Abstract
Background:
The extent to which uptake of biomedical HIV prevention strategies has impacted population-level sexual behavior and sexually transmitted infections (STI) among men who have sex with men (MSM) is not well understood.
Methods:
We collected data as part of routine care from MSM attending the municipal STI clinic in Seattle, Washington, 2002–2018. MSM were asked about condom use in the prior 12 months. We classified behaviors into four mutually exclusive categories: no anal sex; consistent condom use for anal sex; serosorting (condomless anal sex [CAS] only with HIV-concordant partners); and CAS with serodiscordant/unknown-status partners. STI/HIV testing was performed per routine clinic protocol.
Results:
There were 45,656 and 6,987 visits by MSM without HIV and MSM with HIV, respectively. Use of antiretroviral therapy and pre-exposure prophylaxis increased substantially during the study period, to 94% and 50%, respectively, by 2018. CAS with serodiscordant/unknown-status partners decreased through 2013 but increased thereafter (to 40% among MSM without HIV; 68% among MSM with HIV). Serosorting increased among MSM without HIV, but declined after 2013 among MSM with HIV. Consistent condom use declined for all MSM (from 35% to 11% among MSM without HIV; from 20% to 5% among MSM with HIV). HIV test positivity declined substantially (3.5% to 0.5%) while STI test positivity increased over time.
Conclusions:
Since 2013, CAS with HIV-discordant/unknown-status partners increased substantially concurrent with declining HIV test positivity and increasing STI test positivity. This highlights the success of biomedical HIV prevention strategies to reduce HIV incidence while affirming the need for new approaches to STI prevention.
Keywords: HIV, men who have sex with men, sexual behavior, sexually transmitted diseases
INTRODUCTION
Behavioral HIV prevention strategies that incorporate sex partners’ perceived HIV status have been commonly reported by men who have sex with men (MSM) since the early 1990s.1,2 These behaviors, which include serosorting (i.e., choosing partners or using condoms based on partners’ perceived HIV status), have been increasing since the early 2000s and have expanded to incorporate partners’ antiretroviral therapy (ART) or pre-exposure prophylaxis (PrEP) use.3–5 Some of these behavioral strategies, including serosorting, are associated with a lower risk of HIV compared to condomless anal sex (CAS) with partners living with HIV or of unknown status, but are also associated with a higher risk of bacterial sexually transmitted infections (STI).2,6–9 Accordingly, large shifts in the MSM population’s behavior has the potential to modify population-level HIV/STI rates, depending on which behaviors are being adopted with greater frequency. HIV incidence among MSM in the United States has declined somewhat over the past 10 years and, in some areas, has declined dramatically10 while rates of STI have increased substantially during that same period11, suggesting that increasing use of ART and PrEP, as well as changing patterns in the MSM population’s sexual behavior, may be contributing to these divergent trends in the incidence of HIV and STIs.
At the Public Health – Seattle and King County (PHSKC) Sexual Health Clinic (SHC; previously known as the STD clinic), we have collected detailed sexual behavior data from MSM patients since October 2001 and have used these data to monitor changes in the population’s sexual behavior. In our most recent published report7, we observed that CAS with serodiscordant or unknown-status partners had declined substantially from 2002 to 2013 concurrent with significant increases in serosorting. We concluded that this change represented a shift toward behaviors associated with a lower risk of HIV, which likely contributed to a decline in HIV test positivity during that time. However, with widespread promotion of treatment as prevention since 201112 and the approval of Truvada® for PrEP in 2012, it is unclear if these previously observed patterns of behavior have persisted. The objective of this study was to extend our previous findings by examining trends in sexual behavior in the SHC from 2002 to 2018, and to examine changes in the risk of STI over time for different behavioral HIV prevention strategies.
METHODS
Study design and population
This is a secondary data analysis of clinical records from MSM who attended the PHSKC SHC from January 1, 2002 to December 31, 2018. The start date for this study reflects the first full year when the PHSKC SHC began collection of detailed sexual behavior information. We defined MSM to be cisgender men who reported a male sex partner in the prior 12 months. We limited the analysis to MSM with complete sexual behavior data.
Data collection and measures
All data in this analysis were collected as part of routine clinical care. Until October 2010, clinicians conducted face-to-face interviews (FTFI) with patients to collect information on sexual behavior, HIV testing, drug use, and STI history. All information from FTFI were recorded on standardized paper chart forms and subsequently entered into the clinic’s electronic medical record database. Beginning in October 2010, the clinic began collecting these data from patients via a computer-assisted self-interview.
As part of routine care, we ask all patients about the gender of their sex partners. MSM patients are asked if they had insertive or receptive anal sex with partners who were living with HIV, did not have HIV, or were of unknown status, and how often they used condoms with partners (always/usually/sometimes/never), stratified by sexual role (insertive or receptive) and partner HIV status. All sexual behavior questions reference the prior 12 months. Using these data, we constructed the following mutually exclusive sexual behavior categories: (1) no anal sex: did not report anal sex; (2) consistent condom use: always used condoms with anal sex partners regardless of partner HIV serostatus; (3) serosorting: condomless anal sex (CAS) exclusively with HIV-concordant partners and always used condoms with discordant/unknown-status partners or did not have discordant/unknown-status partners; and (4) serodiscordant CAS: men who reported usually, sometimes, or never using condoms for anal sex with HIV-discordant/unknown-status partners.
Since 2002, we have asked patients living with HIV if they are currently taking ART. In 2013 we began asking patients without HIV if they had ever used PrEP. During the study period, we did not ask patients about current PrEP use. For this analysis, men who did not provide data on PrEP use were considered to have never used PrEP. Our clinic began offering PrEP to patients in October 2014.
HIV and STI Testing
All HIV and STI testing were performed per routine standard of care. Details on the types of laboratory tests used and how these changed over the study period have been previously described.7 Briefly, HIV testing was recommended for MSM who had not previously tested HIV positive and syphilis testing was recommended for all MSM. Before 2013, urethral specimens (swab or urine) for Neisseria gonorrhoeae (GC) and Chlamydia trachomatis (CT) testing were obtained from patients who reported urethral exposures. Beginning in 2013, urethral specimens were obtained from patients with signs/symptoms of urethritis or who reported contact to a partner with GC/CT. We obtained rectal specimens from MSM who reported receptive anal sex in the prior year. Our clinic transitioned from culture to nucleic acid amplification testing (NAAT) for GC/CT in 2011. For this analysis we grouped GC and CT test positivity together. We defined early syphilis as primary, secondary, or early latent stages.
Statistical analysis
We used Stata version 16.1 (StataCorp LLC, College Station, TX) for all analyses. Tests were performed at a significance level of 0.05. This study was reviewed and approved by the University of Washington Institutional Review Board.
We conducted three analyses: describing trends in sexual behavior over time, describing trends in HIV/STI test positivity over time by reported behavior, and testing the association between behavior and STI test positivity over time. All analyses were stratified by HIV status.
Trends in Sexual Behavior
We restricted this analysis to each man’s first visit to the SHC in a calendar year, and report trends in behavior using the four behavioral categories outlined above. We also compare behaviors among MSM who reported ever versus never using PrEP.
Trends in HIV/STI Test positivity
The unit of analysis was the clinic visit and was limited to individuals who were tested for HIV or an STI at that visit. For this analysis we combined the behavioral categories “no anal sex” and “consistent condom use” into a single category called “no condomless anal sex”.
Association between Behavior and HIV/STI Test Positivity
Using the same study population and behavioral categories described for the HIV/STI trends analysis above, we tested the association between behaviors and HIV/STI risk using log binomial regression models with robust standard errors to estimate relative risks (RR) and 95% confidence intervals (CI). All models were adjusted for age, race and ethnicity, number of sex partners in the past 12 months, calendar year, and methamphetamine use. We present RR comparing HIV/STI risk for serosorting compared to serodiscordant CAS and serosorting compared to no CAS. To determine whether or not the association between sexual behavior and HIV/STI risk changed over time, we included an interaction term for calendar year to test for statistical evidence of interaction. We also present RRs stratified by calendar time using the following three time periods: 2002–2007, 2008–2013, and 2014–2018.
RESULTS
From 2002 to 2018 there were 62,058 SHC visits by MSM, of which 52,643 (85%) had complete behavioral data and were included in this analysis. This included 45,656 visits by MSM without HIV (representing 19,354 unique MSM) and 6,987 MSM with HIV (representing 3,097 unique MSM). Approximately half of men were less than 35 years old, two-thirds reported being White race, and over 50% reported more than five male sex partners in the prior year. ART use and having ever used PrEP increased steadily during the study period (Table 1); by 2018, 94% of men living with HIV reporting ART use and 50% of men without HIV reported ever using PrEP.
Table 1.
Characteristics of MSM Visits at the PHSKC SHC, 2002–2018, by HIV status (N=52,643)
| Characteristics | Total (N = 52,643) | MSM without HIV (N = 45,656) | MSM living with HIV (N = 6,987) |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Age (years) | |||
| <25 | 9,135 (17) | 8,742 (19) | 393 (6) |
| 25–34 | 19,698 (37) | 17,774 (39) | 1,924 (28) |
| 35–44 | 12,803 (24) | 10,454 (23) | 2,349 (34) |
| ≥45 | 11,006 (21) | 8,685 (19) | 2,321 (33) |
| Latinx Ethnicity | 6,563 (12) | 5,727 (13) | 836 (12) |
| Race | |||
| White | 34,457 (72) | 29,649 (71) | 4,808 (74) |
| Black / African American | 3,736 (8) | 3,037 (7) | 699 (11) |
| Asian | 3,204 (6.7) | 3,052 (7) | 152 (2) |
| Native Hawaiian or Pacific Islander | 559 (1) | 486 (1) | 73 (1) |
| Native American or Alaska Native | 582 (1) | 468 (1) | 114 (2) |
| Multi-race or Other race | 1,418 (3) | 1,222 (3) | 196 (3) |
| Unknown race | 4,230 (9) | 3,751 (9) | 479 (7) |
| Ever used meth | 8,919 (17) | 6,324 (14) | 2,595 (37) |
| Number of sex partners, past 12 months | |||
| 1 | 4,620 (10) | 4,146 (10) | 474 (8) |
| 2–5 | 17,352 (37) | 15,284 (38) | 2,068 (34) |
| 6–10 | 11,244 (24) | 9,913 (25) | 1,331 (22) |
| >10 | 13,124 (28) | 10,931 (27) | 2,193 (36) |
| Year of visit | |||
| 2002–2008 | 13,633 (26) | 11,817 (26) | 1,816 (26) |
| 2009–2013 | 20,115 (38) | 17,358 (38) | 2,757 (39) |
| 2014–2018 | 18,895 (36) | 16,480 (36) | 2,415 (35) |
| On ART* | |||
| 2002–2008 | - | - | 701 (53) |
| 2009–2013 | - | - | 1,618 (76) |
| 2014–2018 | - | - | 1,943 (92) |
| Ever Used PrEP* | |||
| 2002–2008 | - | 0 (0) | - |
| 2009–2013 | - | 57 (2) | - |
| 2014–2018 | - | 5,782 (35) | - |
ART, antiretroviral therapy; MSM, men who have sex with men; PHSKC, Public Health – Seattle & King County; PrEP, pre-exposure prophylaxis; SHC, Sexual Health Clinic
Percent represents the percent of individuals on ART or PrEP out of those who attended the clinic during that time period. Denominator excludes those who had data missing for that variable
Trends in Sexual Behavior
There were 38,061 visits included in this analysis (these represent the first visit in a calendar year). The proportion of MSM reporting serodiscordant CAS declined steadily from 2002 to 2013 but increased thereafter; 68% of MSM living with HIV and 40% of MSM without HIV reporting CAS with a serodiscordant/unknown-status partner in 2018 (Figure 1). Serosorting increased among all MSM from 2002–2010 but trends diverged thereafter. Among MSM living with HIV, the proportion reporting serosorting declined substantially from 40% in 2011 to 22% in 2018. Among MSM without HIV, serosorting continued to increase, from 27% in 2011 to 42% in 2018. The proportion of MSM reporting consistent condom use and no anal sex was relatively stable through 2012 and declined steadily thereafter. By 2018, 10% of MSM living with HIV and 18% of MSM without HIV reported consistent condom use or no anal sex. We also examined the proportion of MSM who reported never using condoms with any partners (a subset of those reporting CAS or serosorting; data not displayed in Figure 1). Among MSM without HIV, the proportion who reported never using condoms increased from 5.7% to 10.7% in 2002 to 2018. For MSM living with HIV, the proportion increased from 6.9% to 21.1%.
Figure 1.
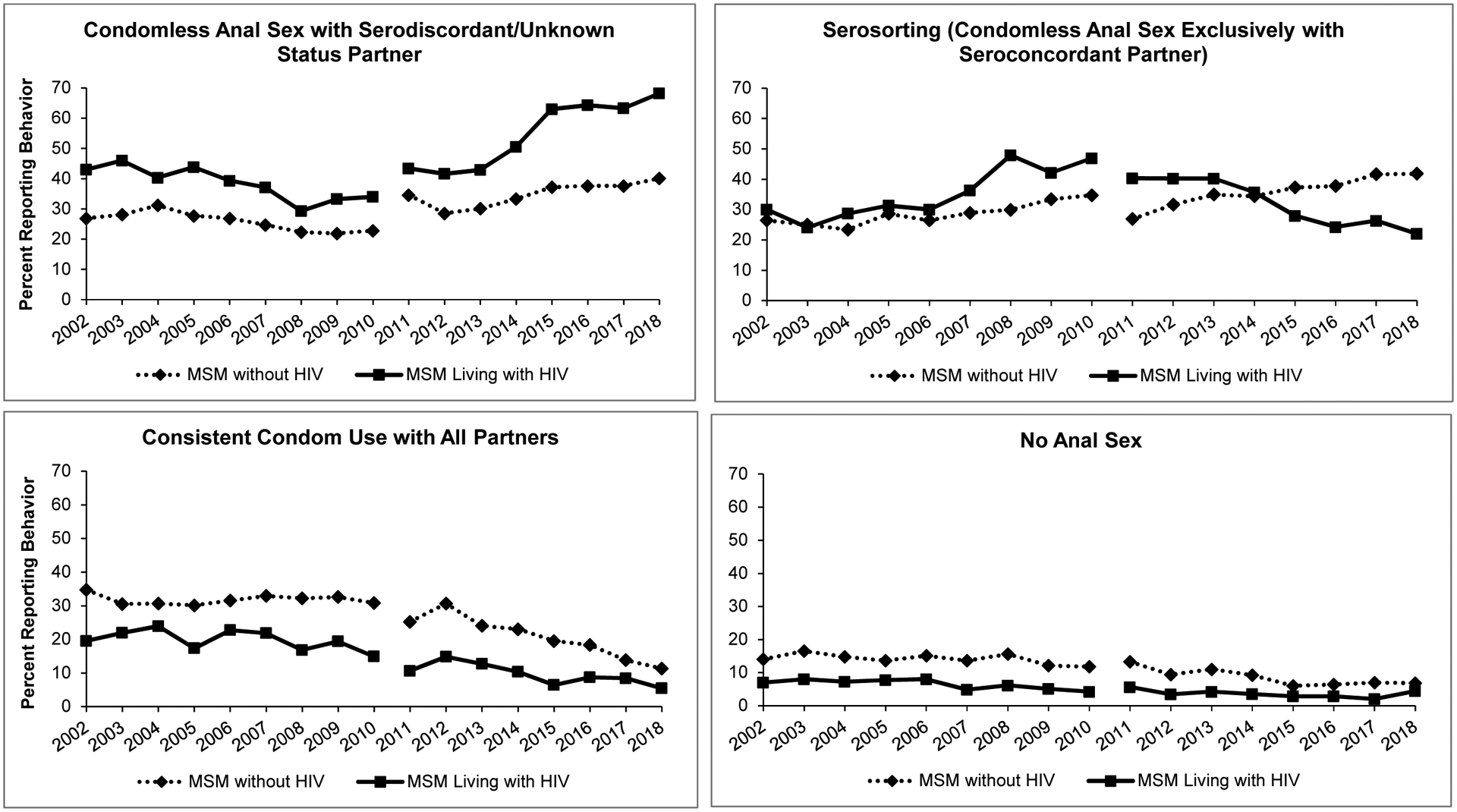
Secular trends in sexual behavior reported at the first visit in a calendar year by MSM without HIV (N=33,007) and MSM living with HIV (N=5,054) attending the PHSKC SHC Clinic, 2002–2018
During the study period, the percentage of visits where MSM without HIV reported ever using PrEP increased from 1.7% in 2013 to 50.1% in 2018. Those who reported ever using PrEP (n=5,839 visits) were more likely than non-PrEP users (n=13,769 visits) to report CAS with a serodiscordant partner (49.2% vs. 31.8%), similarly likely to report serosorting (41.8% vs. 39.1%), and less likely to report always using condoms (8.0% vs. 20.7%) or report not having anal sex (1.0% vs. 8.4%). We also compared trends (2014 to 2018) in ever using PrEP by behavioral category. We noted that PrEP use increased to a much greater degree among MSM reporting CAS with a serodiscordant partner (8% to 54%) and MSM reporting serosorting (2% to 43%) compared to MSM reporting consistent condom use (5% to 19%) and MSM reporting no anal sex (3% to 9%).
Trends in HIV/STI Test Positivity
Among MSM without HIV, the HIV test positivity declined dramatically during the study period (from 3.4% to 0.5% overall) regardless of reported sexual behavior (Figure 2). Conversely, early syphilis test positivity and urethral and rectal GC/CT test positivity steadily increased. However, rectal GC/CT test positivity trends appear to have diverged for MSM without HIV in about 2012, with a decline in test positivity among those reporting serosorting but continued increases among MSM reporting serodiscordant CAS and those reporting no CAS. Among MSM living with HIV (Figure 3), early syphilis and rectal GC/CT test positivity increased, while urethral GC/CT test positivity was somewhat stable. The trends in test positivity were relatively consistent across the three categories of sexual behavior among MSM living with HIV.
Figure 2.
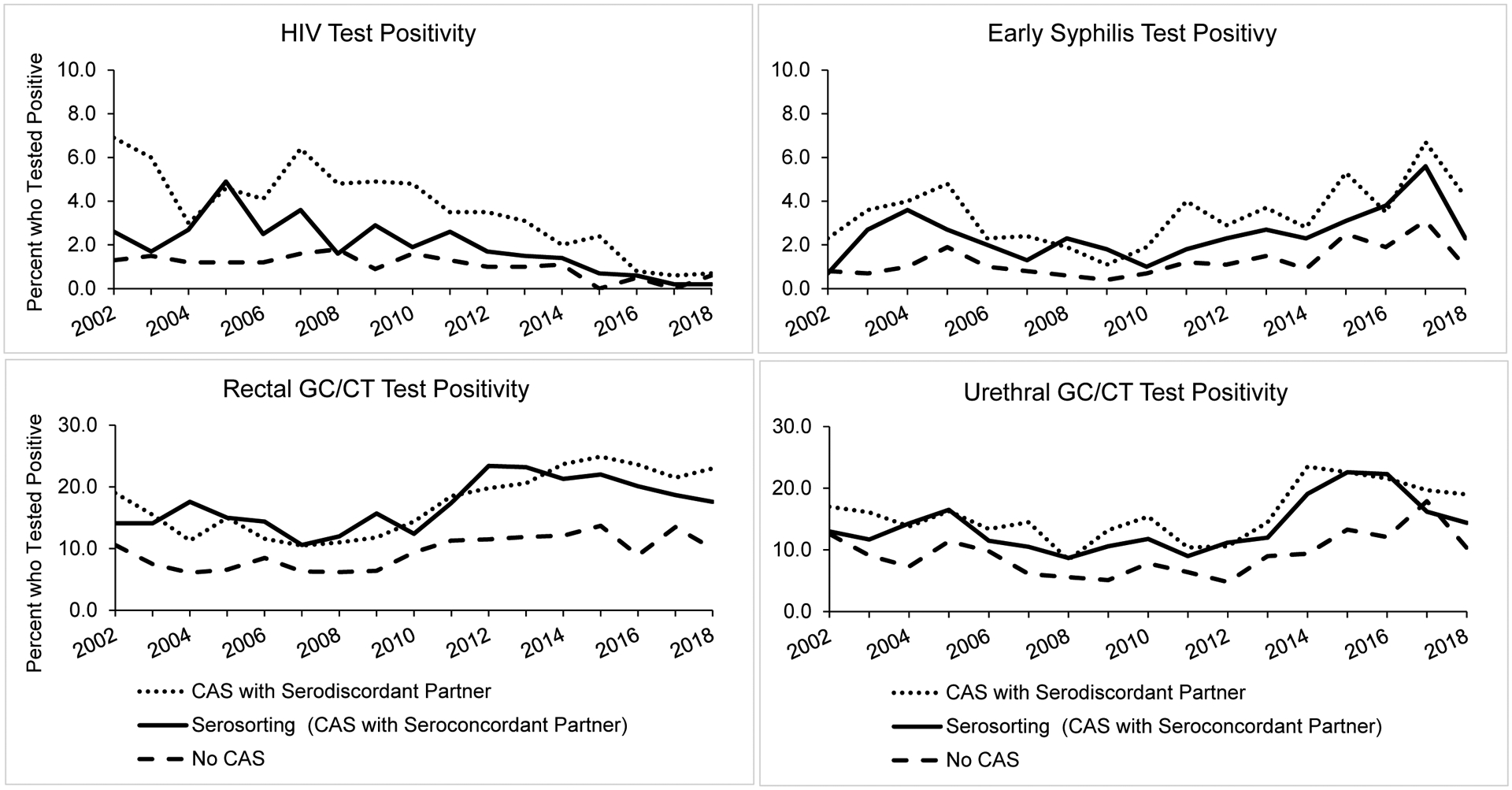
Secular trends in HIV/STI test positivity among MSM without HIV attending the PHSKC SHC, 2002–2018, by reported sexual behavior (N=45,656)
Figure 3.
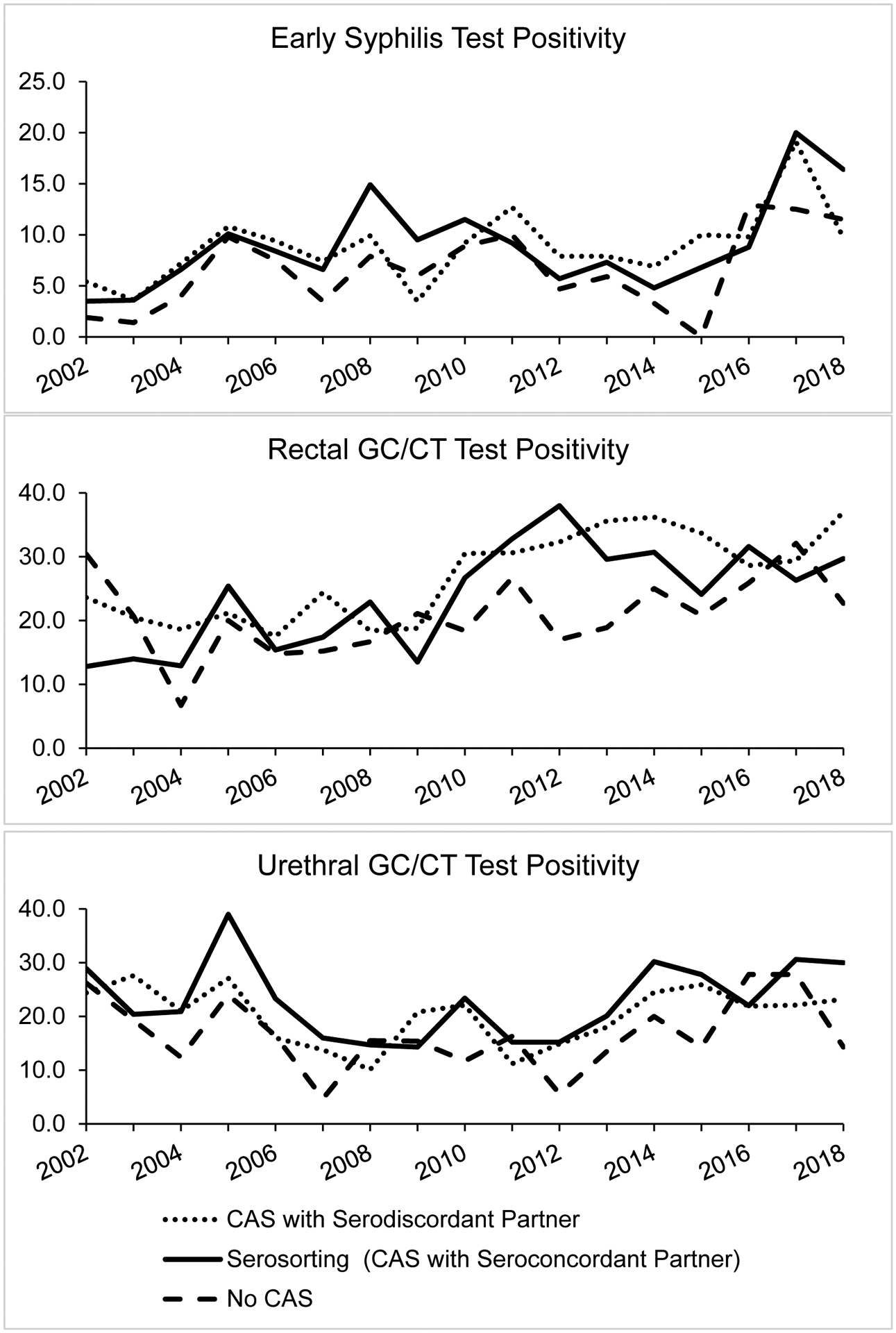
Secular trends in STI test positivity among MSM living with HIV attending the PHSKC SHC, 2002–2018, by reported sexual behavior (N=6,987)
Association between Behavior and HIV/STI Test Positivity
MSM without HIV who reported serosorting had a lower risk of HIV and STI compared to MSM who reported serodiscordant CAS, but a higher risk of HIV and STI compared to MSM who reported no CAS (Table 2). Among MSM living with HIV, there were no significant differences in the risk of STI for individuals reporting serosorting compared to MSM who reported serodiscordant CAS. However, MSM who reported serosorting had a significantly higher risk of urethral GC/CT and rectal GC/CT compared to those reporting no CAS. There was no statistical evidence that the association between serosorting and HIV/STI risk changed during the study period (Table 2). Correspondingly, the magnitude of the association between serosorting and HIV/STI risk compared to other behaviors was relatively consistent across the three specified time periods of 2002–2007, 2008–2013, and 2014–2018 (Supplementary Table 1). However, the relative risk of HIV among those who reported serosorting relative to those reporting no CAS declined over time, from a 2.1-fold higher risk in 2002–2007 to a 1.3-fold higher risk in 2014–2018.
Table 2.
Association between Serosorting and Testing Positive for HIV and Bacterial STIs and Test for Interaction by Year Among MSM attending the PHSKC SHC Clinic, 2002–2018, by HIV Status (N=52,643)*
| Serosorting vs. CAS with serodiscordant partner | Serosorting vs. No CAS | ||
|---|---|---|---|
| aRR (95% CI) | aRR (95% CI) | P-Value** (Test for interaction by calendar year) | |
| MSM without HIV | |||
| HIV | 0.63 (0.53 – 0.75) | 1.71 (1.37 – 2.14) | 0.56 |
| Early Syphilis | 0.78 (0.68 – 0.89) | 1.97 (1.63 – 2.37) | 0.58 |
| Urethral GC/CT | 0.86 (0.80 – 0.93) | 1.52 (1.40 – 1.67) | 0.34 |
| Rectal GC/CT | 0.90 (0.85 – 0.96) | 1.80 (1.66 – 1.96) | 0.12 |
| MSM living with HIV | |||
| Early Syphilis | 0.99 (0.83 – 1.18) | 1.30 (0.98 – 1.71) | 0.71 |
| Urethral GC/CT | 1.15 (1.00 – 1.32) | 1.33 (1.09 – 1.61) | 0.97 |
| Rectal GC/CT | 0.89 (0.80 – 1.00) | 1.23 (1.02 – 1.47) | 0.53 |
aRR, adjusted relative risk; CAS, condomless anal sex; CI, confidence interval; CT, chlamydia; MSM, men who have sex with men; PHSKC, Public Health – Seattle & King County; SHC, Sexual Health Clinic
Models adjusted for age, Latinx ethnicity, race, number of sex partners in the past 12 months, year and methamphetamine use
P-value is from Wald Chi-square; non-significant p-value (>0.05) indicates no statistical evidence that the aRR changed significantly during the study period; P-value is same regardless of referent group
DISCUSSION
In this study of MSM sexual behaviors over a 17-year period, the proportion of MSM reporting CAS with a serodiscordant or unknown-status partner has increased since 2013, following almost a decade of a decline in this behavior. Similarly, the proportion reporting consistent condom use or no anal sex has declined steadily over the last several years. Concurrent with these changes in behavior, we noted increases in the proportion of MSM reporting ART and PrEP use and dramatic declines in HIV test positivity regardless of reported behavior. Conversely, bacterial STI test positivity in our SHC has increased steadily. The risk of HIV/STI differed significantly by reported behavior, but there were no significant changes in the relative risk of HIV/STI over time by reported behavior. These findings highlight the success of biomedical HIV prevention strategies in preventing HIV despite population-level changes in sexual behavior that would probably have increased HIV transmission in an earlier era. Our findings are also consistent with the view that changes in sexual behavior that likely resulted from the availability of biomedical HIV prevention strategies have contributed to increases in STI.
The pattern of sexual behavior among MSM in our SHC since 2013 represent a stark contrast to our previously observed trends. At the time of our prior report7, which focused on the period of 2002 to 2013, we had observed large declines in serodiscordant CAS, increases in serosorting, and relative stability in the proportion of MSM reporting consistent condom use or no anal sex. But from 2014–2018 we observed a reversal in most of those trends. Most notably, our findings demonstrate a doubling in the percent of MSM who reported serodiscordant CAS since 2013 and a halving in the percent of MSM who reported consistent condom use. Further, we noted a nearly 50% relative reduction in serosorting among MSM living with HIV. Although these behaviors carry the potential for HIV transmission, the increased frequency of these behaviors during this time period occurred concurrently with substantial declines in HIV test positivity. This finding is consistent with the fact that over 90% of MSM living with HIV in the SHC report ART use, that over 80% of people living with HIV in King County are virally suppressed13, and that PrEP use has increased dramatically among our MSM clinic population since 2014 – when we started offering PrEP in our clinic – and in King County overall.13 These trends are also consistent with modeling data suggesting that decreases in serosorting among MSM living with HIV increases the influence of ART use on population-level HIV incidence.14 Thus, our findings – which are remarkably consistent with trends reported from MSM in San Francisco15 – demonstrate the success of biomedical prevention strategies in reducing population HIV incidence.
At the same time, the patterns of behavior change that we observed may also provide some insight into recent increases in syphilis, GC, and CT rates in King County and in the U.S. Nationally, the incidence of primary and secondary syphilis among men has increased steadily since 2000, and sharply since 2012.11 Historically, most primary and secondary syphilis cases among MSM have occurred in MSM living with HIV. However, over the last decade, increases in syphilis have affected MSM regardless of HIV status, leading to a rising proportion of cases occurring in MSM without HIV. This shift has been particularly pronounced since 2014, corresponding to the shift in behaviors that we observed among our clinic population, which also align with increased promotion of treatment as prevention, and later, undetectable=untransmittable, and more widespread PrEP uptake locally. Indeed, the decline in behaviors associated with a lower risk of STI (i.e., consistent condom use and no anal sex) and increase in behaviors associated with a higher risk of STI (i.e., serodiscordant CAS) is consistent with changing syphilis epidemiology and increases in GC/CT incidence.
Consistent with prior studies2, we found that serosorting among MSM without HIV was associated with an increased risk of HIV/STI relative to consistent condom use or no anal sex, but a decreased risk relative to serodiscordant CAS. However, we were surprised that the relative risk of HIV/STI by behavior did not change significantly over time. Given the increases in ART and PrEP use during the study period, we hypothesized that, over time, the risk of HIV for MSM who reporting serosorting would become more similar to the risk of HIV for MSM who reported CAS with serodiscordant partners (i.e., that the relative risks would move closer to the null value of 1.0 in 2014–2018 compared to prior years). Although we did not observe that in our data, we did note that the relative risk of HIV for MSM reporting serosorting compared to those reporting no CAS declined over time, from a 2.1-fold higher risk in 2002–2007 to a 1.3-fold higher risk in 2014–2018. We postulate that as PrEP use continues to increase, we will continue to observe a convergence in the risk of HIV by reported behavior.
We found that MSM who reported ever using PrEP were significantly more likely to report behaviors traditionally associated with HIV acquisition (e.g., CAS with serodiscordant partners) compared to MSM who had not taken PrEP. However, we are cautious to draw conclusions about the influence of PrEP on sexual behaviors from these data, since we are unable to discern if MSM engaged in these behaviors before, during, or after PrEP use. Importantly however, our findings call into question the utility of measuring CAS as a risk factor for HIV exclusive of other partner factors such as ART or PrEP use.16 Although we did not ask MSM patients about their partners’ ART or PrEP use, nor did we ask if their own ART or PrEP use motivated their behavior, it is likely that at least some of the behavioral changes we observed were a result of ART or PrEP use. For example, the increases in serodiscordant CAS may be due to MSM engaging in CAS with partners who are taking ART and/or virally suppressed, or due to increasing uptake of PrEP use. Indeed, the combination of behavioral and biomedical prevention strategies – titled “biomed matching” or “biomed sorting” – have been increasingly recognized.3–5,17,18 Ascertaining detailed partner-level data is challenging, particularly in clinical settings, because of the complexity of data collection and the length of time required for patients to complete behavioral assessments. Although traditionally our SHC has not collected this type of information, we have recently included a question19 in our routine behavioral data collection instrument to more accurately monitor the prevalence of these HIV prevention strategies.
This study has several strengths. Our SHC has systematically collected sexual behavior data for nearly two decades, which allows us to describe changes in behavior using a large study population. Our data should also be interpreted in light of a number of important limitations. First, these data were collected as part of routine clinical care, and we did not ask about partner ART or PrEP use. Thus, the data we report here do not present a complete picture of behavioral strategies used by MSM to prevent HIV. Second, we were not able to carry out a robust analysis of differences in behavior or HIV/STI risk by PrEP use because our clinical intake form only asked patients about ever PrEP use, not current PrEP use. PrEP use was also missing for approximately 25% of MSM. We categorized these men as non-PrEP users but it is possible that some of them had previously used PrEP. Third, HIV/STI test positivity in part reflects who was tested and testing modality. We transitioned to NAAT in 2011 and reduced urethral screening in 2013 which may have affected test positivity. Fourth, we were missing behavioral data on 15% of MSM, but it unclear why these data were missing. Fifth, we do not know if the changes in behavior we observed reflect changes among a consistent population over time, or a change in the population attending the SHC. However, given that 22,451 unique men contributed 52,643 visits to this analysis, there is at least some consistency in the population throughout the study period. Finally, these data are specific to MSM patients at a single SHC in Seattle. Although our findings are in line with what has been observed in San Francisco, it is important to note that both San Francisco and Seattle/King County have relatively high rates of viral suppression and PrEP uptake. These findings may not be generalizable to populations where biomedical prevention uptake is low.
In conclusion, we have observed a substantial change in the Seattle/King County MSM population’s sexual behaviors since 2013, including increases in CAS with serodiscordant partners, decreases in consistent condom use, and decreases in serosorting among MSM living with HIV. Given the increasing uptake of ART and PrEP use during this time, our findings suggest that these shifts in behavior may have been the result of an increase in these biomedical HIV prevention tools. However, the dramatic declines in HIV test positivity that we observed during this time underscores the success of these tools to substantially reduce HIV incidence at the population level, even in the face of large shifts in behavior that would likely have fueled HIV transmission in an earlier era. At the same time, it is important to recognize that these changes in behavior have also likely contributed to increases in STI incidence, particularly syphilis. Although promotion of condom use continues to be an important STI prevention strategy and we fully support the promotion of candid discussion between medical providers and MSM patients about behavioral strategies to mitigate both HIV and STI risk, we also recognize that biomedical STI prevention strategies – such as antibiotic pre- or post-exposure prophylaxis and STI vaccines – may be the key to reversing rising STI rates.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank the Public Health – Seattle & King County SHC staff, clinicians, and disease investigation specialists and the patients in the SHC whose data we present here.
Source of Funding:
This work was supported by Public Health – Seattle & King County and the University of Washington Center for AIDS Research, a National Institutes of Health-funded program [grant P30 AI027757] which is supported by the following NIH Institutes and Centers: National Institute of Allergy and Infectious Diseases, National Cancer Institute, National Institutes of Mental Health, National Institute on Drug Abuse, National Institute of Child Health and Human Development, National Heart, Lung, and Blood Institute, National Institute on Aging.
Footnotes
Conflicts of interest: CMK, LAB, and MRG have received donations of test kits and reagents from Hologic, Inc. unrelated to this study. LAB has received research support for studies unrelated to this work from SpeeDx and Nabriva. MRG has received research support from Hologic, Inc. JCD has conducted studies unrelated to this work funded by grants to the University of Washington from Hologic, Inc. All other authors report no conflicts of interest.
Previous Presentations: These data were presented in part at the 2020 CDC National STD Prevention Conference, Virtual Meeting, September 14–24, 2020
REFERENCES
- 1.Hess KL, Crepaz N, Rose C, Purcell D, Paz-Bailey G. Trends in Sexual Behavior Among Men Who have Sex with Men (MSM) in High-Income Countries, 1990–2013: A Systematic Review. AIDS and behavior. 2017;21(10):2811–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Purcell DW, Higa D, Mizuno Y, Lyles C. Quantifying the Harms and Benefits from Serosorting Among HIV-Negative Gay and Bisexual Men: A Systematic Review and Meta-analysis. AIDS and behavior. 2017;21(10):2835–2843. [DOI] [PubMed] [Google Scholar]
- 3.Newcomb ME, Mongrella MC, Weis B, McMillen SJ, Mustanski B. Partner Disclosure of PrEP Use and Undetectable Viral Load on Geosocial Networking Apps: Frequency of Disclosure and Decisions About Condomless Sex. Journal of acquired immune deficiency syndromes. 2016;71(2):200–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holt M, Lea T, Mao L, Zablotska I, Prestage G, de Wit J. Brief Report: HIV Prevention by Australian Gay and Bisexual Men With Casual Partners: The Emergence of Undetectable Viral Load as One of a Range of Risk Reduction Strategies. Journal of acquired immune deficiency syndromes. 2015;70(5):545–548. [DOI] [PubMed] [Google Scholar]
- 5.Roth EA, Cui Z, Rich A, et al. Seroadaptive Strategies of Vancouver Gay and Bisexual Men in a Treatment as Prevention Environment. J Homosex. 2018;65(4):524–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khosropour CM, Dombrowski JC, Hughes JP, Manhart LE, Simoni JM, Golden MR. Operationalizing the Measurement of Seroadaptive Behaviors: A Comparison of Reported Sexual Behaviors and Purposely-Adopted Behaviors Among Men who have Sex with Men (MSM) in Seattle. AIDS and behavior. 2017;21(10):2935–2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khosropour CM, Dombrowski JC, Swanson F, et al. Trends in Serosorting and the Association With HIV/STI Risk Over Time Among Men Who Have Sex With Men. Journal of acquired immune deficiency syndromes. 2016;72(2):189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin F, Prestage GP, Templeton DJ, et al. The impact of HIV seroadaptive behaviors on sexually transmissible infections in HIV-negative homosexual men in Sydney, Australia. Sexually transmitted diseases. 2012;39(3):191–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Truong HM, Kellogg T, Klausner JD, et al. Increases in sexually transmitted infections and sexual risk behaviour without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: a suggestion of HIV serosorting? Sex Transm Infect. 2006;82(6):461–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh S, Song R, Johnson AS, McCray E, Hall HI. HIV Incidence, Prevalence, and Undiagnosed Infections in U.S. Men Who Have Sex With Men. Annals of internal medicine. 2018;168(10):685–694. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2018. Atlanta, Georgia: US Department of Health and Human Services;2019. [Google Scholar]
- 12.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.HIV/AIDS Epidemiology Unit PH-SKC, Infectious Disease Assessment Unit WSDoH. 2019 HIV/AIDS Epidemiology Report & Community Profile, 2019, Volume 88. 2019. [Google Scholar]
- 14.Delva W, Helleringer S. Beyond Risk Compensation: Clusters of Antiretroviral Treatment (ART) Users in Sexual Networks Can Modify the Impact of ART on HIV Incidence. PloS one. 2016;11(9):e0163159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen YH, Guigayoma J, McFarland W, Snowden JM, Raymond HF. Increases in Pre-exposure Prophylaxis Use and Decreases in Condom Use: Behavioral Patterns Among HIV-Negative San Francisco Men Who have Sex with Men, 2004–2017. AIDS and behavior. 2019;23(7):1841–1845. [DOI] [PubMed] [Google Scholar]
- 16.Jin F, Prestage GP, Mao L, et al. “Any Condomless Anal Intercourse” is No Longer an Accurate Measure of HIV Sexual risk Behavior in Gay and Other Men Who have Sex with Men. Frontiers in immunology. 2015;6:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grov C, Jonathan Rendina H, Patel VV, Kelvin E, Anastos K, Parsons JT. Prevalence of and Factors Associated with the Use of HIV Serosorting and Other Biomedical Prevention Strategies Among Men Who Have Sex with Men in a US Nationwide Survey. AIDS and behavior. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes AJ, Chen YH, Scheer S. Condomless Anal Sex Among HIV-Positive Men Who Have Sex with Men: Biomedical Context Matters. AIDS and behavior. 2017;21(10):2886–2894. [DOI] [PubMed] [Google Scholar]
- 19.Khosropour CM, Dombrowski JC, Katz DA, Golden MR. A Single Question to Examine the Prevalence and Protective Effect of Seroadaptive Strategies Among Men Who Have Sex With Men. Sexually transmitted diseases. 2017;44(11):643–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


