Abstract
In a trial of patients with high grade serous ovarian cancer (HGSOC), addition of the ATR inhibitor berzosertib to gemcitabine improved progression free survival (PFS) compared to gemcitabine alone but biomarkers predictive of treatment are lacking. Here we report a candidate biomarker of response to gemcitabine versus combined gemcitabine and ATR inhibitor therapy in HGSOC ovarian cancer. Patients with replication stress (RS)-high tumors (n = 27), defined as harboring at least one genomic RS alteration related to loss of RB pathway regulation and/or oncogene-induced replication stress achieve significantly prolonged PFS (HR = 0.38, 90% CI, 0.17–0.86) on gemcitabine monotherapy compared to those with tumors without such alterations (defined as RS-low, n = 30). However, addition of berzosertib to gemcitabine benefits only patients with RS-low tumors (gemcitabine/berzosertib HR 0.34, 90% CI, 0.13–0.86) and not patients with RS-high tumors (HR 1.11, 90% CI, 0.47–2.62). Our findings support the notion that the exacerbation of RS by gemcitabine monotherapy is adequate for lethality in RS-high tumors. Conversely, for RS-low tumors addition of berzosertib-mediated ATR inhibition to gemcitabine is necessary for lethality to occur. Independent prospective validation of this biomarker is required.
Subject terms: Molecular medicine, Ovarian cancer
A randomized phase 2 study recently showed that the addition of ATR inhibitor berzosertib to gemcitabine improved PFS compared to gemcitabine alone in patients with ovarian cancer. In this preplanned exploratory study, the authors demonstrate that a genomic biomarker of replication-stress is associated with outcome to gemcitabine alone and may predict which patients benefit from addition of the ATR inhibitor berzosertib.
Introduction
Effective treatment of patients with platinum-resistant ovarian cancer (PROC) remains a significant unmet medical need1. Nonplatinum cytotoxic chemotherapy (with or without bevacizumab) is the standard of care for these patients, who typically have poor prognosis and no targeted treatment options except for PARP inhibitors (PARPi) if their tumors are BRCA1/2 mutated1–4. Weekly gemcitabine has demonstrated similar activity as pegylated liposomal doxorubicin in two randomized phase 3 studies in PROC and is a commonly used chemotherapy regimen in this setting5–7.
Preclinical studies have demonstrated synergistic antitumor activity for the combination of gemcitabine and the ATR inhibitor berzosertib8. Gemcitabine induces replication stress (RS) and dependence on the ATR-mediated replication stress response (RSR) via two mechanisms: (i) inhibition of DNA repair by incorporation of gemcitabine nucleotides into the DNA; and (ii) inhibition of ribonucleotide reductase leading to depletion of the deoxyribonucleotide pool required for replication and repair9–13. Targeting the ATR-mediated RSR is particularly relevant to high-grade serous ovarian cancers (HGSOCs), which commonly exhibit molecular alterations associated with increased RS. Specifically, large-scale genomic studies have demonstrated that HGSOCs exhibit: (i) near universal loss of the G1/S checkpoint (via deleterious TP53 mutations); (ii) loss of RB pathway regulation leading to premature G1- > S phase entry due to CCNE1 amplification and RB1 loss in ~20% and 10% of tumors, respectively; and (iii) oncogene-induced replication stress via amplification of the MYC oncogene in up to ~30% of tumors, KRAS amplification (or more rarely mutations) in ~11% of tumors and NF1 loss or mutations in ~12% of tumors14–18. In addition, ~50% of HGSOCs exhibit defective homologous recombination repair (HRR) due to genetic and epigenetic alterations involving HRR genes, and are therefore good candidates for ATR inhibition19–21.
Based on these considerations, we conducted a randomized phase 2 (RP2) study (NCI-CTEP #9944, NCT02595892) to evaluate whether addition of the ATR inhibitor berzosertib to gemcitabine would show acceptable toxicity and superior activity compared with gemcitabine alone in patients with recurrent, platinum-resistant HGSOC22. This was a multicenter, open-label, RP2 study, involving 11 different centers within the US NCI Experimental Therapeutics Clinical Trials Network (ETCTN), which randomly assigned 70 patients (1:1) to treatment with gemcitabine alone (36 patients) or gemcitabine plus berzosertib (34 patients), stratified by platinum-free interval into two strata (PFI ≤ 3 months vs 3–6 months)22. The study met its primary endpoint demonstrating that addition of berzosertib to gemcitabine increased progression-free survival (PFS, the primary endpoint of the study) compared to gemcitabine alone (HR = 0.57, one-sided log-rank p = 0.044), which met the one-sided significance level of 0.1 used for the sample size calculation. Exploratory post-hoc subgroup analyses of PFS showed that the benefit of berzosertib was consistent across various clinical subgroups (including BRCA-mutation status and prior PARPi therapy). However, analysis within the two PFI strata (PFI ≤ 3 months vs 3–6 months) demonstrated that the benefit of addition of berzosertib was only present in the PFI ≤ 3 months subgroup. Here, we report the results of preplanned exploratory correlative studies on tumor specimens from study subjects and demonstrate that a genomic biomarker of RS is associated with outcome to gemcitabine alone and may predict which patients benefit from addition of the ATR inhibitor berzosertib.
Results
ATM mutations and protein expression
Preclinical studies have demonstrated a synthetic lethal interaction between ATM deficiency and ATR inhibition17,23,24. In addition, phase I studies have shown that ATR inhibitors exhibit durable antitumor activity in patients with advanced cancers harboring ATM aberrations (ATM protein expression loss and/or ATM deleterious mutations)25,26. In this regard, we evaluated patient tumor specimens for the presence of ATM mutations via targeted next-generation sequencing (NGS) and for loss or reduction of ATM protein expression via immunohistochemistry (IHC). Archival formalin-fixed tumor specimens were available for targeted NGS from 57 of 70 patients (for the remaining 13 patients there was either inadequate tissue or test failure) and for ATM IHC testing from 60 patients (for the remaining 10 patients there was inadequate tissue).
Targeted NGS using our institutional CLIA-certified OncoPanel assay27 showed that only one patient (1.8%) had a tumor with an ATM mutation (ATM c.3078-5_3078-4insC), which also exhibited negative ATM protein expression by IHC. This patient was randomized to gemcitabine alone and developed clinical progression after three cycles of therapy. The low frequency of ATM mutations in our dataset is consistent with data from The Cancer Genome Atlas (TCGA) showing that ATM mutations are rare in HGSOC (only 1.3% of patients)18.
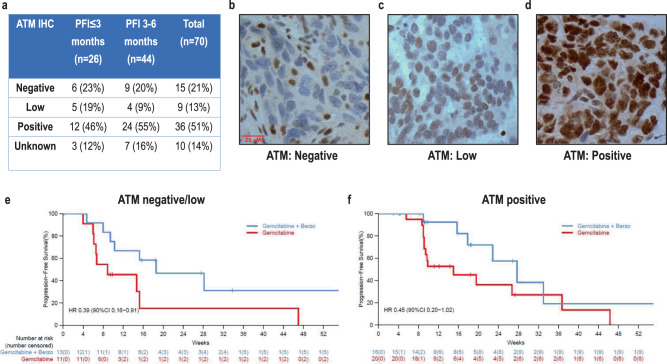
In the 60 patients with ATM IHC data, ATM IHC demonstrated that 15 (25%) patients had tumors negative for ATM protein expression, 9 (15%) had tumors with low ATM protein expression, and 36 (60%) had tumors considered to have positive/retained ATM expression (Fig. 1a–d). There was no difference in ATM protein expression between tumors from patients in the PFI ≤ 3 months versus the PFI 3–6 months strata (Fig. 1a). Overall, the benefit of the addition of berzosertib to gemcitabine was observed across all ATM expression groups (Fig. 1e, f) suggesting that ATM expression by IHC was not associated with patients who benefited from addition of berzosertib to gemcitabine.
Fig. 1. Correlation of ATM expression via immunohistochemistry (IHC) with benefit of addition of berzosertib to gemcitabine.
a Results of ATM IHC presented by PFI strata (PFI ≤ 3 vs 3–6 months). b Figure of ATM IHC highlighting a tumor with negative ATM expression. c Figure of ATM IHC results highlighting tumor with low ATM expression. d Figure of ATM IHC results highlighting tumor with positive ATM expression. e Progression-free survival among patients with tumors with negative/low ATM expression. f Progression-free survival among patients with tumors with positive (retained) ATM expression.
Homologous recombination repair (HRR) alterations and deficiency
Activation of ATR facilitates DNA repair through phosphorylation of several proteins involved in homologous recombination and interstrand cross link (ICL) repair pathways20,21,28. Previous studies have also demonstrated that ATR inhibitors exhibit strong antitumor activity against HRR-deficient tumor models, such as those that are deficient in BRCA1/2, RAD51, or ATM-mutated24,29,30.
Here, we assessed three different biomarkers of HRR deficiency: (i) tumor BRCA1/2 mutation status; (ii) presence of HRR gene mutations by targeted NGS (using our CLIA-certified institutional OncoPanel assay27); and (iii) presence of mutational signature 3 (Sig3), a specific mutational signature characterized by a high number of larger deletions (up to 50 bp) with overlapping microhomology at breakpoint junctions31. Sig3 has been proposed as a biomarker of HRR deficiency reflecting the fact that deficient HRR leads to dependence on alternative error-prone repair mechanisms such as alternative nonhomologous end joining or microhomology-mediated end joining, which utilize microhomology at rearrangement junctions to rejoin and repair DNA double strand breaks32,33.
OncoPanel targeted NGS was performed in 57 patient tumor specimens and identified 14 (25%) patients with HRR mutated/altered tumors (Fig. 2a). Of these, 11 (19%) patients had BRCA1/2-mutated tumors (7 BRCA1 and 4 BRCA2), 2 (4%) patients had tumors with BRIP1 mutations, and 1 (2%) patient had a tumor with a two-copy deletion of RAD51C (Fig. 2a, b). Using a previously developed and validated computational tool called SigMA (Signature Multivariate Analysis)32,34 on the OncoPanel sequencing data, we identified the presence of Sig3 in 23 (40%) of the patients, thereafter denoted as Sig3 positive. SigMA thus identified a larger proportion of tumors as HRR-deficient compared to BRCA1/2 and HRR gene mutations/alterations (Fig. 2a). Among BRCA1/2 wild-type tumors, both BRIP1-mutated tumors were Sig3 positive while the RAD51C deleted tumor was Sig3 negative.
Fig. 2. Correlation of biomarkers of homologous recombination repair deficiency with benefit of addition of berzosertib to gemcitabine.
a SigMA identified a larger proportion of tumors positive for Sig3 compared to BRCA1/2 and homologous recombination repair (HRR) alterations. b HRR (including BRCA1/2) gene alterations identified in patient tumor specimens from the study. c Progression-free survival among patients with Signature 3 (Sig3) positive tumors. d Progression-free survival among patients with Sig3-negative tumors.
Overall, the benefit of the addition of berzosertib to gemcitabine was observed both among patients with tumors with HRR alterations/mutations and among those with tumors without HRR alterations (Supplement Fig. 1). Similarly, the benefit of the addition of berzosertib to gemcitabine was observed independently of Sig3 status (Fig. 2c, d). Taken together, these data indicate that these biomarkers of HRR deficiency were not associated with benefit of addition of berzosertib to gemcitabine. It is also important to note that although there was a trend that patients in the Sig3-negative subgroup responded better to gemcitabine compared to patients in the Sig3-positive subgroup, this was not significant [HR 1.51 (90% CI 0.72–3.18)], Supplement Fig. 2. We also assessed for alterations of nucleotide excision repair (NER) in our dataset and found no tumors with such alterations15,21.
Replication stress (RS) alterations
We used OncoPanel targeted NGS to examine events associated with RS. All but 2 of the 57 (96%) patients had TP53-mutated tumors, which is consistent with the prevalence of TP53 mutations in HGSOC reported in TCGA dataset (also 96%)18. Both p53 wild-type tumors were confirmed to be high-grade serous and both exhibited high somatic copy number alterations consistent with HGSOC.
The prevalence of RS alterations (please also refer to Methods) in our clinical trial dataset is shown in Fig. 3a, grouped by the mechanism of increased RS: (i) alterations leading to loss of RB pathway regulation and premature G1- > S phase entry; and/or (ii) alterations associated with oncogene-induced replication stress. The most prevalent RS alterations included CCNE1 amplification in 8 (14%) patients, MYCL1 amplification in 6 (11%) patients, KRAS amplification in 5 patients (9%), and MYC amplification in 5 patients (9%). Six of eight (75%) CCNE1-amplified tumors also exhibited overexpression of CCNE1 by IHC (median or high CCNE1 expression, Supplement Fig. 3); in the remaining two (25%) CCNE1-amplified tumors, CCNE1 expression was low (Supplement Fig. 3).
Fig. 3. Correlation of a replication stress biomarker with benefit of addition of berzosertib to gemcitabine.
a Prevalence of replication stress (RS) alterations grouped by the mechanism of increased RS: (i) alterations leading to loss of RB pathway regulation and premature G1- > S phase entry, and (ii) alterations associated with oncogene-induced replication stress. Tumors with at least one of these alterations were classified as RS-high; tumors with none of these alterations were classified as RS-low. b Progression-free survival among patients with RS-low tumors. c Progression-free survival among patients with RS-high-negative tumors. Unlike patients with RS-low tumors, there was no benefit of addition of berzosertib to gemcitabine among patients with RS-high tumors.
As evident in Fig. 3a, the RS alterations were spread across tumors without a dominant element, precluding selective statistical analysis of the association of individual RS alterations with berzosertib benefit. Therefore, RS alterations were grouped together, and tumors were assigned into two different groups based on the presence or not of at least one of these genomic RS alterations. Specifically, the first group included patients with tumors with at least one of these RS alterations (defined as RS-high tumors): CCNE1 amplification, RB1 two-copy loss, CDKN2A two-copy loss, KRAS amplification, NF1 mutations, ERBB2 amplification, MYC amplification, and MYCL1 amplification (Fig. 3a). The second group included patients with tumors without any of these RS alterations (defined as RS-low tumors). Overall, 30 (53%) tumors were RS-low and 27 tumors (47%) were RS-high; five (19%) of 27 RS-high tumors had more than one RS-associated events. Supplement Table 1 presents the genomic alterations within the context of patients with RS-high and RS-low tumors. There was no significant difference in the prevalence of RS-low and RS-high tumors between patients in the PFI ≤ 3 months versus the PFI 3–6 months strata (54% of PFI ≤ 3 months and 51% of PFI 3–6 months were RS-low).
A PFS benefit of addition of berzosertib to gemcitabine was observed only in the RS-low tumors (HR = 0.34,90% CI, 0.13–0.86, median PFS 27.7 weeks versus 9.9 weeks; Fig. 3b, c). Furthermore, among RS-low tumors, there was no difference in the benefit of addition of berzosertib between PFI ≤ 3 months and PFI 3–6 months (the PFS benefit of addition of berzosertib was 0.47 (0.13–1.68) in the PFI ≤ 3 months stratum and 0.25 (0.04–1.43) in the PFI 3–6 months). Interestingly, no benefit of addition of berzosertib to gemcitabine was observed in the RS-high tumors (PFS HR = 1.11, 90% CI, 0.47–2.62) suggesting that this genomic biomarker may be an important biological discriminant for benefit of ATR inhibition to gemcitabine, and worthy of future, statistically powered evaluation. Correlation of this biomarker with objective response rate, clinical benefit response rate and PFS at 6 months is presented in Supplement Table 2.
Although limited by small numbers, we also performed two separate analyses for the alterations associated with each of the two mechanisms of increased RS, i.e., separately for the alterations associated with loss of RB pathway regulation and separately for the alterations associated with oncogene-induced replication stress. Specifically, when focused only on RS alterations associated with oncogene-induced replication stress, the benefit of addition of berzosertib was again observed only in tumors without any oncogene alterations with a HR 0.49 (90% CI 0.23–1.02), similar with the finding in RS-low tumors, Supplement Fig. 4. Conversely, there was no berzosertib benefit in the group of tumors with oncogene alterations (HR 1.25, 90% CI 0.41–3.81), Supplement Fig. 4.
When focused only on RB pathway alterations, again, the benefit of addition of berzosertib was observed only in tumors without any RB pathway alterations with a HR 0.48 (90% CI 0.23–1.02), similar with the finding in RS-low tumors, Supplement Fig. 5. Conversely, there was no berzosertib benefit in the group of tumors with RB pathway alterations with a HR 0.8 (90% CI 0.25–2.57), Supplement Fig. 5.
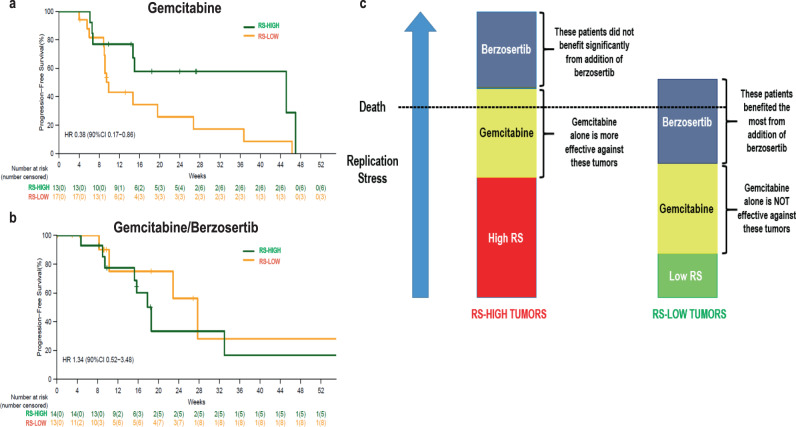
RS alterations and response to gemcitabine
The finding that the benefit of addition of berzosertib to gemcitabine was evident only in the RS-low tumors may be explained by the fact that patients with RS-low tumors who received gemcitabine alone did significantly worse compared to patients with RS-high tumors (i.e., RS-high may be a biomarker of response to gemcitabine monotherapy). Specifically, as shown in Fig. 4a, patients with RS-high tumors did significantly better with gemcitabine alone compared to patients with RS-low tumors (HR = 0.38, 90% CI, 0.17–0.86, median PFS 45.1 vs 9.9 weeks). On the contrary, there was no statistically significant difference in response to gemcitabine/berzosertib between RS-low and RS-high tumors (HR = 1.34, 90% CI, 0.52–3.48, median PFS 18.6 vs 27.7 weeks), Fig. 4b.
Fig. 4. Correlation of a replication stress biomarker with response to gemcitabine alone and response to gemcitabine/berzosertib.
a Patients with replication stress (RS)-high tumors responded better to gemcitabine alone compared to patients with RS-low tumors (HR = 0.38, 90% CI, 0.17–0.86, median PFS 45.1 vs 9.9 weeks). b On the contrary, there was no difference in the response to gemcitabine/berzosertib between patients with RS-low versus RS-high tumors. c Working model of the correlation of RS-low and RS-high tumors with outcome to gemcitabine and gemcitabine/berzosertib. Based on this model, gemcitabine, a drug which increases replication stress has better monotherapy activity against RS-high tumors (left panel) than RS-low tumors (right panel). Unlike RS-high tumors, RS-low tumors need the addition of the ATR inhibitor (ATRi) berzosertib, which explains why the benefit of addition of berzosertib to gemcitabine is only observed among RS-low tumors.
Taken together, these results indicate that patients with RS-high tumors did better with gemcitabine alone (Fig. 4a) and that for these patients, addition of berzosertib did not appear to provide benefit (Fig. 3c). Conversely, patients with RS-low tumors did worse with gemcitabine alone (Fig. 4a) and for these patients, addition of berzosertib provided PFS benefit (Fig. 3b). All four PFS curves are also presented in the same Figure as reference (Supplement Fig. 6). Figure 4c shows a working model highlighting: (i) the better outcome with gemcitabine alone among patients with RS-high tumors (compared to RS-low tumors), and (ii) the benefit of addition of berzosertib to gemcitabine among patients with RS-low tumors. According to this model, gemcitabine, a drug that increases replication stress, has better monotherapy activity against RS-high tumors (left panel) than RS-low tumors (right panel). In RS-high tumors, the exacerbation of replication stress by gemcitabine monotherapy is adequate for lethality. However, in RS-low tumors, the addition of berzosertib-mediated ATR inhibition to gemcitabine is necessary for lethality to occur, explaining why the benefit of addition of berzosertib to gemcitabine is only observed among RS-low tumors.
Discussion
We report a candidate, previously unrecognized, potentially predictive biomarker of response to gemcitabine monotherapy in HGSOC. Patients with RS-high tumors, defined as harboring at least one genomic RS alteration related to (i) loss of RB pathway regulation (CCNE1 amplification, RB1 two-copy loss, CDKN2A two-copy loss), and/or (ii) oncogene-induced replication stress (KRAS amplification, NF1 mutations, ERBB2 amplification, MYC amplification and MYCL1 amplification) achieved significantly prolonged PFS (HR = 0.38) on gemcitabine monotherapy compared to those with tumors without such alterations. Although sensitivity to gemcitabine has been previously associated with specific genomic alterations (such as ARID1A deficiency) in preclinical models, a genomic biomarker has not been previously associated with clinical response to gemcitabine in ovarian cancer or any other malignancy35. The improved response of RS-high tumors is consistent with the mechanism of action of gemcitabine, which induces RS via: incorporation of gemcitabine nucleotides into the DNA and by inhibition of ribonucleotide reductase9–13. Conceptually, RS-high tumors are less likely to tolerate the increased RS induced by gemcitabine compared to RS-low tumors and are therefore more likely to respond (Fig. 4c).
Evaluation of the association of response to gemcitabine with markers of HRR deficiency revealed a nonsignificant trend that patients in the Sig3-negative subgroup (reflective of HRR proficient tumors) responded better to gemcitabine compared to patients in the Sig3-positive subgroup (reflective of HRR-deficient tumors), Supplement Fig. 2. This observation is consistent with available literature in ovarian cancer suggesting that response to gemcitabine is at least equal (or even better) in patients with platinum-resistant disease (a setting enriched for HRR proficient tumors) compared to platinum sensitive disease (a setting enriched for HRR-deficient tumors)36,37.
While patients with RS-high tumors fared better with gemcitabine alone (compared to RS-low), only patients with RS-low tumors benefited from addition of the ATR inhibitor berzosertib to gemcitabine (gemcitabine/berzosertib HR compared to gemcitabine was 0.34 in RS-low vs 1.11 in RS-high tumors). This finding appears counterintuitive as patients with RS-high tumors would have been expected to derive more benefit from ATR inhibitor therapy (given the implication of ATR kinase in regulation of the RS response). However, our study did not explore which patients benefit the most from berzosertib monotherapy (there was no berzosertib monotherapy arm in the clinical trial); rather, our study explored which patients benefited the most from the addition of berzosertib to gemcitabine. Given that gemcitabine monotherapy exhibited poor activity against RS-low tumors and given the known synergism between gemcitabine and ATR inhibitor therapy, it is not surprising that it was patients with RS-low tumors that benefited the most from addition of berzosertib. Conversely, for patients with RS-high tumors who fared significantly better with gemcitabine alone, addition of berzosertib did not appear to provide benefit. Importantly, the benefit of addition of berzosertib in patients with RS-low tumors was seen in both PFI (PFI ≤ 3 months and 3–6 months) strata, including the PFI 3–6 months stratum, where in the overall analysis of all patients, the benefit of addition of berzosertib was not present22.
It is important to note that alternative biomarkers of RS have also been reported in the literature for other tumor types38–40. In hepatocellular carcinoma (HCC), a unique signature of Cyclin A2 or E1 activating alterations associated with an aggressive HCC subtype and characterized by structural rearrangements with hundreds of tandem duplications and templated insertions frequently activating the TERT promoter has been reported38. A similar signature is present in ovarian cancer but solely in BRCA1-mutated tumors38. In pancreatic cancer, a transcriptomic signature of replication stress that predicts response to ATR and WEE1 inhibitors has been reported, which, similar to our findings, was not associated with homologous recombination deficiency40. However, development of this transcriptomic signature was based solely on preclinical models of patient derived cell lines and organoid models without any human response data.
No other biomarker including ATM aberrations (ATM protein expression loss and/or ATM deleterious mutations) and HRR deficiency (BRCA1/2 mutations, HRR alterations and presence of Sig3) could predict benefit from addition of berzosertib to gemcitabine. These biomarkers have been associated with response to ATRi monotherapy24–26,29,30 but our study could not evaluate this association as there was no berzosertib monotherapy arm. Furthermore, these biomarkers could not predict response to gemcitabine monotherapy. Our study confirmed that ATM mutations are rare in HGSOC (<2%); however, loss of ATM expression was not uncommon, with 25% and 15% of tumors being negative and low for ATM protein expression by IHC, respectively. Consistent with previous studies32, Sig3 positivity was identified in a larger proportion of tumors (40% of samples) than positivity for BRCA1/2 mutations and HRR alterations, suggesting that Sig3 may identify HRR-deficient (HRD) tumors beyond BRCA/HRR alterations. However, it is important to underscore that the ability of HRD assays to predict deficient homologous recombination in the setting of platinum- and PARPi-resistant ovarian cancer is limited by the fact that tumors predicted to be HRD may have restored HRR as a mechanism of resistance driven by selection pressure from prior platinum and/or PARPi therapy41,42.
We acknowledge certain limitations of this study. The sample size was small, as this trial was a hypothesis-generating study powered to detect an improvement in median progression-free survival at a one-sided significance level of 0.1. The candidate predictive biomarker we identified is exploratory and hypothesis-generating on which to base future studies and will require independent validation in subsequent studies of gemcitabine with and without ATRi therapy. In this regard, a randomized phase 2/3 study of gemcitabine with or without berzosertib with prospective validation of this biomarker is being planned. Samples were collected from patients enrolled in 11 different study sites in the United States, and, despite our best efforts, insufficient tumor material was available for all patients for completion of all correlative studies. These limitations notwithstanding, our hypothesis-generating findings are interesting because they challenge the notion that ATR inhibitor therapy should only be considered for tumors with high replication stress. In fact, for tumors with low replication stress, a strategy of combining ATR inhibitors with agents that induce replication stress (such as gemcitabine) and therefore sensitize to ATR inhibition may be particularly appealing and, when compared to gemcitabine alone, may provide greater benefit among RS-low tumors (where single agent gemcitabine has low activity). Furthermore, the proposed genomic biomarker is mechanistically relevant, developed using our CLIA-certified targeted NGS assay and, assuming it is independently validated, may be readily applicable to clinical practice. Our study highlights that careful analysis of genomic information from clinical samples can provide valuable information on the determinants of response to therapy and may accelerate the development of predictive biomarkers to aid in patient stratification.
Methods
Patient samples
Archival Formalin-Fixed Paraffin-Embedded (FFPE) tumor samples were collected from patients enrolled in an investigator-initiated phase 2, multicenter, open-label, randomized study of berzosertib combined with gemcitabine compared with gemcitabine alone in subjects with platinum-resistant recurrent HGSOC (NCT02595892) sponsored by the National Cancer Institute (NCI)22. Patients were enrolled at 11 different centers in the United States through the Experimental Therapeutics Clinical Trials Network (ETCTN). Overall, 70 patients were randomly assigned (1:1) to treatment with gemcitabine alone (36 patients) or gemcitabine plus berzosertib (34 patients), stratified by platinum-free interval (PFI ≤ 3 months vs 3–6 months). Availability of archival FFPE tumor specimens was required for participation. The clinical trial was approved by the NCI Central Institutional Review Board (CIRB) and the US Food and Drug Administration (NCT02595892). All procedures involving human participants were carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained from patients or guardians before enrolment in the study. The REporting recommendations for tumour MARKer prognostic studies (REMARK)
The clinical trial was designed to have 80% power to detect an improvement of median progression-free survival from 15 weeks with gemcitabine alone to 27.3 weeks with gemcitabine plus berzosertib at a one-sided alpha level of 0.1. Anticipating that 10% of participants would not be evaluable, the maximum total number of patients that needed to be enrolled was 70.
The median follow-up was 53.2 weeks (interquartile (IQR) 25.6–81.8) in the gemcitabine plus berzosertib group and 43.0 weeks (IQR 23.2–69.1) in the gemcitabine alone group.
Targeted sequencing and detection of mutational signature 3
Of the 70 patients who participated in the study, archival formalin-fixed tumor specimens were available for targeted NGS from 57 patients (for the remaining 13 patients there was either inadequate tissue or test failure). Targeted panel NGS was performed on FFPE tissue samples using OncoPanel, a Clinical Laboratory Improvement Amendments (CLIA) certified assay performed at Dana-Farber Cancer Institute (DFCI). The Oncopanel test consists of NGS of formalin-fixed tumor samples covering exons of 447 cancer-associated genes plus intronic regions of genes involved in somatic rearrangements27,43,44. Oncopanel tests are reviewed by molecular pathologists and report mutations, insertion-deletions, copy number variations, and structural variants in the targeted genes. Amplification was defined as at least six estimated number of copies. The following HRR genes were assessed (besides BRCA1 and BRCA2): PALB2, BARD1, BRIP1, RAD50, RAD51C, RAD51D, RAD54L, FANCA, FANCB, FANCC, CHEK1, CHEK2, BLM, NBN, and MRE11A. Mutational signature 3 was called using SigMA34,32. For this study, SigMA was optimized for OncoPanel using simulations generated specifically for its library using whole-genome sequenced ovarian cancer datasets34. To minimize false positives, we applied a stringent threshold so that the estimated false positive rate was <0.05%, which corresponds to a sensitivity of 71%.
The selection of genes included as replication stress alterations was based on alterations that are known to be prevalent and drivers in high-grade serous ovarian cancer (HGSOC) based on large-scale genomic studies such as the ovarian cancer TCGA dataset, and also known to be associated with increased replication stress18. Specifically, oncogene-induced replication stress associated with CCNE1 amplification, MYC and MYCL1 amplification is prevalent in HGSOC18. Several lines of evidence suggest that KRAS amplification, NF1 loss and ERBB2 amplification are also prevalent in that setting18,45. CDKN2A and RB1 loss were also included given their strong mutual exclusivity with CCNE1 amplification in HGSOC reflecting a strong selection pressure for premature G1- > S phase entry and increased replication stress18.
Immunohistochemistry
Of the 70 patients who participated in the study, archival FFPE tumor specimens were available for IHC testing from 60 patients (for the remaining 10 patients there was inadequate tissue). Staining for ATM was performed on FFPE sections using the anti-ATM antibody (clone Y170, Abcam, ab32420) at a dilution 1:100. The staining was performed on the Leica BOND automated staining instrument. Staining for ATM was considered positive if almost all cells in the sample contained nuclear ATM stain, including tumor and surrounding stroma. Staining for ATM was considered negative if tumor cells were negative while stromal cells were positive while staining was considered low if the percentage of tumor cells that contained nuclear staining was <50%. The ATM positive group included samples where nuclear ATM staining was observed in at least 50% of the tumor cells and up to 100%.; samples in this group exhibited different levels of staining between 50–100%, i.e., not all samples were 100% positive for ATM. The anti-CCNE1 (clone HE12, Cell Signaling, #4129) was used for assessing CCNE1 levels at a dilution 1:60,000. CCNE1 staining was scored as low if there was weak staining in <25% of tumor cell nuclei, medium if there was weak-to-moderate staining in 25–75% of tumor nuclei, and high if there was moderate-to-strong staining in >75% of tumor nuclei.
Statistics
The PFS time [defined as the number of days between registration in the study until the date of development of progressive disease or death (regardless of cause)22] associated with each treatment arm was summarized using the Kaplan–Meier method and displayed graphically. Median PFS time and 6-month PFS were also reported. The Cox proportional hazards models were fit to estimate the treatment hazard ratio and the corresponding two-sided 90% CI. Point and confidence estimates were provided throughout the manuscript; no p-values were reported as analyses were exploratory. Analyses were done using R (version 4.0.5).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
We thank the patients and their families for their participation in this study. This study was funded by the NCI-Cancer Therapy Evaluation Program (CTEP) and conducted under the auspices of the Experimental Therapeutics Clinical Trials Network (ETCTN). Dana-Farber/Harvard Cancer Center served as the lead site for the study, supported by NIH grant UM1 CA186709 (G.I.S., Principal Investigator). This work was also funded by Supplements to UM1 CA186709 for the development of immunohistochemical biomarkers for homologous recombination repair and ATM proficiency (B.K., A.D.D., and G.I.S.) and by the Dana-Farber/Harvard Cancer Center Specialized Program of Research Excellence (SPORE) (P50CA240243) in Ovarian Cancer (P.A.K., B.K., J.F.L., N.T., U.A.M., A.D.D., and G.I.S.).
Author contributions
P.A.K. conceived, supervised, coordinated, and analyzed all the correlative data and wrote the manuscript; A.A.B.A.dC. and E.K.L. analyzed the Oncopanel sequencing data and wrote the manuscript; D.G. performed the mutational signature analysis; S.C. performed the statistical analysis and was the lead statistician of the study; A.E.W. provided clinical data to the study; B.K. and D.L.K. performed and analyzed the IHC data; E.C.K. supported the trial and contributed to the analysis of all correlative data; J.F.L. and E.H.S. provided clinical data and contributed to the analysis of all correlative data; J.C. and M.P. coordinated the processing and distribution of the clinical trial samples; N.T. contributed to the statistical analysis; D.C. contributed to the analysis of all correlative data; U.A.M. supported and coordinated the trial and contributed to the analysis of all correlative data; A.F. analyzed the sequencing and mutational signature data and wrote the manuscript; A.D.D. supported and contributed to the analysis of all correlative data. G.I.S. supported, conceived, and supervised the correlative analyses and wrote the manuscript. All authors contributed to the writing and editing of the manuscript.
Data availability
The Oncopanel data generated in this study have been deposited in the Synapse.org database under accession code syn25982096 [DOI: 10.7303/syn25982096]. All the data behind all the Kaplan–Meier curves of the manuscript are also available at DOI: 10.7303/syn25982096. The associated data are available under restricted access for noncommercial use, access can be obtained by accepting the Synapse terms and conditions.
Competing interests
A.D.D. is a consultant/advisory board member for Merck-EMD-Serono. G.I.S. has received research funding from Merck KGaA/EMD-Serono and has served on advisory boards for Merck KGaA/EMD-Serono DNA repair inhibitors. The remaining authors declare no competing interests.
Footnotes
Peer review informationNature Communications thanks Dmitriy Zamarin and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Alexandre André B. A. da Costa, Doga Gulhan, Elizabeth K. Lee.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-021-25904-w.
References
- 1.Matulonis UA, et al. Ovarian cancer. Nat. Rev. Dis. Prim. 2016;2:16061. doi: 10.1038/nrdp.2016.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lorusso D, et al. Investigational agents against platinum-resistant ovarian cancer. Expert Opin. Invest. Drugs. 2007;16:325–336. doi: 10.1517/13543784.16.3.325. [DOI] [PubMed] [Google Scholar]
- 3.Pignata, S. et al. Treatment of recurrent ovarian cancer. Ann. Oncol. 28, viii51–viii56 (2017). [DOI] [PubMed]
- 4.Konstantinopoulos PA, Awtrey CS. Management of ovarian cancer: a 75-year-old woman who has completed treatment. JAMA. 2012;307:1420–1429. doi: 10.1001/jama.2012.269. [DOI] [PubMed] [Google Scholar]
- 5.Ferrandina G, et al. Phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in progressive or recurrent ovarian cancer. J. Clin. Oncol. 2008;26:890–896. doi: 10.1200/JCO.2007.13.6606. [DOI] [PubMed] [Google Scholar]
- 6.Kurzeder C, et al. Double-blind, placebo-controlled, randomized phase III trial evaluating pertuzumab combined with chemotherapy for low tumor human epidermal growth factor receptor 3 mRNA-expressing platinum-resistant ovarian cancer (PENELOPE) J. Clin. Oncol. 2016;34:2516–2525. doi: 10.1200/JCO.2015.66.0787. [DOI] [PubMed] [Google Scholar]
- 7.Mutch DG, et al. Randomized phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in patients with platinum-resistant ovarian cancer. J. Clin. Oncol. 2007;25:2811–2818. doi: 10.1200/JCO.2006.09.6735. [DOI] [PubMed] [Google Scholar]
- 8.Serono MKaE. M6620 Investigator’s Brochure. (2018).
- 9.Fordham SE, et al. Inhibition of ATR acutely sensitizes acute myeloid leukemia cells to nucleoside analogs that target ribonucleotide reductase. Blood Adv. 2018;2:1157–1169. doi: 10.1182/bloodadvances.2017015214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karnitz LM, et al. Gemcitabine-induced activation of checkpoint signaling pathways that affect tumor cell survival. Mol. Pharmacol. 2005;68:1636–1644. doi: 10.1124/mol.105.012716. [DOI] [PubMed] [Google Scholar]
- 11.Liu S, et al. Inhibition of ATR potentiates the cytotoxic effect of gemcitabine on pancreatic cancer cells through enhancement of DNA damage and abrogation of ribonucleotide reductase induction by gemcitabine. Oncol. Rep. 2017;37:3377–3386. doi: 10.3892/or.2017.5580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallez Y, et al. The ATR inhibitor AZD6738 synergizes with gemcitabine in vitro and in vivo to induce pancreatic ductal adenocarcinoma regression. Mol. Cancer Ther. 2018;17:1670–1682. doi: 10.1158/1535-7163.MCT-18-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huntoon CJ, et al. ATR inhibition broadly sensitizes ovarian cancer cells to chemotherapy independent of BRCA status. Cancer Res. 2013;73:3683–3691. doi: 10.1158/0008-5472.CAN-13-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bell D, et al. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ceccaldi R, et al. A unique subset of epithelial ovarian cancers with platinum sensitivity and PARP inhibitor resistance. Cancer Res. 2015;75:628–634. doi: 10.1158/0008-5472.CAN-14-2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mouw KW, D’Andrea AD, Konstantinopoulos PA. Nucleotide excision repair (NER) alterations as evolving biomarkers and therapeutic targets in epithelial cancers. Oncoscience. 2015;2:942–943. doi: 10.18632/oncoscience.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konstantinopoulos PA, Lheureux S, Moore KN. PARP inhibitors for ovarian cancer: current indications, future combinations, and novel assets in development to target DNA damage repair. Am. Soc. Clin. Oncol. Educ. Book. 2020;40:1–16. doi: 10.1200/EDBK_288015. [DOI] [PubMed] [Google Scholar]
- 18.Cancer Genome Atlas Research N. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konstantinopoulos PA, et al. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian. Cancer Cancer Discov. 2015;5:1137–1154. doi: 10.1158/2159-8290.CD-15-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee KY, Chung KY, Koo HS. The involvement of FANCM, FANCI, and checkpoint proteins in the interstrand DNA crosslink repair pathway is conserved in C. elegans. DNA Repair (Amst.) 2010;9:374–382. doi: 10.1016/j.dnarep.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Curtin NJ. DNA repair dysregulation from cancer driver to therapeutic target. Nat. Rev. Cancer. 2012;12:801–817. doi: 10.1038/nrc3399. [DOI] [PubMed] [Google Scholar]
- 22.Konstantinopoulos PA, et al. Berzosertib plus gemcitabine versus gemcitabine alone in platinum-resistant high-grade serous ovarian cancer: a multicentre, open-label, randomised, phase 2 trial. Lancet Oncol. 2020;21:957–968. doi: 10.1016/S1470-2045(20)30180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mei L, et al. Ataxia telangiectasia and Rad3-related inhibitors and cancer therapy: where we stand. J. Hematol. Oncol. 2019;12:43. doi: 10.1186/s13045-019-0733-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reaper PM, et al. Selective killing of ATM- or p53-deficient cancer cells through inhibition of ATR. Nat. Chem. Biol. 2011;7:428–430. doi: 10.1038/nchembio.573. [DOI] [PubMed] [Google Scholar]
- 25.Yap TA, et al. Phase I trial of first-in-class ATR inhibitor M6620 (VX-970) as monotherapy or in combination with carboplatin in patients with advanced solid tumors. J. Clin. Oncol. 2020;38:3195–3204. doi: 10.1200/JCO.19.02404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yap TA, et al. First-in-human trial of the oral ataxia telangiectasia and RAD3-related (ATR) inhibitor BAY 1895344 in patients with advanced solid tumors. Cancer Discov. 2021;11:80–91. doi: 10.1158/2159-8290.CD-20-0868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagle N, et al. High-throughput detection of actionable genomic alterations in clinical tumor samples by targeted, massively parallel sequencing. Cancer Discov. 2012;2:82–93. doi: 10.1158/2159-8290.CD-11-0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flynn RL, Zou L. ATR: a master conductor of cellular responses to DNA replication stress. Trends Biochem. Sci. 2011;36:133–140. doi: 10.1016/j.tibs.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hill SJ, et al. Prediction of DNA repair inhibitor response in short-term patient-derived ovarian cancer organoids. Cancer Discov. 2018;8:1404–1421. doi: 10.1158/2159-8290.CD-18-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Young LA, et al. Differential activity of ATR and WEE1 inhibitors in a highly sensitive subpopulation of DLBCL lnked to replication stress. Cancer Res. 2019;79:3762–3775. doi: 10.1158/0008-5472.CAN-18-2480. [DOI] [PubMed] [Google Scholar]
- 31.Alexandrov LB, et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415–421. doi: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Farkkila A, et al. Immunogenomic profiling determines responses to combined PARP and PD-1 inhibition in ovarian cancer. Nat. Commun. 2020;11:1459. doi: 10.1038/s41467-020-15315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ceccaldi R, et al. Homologous-recombination-deficient tumours are dependent on Poltheta-mediated repair. Nature. 2015;518:258–262. doi: 10.1038/nature14184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gulhan DC, et al. Detecting the mutational signature of homologous recombination deficiency in clinical samples. Nat. Genet. 2019;51:912–919. doi: 10.1038/s41588-019-0390-2. [DOI] [PubMed] [Google Scholar]
- 35.Kuroda T, et al. Therapeutic preferability of gemcitabine for ARID1A-deficient ovarian clear cell carcinoma. Gynecol. Oncol. 2019;155:489–498. doi: 10.1016/j.ygyno.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Friedlander M, et al. A phase II study of gemcitabine in platinum pre-treated patients with advanced epithelial ovarian cancer. Ann. Oncol. 1998;9:1343–1345. doi: 10.1023/A:1008469212268. [DOI] [PubMed] [Google Scholar]
- 37.Lund B, et al. Phase II study of gemcitabine (2’,2’-difluorodeoxycytidine) in previously treated ovarian cancer patients. J. Natl Cancer Inst. 1994;86:1530–1533. doi: 10.1093/jnci/86.20.1530. [DOI] [PubMed] [Google Scholar]
- 38.Bayard Q, et al. Cyclin A2/E1 activation defines a hepatocellular carcinoma subclass with a rearrangement signature of replication stress. Nat. Commun. 2018;9:5235. doi: 10.1038/s41467-018-07552-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dereli-Oz A, Versini G, Halazonetis TD. Studies of genomic copy number changes in human cancers reveal signatures of DNA replication stress. Mol. Oncol. 2011;5:308–314. doi: 10.1016/j.molonc.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dreyer SB, et al. Targeting DNA damage response and replication stress in pancreatic cancer. Gastroenterology. 2021;160:362–377 e13. doi: 10.1053/j.gastro.2020.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fuh K, et al. Homologous recombination deficiency real-time clinical assays, ready or not? Gynecol. Oncol. 2020;159:877–886. doi: 10.1016/j.ygyno.2020.08.035. [DOI] [PubMed] [Google Scholar]
- 42.Stover EH, et al. Clinical assays for assessment of homologous recombination DNA repair deficiency. Gynecol. Oncol. 2020;159:887–898. doi: 10.1016/j.ygyno.2020.09.029. [DOI] [PubMed] [Google Scholar]
- 43.Sholl LM, et al. Institutional implementation of clinical tumor profiling on an unselected cancer population. JCI Insight. 2016;1:e87062. doi: 10.1172/jci.insight.87062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garcia EP, et al. Validation of OncoPanel: a targeted next-generation sequencing assay for the detection of somatic variants in cancer. Arch. Pathol. Lab Med. 2017;141:751–758. doi: 10.5858/arpa.2016-0527-OA. [DOI] [PubMed] [Google Scholar]
- 45.Oh DY, Bang YJ. HER2-targeted therapies—a role beyond breast cancer. Nat. Rev. Clin. Oncol. 2020;17:33–48. doi: 10.1038/s41571-019-0268-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Oncopanel data generated in this study have been deposited in the Synapse.org database under accession code syn25982096 [DOI: 10.7303/syn25982096]. All the data behind all the Kaplan–Meier curves of the manuscript are also available at DOI: 10.7303/syn25982096. The associated data are available under restricted access for noncommercial use, access can be obtained by accepting the Synapse terms and conditions.