Abstract
Purpose:
Pregnant women across the rural United States have increasingly limited access to obstetric care, especially specialty care for high-risk women and infants. Limited research focuses on access for rural American Indian/Alaskan Native (AIAN) women, a population warranting attention given persistent inequalities in birth outcomes.
Methods:
Using Montana birth certificate data (2014–2018), we examined variation in travel time to give birth and access to different levels of obstetric care (ie, the proportion of individuals living within 1- and 2-hour drives to facilities), by rurality (Rural-Urban Continuum Code) and race (White and AIAN people).
Findings:
Results point to limited obstetric care access in remote rural areas in Montana, especially higher-level specialty care, compared to urban or urban-adjacent rural areas. AIAN women traveled significantly farther than White women to access care (24.2 minutes farther on average), even compared to White women from similarly rural areas (5 to 13 minutes farther, after controlling for sociodemographic characteristics, risk factors, and health care utilization). AIAN women were 20 times more likely to give birth at a hospital without obstetric services and had less access to complex obstetric care. Poor access was particularly pronounced among reservation-dwelling AIAN women.
Conclusions:
It is imperative to consider racial disparities and health inequities underlying poor access to obstetric services across rural America. Current federal policies aim to reduce maternity care professional shortages. Our findings suggest that racial disparities in access to complex obstetric care will persist in Montana unless facility-level infrastructure is also expanded to reach areas serving AIAN women.
Keywords: American Indians, driving time, health care access, obstetrics, rural perinatal care
Maternal outcomes in the United States (US) are abysmal for a developed country. Nearly 700 women die each year due to pregnancy-related complications, and more than 50,000 women suffer from life threatening pregnancy-related complications, of which 60% are preventable.1,2 Black and American Indian/Alaskan Native (AIAN) women are 2 to 5 times more likely to die from a pregnancy-related complication compared to White women. Over 2.2 million childbearing-aged women live in maternity care deserts (a county bereft of a birth center, obstetric provider, and hospital-based obstetric unit), and another 4.8 million women live in counties with limited access to maternity care.3,4 Improving health care access is one way to improve maternal health outcomes amidst the intersections of rurality and race for AIAN women.
The concept of health care access includes potential and realized access to medical care.5 Facilities that provide specific services form the system that may be potentially accessed. Health care utilization is realized access. Lack of services within a reasonable travel time imposes a barrier to care when living rurally. For rural AIAN women, barriers to care are further compounded by high poverty rates and longer distances to available services covered by Indian Health Services (IHS)-funded programs.6 Improving understanding of rural racial inequalities in obstetric care access is paramount, given recent legislation to designate areas with limited obstetric care and to inform federal resource allocation decisions.7
Across the US, access to obstetric services has declined, particularly in rural counties with a higher percentage of racial minority women of childbearing age.8 Rural areas have a higher rate of under-insured women, fewer obstetrical providers, and limited access to facilities providing obstetric care, especially specialty clinical care.4,9 An increasing share of births to rural women occur in hospitals that lack an obstetrics unit or at non-local facilities.8,10 Rural women drive longer distances to access perinatal care,11 which is concerning since longer driving time and giving birth at facilities without an obstetrics unit increase the likelihood of poor outcomes, especially for high-risk deliveries.12,13,14 Using Montana as a case study, the current paper examines variation in travel time and access to different levels of obstetric care, and it considers how access varies by rurality and race.
Rural areas have poorer access to health care, and scarcity of services may be further exacerbated by cultural and financial constraints that reduce health-care-seeking behavior.15 Women living in rural and geographically isolated areas often travel long distances to obtain goods and services, including specialized obstetric care.11 Just 28.8% of reproductive-aged women in remote rural areas live within a 30-minute drive of hospital-based obstetrics services compared to 77.1% in micropolitan areas and 93.4% in metropolitan areas.11 Montana has the poorest access to obstetric services, in terms of long drive times.11 Maternal morbidity and birth outcomes are worse in remote rural areas,12,16,17 particularly at lower-volume rural hospitals.18 Losing obstetric services in remote rural areas appears to be more consequential than losing services in more urban or urban-adjacent rural areas in terms of increases in unplanned out-of-hospital births, births at hospitals without an obstetric unit, and preterm births.9
Access to obstetric care is worse for rural racial minorities.8 Counties with a high proportion of Non-Hispanic Black women had up to ten-fold higher odds of never having a hospital with obstetric services between 2004 and 2014, compared to counties with lower proportions of Non-Hispanic Black women.8 Racial disparities in health care access are more severe in rural areas than urban areas, including access to providers, procedures received, and travel time to health care generally and obstetric care specifically.11,19,20 Historically, scant attention has been given to the AIAN population; this is an important oversight.21
Despite long-standing federal government legal obligations to provide health care access to AIAN people, health services for this population are chronically underfunded.22 As a result, health care access is bleak; 92% of counties with an AIAN majority are designated as Health Professional Shortage Areas (HPSAs), compared to 65% of rural counties overall.19 AIAN women are nearly twice as likely as White women to travel outside of their residential county to give birth (37% verses 19%), and they are 3 times less likely to live in or travel to a county with a hospital that provides complex obstetric care (18% versus 61%).23 Compared to women of other racial backgrounds, AIAN women comprise the smallest percentage of childbearing-aged women who live within an hour of their nearest hospital-based obstetrics services (83.2%, compared to 97.3% for the overall US population of childbearing-aged women), and that nearest hospital is often one that provides only basic perinatal care.11
Although the AIAN population is diverse and rich with differing languages, customs, beliefs, and cultural practices, there is a shared history and experience of ongoing traumatic events and policies marked by genocide, forced acculturation and assimilation, loss of land, and chronic underfunding of trust obligations that have gravely impacted AIAN health regardless of location, and have contributed to a generalized mistrust.24,25 The enduring legacy of historical trauma is compounded with ongoing socioeconomic and structural conditions that create barriers for accessing services.20,26 Higher poverty rates (non-metro AIAN people’s incidence of poverty is 30.9%, more than double that of non-metro White people), limited economic development, declining infrastructure, problems recruiting and retaining specialty providers, geographic isolation of rural AIAN people, and difficulties accessing reliable transportation act as barriers to seeking care, especially specialized clinical care, and increase risk for poor birth outcomes.27,28
Despite provisions for health care through trust responsibility between the federal government and federally recognized tribes, the Indian Health Service (IHS) is severely underfunded, contributing to AIAN health disparities.22,29 AIAN women have higher rates of inadequate prenatal care. For example, 32.6% of AIAN women enter into prenatal care late, compared to 13.1% of White women. In addition, 44.6% of AIAN women have inadequate prenatal care using the Adequacy of Prenatal Care Utilization Index, compared to 23.9% of White women.29 Montana reservation-dwelling AIAN women served by IHS face a number of barriers to accessing care, including: remote proximity to obstetric services, clinician shortages, lack of provider continuity, limited maternal health services availability, communication barriers, financial burdens, and transportation barriers.30,31,32 Beyond geographic access to services, AIAN women may lack access to health care that is culturally safe, defined as patient-centered culturally congruent care that improves the provision of care and patient health outcomes.33
AIAN women have higher rates of poor birth outcomes compared to White women, including low birth-weight births (8.1% for AIAN women, compared to 7.1% for White women), twice the odds of pre-term delivery, almost twice the odds of infant mortality, and 4 times the odds of maternal mortality. 34,35,36,37,38 Rural AIAN women have almost double the risk of severe maternal morbidity and mortality (2.3%) compared to rural White women (1.3%).36 Racial inequalities in birth outcomes are wider in rural areas, due in part to closure of 100 rural hospitals since 2010.6,39 Remote-dwelling AIAN women may simultaneously need to drive farther to access obstetric services, especially higher-level specialty care, compared to their White counterparts, while experiencing higher risk of poor birth outcomes, and therefore greater need for more specialized services. As stated by Andersen and colleagues, “Equity of access may be said to exist when services are distributed on the basis of people’s need for them.”40 This scenario for AIAN women, in which services are least available to those with the greatest need, epitomizes health care inequity.5
Leveraging birth certificate data for the large rural state of Montana, we examined the supply of obstetric services, how well this supply of services covered the population, and equity in women’s access to services (ie, drive times). Montana is a very rural state, with 65% of its population living in rural areas compared to 14% of the total US population.41 Within Montana, approximately 78,000 people (6.7% of the population) self-identify as AIAN, and this state is home to 12 federally recognized tribal nations.42,43 Seven reservations are located across the state, and between 43% and 75% of enrolled members of these tribes live on or near their tribal reservation, with increasing recognition that AIAN people are not stagnant but move dynamically across reservation and state borders.43
Treaties within Montana were signed between 1851 and 1855, creating the original 7 reservations comprised of 12 nations.44Although each nation has its own unique identity, culture, language, and history, they share a common past marked by marginalization from systematic Westward Expansion and ensuing aftereffects. US federally recognized tribes have a sovereign, government-to-government relationship with the federal government. In exchange for ceding land, federally recognized tribes possess certain rights to self-government and entitlement to some federal benefits, services and protections including access to health care.44,45 It is beyond the scope of this paper to outline intricate similarities and differences among tiered federal, state, and municipal tribal recognition; however, similarities of a common experience have translated into shared maternal/infant outcomes, which demonstrate that our current system for maternal/infant care among this population is failing.
This study addresses several research gaps. First, evidence suggests that access to obstetric care is worse in rural compared to urban areas but few studies have examined variation across rural areas.8 Second, prior research indicates racial inequalities exist in obstetric care access, but with limited attention to AIAN women’s experiences.21 Moreover, research has not examined how intersecting identities of being an AIAN woman and living rurally impede access to obstetric services.8,11 Finally, this study extends previous research by examining access to multiple levels of obstetric care, which is especially critical given the higher health risk and poorer birth outcomes among AIAN women.34,46,47
Our findings highlight rural and racial health disparities that persist in Montana. This evidence can inform policy makers about the supply-demand alignment for obstetric services in rural America for White and AIAN women. Findings may inform federal and state policies for equitably allocating resources to hospitals. Current efforts to designate Maternity Care Health Professional Shortage Areas (MCTAs) should incorporate information on racial differences in access to and need for services to ensure efforts to bolster care in MCTAs address health care inequalities.48
Study Data and Methods
Data
The primary source of data was Montana birth certificates from 2014–2018 (n=60,461). Excluded from all samples were data on women who did not reside in Montana (n=961; 1.6%), Hispanic (n=2,694; 4.5%), Non-Hispanic Black (n=411; 0.7%), Non-Hispanic Asian or Pacific Islander women (n= 751; 1.3%), and records missing information on the birth facility (n=36; 0.1%) (Figure 1 and Table 1, n=55,608). Analyses examining driving time further excluded women who gave birth at home (n=1,377; 2.5%) or at birthing centers (n=833; 1.5%), and women missing data on driving time (n= 11; 0.0%), resulting in a sample size of 53,387 birth records (Table 2). Records missing values for variables in the final multivariate OLS model (n=2,708; 5.1%) were excluded from models in Table 3 (n = 50,679).
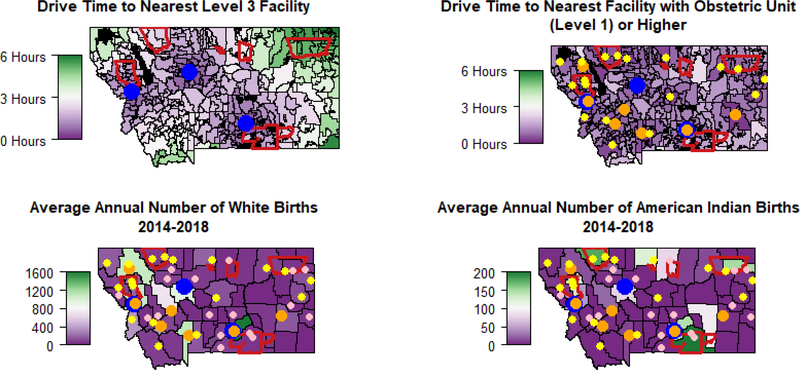
Figure 1. Obstetric Services Supply and Demand in Montana.
SOURCE: Author’s analysis of data from 55,608 Montana birth certificates from 2014–2018 of birth to White and AIAN women residing in Montana at the time of the birth who were not missing information on birth facility, with information on the birth facility from the 2018 American Hospital Association (AHA) Annual Survey.
NOTES: 1) Blue – Level 3 Facility, Orange – Level 2 Facility, Yellow – Level 1 Facility, Pink – Level 0 Facility
2) AIAN Reservation Borders are Outlined in Red
3) Large Water Bodies and Unpopulated Areas with no ZCTA are Black
Table 1:
Births occurring in Montana to women residing in Montana, by race and facility type, and by potential driving time thresholds, 2014–2018
| Facility type | Births | Number residing within one hour drive time of nearest facility type | Number residing within two hour drive time of nearest facility type | |||
|---|---|---|---|---|---|---|
| White women | AIAN women | White women | AIAN women | White women | AIAN women | |
| Obstetric Level 0 | 0.1% (25) | 1.2% (84) | 46.7% (22,817) | 59.3% (3,998) | 85.2% (41,615) | 98.5% (6,636) |
| Obstetric Level 1 | 18.8% (9,204) | 43.4% (2,938) | 52.2% (25,502) | 55.2% (3,723) | 94.3% (46,087) | 77.9% (5,250) |
| Obstetric Level 2 | 41.8% (20,444) | 24.2% (1,628) | 67.8% (33,145) | 25.6% (1,727) | 89.7% (43,825) | 52.1% (3,509) |
| Obstetric Level 3 | 34.9% (17,070) | 29.9% (2,015) | 40.1% (19,591) | 24.2% (1,634) | 57.8% (28,243) | 53.7% (3,620) |
| Birthing Center | 1.7% (827) | 0.1% (6) | 66.0% (32,250) | 27.4% (1,847) | 86.4% (42,230) | 58.2% (3,926) |
| Home Birth | 2.7% (1,298) | 1.2% (79) | n.a. | n.a. | n.a. | n.a. |
SOURCE: Authors’ analysis of data from 55,608 Montana birth certificates from 2014–2018 of births to White and AIAN women residing in Montana at the time of the birth who were not missing information on birth facility, with information on the birth facility from the 2018 American Hospital Association (AHA) Annual Survey.
NOTES: denominator for percentages is total number of White births or total number of AIAN births for which birth facility was identified.
Table 2:
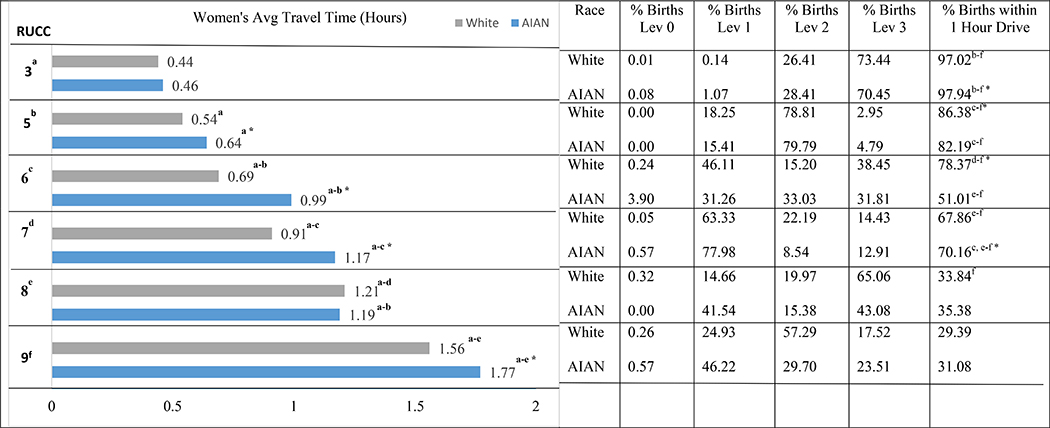
Travel and Facility Statistics by RUCC, Race for births occurring at hospitals
|
SOURCE: Authors’ analysis of data from 53,387 Montana birth certificates from 2014–2018 of births to White and AIAN women residing in Montana at the time of the birth, who gave birth at a hospital and were not missing information on driving distance to the birth facility, with information on the birth facility from 2018 American Hospital Association (AHA) Annual Survey.
NOTES: a-f represent that the mean is significantly larger than the mean for another RUCC within the same race at P < .05 based on Games-Howell post hoc paired comparisons of Analysis of Variance (ANOVA) test, assuming unequal variances. For % births within 1 hour, a-f represent that the odds ratio is significantly larger than 1 for another RUCC within the same race at P < .05 (Binary Logistic Regression).
denotes that the mean is significantly larger than the mean for the other race within the same RUCC at P < .05
Table 3:
Realized driving time to give birth (hours; OLS regression)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
|
| ||||||
| Race (White is ref) | ||||||
| American Indian/Alaskan Native | 0.404*** (0.01) | 0.205*** (0.01) | 0.143*** (0.01) | 0.009 (0.02) | 0.019 (0.02) | −0.006 (0.02) |
| Lives on reservation | 0.126*** (0.01) | 0.059** (0.02) | 0.220*** (0.01) | 0.222*** (0.01) | ||
| RUCC Rurality Measure (category 3 is ref) | ||||||
| RUCC 5 | 0.115*** (0.01) | 0.112*** (0.01) | 0.104*** (0.01) | 0.411*** (0.01) | 0.399*** (0.01) | |
| RUCC 6 | 0.301*** (0.01) | 0.259*** (0.01) | 0.231*** (0.01) | 0.518*** (0.01) | 0.493*** (0.01) | |
| RUCC 7 | 0.507*** (0.01) | 0.490*** (0.01) | 0.465*** (0.01) | 0.956*** (0.01) | 0.925*** (0.01) | |
| RUCC 8 | 0.784*** (0.02) | 0.777*** (0.02) | 0.775*** (0.02) | 0.856*** (0.01) | 0.837*** (0.01) | |
| RUCC 9 | 1.140*** (0.01) | 1.126*** (0.01) | 1.130*** (0.01) | 1.423*** (0.01) | 1.400*** (0.01) | |
| Race X RUCC interactions | ||||||
| AIAN X RUCC 5 | 0.091* (0.04) | 0.057 (0.04) | 0.062 (0.04) | |||
| AIAN X RUCC 6 | 0.274*** (0.03) | 0.142*** (0.03) | 0.158*** (0.03) | |||
| AIAN X RUCC 7 | 0.255*** (0.03) | 0.182*** (0.02) | 0.228*** (0.02) | |||
| AIAN X RUCC 8 | −0.030 (0.09) | 0.102 (0.08) | 0.123 (0.08) | |||
| AIAN X RUCC 9 | 0.134*** (0.03) | 0.084*** (0.03) | 0.093** (0.03) | |||
| Obstetric (OB) Level of care (level 3 ref) | ||||||
| OB Level 0 | −0.926*** (0.06) | −0.932*** (0.07) | ||||
| OB Level 1 | −0.800*** (0.01) | −0.761*** (0.01) | ||||
| OB Level 2 | −0.309*** (0.01) | −0.291*** (0.01) | ||||
SOURCE: Authors’ analysis of data from 50,679 Montana birth certificates from 2014–2018 of births to White and AIAN women residing in Montana at the time of the birth, who gave birth at a hospital and were not missing information on driving distance to the birth facility or missing data for variables in final multivariate model, with information on the birth facility from 2018 American Hospital Association (AHA) Annual Survey.
NOTES: standard errors in parentheses
P < .05
P < .01
P < .001
Model 6 is the full multivariate model controlling for: maternal education, marital status, WIC status, risk factors in pregnancy, smoking during pregnancy, pre-pregnancy obesity, Kotelchuck adequacy of prenatal care index, health insurance, and if the birth was preterm.
Hospital-level data from the 2018 American Hospital Association (AHA) Annual Survey were used to measure obstetric unit care level (level 1, offers services for uncomplicated cases; level 2, offers services for all uncomplicated and most complicated cases; level 3, offers services for all complicated cases).47 Hospitals where births occurred that did not have an obstetrics unit were categorized as level 0.
Measures
The dependent variable was pregnant women’s driving time (in hours) from home to birth facility. We calculated the driving distances and driving times from the centroid of the ZIP Code of residence to the address of each birth facility using a Python script to access the Google Distance Matrix API.49
Rurality of residence was measured at the county level, based on the Department of Agriculture’s Economic Research Service classification scheme called the Rural-Urban Continuum Code (RUCC). Out of the 9 possible categories of RUCC, the following 5 RUCC categories were present in our dataset: 3 “metro, population < 250,000,” 5 “nonmetro, urban population > 20,000, nonadjacent to metro area,” 6 “nonmetro, urban population between 2,500 and 19,999, adjacent to metro area,” 7 “nonmetro, urban population between 2,500 and 19,999, nonadjacent to metro area,” 8 “nonmetro, completely rural or less than 2,500 urban population, adjacent to metro area,” and 9 “nonmetro, completely rural or less than 2,500 urban population, nonadjacent to metro area.” RUCC defines a county as adjacent if it physically borders a metro county, and some of its population commutes to the metro county.
Several maternal characteristics were included in the study, including race. In our data, 82.2% of births were to White women, 11.2% of births were to AIAN women, and 6.5% of births were to women of other races. We focused our analyses on births to White and AIAN women. Several sociodemographic characteristics were also examined, given their association with maternal health and health care.50 Information from the birth certificate data, completed by the birthing person, was used to measure binary indicators of whether the birthing woman: lived on an Indian reservation, was married, received assistance from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and paid for the childbirth using any of the following sources (Medicaid, Private, Indian Health Service, Military, or Self-pay). We included a categorical variable measuring education (less than high school education, high school education, some college, college degree plus). These measures act as proxies for socioeconomic status and social location. Prior literature indicates that AIAN women and individuals living in more socioeconomically disadvantaged environments have substantially longer travel distances to access perinatal care.8,11,51 Given evidence of social gradients in health care access and under-funding of IHS, we hypothesize that AIAN women, women living on reservations, unmarried women, women on WIC, women with lower levels of education, and women who lack health insurance will travel significantly farther to access obstetric care.
To account for the riskiness of the pregnancy and births, we included several controls including: health risk factors in pregnancy (0 “none,” 1 “one,” 2 “two or more”; eg, diabetes, pre-eclampsia), binary indicators if the woman smoked during pregnancy, pre-pregnancy obesity (body mass index > 30 km/m2), and preterm birth (less than 37 weeks gestation). We included the Kotelchuck adequacy of prenatal care index, which defines prenatal care adequacy based on earlier initiation of care and utilization of the expected, appropriate number of prenatal visits after initiating care (range: 0 “no prenatal care” to 4 “adequate plus prenatal care”).52
Analysis
We analyzed access to hospital-based childbirth facilities in Montana in several ways. First, using maps we visualized the differences between obstetric service demand (average annual number of births by county) across the state for White and AIAN women along with the differences in drive time to birth facilities by ZIP Code tabulated area (ZCTA).
Next, we examined the supply of obstetric services as the proportion of White and AIAN pregnant women within 1- and 2-hour drive times from the nearest facility providing each obstetric care level. The unit of analysis was the birth facility. A 1-hour drive time is approximately the farthest people are inclined to travel for specialty health care, and it has been shown to be the farthest safe drive time for maternity patients.11,40 Given our focus on Montana, a very rural state with some extreme travel times, we also identified women within a 2-hour drive time.
Third, we examined differences in women’s actual drive times by rurality and maternal race using Analysis of Variance (ANOVA) tests. Finally, we performed a series of multivariate linear regression analyses to examine associations between maternal demographics, obstetric unit care level, and drive times. The unit of analysis was the birth record. This research was approved by the IRB at Montana State University.
Results
As with other rural places, Montana’s supply of obstetric services is limited. Spanning 145,545 square land miles and with a population of 1.07 million, the fourth-largest state geographically in the United States and the third least-densely populated, the state of Montana has only 3 hospitals categorized as level 3 facilities capable of providing care for complex maternal and fetal medical conditions and obstetric complications.30,46,53
Figure 1 displays the supply and demand for obstetric services in Montana. The upper-left image shows drive time to the nearest level 3 facility and the upper-right shows drive time to the nearest facility with an obstetric unit. Approximately 24% of all ZCTAs are more than 3 hours away from a level 3 facility (9% of total births). While most women in Montana live closer to hospitals with an obstetric unit (level 1 or higher), 40% of ZCTA’s are more than 1 hour away from any facility with an obstetric unit (12% of total births). The 2 lower images display county-level, average annual number of White and AIAN births. The facilities that can handle more complicated births, levels 2 and 3, generally align with counties where more births occurred, particularly White births.
Table 1 presents information on the supply of obstetric services in Montana. The system of hospital-based obstetric units was very stable between 2014–2018, with 0 closures and only 1 addition of hospital-based obstetrics. Births to White women were more likely to occur at a level 2 than at a level 1 facility (41.8% versus 18.8%), while births to AIAN women were more likely to occur at a level 1 than at a level 2 facility (43.4% versus 24.2%). The differences were less pronounced for level 3 facilities, with 34.9% of births to White women and 29.9% of births to AIAN women occurring at these facilities. AIAN women were over 20 times more likely to give birth at a hospital that lacked an obstetric unit (level 0).
Examining proximity to potential birth facilities, we found that a majority of White women (67.8%) resided within a 1-hour drive of a level 2 facility, with the preponderance of White women (89.7%) residing within a 2-hour drive of a level 2 facility. Conversely, fewer AIAN women resided within such proximity to level 2 facilities, with a minority (25.6%) residing within a 1-hour drive and a slight majority (52.1%) residing within a 2-hour drive. Considering proximity to level 3 facilities, a minority of White and AIAN women resided within a 1-hour drive (40.1% and 24.2%, respectively), while a majority of White and AIAN women resided within a 2-hour drive (57.8% and 53.7%, respectively). These differences were all statistically significant (P < .001). Supplementary analyses suggest that proximity to higher-level obstetric services is particularly poor among AIAN women living on reservations (see Appendix Table A1).
Turning next to realized access, results suggest that drive times to give birth varied among women, particularly by the degree of rurality where they lived and their racial identity. On average women traveled 42 minutes (32 miles) from their home to give birth, but approximately 20% drove over 1 hour, with some women driving upwards of 10 hours. Rurality was associated with travel time, with significantly shorter travel times for women living in more urban areas (Table 2). Further, most births to women living in more populated counties (RUCC 3 and 5) occurred at level 2 and level 3 facilities, but significantly fewer births to women living in rural counties took place at level 2 or 3 facilities. Supplementary analyses suggest that, with respect to potential access, rural women would need to travel significantly farther to access facilities with higher levels of obstetric care (see Appendix Table A2).
Considering racial differences, in terms of realized access, AIAN pregnant women traveled significantly farther than White women to access care, even when compared to White women living in similarly rural areas (Table 2). A smaller percentage of AIAN women gave birth at higher-level facilities compared to White women living in similarly rural areas. In terms of potential access, pregnant AIAN women would have to travel significantly farther to access higher-level facilities compared to White women (see Appendix Table A2).
Racial differences are larger for hospitals with obstetric units addressing complicated cases (levels 2 and 3). In supplementary analyses we found that 33% of AIAN women in our sample were diagnosed with 1 or more pregnancy health risk factor(s), compared to 27% of White women (a statistically significant difference at P < .001 based on t-test). Focusing on the most remote, rural areas (RUCC 7 and 9), we found that White women diagnosed with 1 or more pregnancy risks resided, on average, 1.84 hours from the nearest level 2 and 2.91 hours from the nearest level 3 hospital; the comparable values for AIAN women were 2.64 and 3.12 hours, respectively. High-risk pregnant AIAN women would have to travel statistically significantly farther than White women to access the same level of care (P < .001, based on t-test). Considering utilization, these same high-risk pregnant AIAN women, diagnosed with 1 or more pregnancy health risk(s), were less likely than White women to give birth at level 2 or level 3 hospitals (58% vs 81%; see Appendix Table A3).
Results thus far suggest that both rurality and race are associated with women’s access to obstetric services. Table 3 presents the results of a series of ordinary least-squares (OLS) regression models predicting actual driving time to give birth, in hours. Pregnant AIAN women drove farther than White women to give birth (24.2 minutes further; CI: 23.1–25.4; Model 1). Women living in more rural areas (Models 2–6) and women living on reservations (Models 3–6) also drove farther to give birth. The longer driving times among AIAN women were mediated in part by rurality (Model 2), and residence on reservation (Model 3). Significant interactions between rurality and race (Models 4–6) indicate that AIAN women living in rural and geographically isolated areas traveled significantly farther to give birth compared to White women living in similarly rural places, in particular for RUCCs 6, 7 and 9.
Turning to obstetric care level (Models 5–6), results suggest that women who gave birth at level 3 facilities traveled the farthest to give birth. Controlling for level of care also helps to mediate the longer travel time among rural AIAN women; rural AIAN women traveled farther than their White counterparts in part because they are traveling farther to access higher levels of obstetric care. Supplementary analyses suggest that the longer travel time to access higher levels of care is especially pronounced among women living on reservations (see Appendix Table A4). Results in the final multivariate model (model 6) suggest that when controlling for sociodemographic characteristics, health and health care utilization in pregnancy, AIAN women travel significantly farther to give birth than White women, but only in rural areas. Results of interactions in the final multivariate model indicate that driving time is significantly longer for rural AIAN women compared to White women living in similarly rural areas (RUCC 6 = 9.5 minutes longer, CI: 6.5–12.5; RUCC 7 = 13.7 minutes, CI: 10.8–16.5, RUCC 9 = 5.6 minutes, CI: 2.1–9.1).
Discussion
Women face barriers to accessing obstetric care in rural America. We found that rural AIAN women are additionally disadvantaged, relative to rural White women, with respect to both their potential and realized access to obstetric services. Hospitals with obstetric units, especially those providing complex care, were located farther from AIAN women, particularly those living on reservations. When they gave birth, AIAN women traveled significantly farther and were less likely to give birth at facilities that provided complex care. These findings hold when comparing White and AIAN women who had riskier pregnancies. The barrier to seeking specialized care was particularly great for AIAN women living in remote, rural areas; AIAN women with diagnosed pregnancy complications living in these areas would, in most cases, have to travel over 3 hours to give birth at level 3 facilities that are best equipped to handle high-risk deliveries. Future research will examine how limited access to care is linked with birth outcomes among rural AIAN women and communities. The broader regional context should also be considered, including racial and socioeconomic composition, given prior research suggesting these factors are associated with both perinatal care utilization and birth outcomes.54
Our results echo that inequities exist in the current health care system for AIAN women.11,13,23 Further, we recognize that diversity among AIAN cultures, beliefs and practices exists; however, we propose that a shared history born from colonization and assimilation contribute to a “global” and “common” lived AIAN experience which impacts health.25 Though geographical and local cultural differences exist among AIAN people (Alaska vs. Southwest vs. Midwest), we propose that broader policy efforts to address the limited and decreasing supply of obstetric services and shortages in maternity health care professionals in rural areas should directly address gaps in coverage for racial minorities, especially AIAN women.8,48 Further, any changes made to the system should be guided by input from community and tribal leaders who have the best understanding of the needs and priorities of their community, and build upon resilience or reziliency evident in the mere presence of a people despite systematic oppression.33,55,56 Reziliency refers to the unique set of protective factors within American Indian communities that contribute to “adaptively resilient reintegration” among this population.56
Part of implementing the Improving Access to Maternity Care Act involves distributing maternity care professionals to MCTAs through the National Health Service Corps (NHSC) awarding mechanism.7 Our results point to the challenge of distributing professionals to areas in need without obstetric units, where infrastructure may not be sufficient to provide complex care for high-risk births. For example, a preterm pregnancy complicated by premature rupture of membranes and increasing severity of preeclampsia requires specialized obstetrical and neonatal intensive care unit personnel and resources to promote healthier maternal/infant outcomes. Even with policy efforts to increase the number of professionals in underserved areas, our findings suggest that racial disparities in access to complex obstetric care will persist unless facility-level infrastructure is also expanded to reach areas serving AIAN women.
Furthermore, recruitment and retention of obstetric providers are documented problems among AIAN communities due to remote living situations, understaffed or inadequate technology, and aging infrastructures.28 However, there is ample ground to broaden the pool of allied health professionals such as lactation consultants, certified nurse midwives, certified midwives, physician assistants, and birth workers (eg, doulas and community health partners) to care for this population.57 Investing in the community by increasing the AIAN provider workforce is another route to obtain cultural safety and capitalize upon reziliency, while providing a much-wanted service for this at-risk population.58,59
Issues of maternity health care access are not limited to childbirth; rural AIAN women have poorer prenatal care utilization.21 While in-person perinatal visits are ideal, rural AIAN women face abundant obstacles in access related to transportation and geographic isolation.28 Thus, incorporating telehealth with supplying women health literacy on using self-monitoring devices (eg, blood pressure cuffs) may both improve prenatal visits and the assessment and treatment of high-risk pregnancies. Innovative transportation systems and programs such as mobile obstetrical suites or emergency medical transports that directly link AIAN women to services may improve perinatal care use, identify and treat high-risk pregnancies, and improve subsequent birth outcomes.
Limitations
This study has several limitations. First, Montana-centered data limits the generalizability of our results. However, Montana is an excellent setting to study our research questions since Montana has the 5th highest proportion of AIAN population among US states and is very rural, with 65% of the population living in rural areas.60,27 Further, Montana has the most limited access to obstetric care in the US, in terms of driving time.11 Montana can be considered an ideal case study of how the most rural AIAN women access and utilize obstetrical services given similarly shared access issues across rural AIAN populations.
Second, drive times were approximated using the centroid of women’s residential ZIP Code, as we did not have their residential addresses, leading to some imprecision in our estimates. Third, we do not control for birth to multiples (eg, twins) or siblings during the study period; therefore, multiple birth records could be attributed to the same woman. Fourth, the RUCC measure was aggregated to the county level, but counties in Montana are large and may have variable rurality. It was not possible to measure RUCC at a smaller level of geographic detail, as information on women’s location was limited to ZIP Codes, which often cross multiple census tracts. Finally, the accuracy in which the forms were completed correctly, or entered correctly into the statewide database may affect the validity and reliability of data used.61
Conclusion
Our findings indicate clear divisions between rural AIAN women and rural White women in access to and use of obstetric services. Racial equity in access should be one of the objectives when advocating for wider distribution of advanced obstetrical centers and specialists. Any policy efforts to reduce maternal health inequalities for AIAN women must involve identifying limitations in the current health care delivery system and developing creative solutions, in collaboration with community and tribal leaders, while also identifying and addressing underlying health inequities for this population.
Supplementary Material
Acknowledgments
Funding: Research reported in this manuscript was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number P20GM104417. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Hoyert DL, Miniño AM. Maternal mortality in the United States: changes in coding, publication, and data release, 2018. Natl Vital Stat Rep. 2020. January;69(2):1–18. [PubMed] [Google Scholar]
- 2.Centers for Disease Control. Building U.S. Capacity to Review and Prevent Maternal Deaths. Report from nine maternal mortality review committees. 2018. https://www.cdcfoundation.org/sites/default/files/files/ReportfromNineMMRCs.pdf. Accessed December 4, 2020.
- 3.Centers for Disease Control. Racial and Ethnic Disparities Continue in Pregnancy-Related Deaths. 2019. https://www.cdc.gov/media/releases/2019/p0905-racial-ethnic-disparities-pregnancy-deaths.html. Accessed December 4, 2020.
- 4.March of Dimes. Nowhere to go: Maternity care deserts across the U.S. 2020. https://www.marchofdimes.org/research/maternity-care-deserts-report.aspx. Accessed December 4, 2020
- 5.Slifkin R Developing policies responsive to barriers to health care among rural residents: What Do we need to know? J Rural Health. 2002;18(5):233–241. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin LM, Grossman DC, Casey S, et al. Perinatal and infant health among rural and urban American Indians/Alaska Natives. Am J Public Health. 2002;92(9):1491–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Congress. Improving Access to Maternity Care Act. 2018. P.L. 115–320; Public Health Service Act, Section 332(k). https://www.congress.gov/115/plaws/publ320/PLAW-115publ320.pdf. Published December 17, 2018. Accessed September 14, 2020.
- 8.Hung P, Henning-Smith CE, Casey MM, Kozhimannil KB. Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004–14. Health Aff. 2017;36(9):1663–1671. [DOI] [PubMed] [Google Scholar]
- 9.Kozhimannil KB, Hung PY, Henning-Smith C, Casey MM, Prasad S. Association between loss of hospital-based obstetric services and birth outcomes in rural counties in the United States. JAMA. 2018;319(12):1239–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kozhimannil KB, Casey MM, Hung PY, Prasad S, Moscovice IS. Location of childbirth for rural women: implications for maternal levels of care. Am J Obstet Gynecol. 2016;214(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rayburn WF, Richards ME, Elwell EC. Drive times to hospitals with perinatal care in the United States. Obstet Gynecol. 2012;119(3):611–616. [DOI] [PubMed] [Google Scholar]
- 12.Grzybowski S, Stoll K, Kornelsen J. Distance matters: a population based study examining access to maternity services for rural women. BMC Health Serv Res. 2011;11,147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nesbitt TS, Connell FA, Hart LG, Rosenblatt RA. Access to obstetric care in rural-areas - Effect on birth outcomes. Am J Public Health. 1990;80(7):814–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109(5):745–751. [DOI] [PubMed] [Google Scholar]
- 15.Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. [DOI] [PubMed] [Google Scholar]
- 16.Sparks PJ, McLaughlin DK, Stokes CS. Differential neonatal and postneonatal infant mortality rates across US counties: the role of socioeconomic conditions and rurality. J Rural Health. 2009;25(4):332–341. [DOI] [PubMed] [Google Scholar]
- 17.Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK. Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health Aff. 2019;38(12):2077–2085. [DOI] [PubMed] [Google Scholar]
- 18.Kozhimannil KB, Hung P, Prasad S, Casey M, McClellan M, Moscovice IS. Birth volume and the quality of obstetric care in rural hospitals. J Rural Health. 2014;30(4):335–343. [DOI] [PubMed] [Google Scholar]
- 19.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health. 2004;94(10):1695–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health. 2016;106(8):1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kozhimannil KB. Indigenous maternal health – A crisis demanding attention. JAMA Health Forum. 2020;1(5):e200517–e200517. [DOI] [PubMed] [Google Scholar]
- 22.Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. Am J Public Health. 2014;104(S3):S263–S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Von Reichert C, McBroom WH, Reed FW, Wilson PB. Access to health care and travel for birthing: Native American-white differentials in Montana. Geoforum. 1995;26(3):297–308. [Google Scholar]
- 24.Canales MK, Weiner D, Samos M, Wampler NS, Cunha A, Geer B. Multi-generational perspectives on health, cancer, and biomedicine: Northeastern Native American perspectives shaped by mistrust. J Health Care Poor Underserved. 2011;22(3):894–911. [DOI] [PubMed] [Google Scholar]
- 25.Palacios JF, Portillo CJ. Understanding Native women’s health: Historical legacies. J Transcult Nurs. 2009;20(1):15–27. [DOI] [PubMed] [Google Scholar]
- 26.Braveheart MYH, DeBruyn LM. The American Indian holocaust: Healing historical unresolved grief. Am Indian Alsk Native Ment Health Res. 1998;8(2):56–78. [PubMed] [Google Scholar]
- 27.United States Department of Agriculture, Economic Research Service. Rural Poverty and Well-being. 2020. https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/#historic. Published February 12, 2020. Accessed September 14, 2020.
- 28.Cromer KJ, Wofford L, Wyant DK. Barriers to Healthcare Access Facing American Indian and Alaska Natives in Rural America. J Community Health Nursing. 2019;36(4):165–187. [DOI] [PubMed] [Google Scholar]
- 29.Johnson PJ, Call KT, Blewett LA. The importance of geographic data aggregation in assessing disparities in American Indian prenatal care. Am J Public Health. 2010;100(1):122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ranji U, Long M, Salganicoff A, et al. Beyond the Numbers: Access to reproductive health care for low-income women in five communities. Kaiser Family Foundation. https://www.kff.org/report-section/beyond-the-numbers-access-to-reproductive-health-care-for-low-income-women-in-five-communities-crow-tribal-reservation-mt/. Published November 14, 2019. Accessed September 15, 2020. [Google Scholar]
- 31.Committee on American Indian/Alaska Native Women’s Health. Committee Opinion: Health Care for Urban American Indian and Alaska Native Women. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2012/01/health-care-for-urban-american-indian-and-alaska-native-women. Published January 2012. Accessed September 15, 2020.
- 32.Hanson JD. Understanding prenatal health care for American Indian women in a Northern Plains tribe. J Transcult Nurs. 2012;23(1):29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brooks-Cleator L, Phillipps B, Giles A. Culturally safe health initiatives for Indigenous Peoples in Canada: a scoping review. Can J Nurs Res. 2018;50(4):202–213. [DOI] [PubMed] [Google Scholar]
- 34.March of Dimes. Peristats. Low birthweight by race. https://www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=99&top=4&stop=45&lev=1&slev=1&obj=1#:~:text=During%202016%2D2018%20(average),%25)%20and%20whites%20(7.1%25). Accessed on December 4, 2020.
- 35.Centers for Disease Control. Infant Mortality. 2020. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.html. Accessed December 4, 2020.
- 36.Kozhimannil KB, Interrante JD, Tofte AN, Admon LK. Severe Maternal Morbidity and Mortality Among Indigenous Women in the United States. Obstetrics and Gynecology. 2020;135(2):294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control. Racial and Ethnic Disparities Continue in Pregnancy-Related Deaths. 2019. https://www.cdc.gov/media/releases/2019/p0905-racial-ethnic-disparities-pregnancy-deaths.html. Accessed December 4, 2020.
- 38.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202(4):335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Medicare and Medicaid Services. Improving access to maternal health care research in communities. Issue Brief. https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/rural-health/09032019-Maternal-Health-Care-in-Rural-Communities.pdf. Published September 3, 2019. Accessed August 24, 2020.
- 40.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res. 1983;18(1):49. [PMC free article] [PubMed] [Google Scholar]
- 41.United States Department of Agriculture. Economic Research Service. State Fact Sheets 2020. https://www.ers.usda.gov/data-products/state-fact-sheets/. Accessed December 4, 2020.
- 42.United States Census Bureau. Quickfacts: Montana. 2020. https://www.census.gov/quickfacts/MT. Accessed December 4, 2020.
- 43.Montana Governor’s Office of Indian Affairs. Tribal Nations. https://tribalnations.mt.gov/tribalnations. Accessed December 4, 2020. [Google Scholar]
- 44.Montana Office of Public Instruction. Division of Indian Education. Montana Indians: Their History and Location. http://opi.mt.gov/Portals/182/Page%20Files/Indian%20Education/Indian%20Education%20101/Montana%20Indians%20Their%20History%20and%20Location.pdf. Accessed December 4, 2020. [Google Scholar]
- 45.Haozous EA, Strickland CJ, Palacios JF, Solomon TG. Blood politics, ethnic identity, and racial misclassification among American Indians and Alaska Natives. J Environ Public Health. 2014; 2014:321604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brantley MD, Davis NL, Goodman DA, Callaghan WM, Barfield WD. Perinatal regionalization: a geospatial view of perinatal critical care, United States, 2010–2013. Am J Obstet Gynecol. 2017;216(2):185–e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine, ilpatrick SJ, Menard MK, Zahn CM, Callaghan WM. Obstetric Care Consensus #9: Levels of Maternal Care. Am J Obstet Gynecol. 2019;221(6):B19–B30. [DOI] [PubMed] [Google Scholar]
- 48.Health Resources and Services Administration. Maternity Care Health Professional Target Area Criteria Request for Information (RFI). https://bhw.hrsa.gov/shortage-designation/maternity-care-information-request?utm_campaign=Learn+the+Latest+Tools+to+Address+Clinician+Burnout+-+webinar+on&utm_medium=email&utm_source=govdelivery. Published May 2020. Accessed September 14, 2020.
- 49.Ozimek A, Miles D. Stata utilities for geocoding and generating travel time and travel distance information. The Stata Journal. 2011;11(1):106–119. [Google Scholar]
- 50.Wang E, Glazer KB, Howell EA, Janevic TM. Social Determinants of Pregnancy-Related Mortality and Morbidity in the United States: A Systematic Review. Obstetrics & Gynecology. 2020;135(4):896–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hung P, Casey MM, Kozhimannil KB, Karaca-Mandic P, Moscovice IS. Rural-urban differences in access to hospital obstetric and neonatal care: how far is the closest one? Journal of Perinatology. 2018;38(6):645–652. [DOI] [PubMed] [Google Scholar]
- 52.Kotelchuck M An evaluation of the Kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health. 1994;84(9):1414–14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.US Census Bureau. QuickFacts: Montana. US Census Bureau. https://www.census.gov/quickfacts/MT. Published 2019. Accessed September 14, 2020. [Google Scholar]
- 54.Thorsen ML, Thorsen A, McGarvey R. Operational efficiency, patient composition and regional context of US health centers: Associations with access to early prenatal care and low birth weight. Soc Sci Med. 2019;226:143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bylander J Designing a health system that works for the tribe. Health Aff 2017; 36(4):592–595. [DOI] [PubMed] [Google Scholar]
- 56.Belcourt-Dittloff AE. Resiliency and risk in Native American communities: A culturally informed investigation (Doctoral dissertation, University of Montana). [Google Scholar]
- 57.Thomas MP, Ammann G, Brazier E, Noyes P, Maybank A. Doula services within a healthy start program: increasing access for an underserved population. Matern Child Health J. 2017;21(1):59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morales L Indigenous initiative on Navajo Nation seeks to reduce maternal mortality rate. Arizona Central. 2019. https://www.azcentral.com/story/news/local/arizona/2019/11/18/changing-woman-initiative-navajo-nation-seeks-reduce-maternal-mortality-rate/4202343002/. Accessed December 2, 2020. [Google Scholar]
- 59.Robeznieks A Native Americans work to grow their own physician workforce. American Medical Association. 2019. https://www.ama-assn.org/practice-management/physician-diversity/native-americans-work-grow-their-own-physician-workforce. Accessed December 2, 2020. [Google Scholar]
- 60.US Census Bureau. Table PEPASR5H: Annual Estimates of the Resident Population by Sex, Age, Race Alone or in Combination, 2018 Population Estimates. https://factfinder.census.gov/bkmk/table/1.0/en/PEP/2018/PEPASR5H. Published June 20, 2019. Accessed June 30, 2019.
- 61.Northam S, Knapp TR. The reliability and validity of birth certificates. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2006;35(1):3–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.