Abstract
Background
In recent years, the incidence of male infertility has increased worldwide. It is necessary to study the factors that influence male infertility in each area/region for better management.
Objective
To determine the factors affecting male infertility in the Iranian male population.
Materials and Methods
An online search was conducted in electronic databases including PubMed, Google Scholar, SID, and Scopus to identify articles on the factors associated with male infertility, published in English and Persian. The keywords used to perform the search included “factor", “epidemiology", “causes of infertility", and “male infertility". The search was conducted without a time restriction, up to April 2020.
Results
The search resulted in a total number of 691 studies. After an assessment of the articles, finally 14 studies were included in this study with a total number of 26,324 infertile males. The factors associated with male infertility included semen abnormalities, varicocele and testis disorder, smoking, exposure to heat, obesity, anabolic steroids, vascular abnormalities, anti-spermatogenesis factors, antidepressants, taking ranitidine and cimetidine, penile discharge and genital ulcers, painful micturition, occupational factors, alcohol, chronic disease, sexual disorder, Surgical and urological diseases, genetic factors and herpes infection. Among these, the semen and varicocele disorders were common in most studies.
Conclusion
The present review suggests that the factors affecting male infertility in Iran are similar to those reported from other countries. The results of this study can be used in adopting appropriate strategies for infertility management in Iran.
Keywords: Male, Infertility, Sterility, Urogenital diseases.
1. Introduction
Infertility and its treatment are important global concerns that have different social dimensions (1-4). Infertility is the inability of a couple to get pregnant within one year of regular unprotected intercourse. The prevalence of primary infertility among couples is 13.2-17.3% (5, 6). The main causes of primary infertility are the ovulatory problem (39.7%) and male factors (29.1%) (6). At least half of all infertility cases are related to male infertility (7). Jafari estimated the prevalence of male factors as 40.9% (8). In another study, the distribution of infertility due to male factors was reported to range from 20-70% and the percentage of infertile men from 2.5 to 12% (9). Evidence indicates that male infertility has increased in some populations (10). Worldwide studies have shown that the increasing infertility in recent years could be due to anatomical, physiological, and genetic factors. Many environmental conditions and acquired factors, such as smoking and alcohol consumption, changes in sexual behavior, and diet, also influence fertility and semen quality, and therefor can lead to the diversity in etiology and patterns of infertility in different regions (6, 11-13). Male infertility is a global health concern and its management is important because it not only affects the infertile couple but also the phenomenon of childbearing as a whole. Understanding the factors related to male infertility in each region separately can help healthcare providers and policymakers to plan appropriate strategies for its management. Without accurate and precise data from the region, planning to comprehensively identify and treat infertile men is not possible (14). Therefore, this systematic review aimed to determine the factors affecting male infertility in Iran.
2. Materials and Methods
In this systematic review, articles were identified in the following databases: PubMed, Google Scholar, Scopus, SID, and Magiran. The search was performed using the following keywords: “factor,” “epidemiology,” “causes of infertility,” “male infertility,” “fertility,” and “infertility” in English and Persian. The search was conducted without a time restriction, up to April 2020.
All relevant studies and references were searched to detect additional articles, and the quality of the articles was evaluated using the Joanna Briggs Institute Critical Appraisal tools (15). All collected articles were reviewed and some were excluded based on the title, abstract, or duplication. Then, selected studies were assessed based on the inclusion and exclusion criteria of the study.
The Inclusion criteria were research on infertile male participants, conducted in Iran, and reporting human studies. The exclusion criteria were infertile women with fertile/normal male participants, duplicate paper, review studies, animal studies, infertile couples with unspecified gender, and abstracts presented in congresses.
Data were extracted independently by two reviewers. Disagreement between the researchers were resolved through discussion. The following information was extracted from each study: the authors' names, date of publication, study design, reported results, and total number of infertile men.
3. Results
A total of 691 articles were found through the database search. After an assessment of the titles and abstracts, 674 duplicates and irrelevant studies were excluded and 17 articles were assessed for eligibility. At this stage, 3 articles were excluded from the study process, too, one article due to inaccessibility of the full-text and two articles due to the inclusion of infertile couples without separating male and female categories. Finally, 14 studies were included in this study including retrospective, cohort, and cross-sectional studies (Table I, Figure 1). The quality assessment of the articles was done using the Joanna Briggs Institute Critical Appraisal checklist.
A total of 26,324 infertile men were studied in these articles, which were published between 2007 and 2018.
While the study of Ahmadi with 96 participants had the lowest sample size, the study of Safari Nejad with 12,284 infertile men had the largest (16, 17). The factors related to male infertility included semen abnormalities (12, 18-24); genetic factors (12); vascular abnormalities (12); anti-spermatogenesis factors (12, 22, 25); cryptorchidism; varicocele, and testis disorder (16-23, 25-27); smoking and lead exposure (17, 22, 23, 25, 27); exposure to heat (17); obesity (17, 22, 23); anabolic steroids (17, 22); antidepressants; penile discharge, painful micturition, and genital ulcers (17); occupational factors (17, 21); alcohol consumption (25); chorionic disease (16, 20); sexuality disorder (17, 19); surgery record (16, 20, 25); ranitidine (23); cimetidine (25); urinary tract infection (27); and herpes infection (28). Among of the mentioned factors, semen and varicocele disorders were common in most studies. The studies have been summarized in Table I.
Table 1.
General features of the studies
|
| ||||
| Authors, year (Ref number) | Center | Sample size | Object | Result |
| Karimpour, 2006 (26) | Infertility centers in Mazandaran | 2,235 | Determine the incidence of varicocele in men with infertility | Varicocele (42.6)- Congenital bilateral absence of the vas deferens (1.8)- Testicular torsion (0.1)- Cryptorchidism (14) |
| Kamali, 2007 (18) | Royan Institute in Tehran | 2,492 | Survey the epidemiology of infertility in Royan Institute | Semen abnormalities (63.9)- Azoospermia (23.6)- Varicocele (21) |
| Safarinejad, 2008 (17) | A population-based study in Iran | 12,285 | Prevalence and risk factors of infertility in Iran | Varicocele (16)- Cryptorchidism (1.5)-Current smoker (42)- Ex-smoker (16)- BMI-Male exposure to heat (28)- Anabolic steroids (3.5)- Antidepressants (22)- penile discharge, painful-micturition, and genital ulcers (8.8) |
| Karimpour Malekshah, 2011 (19) | Infertility Clinics in Mazandaran | 3,734 | Determine the clinical patterns and major causes of infertility in Mazandaran | Semen factor (50.5)- Varicoceles (42.7)- Deferens agenesis (1.2)- Cryptorchidism (0.5)- Testicular torsion (0.1)- Miscellaneous male factors (hypospadias, retrograde ejaculation, coital problem) (3.1) |
| Taghavi, 2011 (20) | Urology Clinic of Imam Reza Hospital of Mashhad | 2,000 | Determine the clinical major causes of infertility in Mashhad | Varicocele (37.4)- Testis atrophy (6.15)- Ectopic testis (1.25)- Spermatocele (0.95)- Gynecoplasty (0.3)- Hydrocele (0.65)- Inguinal hernia (0.35)- Sperm abnormality (55.2)- Azoospermia (21.7)- Chronic disease (3.65) |
| Choobineh, 2013 (15) | Shariati Hospital Infertility Clinic, Tehran | 200 | Examine the demographic characteristics of infertile men | Dealt with chemicals in worker (26)- Varicocele decreased sperm motility (81)- Decrease in sperm count (42)- Azoospermia (46) |
| Keshavarzi, 2013 (22) | Infertility Center of Mo'tazedi Hospital in Kermanshah | 514 | Determine the associated risk factors of infertility | Varicocele (1.15)- Azoospermia (3.89) BMI-smoking (55.3) - Anabolic steroids (3.5) |
| Monavari, 2013 (28) | Clinical Center for Infertility in Yazd | 70 | Determine the prevalence of HSV-1 and HSV-2 using real-time PCR in the semen of a randomized asymptomatic infertile male | HSV infection in semen HSV-1 (22.9) HSV-2 (14.3) |
| Ahmadi, 2014 (16) | Infertility clinics of Ilam province | 96 | Determine associated factors with male infertility by using semen analysis | Surgical and urological diseases (45.8) |
| Mahboubi, 2014 (23) | Infertility clinic in Shiraz | 268 | Determine the most common risk factors for male infertility in Iranian men | Varicocele (36)- Azoospermia (30.6)- Smoking (32.4)- Taking ranitidine (14.8)- Cigarette smoking (32.4)– BMI*- Job (62)- Teratospermia (84)- Asthenospermia (82.7)- Oligospermia (52.7)- Hernia (36) |
| Sohrabvand 2015 (25) | Infertility clinics of Vali-e-Asr, Tehran | 430 | Clarify the associated factors that might play a role in Iranian infertile men | Cigarette smoking (29)- Varicocele operation (22)- Hernia operation (6.2)- Orchiopexy operation (4.2)- Undescended testis (6.2)- Opium addiction (9.2)- Alcohol consumption (5.5)- Cimetidine (0.9)- Lead exposure (0.6) |
| Masoumi, 2015 (13) | Infertility center in Fatemieh Hospital in Hamadan | 1,200 | Determine the frequency of the causes of infertility in infertile couples | Semen abnormalities (44.6)- Genetic factors (29.8)- Anti-spermatogenesis agents (11)- Vascular disorders (17.2) |
| Shafabakhsh, 2017 (27) | Clinical Center for Infertility in Yazd | 600 | Determine the influence of infertility, smoking, alcohol, and addictive drugs | Varicocele (20.7)- Smoking (34)- Urinary tract infection (6.3)- Hookah (5.7)- Opium (19)- Naswar (0.7) |
| Hashemzadeh, 2018 (24) | Infertility clinics of Vali-e-Asr, Tehran | 200 | Determine the relationship between body mass index and quality of sperm parameters | Oligospermia (34)- Asthenospermia (27.5)- Teratospermia (3) |
| Numbers are presented as percentages, *The difference between average BMI was statistically significant in both fertile and infertile groups p 0.05. BMI: Body mass index, HSV: Herpes simplex virus | ||||
Figure 1.
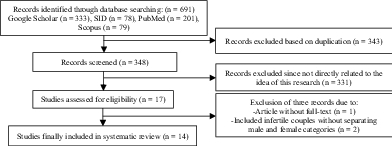
Outline of the article search process.
4. Discussion
This systematic review investigated the causes of male infertility. Semen parameters and varicocele were included in most studies (12, 16, 18-27). The prevalence of varicocele in men with infertility problems is twice that of the normal population. In Karimpur's study in 2011, varicocele was responsible for 42.7% of cases of infertility in males (19). The higher prevalence of varicocele in the infertile men population is the most important evidence supporting the theory of the relationship between varicocele and male infertility (29). Varicocele can lead to an increase in the temperature of the testes and cause reflux of toxic metabolites from the adrenal vein to the left kidney (30).
Li and Skakkebaek indicated that “according to many studies the semen quality in men is declining throughout the world and during the past decades a possible degradation in human semen quality has become an important public health issue" (31, 32). In a nine-year study, one in five investigated men (1737/8518) was diagnosed with reduced sperm counts (33). In 50% of infertile couples, semen disorders is the male infertility-associated influence (34). A study conducted in China reported that men's lifestyles there are related to their sperm quality (35). Durairajanayagam found that “a wide variety of risk factors could potentially influence sperm quality. These include lifestyle factors such as cigarette smoking, alcohol intake, use of illicit drugs, anabolic–androgenic steroids, obesity, psychological stress, diet, and caffeine intake" (36). In the present evaluation of studies, smoking and obesity were among the factors affecting infertility. Perhaps one of the reasons for this is their impact on the quality of sperm, which has been mentioned in several studies. Kazemijaliseh found that aging, higher body mass index (BMI), active smoking, and higher educational levels are associated with increased infertility (6). Obesity is associated with lower serum testosterone and luteinizing hormone, elevated rates of oligospermia or azoospermia, decreased semen volume, and sperm concentration. It seems that multiple factors are involved in the relationship between obesity and male infertility (37), including that obesity can affect male fertility through erectile dysfunction. Many studies have demonstrated the adverse effects of smoking, alcohol drinking, and weight on sperm; only a few observed no effect on any semen parameters (31, 38-40). For example, Hashemzadeh indicated that there was no significant relationship between the BMI in three groups of men (grouped based on BMI and their overall sperm analysis (counts, motility, and shape) (24). Dechanet reported that “obesity and cigarette smoking were factors associated with decreased fertility by causing a delay in conception and decreased in vitro fertilisation results" (41).
According to the studies, tobacco smoking has many negative effects on semen parameters (i.e impaired motility of spermatozoa, lower semen concentration, and increased morphology defects in tail, neck, and head) resulting in male infertility (10, 42-46).
The cigarette toxic contents might have adverse effects on the developmental processes of the male germ cells (10, 47, 48). Also, products in alcohol and cigarettes that cause oxidative stress could be have a role in the pathogenesis of birth defects, embryo development, moles, cancers, preeclampsia and preterm labor, thus might lead to abortion and infertility (49).
Other factors that can affect male infertility are environmental and occupational agents that may result in genetic disorders in gonadal cells (50, 51).
The association of toxic materials as an environmental factor with infertility has been considered (52). In our review, some studies indicated the influence of occupational and environmental factors on infertility (17, 21, 22). Sedentary jobs are frequently associated with testicular overheat and possible risk of sperm DNA harm (3, 53-55).
Other factors associated with male infertility in our study were herpes infection (28) and urinary tract infection (27). According to these studies, asymptomatic seminal infection with herpes simplex virus adversely affects the sperm count (28). Punab's study indicated that “the majority of azoospermia cases had epididymis obstruction, which has most probably been caused by sexually transmitted diseases in the past" (33). Infectious diseases such as inflammatory reactions within the male genital tract are responsible for a greater proportion of infertility (7, 56).
Based on the available scientific evidence, it is not possible to say with certainty whether these are true “potential contributing factors” or a result of impaired physiology and health. More high-quality research with well-designed studies is needed to reach a strong evidence base on the factors affecting male fertility and for developing treatment guidelines in this context (57-59). However, in most of the studies, semen and varicocele disorders were common problems that therefore warrant further consideration. Also, smoking and obesity are factors that can be reduced through behavioral change. It is necessary to assess lifestyle patterns of infertile men before and during infertility treatments and to implement healthy lifestyle counseling programs for them.
5. Conclusion
The present review suggests that the factors affecting male infertility in Iran are similar to those reported in other countries. The results of this study can be used in planning appropriate strategies for the management of infertility in Iran.
Conflict of Interest
None declared.
References
- Latifnejad Roudsari R, Jafari H, Taghipour A, Khadem N, Ebrahimzdeh S. The association of religious beliefs in infertile couples’ attitude towards donation procedures and its selection as a therapeutic approach to infertility. Iran J Obstet Gynecol Infertil. 2013;16:1–10. [Google Scholar]
- Latifnejad Roudsari R, Jafari H, Taghipour A. The relationship of sociocultural beliefs andinfertile couples’ attitude toward reproductivedonation: A descriptive-correlational study. Int J Reprod BioMed. 2018;17:315–324. doi: 10.18502/ijrm.v17i5.4599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill K, Jakubik J, Kups M, Rosiak-Gill A, Kurzawa R, Kurpisz M, et al. The impact of sedentary work on sperm nuclear DNA integrity. Folia Histochem Cytobiol. 2019;57:15–22. doi: 10.5603/FHC.a2019.0002. [DOI] [PubMed] [Google Scholar]
- Hadizadeh-Talasaz F, Simbar M, Latifnejad Roudsari R. Exploring infertile couples’ decisions to disclose donor conception to the future child. Int J Fertil Steril. 2020;14:240–246. doi: 10.22074/ijfs.2020.44408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Direkvand Moghaddam A, Delpisheh A, Sayehmiri K. An investigation of the worldwide prevalence of infertility as a systematic review. Qom Univ Med Sci J. 2016;10:76–87. [Google Scholar]
- Kazemijaliseh H, Tehrani FR, Behboudi-Gandevani S, Hosseinpanah F, Khalili D, Azizi F. The prevalence and causes of primary infertility in Iran: A population-based study. Glob J Health Sci. 2015;7:226–232. doi: 10.5539/gjhs.v7n6p226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuppe HC, Pilatz A, Hossain H, Diemer T, Wagenlehner F, Weidner W. Urogenital infection as a risk factor for male infertility. Deutsches Arzteblatt Int. 2017;114:339–346. doi: 10.3238/arztebl.2017.0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafari H, Latifnejad Roudsari R, Taghipour A, Khadem Ghaebi N, Ebrahim Zadeh S. Comparison of knowledge and attitude towards reproductive donation procedures between recipient and non-recipient infertile couples at Mashhad Infertility Center. J Torbat Heydariyeh Univ Med Sci. 2015;3:16–25. [Google Scholar]
- Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrin. 2015;13:1–9. doi: 10.1186/s12958-015-0032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundhun PK, Janoo G, Bhurtu A, Teeluck AR, Soogund MZS, Pursun M, et al. Tobacco smoking and semen quality in infertile males: A systematic review and meta-analysis. BMC Public Health. 2019;19:1–11. doi: 10.1186/s12889-018-6319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macaluso M, Wright-Schnapp TJ, Chandra A, Johnson R, Satterwhite CL, Pulver A, et al. A public health focus on infertility prevention, detection, and management. Fertil Steril. 2010;93:1–10. doi: 10.1016/j.fertnstert.2008.09.046. [DOI] [PubMed] [Google Scholar]
- Masoumi SZ, Parsa P, Darvish N, Mokhtari S, Yavangi M, Roshanaei G. An epidemiologic survey on the causes of infertility in patients referred to infertility center in Fatemieh Hospital in Hamadan. Iran J Reprod Med. 2015;13:513–516. [PMC free article] [PubMed] [Google Scholar]
- Ombelet W. Global access to infertility care in developing countries: A case of human rights, equity and social justice. Facts Views Vis Obgyn. 2011;3:257–266. [PMC free article] [PubMed] [Google Scholar]
- Taghipour A, Latifnejad Roudsari R. The association of socio-demographic characteristics of infertile men and women with their attitude towards donation procedures. Journal of Torbat Heydariyeh University of Medical Sciences. 2019;7:65–76. [Google Scholar]
- Critical appraisal tools 2018 https://jbi.global/critical-appraisal-tools
- Ahmadi MRH, Yasemi M, Peyman H, Hemati K, Khajavikhan J, Yaghoubi M, et al. Associated factors with male infertility: A case control study. J Clin Diagn Res. 2014;8:11–13. doi: 10.7860/JCDR/2014/8611.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safarinejad MR. Infertility among couples in a population-based study in Iran: Prevalence and associated risk factors. Int J Androl. 2008;31:303–314. doi: 10.1111/j.1365-2605.2007.00764.x. [DOI] [PubMed] [Google Scholar]
- Kamali M, Baghestani AR, Kashfi F, Kashani H, Tavajohi S, Amir Chaghmaghi E. A survey on infertility in Royan Institute. Iran J Fertil Steril. 2007;1:23–26. [Google Scholar]
- Karimpur Malekshah A, Moghaddam AE, Moslemizadeh N, Peivandi S, Barzegarnejad A, Musanejad N, et al. Infertility in Mazandaran province-north of Iran: An etiological study. Iran J Reprod Med. 2011;9:21–24. [PMC free article] [PubMed] [Google Scholar]
- Taghavi R, Tavakkoli Tabassi K, Mohammadi Sh, Kor K. Epidemiologic study 2000 infertile males in urology clinic of Imam Reza Hospital of Mashhad. J Zabol Univ Med Sci. 2011;3:11–16. [Google Scholar]
- Choobineh H, Sadighi Gilani M, Hassanzadeh G, Saeepour N, Habibi M, Falahi P, et al. Assessment of socio-demographic characteristics of infertile men who referred to Shariati Hospital, Tehran, Iran. Iran J Obstet Gynecol Infertil. 2013;16:6–12. [Google Scholar]
- Keshavarzi F, Borna MHO, Bakhtiari F. [The survey of infertility risk factors in admitted men to infertility center of Mo’tazedi hospital in Kermanshah, 2012-2013] J Clin Res Paramed Sci. 2016;5:78–85. [Google Scholar]
- Mahboubi M, Foroughi F, Ghahramani F, Shahandeh H, Moradi S, Shirzadian T. A case-control study of the factors affecting male infertility. Turkish J Med Sci. 2014;44:862–865. doi: 10.3906/sag-1304-35. [DOI] [PubMed] [Google Scholar]
- Hashemzadeh M, Tagizadeh Z, Behboodi Mogadam Z, Montazeri A, Rashidi B, Shams M, et al. Relationship between obesity and sperm parameters in men with idiopathic infertility. Iran J Obstet Gynecol Infertil. 2018;21:35–41. [Google Scholar]
- Sohrabvand F, Jafari M, Shariat M, Haghollahi F, Lotfi M. Frequency and epidemiologic aspects of male infertility. Acta Medica Iranica. 2015;53:231–235. [PubMed] [Google Scholar]
- Karimpur Malekshah A, Joursaraii GA, Mousanejad N, Mir MRA, Moghaddam AE. [The frequency of varicoceles in men with primary and secondary infertility referring to two infertility centers in Mazandaran during 2001-2005] Feyz. 2006;10:50–54. [Google Scholar]
- Shafabakhsh M, Sadeghian HA, Ehramposh MH, Aflatoonian A, Dehghani A, Ghaneian MT. [The relationship of smoking, alcohol, and drugs consumption on the quality of semen parameters in males referring to the infertility center of Yazd in 2016] Tolooebehdasht. 2019;17:44–54. [Google Scholar]
- Monavari SH, Vaziri MS, Khalili M, Shamsi-Shahrabadi M, Keyvani H, Mollaei H, et al. Asymptomatic seminal infection of herpes simplex virus: Impact on male infertility. J Biomed Res. 2013;27:56–61. doi: 10.7555/JBR.27.20110139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarow JP. Effects of varicocele on male fertility. Hum Reprod Update. 2001;7:59–64. doi: 10.1093/humupd/7.1.59. [DOI] [PubMed] [Google Scholar]
- Aubuchon M, Burney RO, Schust DJ, Yao MW. Infertility and assisted reproductive technology. Berek & Novak’s Gynecology Fifteenth ed: Lippincott Williams & Wilkins, a Wolters KLuwer business; 2012. [Google Scholar]
- Li Y, Lin H, Li Y, Cao J. Association between socio-psycho-behavioral factors and male semen quality: Systematic review and meta-analyses. Fertil Steril. 2011;95:116–123. doi: 10.1016/j.fertnstert.2010.06.031. [DOI] [PubMed] [Google Scholar]
- Skakkebaek NE, Rajpert-De Meyts E, Buck Louis GM, Toppari J, Andersson AM, Eisenberg ML, et al. Male reproductive disorders and fertility trends: Influences of environment and genetic susceptibility. Physiol Rev. 2015;96:55–97. doi: 10.1152/physrev.00017.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punab M, Poolamets O, Paju P, Vihljajev V, Pomm K, Ladva R, et al. Causes of male infertility: A 9-year prospective monocentre study on 1737 patients with reduced total sperm counts. Hum Reprod. 2016;32:18–31. doi: 10.1093/humrep/dew284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European association of urology guidelines on male infertility: The 2012 update. Eur Urol. 2012;62:324–332. doi: 10.1016/j.eururo.2012.04.048. [DOI] [PubMed] [Google Scholar]
- Junqing W, Ersheng G, Qiuying Y. The investigation on working and other lifestyles influencing semen quality of Chinese young men. Chinese J Fam Plan. 2004;12:346–349. [Google Scholar]
- Durairajanayagam D. Lifestyle causes of male infertility. Arab J Urol. 2018;16:10–20. doi: 10.1016/j.aju.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao DF, Mills JN. Male infertility: Lifestyle factors and holistic, complementary, and alternative therapies. Asian J Androl. 2016;18:410–418. doi: 10.4103/1008-682X.175779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotti F, Corona G, Vitale P, Maseroli E, Rossi M, Fino M, et al. Current smoking is associated with lower seminal vesicles and ejaculate volume, despite higher testosterone levels, in male subjects of infertile couples. Hum Reprod. 2015;30:590–602. doi: 10.1093/humrep/deu347. [DOI] [PubMed] [Google Scholar]
- Ricci E, Al Beitawi S, Cipriani S, Candiani M, Chiaffarino F, Viganò P, et al. Semen quality and alcohol intake: A systematic review and meta-analysis. Reprod Biomed. 2017;34:38–47. doi: 10.1016/j.rbmo.2016.09.012. [DOI] [PubMed] [Google Scholar]
- Tsao CW, Liu CY, Chou YC, Cha TL, Chen SC, Hsu CY. Exploration of the association between obesity and semen quality in a 7630 male population. PLoS One. 2015;10:1–13. doi: 10.1371/journal.pone.0119458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dechanet C, Belaisch-Allart J, Hedon B. [Prognosis criteria for the management of the infertile couple] J Gynecol Obstet Biol Reprod. 2010;39:9–26. doi: 10.1016/S0368-2315(10)70027-2. [DOI] [PubMed] [Google Scholar]
- Daumler D, Chan P, Lo KC, Takefman J, Zelkowitz P. Men’s knowledge of their own fertility: A population-based survey examining the awareness of factors that are associated with male infertility. Hum Reprod. 2016;31:2781–2790. doi: 10.1093/humrep/dew265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma R, Harlev A, Agarwal A, Esteves SC. Cigarette smoking and semen quality: A new meta-analysis examining the effect of the 2010 World Health Organization laboratory methods for the examination of human semen. Eur Urol. 2016;70:635–645. doi: 10.1016/j.eururo.2016.04.010. [DOI] [PubMed] [Google Scholar]
- Davar R, Sekhavat L, Naserzadeh N. Semen parameters of non-infertile smoker and non-smoker men. J Med Life. 2012;5:465–468. [PMC free article] [PubMed] [Google Scholar]
- Lingappa HA, Govindashetty AM, Puttaveerachary AK, Manchaiah S, Krishnamurthy A, Bashir S, et al. Evaluation of effect of cigarette smoking on vital seminal parameters which influence fertility. J Clin Diag Res. 2015;9:13–15. doi: 10.7860/JCDR/2015/13295.6227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elshal MF, El-Sayed IH, Elsaied MA, El-Masry SA, Kumosani TA. Sperm head defects and disturbances in spermatozoal chromatin and DNA integrities in idiopathic infertile subjects: Association with cigarette smoking. Clin Biochem. 2009;42:589–594. doi: 10.1016/j.clinbiochem.2008.11.012. [DOI] [PubMed] [Google Scholar]
- Zenzes MT. Smoking and reproduction: Gene damage to human gametes and embryos. Hum Reprod Update. 2000;6:122–131. doi: 10.1093/humupd/6.2.122. [DOI] [PubMed] [Google Scholar]
- Schagdarsurengin U, Western P, Steger K, Meinhardt A. Developmental origins of male subfertility: Role of infection, inflammation, and environmental factors. Seminars in Immunopath. 2016;38:765–781. doi: 10.1007/s00281-016-0576-y. [DOI] [PubMed] [Google Scholar]
- Zeinab H, Zohreh S, Gelehkolaee KS. Lifestyle and outcomes of assisted reproductive techniques: A narrative review. Glob J Health Sci. 2015;7:11–22. doi: 10.5539/gjhs.v7n5p11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joffe M. doi: 10.1093/humrep/dep390. What has happened to human fertility? Hum Reprod 2009; 25: 295–3. [DOI] [PubMed]
- Povey A, Stocks S. Epidemiology and trends in male subfertility. Hum Fertil. 2010;13:182–188. doi: 10.3109/14647273.2010.515700. [DOI] [PubMed] [Google Scholar]
- Ghanei M, Rajaee M, Khateri S, Alaeddini F, Haines D. Assessment of fertility among mustard-exposed residents of Sardasht, Iran: A historical cohort study. Reprod Toxicol. 2004;18:635–639. doi: 10.1016/j.reprotox.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Boggia B, Carbone U, Farinaro E, Zarrilli S, Lombardi G, Colao A, et al. Effects of working posture and exposure to traffic pollutants on sperm quality. J Endocrin Invest. 2009;32:430–434. doi: 10.1007/BF03346481. [DOI] [PubMed] [Google Scholar]
- Figà -Talamanca I, Cini C, Varricchio G, Dondero F, Gandini L, Lenzi A, et al. Effects of prolonged autovehicle driving on male reproductive function: A study among taxi drivers. American J of Indust Med. 1996;30:750–758. doi: 10.1002/(SICI)1097-0274(199612)30:6<750::AID-AJIM12>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Støy J, Hjøllund NHI, Mortensen JT, Burr H, Bonde JP. Semen quality and sedentary work position. Int J Andr. 2004;27:5–11. doi: 10.1046/j.0105-6263.2003.00428.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization . WHO laboratory manual for the examination and processing of human semen. 5 th Ed. Switzerland: World Health Organization Press; 2010. [Google Scholar]
- Jensen TK, Jacobsen R, Christensen K, Nielsen NC, Bostofte E. Good semen quality and life expectancy: A cohort study of 43,277 men. Am J Epidemiol. 2009;170:559–565. doi: 10.1093/aje/kwp168. [DOI] [PubMed] [Google Scholar]
- Eisenberg ML, Li S, Behr B, Cullen MR, Galusha D, Lamb DJ, et al. Semen quality, infertility and mortality in the USA. Hum Reprod. 2014;29:1567–1574. doi: 10.1093/humrep/deu106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsanezhad M, Jahromi B, Zare N, Keramati P, Khalili A, Parsa-Nezhad M. Epidemiology and etiology of infertility in Iran, systematic review and meta-analysis. J Womens Health, Issues Care. 2013;2:2–6. [Google Scholar]


