an external cohort.
Introduction
Cerebral palsy
Cerebral palsy (CP) is a condition that describes a group of disorders (altered muscle tone, movement disorders, muscle weakness, ataxia and rigidity) related to the development of movement and posture causing activity limitations and reduced quality of life (QoL).1 CP is a common impairment among children, with a prevalence of 2.1 per 1000 live births worldwide2 and 2.4 per 1000 live births in Denmark.3 CP is attributed to non-progressive disturbances in the fetal central nervous system or in the developing infant within the first 2 years of life.1 4 Although CP is a non-progressive diagnosis, it is a lifelong condition that requires attention through most of the person’s life, as impairments are constantly evolving and inhibit performance of activities and participation in daily living.1 5
Physical activity
Low levels of physical activity (PA) are a worldwide threat to the health of children, including those with disabilities. For this reason, WHO recommends children to be moderate to vigorous physical active for at least 60 min per day, including muscle-strengthening and bone-strengthening activities at least 3 days per week.6 Although there are no specific evidence-based PA guidelines for children with CP, it is clear that they have lower levels of PA and higher levels of time spent sedentary than their peers7 and that their level of mobility limitation is negatively associated with their level of PA.8
The long-term effects of reduced habitual PA and increased sedentary time include a greater risk of developing non-communicable diseases such as metabolic dysfunction, cardiovascular disease and poor bone density. These problems can, in turn, result in poorer overall health, reduced life expectancy and a greater burden of disease in years of life lost to disability.9 10 Furthermore, evidence suggests that more than 25% of adults with CP experience mobility decline, for some resulting in persistent loss of independent gait function, thus, emphasising the importance of maintaining a physical active lifestyle throughout childhood and adolescence.11 Ideally, childhood should be marked by high levels of intense play and habitual PA, which, in addition to providing protective physical benefits, also appears to improve mental health.12 13
Predictors of PA
In Scandinavia, healthcare professionals offer standardised clinical examinations throughout childhood using the Cerebral Palsy Follow-Up Programme (CPUP), which was developed in Sweden more than 20 years ago14 and was adopted in Denmark as a National Clinical Quality Database by the Danish Clinical Registries in 2015. CPUP is designed to support early detection of complications, such as hip dislocation, scoliosis and muscle contracture, as well as to improve the quality of healthcare.14 15 Danish clinical guidelines for physiotherapy and occupational therapy for children with CP emphasise that future research should focus on the short-term and long-term effects of the interventions applied to improve the children’s activities of daily living.16 Despite this recommendation, it has not been investigated whether the standardised examinations and accompanying variables of CPUP are associated with habitual PA. Thus, potential objective predictors of PA can be identified through this national clinical quality database, allowing early detection and potentially improved interventions.
To optimise activities of daily living and long-term health outcomes for the present population, a key objective is to encourage and facilitate an increase in habitual PA and reduce the amount of time spent sedentary.7 However, the current literature does not provide evidence for barriers to or motivators for PA in children and adolescents with CP. Furthermore, no studies have examined the underlying reasons for altering habitual PA.
Aim and hypothesis
The aim of the present cohort study is to identify and investigate potential predictors of habitual PA in children and adolescents with CP, with the perspective of providing evidence to optimise PA levels and associated overall health.
We hypothesise that potential predictors of habitual PA can be identified through objective variables included in the CPUP database and in supplementary questionnaires on proxy-reported outcome measures, using a modified International Classification of Functioning, Disability and Health (ICF) model (Body Functions and Structures, Activities, Participation, Personal Factors, Environmental Factors and QoL) as a conceptual statistical framework.
Methods and analysis
Study design
A prospective clinical cohort study using historical registry data from CPUP and supplementary proxy-reported outcome measures will be conducted. The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist for reporting cohort studies will be used to report the study findings.17 Enrolment commenced on 3 November 2020 and is expected to end by December 2021.
Ethics and dissemination
The project has been approved by the Danish Data Protection Agency (19/16396) and has been declared not notifiable by the Regional Committee on Health Research Ethics, cf. Committee Act Art. 14, paragraph 1 (S-20192000-23). The Danish Clinical Registries granted access to the CPUP database in June 2019.
The project will be conducted in accordance with the Declaration of Helsinki II. Before participants (parents/guardians) give their informed written consent to take part in the study, they will receive written and oral information on the experimental procedure and potential risks. The families will be informed that they can withdraw from the study at any time. All subject data will be treated confidentially and in confidence according to the European Union’s General Data Protection Regulation.
The study results, whether positive, negative or inconclusive, will be published in international peer-reviewed journals, presented at international conferences and published in a PhD dissertation. The articles and presentation will not contain any information that could lead to identification of any participants.
Participants and study setting
Participants will be recruited from the five regions of Denmark.
To increase the external validity and sample size of the present project, the inclusion criteria will include children and adolescents of 8–15 years (born between 1 January 2003 and 31 December 2013) who are diagnosed with CP. Inclusion via invitation commenced on 3 November 2020.
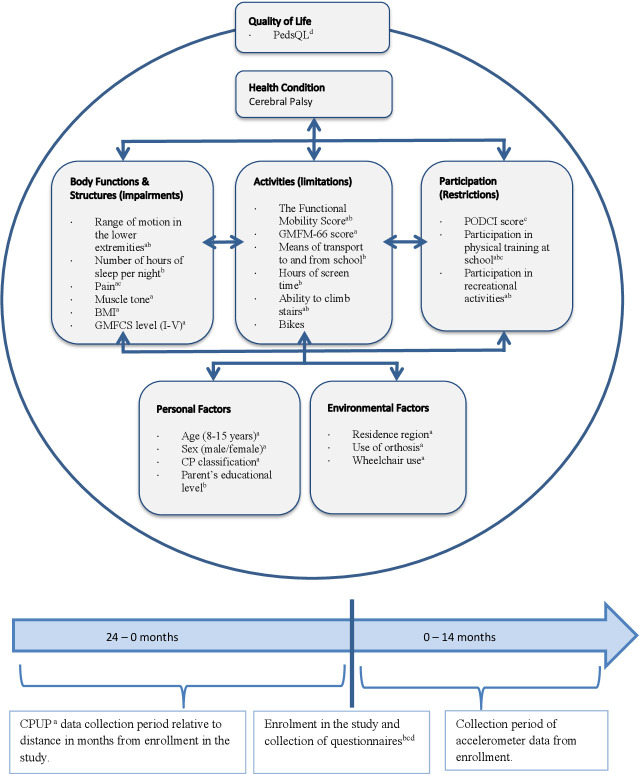
The children/adolescents must be registered in the Danish CPUP and classified at Gross Motor Function Classification System (GMFCS) levels I–III, demonstrating an independent gait function with or without mobility devices. A flow diagram of participants through the study is illustrated in figure 1. Parents/guardians must be able to read and understand Danish.
Figure 1.
Flow diagram. GMFCS, Gross Motor Function Classification System.
Eligible participants will be identified through the Danish Health Data Authority, after which the parents/guardians will receive written information through secure digital post (e-Boks). If clarification is needed, the project manager can be contacted via telephone or email. Interested parents/guardians will consent electronically via personal link in e-Boks and will automatically be forwarded the questionnaires, which will be filled out electronically. For non-responders, an email reminder will be sent out a total of three times. Habitual PA is to be measured using accelerometers (see below for further description). Participants will receive an accelerometer via postal mail, including a prepaid return envelope.
Data sources and measurements
Parents’/guardians’ perceptions of their child’s activity behaviour, health status, sociodemographic background, sleep and screen habits will be collected in an electronic questionnaire. Demographic characteristics (age, sex, CP type and subtype, GMFCS level) and detailed information on the participants’ health and physical abilities, as evaluated by healthcare professionals, will be collected through CPUP (see below for further description of collected variables).
The patient-reported outcome measures will be entered directly into a secure web database, Research Electric Data Capture (REDCap), under Open Patient data Explorative Network (OPEN), Odense University Hospital, Region of Southern Denmark,18 by the parents/guardians using a web link sent via secure digital post (e-Boks). Legal values have been set where possible, to validate the entered values. All collected data will be stored in OPEN Storage, merged and analysed at the Danish Health Data Authority Research Engine.
Quantitative variables
Accelerometry
Habitual PA will be assessed using the Axivity AX3 accelerometer. The use of an accelerometer is a common method for objectively measuring PA,19 and is considered a feasible and validated measure for ambulatory children and adolescents with CP.20
The Axivity AX3 detects movement in three directions: vertical (X), anteroposterior (Y) and mediolateral (Z). The combination of these three axes allows for movement to be calculated into vector magnitude (VM), with VM = √(X2 + Y2 + Z2). VM will be calculated per epoch of time in activity counts (counts per epoch of time). Sampling frequency will be set at 50 Hz with a dynamic range of ±8 g.21 The collected raw data will provide information on the wearer’s habitual PA behaviour regarding acceleration of bodily movement.
The accelerometer is to be worn in a snug-fitting pouch in an elastic belt, strapped around the hip, with the device placed on the midaxillary line at the level of the iliac crest on the child’s right side.19 22 The accelerometer device is to be worn for seven successive days; five school days and a weekend.23 A valid wear day will be defined as a day where the accelerometer is worn for at least 10 hours out of the expected awake time (defined as hours between 6:00 and 22:00 hours on weekdays, and 7:00 and 23:59 hours on weekend days). A similar method has been used in the study by Rasmussen et al21 to assess non-sedentary time with screen time use.21 The minimum number of valid wear days will be four, including 1 weekend day.24 According to procedures used in previous studies21 non-wear periods are identified and registered as missing data by evaluating three signal features generated from acceleration in combination with temperature and predefined expected awake time. Periods of no movement (acceleration below 20 mg) will be identified as non-wear depending on the timespan: (1) periods longer than 120 min will always be identified as non-wear, (2) periods from 45 to 120 min are identified as non-wear if the average temperature is below an individually estimated non-moving temperature (NMT) threshold and (3) periods of 10–45 min with no movement are only identified as non-wear if the average temperature is below the NMT threshold and if the end of the period is within the expected awake time. Device transportation (registration of movement when the device is not worn by the child) is identified as non-wear if the average temperature of the period is below the NMT threshold.21 Non-valid data will be excluded for further analysis.
Total wear time and activity counts will be processed using Matlab (Mathworks, Natick, Massachusetts, USA). To optimise wear time, parents will be offered a daily SMS message encouraging the child to wear the accelerometer.
The OMGUI V.43 software will be used to set up and configure the accelerometers. The Axivity AX3 raw acceleration data will be converted to ActiGraph counts using the methods described by Brønd et al.25 The overall level of PA will be expressed as average counts per day. Converting Axivity raw data to ActiGraph counts will allow for comparability with typically developed children and for sub-analysis using CP-specific cut-points for estimation of time spent in sedentary, light, or moderate-to-vigorous intensity across the different gross motor function levels.22
Cerebral Palsy Follow-Up Programme
Retrospective variables collected from the CPUP physiotherapy protocol, patient protocol, neuropaediatric protocol and orthopaedic protocol will be used to predict the level of habitual PA. Physiotherapy assessments are reported to the database yearly for persons at GMFCS levels II and III, and biennially for persons at GMFCS level I. Assessments from the paediatricians and the orthopaedic surgeons are collected, respectively, once before the age of 5 years and based on the child’s age and gross motor function.14 Consequently, the retrospective CPUP data has been collected within the 38 months prior to assessment of PA level (see timeline, figure 2).
Figure 2.
Included predictive variables sorted into components according to the modified ICF model, including data collection timeline in months. Variables derived from the following: aCPUP registry, bParent-Reported Questionnaire, cPODCI questionnaire, dPedsQLquestionnaire. BMI, body mass index; CP, cerebral palsy; CPUP, Cerebral Palsy Follow-Up Programme; GMFCS, Gross Motor Function Classification System; ICF, International Classification of Functioning, Disability and Health; PedsQL, Paediatric Quality of Life Inventory; PODCI, Paediatric Outcomes Data Collection Instrument; PedsQL, Paediatric Quality of Life Inventory.
Paediatric Quality of Life Inventory
To evaluate health-related QoL, a linguistically validated Danish version of the Paediatric Quality of Life Inventory (PedsQL) CP Module, which is specifically designed for children with CP, will be used.26 It is based on the parents’ reports and measures physical, emotional, social and school functioning. The construct and discriminant validity of the original version have been supported by comparing the scores from children with CP with a generic measure of the same construct from children without disability.27 Satisfactory internal consistency reliability coefficients of 0.87–0.97 have been demonstrated for the PedsQL parent proxy report for children ages 8–18.28
The Paediatric Outcomes Data Collection Instrument
Overall health, pain and participation in normal daily activities will be assessed by a Danish version of the Paediatric Outcomes Data Collection Instrument (PODCI). Concurrent and discriminant validity have been assessed by comparing the PODCI with other measures of health and well-being, gross motor function and diagnostic subgroups in children with CP.29 Moderate to good test–retest reliability with ICC values of 0.71–0.97 have been reported in children with orthopaedic or musculoskeletal disorders.30
Supplementary questions
The following assessment will be evaluated by means of a supplementary parent-reported questionnaire: The child’s average sleep and screen time on a typical weekday and weekend-day, and parent’s socioeconomic status as determined by the parent (based on questionnaires used in the 'Physical activity in schools after the reform' (PHASER) study).31 Visual evaluation of range of motion for the joint on the most affected side; the parent is shown a picture of a joint movement (positioned in the minimum range of motion considered acceptable according to the CPUP’s physiotherapy protocol),32 and is asked to evaluate whether the child’s joint is capable of ‘more’ or ‘less’ movement than the depicted picture (see online supplemental appendix—Parent-evaluated range of motion in the lower extremity). Furthermore, assessment of mobility through the Functional Mobility Scale33 (for more detail see table 1).
Table 1.
Predictive variables
| ICF component | CPUP variables | Questionnaire variables | |
| Body Function & Structure | Range of motion in the lower extremities |
Continuous value: Variable most associated with habitual physical activity from the following measurements (on the most affected side) measured in degrees: HIP
KNEE
ANKLE
|
Visual evaluation of range of motion for most affected side. Categorical values: ‘more’ or ‘less’ than the depicted picture of the following joints (see appendix for illustrations):
|
| Number of hours of sleep per night |
Continuous value:
|
||
| Pain | Categorised as Yes/No |
||
| Muscle tone (Modified Ashworth Scale) |
Categorical value: The absence or presence of increased muscle tone in the most affected side of the lower extremity as evaluated on the Modified Ashworth scale. |
||
| BMI (body mass index) |
Continuous value: Weight in kg /(Height (m))2 |
||
| GMFCS level |
Categorical values: I-III |
Categorical values: I-III |
|
| Activities | The Functional Mobility Score |
Categorical values FMS score (1-6) for:
|
Categorical values FMS score (1-6) for:
|
| GMFM-66 Score |
Continuous score: 0–100 |
||
| Means of transport to and from school |
Categoricalvalues:
|
||
| Hours of screen time |
Continuous value:
|
||
| Ability to climb stairs |
Categorical values:
|
||
| Bikes (bicycle, tricycle, running bike etc.) |
Categorical values:
|
||
| Participation | PODCI | Continuous score: 0–100 | |
| Participation in physical training at school |
Categorical values: Yes/No |
Categorical values: Yes/No |
|
| Participation in recreational activities |
Categorical values: Yes/No |
Categoricalvalues:
|
|
| Personal Factors | Age | Age in years | Age in years |
| Sex |
Categorical values: Male/Female |
Categorical values: Male/Female |
|
| CP classification |
Categorical values:
|
||
| Parents educational level |
Categorical values:
|
||
| Environmental Factors | Residence region |
Categorical values:
|
|
| Use of orthosis |
Categorical values: Yes/No |
||
| Wheelchair use |
Categorical values:
|
||
| Quality of Life | PedsQL | Continuous score: 0–100 | |
BMI, body mass index; CP, cerebral palsy; CPUP, Cerebral Palsy Follow-Up Programme; FMS, Functional Mobility Scale; GMFCS, Gross Motor Function Classification System; ICF, International Classification of Functioning, Disability and Health; PedsQL, Paediatric Quality of Life Inventory; PODCI, Paediatric Outcomes Data Collection Instrument.
bmjopen-2020-047522supp001.pdf (260.9KB, pdf)
All data from the PedsQL, PODCI and supplementary questionnaires are proxy reported by a parent or caregiver.
Danish National Patient Register
For recruitment purposes, parents’/guardians’ national security numbers will be applied for at the Danish National Patient Register, as will registry data on relevant hospital operations and procedures for the children/adolescents.
Study size
The eligible national cohort comprises a total of approximately 1100 children and adolescents in Denmark in the age group of 8–15 years. Based on previous experience of participation in studies by this patient group, we expect an inclusion of 300–400 children.
Statistical methods
WHO introduced the ICF in 2007 as a framework for discussing health and disability from a biopsychosocial perspective through the interaction of five components (ie, Body Functions and Structures, Activity, Participation, Personal Factors and Environmental Factors).34 In 2010, QoL was integrated in a modified ICF model,35 which will be used in the current study as a statistical framework. This allows separate and combined analyses for each of the six components on the prediction of habitual PA, as measured by accelerometer, and will consequently provide data-driven knowledge about using the modified ICF model as a context for habitual PA for children and adolescents with CP.
The following figure operationalises the statistical framework by sorting included outcome variables according to components in the modified ICF model.
Analysis
The identification of predictive factors of habitual PA in children and adolescents with CP between the ages of 8 and 15 years, will, as described above, be operationalised though a statistical analysis plan using the modified ICF model as a conceptual framework (figure 2). Using a predictive model, the study aims to determine the associations between the response variable and the predictive variables, with the purpose of predicting the output value for new observations given their input values.36 The variable that is to be predicted (the response variable) is habitual PA, represented by accelerometer counts. Regardless of the collection time of the data, all other variables (table 1) are considered prediction variables.36
To determine which variables predict the child’s level of PA, multiple linear regression analysis will be performed according to the following models:
Primary analysis
Model 1
Multiple linear regression analysis between accelerometer counts (response variable) and all CPUP variables within each ICF component (predictive variables).
Secondary analysis
Model 2A
Backward stepwise regression with accelerometer counts as the response variable and all included CPUP variables as predictive variables. The Akaike information criterion will be used to determine which variables to retain in the model. Resampling, as described below, will be used to address potential overfitting and to summarise the variability of selected variables.37
Model 2B
Multiple linear regression analysis between accelerometer counts (response variable) and all included variables as predictive variables. This model will assess the degree of predictive strength that the questionnaire variables adds to model 1.
The coefficient of determination, adjusted R-squared, will illustrate the percentage of variance in PA that is explained by the predictive variables. The higher the coefficient, the stronger the relationship. The root mean squared error of the estimate will indicate the accuracy of the predictions. Results will be presented with an alpha of 0.05 and a 95% CI.
Models will be checked using graphic inspection. Splines will be used to account for non-linear effects, and interactions will be included in the model based on relevant subject-matter knowledge. These will be specified in detail in the statistical analysis plan.
Bootstrapping will be performed to reduce the risk of overfitting the prediction model and will thus increase internal validation.38 Missing data will be addressed using multiple imputation applied to each of the bootstrapped datasets.39 External validation can be verified using the Swedish CPUP registry data; however, this will not be performed in the present study.
To evaluate the significance of CPUP data collection periods relative to the time in months from the measure of PA, the model will test for differences in prediction analyses between the following time periods: 0≤12 months, 13≤24 months and 25+ months (figure 2).
Analysis of non-responders and excluded participants will be performed to disclose potential selection bias.
Statistical analyses will be performed using Stata/IC 17 or later for Windows (StataCorp LLC, College Station Tx, USA).
Additional analyses
Several other related analyses will be reported separately. One further study will be on a subgroup of any children or adolescents who are referred for three-dimensional gait analyses as part of their individualised clinical treatment plan. Another analysis will use cut-points for sedentary, light, moderate and vigorous activity for each of the three separate GMFCS levels22 and then compare sedentary behaviour and PA levels of children and adolescents with CP with those of typically developed children and adolescents. Finally, a qualitative study will be performed to explore the daily life challenges that parents describe facing in their pursuit of helping their children with CP live a physically active lifestyle. The methods and findings of this study will be reported elsewhere.
Adverse events
Measuring habitual PA by accelerometry is a non-invasive method commonly used in research and has no known risks or side effects, including pain or discomfort.
Patient and public involvement statement
A pilot study was conducted during the fall of 2019 in which five families were invited to participate and then give feedback on the questionnaires, the use of the accelerometer and the overall burden of participation. Feedback from the children and adolescents, as well as from their parents, led to minor alterations of the study design, such as the questionnaire setup, the use of a different type of elastic belt as well as eliminating the use of an additional accelerometer worn on the thigh.
Patient user groups contributed to the assessment of the project prior to funding being granted by the Elsass Foundation and the Region of Southern Denmark.
Study results are expected to be disseminated through a national interest organisation for persons with CP (eg, articles on website, oral presentation), ensuring study results are communicated to the participants and also to a general wider patient community.
Discussion
The present study will provide novel evidence of predictors of PA for children and adolescents with CP. Recruitment via secure digital post should increase recruitment efficiency, as eligible parties are invited to participate without dependency on healthcare attendances. Due to the wide inclusion criteria, results of this study are expected to have a high level of external validity and be generalisable to other children and adolescents with CP. To ensure the internal validity of the study, selection bias will be investigated through a non-responder analysis. A high acceptance by the treating health professionals is expected, as the majority of variables of interest are already implemented in CPUP.
The study findings may be implemented in evidence-based PA guidelines, which are currently lacking for children with CP, thus providing health professionals with a clinical instrument to help increase PA levels in children and adolescents with CP.
Limitations
This cohort study will be subject to some methodological limitations. Primarily, the current predictive regression analysis cannot determine causality between the predictive variables and the level of PA endured. Thus, the findings should optimally be validated in an external cohort and/or verified in randomised controlled trails. External validation of the prediction model may be achieved, for example, by using the Swedish CPUP registry data; however, this validation is not a part of the current protocol. Nevertheless, bootstrap validation will be performed to increase internal validation.38
Using registry data supports clinically relevant data on all persons in the target group; however, it also poses a risk of having data that is missing for unidentifiable reasons, which complicates the handling of missing data. In this study, missing data will be addressed using imputation of the missing values with the sample mean of the observed cases, resulting in a potential risk of biased estimates due to variance of the variable may be underestimated.
A possible 0–38 months time lag between variables collected via CPUP and the accelerometer data is a methodology limitation. As the participants are at a developmental age where physical change can be monumental, sensitivity analysis will be performed to evaluate the potential significance of the time lag.
To allow for comparability, data on sleep time, screen time and socioeconomic status were assessed using a questionnaire developed for assessment of typically developed children and adolescents in Denmark.31 Data could have been strengthened by the use of validated questionnaires.
While the WHO definition of QOL is based on an individual’s perception, proxy report by parents or caregivers is often necessary in the paediatric care setting due to a child’s young age and/or limited ability to self-report.40 Although studies have shown that children and adolescents above the age of 5 are capable of self-reporting perceived QoL independently,41 this study will use proxy evaluation due to the diverse cognitive abilities in the target group. Allowing for differentiated evaluation (proxy reported or self-reported) would complicate comparability.
Although the study aims to cover a broad aspect of ICF components, important personal and environmental factors such as self-efficacy, social support, motivation and physical access are not included in the analysis.
While children at GMFCS IV may walk assisted as a means of ambulation over short distances, or participate in active propulsion, neither level IV or V are included in this study as the use of wheelchairs complicate valid measurement of PA using accelerometer. Consequently, results of this study will not be applicable to children at a GMFCS level IV–V and thus hinders external validity.
Using tape as a means of mounting the accelerometers could potentially ensure slightly better data quality and possibly better wear compliance compared with using elastic bands.42 However, placement of the accelerometer with tape requires professional assistance, thus making the use of elastic belts a far more feasible solution. Additionally, elastic belts have been reported to be more comfortable for the user.
Using only one accelerometer instead of two limits the possibility of differentiating activity types.43 Furthermore, a hip worn accelerometer may exclude capturing upper-limb activities, possibly resulting in an underestimation of PA levels. However, this study will only be using one accelerometer to ensure better wear compliance among the children and adolescents.
Recruitment of participants for this study will take place during the COVID-19 pandemic. To account for the possible impact this may have on the study, parents will be asked to evaluate the degree to which their child’s PA level is affected by COVID-19 on a five-point Likert scale ranging from ‘He/she is a lot less physically active now than before COVID-19’ to ‘He/she is a lot more physically active now than before COVID-19.’ Furthermore, accelerometer data are only to be collected on days that represent everyday life, that is, not quarantine days, holidays or sick days.
Conclusion
The present protocol outlines a research project that will investigate predictors of habitual PA in children and adolescents with CP with the perspective of optimising PA levels and associated overall health, activities of daily living and QoL.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Jan Brønd for his input on the use of accelerometers and data processing.
Footnotes
Contributors: Conceptualisation and design of the study: AH-L, JT, JML, UD-H and CEF. First draft of manuscript: CEF. Critical revision of manuscript for important intellectual content and approval of final version: all authors.
Funding: The project is funded by the Elsass Foundation, A.J.Andersen & Hustrus Fond, the Region of Southern Denmark, Familien Hede Nielsens Fond, Dagmar Marshalls Fond and A.P. Moellers Fond.
Disclaimer: These funding sources did not have a role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Koman LA, Smith BP, Shilt JS. Cerebral palsy. Lancet 2004;363:1619–31. 10.1016/S0140-6736(04)16207-7 [DOI] [PubMed] [Google Scholar]
- 2.Oskoui M, Coutinho F, Dykeman J, et al. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 2013;55:509–19. 10.1111/dmcn.12080 [DOI] [PubMed] [Google Scholar]
- 3.Frøslev-Friis C, Dunkhase-Heinl U, Andersen JDH, et al. Epidemiology of cerebral palsy in southern Denmark. Dan Med J 2015;62:A4990. [PubMed] [Google Scholar]
- 4.Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol 2005;47:571–6. 10.1017/S001216220500112X [DOI] [PubMed] [Google Scholar]
- 5.Bell KJ, Ounpuu S, DeLuca PA, et al. Natural progression of gait in children with cerebral palsy. J Pediatr Orthop 2002;22:677–82. 10.1097/01241398-200209000-00020 [DOI] [PubMed] [Google Scholar]
- 6.Global Recommendations on Physical Activity for Health . WHO guidelines Approved by the guidelines review Committee. Geneva: WHO, 2010. [Google Scholar]
- 7.Carlon SL, Taylor NF, Dodd KJ, et al. Differences in habitual physical activity levels of young people with cerebral palsy and their typically developing Peers: a systematic review. Disabil Rehabil 2013;35:647–55. 10.3109/09638288.2012.715721 [DOI] [PubMed] [Google Scholar]
- 8.Bjornson KF, Belza B, Kartin D, et al. Ambulatory physical activity performance in youth with cerebral palsy and youth who are developing typically. Phys Ther 2007;87:248–57. 10.2522/ptj.20060157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durstine JL, Painter P, Franklin BA, et al. Physical activity for the chronically ill and disabled. Sports Med 2000;30:207–19. 10.2165/00007256-200030030-00005 [DOI] [PubMed] [Google Scholar]
- 10.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 11.Morgan P, McGinley J. Gait function and decline in adults with cerebral palsy: a systematic review. Disabil Rehabil 2014;36:1–9. 10.3109/09638288.2013.775359 [DOI] [PubMed] [Google Scholar]
- 12.Fowler EG, Kolobe TH, Damiano DL, et al. Promotion of physical fitness and prevention of secondary conditions for children with cerebral palsy: section on pediatrics research Summit proceedings. Phys Ther 2007;87:1495–510. 10.2522/ptj.20060116 [DOI] [PubMed] [Google Scholar]
- 13.Strong WB, Malina RM, Blimkie CJR, et al. Evidence based physical activity for school-age youth. J Pediatr 2005;146:732–7. 10.1016/j.jpeds.2005.01.055 [DOI] [PubMed] [Google Scholar]
- 14.Rasmussen HM, Nordbye-Nielsen K, Møller-Madsen B, et al. The Danish cerebral palsy follow-up program. Clin Epidemiol 2016;8:457–60. 10.2147/CLEP.S99474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alriksson-Schmidt A, Hägglund G, Rodby-Bousquet E, et al. Follow-Up of individuals with cerebral palsy through the transition years and description of adult life: the Swedish experience. J Pediatr Rehabil Med 2014;7:53–61. 10.3233/PRM-140273 [DOI] [PubMed] [Google Scholar]
- 16.SST . National Klinisk Retningslinje for fysioterapi/ergoterapi TIL børn Med cerebral parese. Available: https://sundhedsstyrelsen.dk/da/udgivelser/2014/nkr-cerebral-parese2014
- 17.Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med 2007;147:W–W-94. 10.7326/0003-4819-147-8-200710160-00010-w1 [DOI] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arvidsson D, Fridolfsson J, Börjesson M. Measurement of physical activity in clinical practice using accelerometers. J Intern Med 2019;286:137–53. 10.1111/joim.12908 [DOI] [PubMed] [Google Scholar]
- 20.Gorter JW, Noorduyn SG, Obeid J. Accelerometry: a feasible method to quantify physical activity in ambulatory and nonambulatory adolescents with cerebral palsy. Int J Pediatr 2012;2012:6. 10.1155/2012/329284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rasmussen MGB, Pedersen J, Olesen LG, et al. Short-Term efficacy of reducing screen media use on physical activity, sleep, and physiological stress in families with children aged 4-14: study protocol for the screens randomized controlled trial. BMC Public Health 2020;20:380. 10.1186/s12889-020-8458-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trost SG, Fragala-Pinkham M, Lennon N, et al. Decision trees for detection of activity intensity in youth with cerebral palsy. Med Sci Sports Exerc 2016;48:958–66. 10.1249/MSS.0000000000000842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ishikawa S, Kang M, Bjornson KF, et al. Reliably measuring ambulatory activity levels of children and adolescents with cerebral palsy. Arch Phys Med Rehabil 2013;94:132–7. 10.1016/j.apmr.2012.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cain KL, Sallis JF, Conway TL, et al. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health 2013;10:437–50. 10.1123/jpah.10.3.437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brønd JC, Andersen LB, Arvidsson D. Generating ActiGraph counts from raw acceleration recorded by an alternative monitor. Med Sci Sports Exerc 2017;49:2351–60. 10.1249/MSS.0000000000001344 [DOI] [PubMed] [Google Scholar]
- 26.Stahlhut M, Wong CTK, Taudorf K. Oversættelse af PedQL [in Danish]. Fag Og Forskning 2010;4. [Google Scholar]
- 27.Carlon S, Shields N, Yong K, et al. A systematic review of the psychometric properties of quality of life measures for school aged children with cerebral palsy. BMC Pediatr 2010;10:81. 10.1186/1471-2431-10-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Varni JW, Burwinkle TM, Berrin SJ, et al. The PedsQL in pediatric cerebral palsy: reliability, validity, and sensitivity of the generic core scales and cerebral palsy module. Dev Med Child Neurol 2006;48:442. 10.1017/S001216220600096X [DOI] [PubMed] [Google Scholar]
- 29.McCarthy ML, Silberstein CE, Atkins EA, et al. Comparing reliability and validity of pediatric instruments for measuring health and well-being of children with spastic cerebral palsy. Dev Med Child Neurol 2002;44:468–76. 10.1111/j.1469-8749.2002.tb00308.x [DOI] [PubMed] [Google Scholar]
- 30.Harvey A, Robin J, Morris ME, et al. A systematic review of measures of activity limitation for children with cerebral palsy. Dev Med Child Neurol 2008;50:190–8. 10.1111/j.1469-8749.2008.02027.x [DOI] [PubMed] [Google Scholar]
- 31.Pedersen NH, Koch S, Larsen KT, et al. Protocol for evaluating the impact of a national school policy on physical activity levels in Danish children and adolescents: the PHASAR study - a natural experiment. BMC Public Health 2018;18:1245. 10.1186/s12889-018-6144-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.HMea R. CPOP manual for physiotherapy protocol, 2014. Available: http://www.cpop.dk/wp-content/uploads/2014.07.03-Fysioterapeut-manual.pdf
- 33.Graham HK, Harvey A, Rodda J, et al. The functional mobility scale (FMS). J Pediatr Orthop 2004;24:514–20. 10.1097/01241398-200409000-00011 [DOI] [PubMed] [Google Scholar]
- 34.Rosenbaum P. Family and quality of life: key elements in intervention in children with cerebral palsy. Dev Med Child Neurol 2011;53 Suppl 4:68–70. 10.1111/j.1469-8749.2011.04068.x [DOI] [PubMed] [Google Scholar]
- 35.McDougall J, Wright V, Rosenbaum P. The ICF model of functioning and disability: incorporating quality of life and human development. Dev Neurorehabil 2010;13:204–11. 10.3109/17518421003620525 [DOI] [PubMed] [Google Scholar]
- 36.Shmueli G. To explain or to predict? Statistical Science 2011;25. [Google Scholar]
- 37.Harrell FE, Strategies MM. Multivariable Modeling Strategies. In: Regression modeling strategies. Springer series in statistics. New York, NY: Springer, 2001. [Google Scholar]
- 38.Austin PC, Steyerberg EW. Events per variable (EPV) and the relative performance of different strategies for estimating the out-of-sample validity of logistic regression models. Stat Methods Med Res 2017;26:796–808. 10.1177/0962280214558972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schomaker M, Heumann C. Bootstrap inference when using multiple imputation. Stat Med 2018;37:2252–66. 10.1002/sim.7654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schiariti V, Klassen AF, Cieza A, et al. Comparing contents of outcome measures in cerebral palsy using the International classification of functioning (ICF-CY): a systematic review. Eur J Paediatr Neurol 2014;18:1–12. 10.1016/j.ejpn.2013.08.001 [DOI] [PubMed] [Google Scholar]
- 41.Germain N, Aballéa S, Toumi M. Measuring the health-related quality of life in young children: how far have we come? J Mark Access Health Policy 2019;7:1618661. 10.1080/20016689.2019.1618661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schneller MB, Bentsen P, Nielsen G, et al. Measuring children's physical activity: compliance using Skin-Taped Accelerometers. Med Sci Sports Exerc 2017;49:1261–9. 10.1249/MSS.0000000000001222 [DOI] [PubMed] [Google Scholar]
- 43.Stewart T, Narayanan A, Hedayatrad L, et al. A Dual-Accelerometer system for classifying physical activity in children and adults. Med Sci Sports Exerc 2018;50:2595–602. 10.1249/MSS.0000000000001717 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-047522supp001.pdf (260.9KB, pdf)