Abstract
Ablative fractionated carbon dioxide (fCO2) laser may be a useful tool to improve noticeable scars after skin cancer surgery. Therefore we evaluated 40 patients who have been treated with fCO2 laser for facial scars after skin cancer surgery. This retrospective study is based on blinded evaluation of pre‐ and postoperative photographs. Patients (n = 40), laypersons (n = 5) and experts (n = 5) evaluated the esthetics and the Vancouver scar scale as primary endpoints. Secondary endpoints included patient satisfaction and treatment safety. Patients, laypersons and experts consistently assessed a significant improvement of scar quality and appearance after fCO2 laser treatment, which was paralleled by high patient satisfaction. In conclusion, ablative fCO2 laser is effective in improving noticeable postsurgical scars. Patients are highly satisfied with post‐laser results.
Keywords: facial scars, fractional CO2 laser treatment, skin cancer surgery
1. INTRODUCTION
Skin cancer has become the most common neoplasia in humans. In the United States, approximately five million skin cancers are surgically removed each year. The face is by far the most concerning location for skin cancer. Despite optimal surgical technique, postoperative scars may remain noticeable or unsightly.
fCO2 laser therapy has emerged as an effective tool to improve disturbing skin scars and is increasingly used to treat unsightly scars post‐skin cancer surgery. Thus it helps improve psychological impairment and raise patients' self‐esteem.1
Several scientific studies have proven that fractional ablative and non‐ablative laser systems achieve a constant functional and cosmetic improvement of scars.2, 3, 4, 5, 6, 7, 8, 9 These lasers work according to the principle of fractional photothermolysis and lead to dermal collagen remodeling and neocollagenesis.10 fCO2 can be utilized earlier postoperatively than conventional ablative CO2 laser, as well as having a shorter postprocedural recovery time.2, 5 We conducted this retrospective study on 40 consecutive patients, in order to evaluate the results of our fCO2 laser treatment for facial scars after skin cancer surgery.
2. PATIENTS AND METHODS
The surgical team of the Department of Dermatology, University Hospital of Zurich, offers skin cancer surgery to approximately 2500 patients annually. In the period of 2015–2019, 47 patients with esthetically disturbing postoperative facial scars were treated with a fCO2 laser. All of these patients were traced and contacted for this study. 40/47 agreed to participate in a retrospective analysis of their treatment outcome.
2.1. Ethics statement
This study meets the requirements of the 1975 Declaration of Helsinki and has been authorized by the responsible ethics committee (project ID: 2018‐01563). All patients have given their written informed consent to participate in this study. The patients also consented to the anonymized use of the photographic material.
2.2. fCO2 laser treatment
We used a fractionated carbon dioxide laser (eCO2; Lutronic Co, Goyang, Korea). Local anesthesia consisted of a lidocaine 23% ‐ tetracain 7% cream. All lesions were treated with a pulse energy of 40–60 mJ in the static mode; two passes were delivered using a 120‐density tip (coverage 10%). Post‐intervention, patients were instructed to apply a skin‐soothing moisturizer several times daily for 5 days. The authors advised the patients to ensure sun protection with sunscreen (SPF 50+).
2.3. Photo documentation
All patients had standard studio photo documentation, which was conducted frontal, from the side and oblique (45%) perspective, using the same distance and illumination.
2.4. Assessment
Patients (n = 40), laypersons (n = 5), and experts (n = 5) assessed the preoperative and postoperative photographs as follows:
The patients rated the esthetics of their own scar, before and 3 months after the laser treatment, on a scale from 1 (esthetically inacceptable) ‐ 10 (no longer recognizable as a scar). First, they evaluated the result from their memory. Then they viewed and rated their photographs before and 3 months after laser treatment. In an additional step they applied the Vancouver scar scale (VSS) to score the scar before and 3 months after laser treatment. Subjective rating encompassed the effect on self‐confidence, therapeutic burden, pain, undesirable effects, time spent, and overall satisfaction, using a numeric scale from 1 (disappointed) to 5 (happy).
Pre‐ and postoperative photographs of each patient were mounted side by side at random and presented to the blinded raters. Five laypersons (employees of the cleaning and hygiene service of the University Hospital Zurich) and five professionals (board certified dermatologists) evaluated the scars on a scale from 1 (esthetically unacceptable) to 10 (no longer recognizable as a scar).
2.5. Statistics
Of the 47 patients who underwent fCO2 laser treatment at the University Hospital of Zurich in 2015–2019, 40 patients returned the declaration of consent, hence they could be included in the study. To our knowledge, this represents one of the largest sample sizes known in the literature, regarding the subject of fCO2 laser for scar treatment.
The mean scores for the ratings of the patients, the five laypersons and the five experts were calculated for each photograph before and after therapy and compared with an exact Wilcoxon signed rank test. The overall scores of the VSS were also compared with an exact Wilcoxon signed rank test. The individual parameters of the VSS before and after therapy were compared with an exact sign test. A p‐value of <0.05 has been defined as significant.11 All analyses were performed in the R programming language (version 3.6.2) (R Core Team, 2019).12, 13, 14, 15
3. RESULTS
A total of 40 patients consented to participate and were enrolled in this retrospective study. Baseline characteristics and the treatment protocols are given in Table 1.
TABLE 1.
Patient characteristics
| Baseline characteristics | n = 40 (100%) |
|---|---|
| Gender | |
| Male | 7 (17%) |
| Female | 33 (83%) |
| Mean age (year) | 62.7 (33–85) |
| Fitzpatrick skin phototype (I–IV) | |
| I | 2.4% |
| II | 73.8% |
| III | 21.4% |
| IV | 2.4% |
| Site | |
| Nose | 28 (70%) |
| Forehead | 5 (12.5%) |
| Cheek | 3 (7.5%) |
| Temples | 2 (5%) |
| Eyelids | 2 (5%) |
| Age of the scar at first laser treatment (months), Mean (range) | 5.7 (1–24) |
| No. of laser treatment sessions, Mean (range) | 2.2 (1–6) |
| Interval between laser treatment sessions (weeks), Mean (range) | 7.3 (4–12) |
| Follow‐up time (months), Mean (range) | 14.7 (3–26) |
Based on their memory, patients rated that the scars significantly improved after fCO2 laser treatment (median 3.5 pre vs. 7.0 post, p < 0.001). After viewing the photographs, rating was even more favorable (median 3.0 pre vs. 7.0 post, p < 0.001) (shown in Figure 1). However, the difference to the rating based on memory remained non‐significant (p = 0.71).
FIGURE 1.
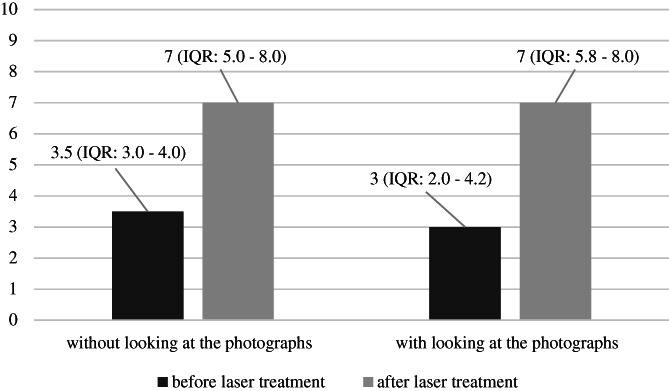
Comparison of the median esthetics scores, evaluated by patients
Ratings with the VSS are given in Table 2. Median sum score was significantly improved (6.0 pre vs. 4.0 post, p = <0.001).
TABLE 2.
Comparison of the VSS before and after laser therapy, evaluated by the patients
| VSS parameter | Pre‐laser treatment | Post‐laser treatment | p‐value |
|---|---|---|---|
| Pigmentation | 1.0 (IQR: 1.0–2.0) | 1.0 (IQR: 1.0–1.0) | 0.004 (9 patients improved; 0 patients deteriorated) |
| Vascularity | 1.0 (IQR: 0–2.0) | 0.5 (IQR: 0.0–1.0) | <0.001 (16 patients improved; 0 patients deteriorated) |
| Pliability | 2.0 (IQR: 2.0–3.0) | 1.0 (IQR: 1.0–2.2) | <0.001 (21 patients improved; 0 patients deteriorated) |
| Height | 1.0 (IQR: 1.0–2.0) | 1.0 (IQR: 0.0–1.0) | <0.001 (23 patients improved; 1 patient deteriorated) |
| Total VSS | 6 (IQR: 5.0–7.0) | 4 (IQR: 2.8–5.0) | <0.001 |
The median patient satisfaction with the overall laser treatment was 4.5 (IQR: 3.8‐5.0). Overall the laser treatment was very well tolerated. Side effects were mild to moderate pain during the treatment and mild to moderate post‐treatment erythema and edema (CTCAE grade 1‐2). There were no other adverse events such as dyspigmentation or worsening of the scar.
Based on blinded photographic scar assessment, both laypersons and experts consistently distinguished the baseline and the post‐interventional photograph in all patients. Furthermore, both groups rated that the scars post‐fCO2 laser treatment significantly improved (p < 0.001). Experts rated the effect higher by 0.5 points (p = 0.017) (shown in Figure 2).
FIGURE 2.
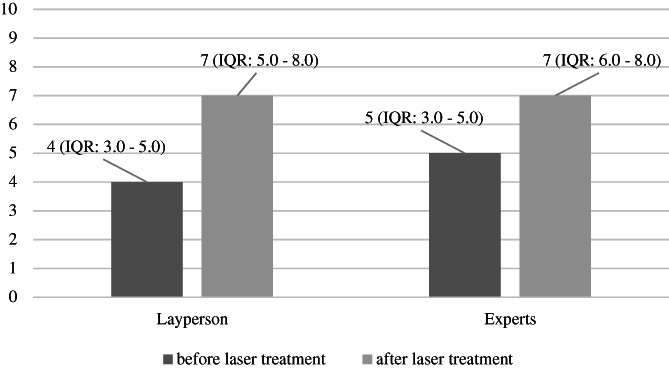
Comparison of the median esthetics scores, evaluated by the layperson and experts
4. DISCUSSION/CONCLUSION
This retrospective study suggests that fCO2 laser effectively improves disturbing facial scars post‐skin cancer surgery. At a first attempt the patients remembered their scars to have significantly improved after the laser intervention. Blinded patients, laypersons and experts rated the post‐interventional photographic aspect significantly higher, and patients rated the effect on the photos even more positive than based on their memory (examples shown in Figures 3, 4, 5, and 6 and in Figures S1 and S2).
FIGURE 3.
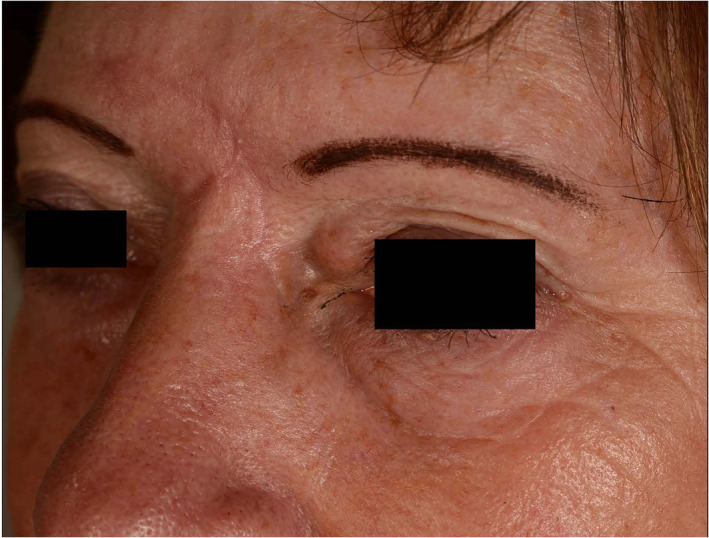
Patient 1: pre‐treatment photograph
FIGURE 4.
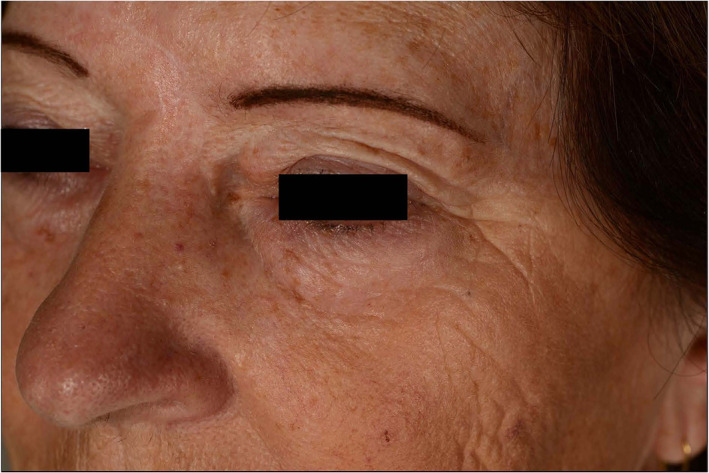
Patient 1: post‐treatment photograph
FIGURE 5.

Patient 2: pre‐treatment photograph
FIGURE 6.

Patient 2: post‐treatment photograph
The assessment of the scars on the Vancouver scar scale also showed significant improvements of the overall scores, as well as of all the individual parameters after laser therapy. The parameters “pliability” and “height” of the VSS improved the most, which did not surprise the authors, as the fCO2 laser most notably leads to collagen remodeling16 and is especially superior in the treatment of hypertrophic scars.2 Compared to Choi et al17 our results not only show an improvement of the parameter “pliability”, but also of the parameters “height”, “pigmentation”, and “vascularization”. The study of Sobanko et al showed a significant improvement in the overall VSS and in 3 out of 4 of its individual parameters, but no significant improvement of the parameter “pigmentation”.7 The study of Lee et al9 showed similar results to ours, but in a substantially smaller patient population.
The significant improvements of the esthetics of the facial scars after fCO2 laser treatment are reflected in the very high patient satisfaction and thus also lead to an improvement in patients' self‐confidence. Also, the side effects are usually mild and temporary such that the burden of treatment is low. High subjective patient satisfaction in connection with a fCO2 laser therapy has already been reported in other studies, however, our study, in addition to the work of Lee et. al, is the only one that has also objectified this through questionnaires.9
In summary, even though the assessments by the three different groups show some subtle differences, our results show a very coherent overall picture. The fact that patients, laypersons and experts consistently assessed a significant improvement of scar quality and appearance after fCO2 laser treatment makes the study results robust and represents definitely one of the biggest strengths of this study. The sample size of 40 patients is also considered another strength of this trial. Nearly all patients with a scar after skin cancer surgery in the face who went for fCO2 laser treatment at the Department of Dermatology USZ have been included in the study. This allows to make robust inference from the sample to the overall population. Other strengths of our study design include: blinding of the layperson and experts to the pre‐ and post‐treatment photographs, similar anatomic locations (centrofacial) as well as same etiology (skin cancer surgery) of all scars and an extended follow‐up of averagely 14.7 months.
There are also some limitations to our study. First, although objective measurement of scar appearance was done by the blinded layperson and experts, the patients could not be blinded to the pre‐ and post‐treatment photographs. This knowledge could have biased their subjective measurement of the scar esthetics. Second and even more important, this retrospective study does not include a control group. Since the whole scar was treated, the authors cannot make any comparison how the scar would have developed without laser treatment.
Next we plan a split‐scar study, where one half of the scar gets fCO2 laser treatment and the other half of the scar remains untreated, like previously performed on skin grafts by Datz E et al.18 Alternatively, a split‐scar study where one half of the scar population receives a fractional CO2 laser treatment and the other half is treated with an ablative fractional Er:YAG (erbium‐doped yttrium aluminum garnet) laser or a normal ablative CO2 laser, would be conceivable. This study would evaluate whether the fCO2 laser is really superior to other lasers or if the lasers all entail similar effectiveness. A recently published study showed a slight superiority of the fCO2 laser over a long pulsed Nd:YAG (neodymium‐doped yttrium aluminum garnet) laser in treatment of hypertrophic scars.19 However, this study had not been conducted in the format of a split‐scar study.
5. CONCLUSION
Disturbing facial scars from skin cancer surgery can be significantly improved by fCO2 laser treatment. Particularly esthetics, pliability, and height become significantly better. To confirm these findings, randomized controlled split scar studies are indispensable.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
AUTHOR CONTRIBUTIONS
Laurence Imhof, Juerg Hafner, Nina Wyss: study design, data collection. Laurence Imhof, Juerg Hafner, Nina Wyss: patient interviews, interviews of the laypersons and experts, writing of the manuscript. Nicole Graf: statistical analysis of the data collected.
Supporting information
Figure S1 Patient 3: pre‐treatment photograph.
Figure S2 Patient 3: post‐treatment photograph.
ACKNOWLEDGMENTS
We would like to thank the whole Department of Dermatology and especially the Units of Physical Therapies and Dermatosurgery of the University Hospital of Zurich for their help and support. Last but not least we would like to thank all the patients who participated in our study.
Wyss N, Graf N, Hafner J, Imhof L. Fractional CO2 laser to improve noticeable scars after skin cancer surgery: An appraisal by the patients, laypersons, and experts. Dermatologic Therapy. 2021;34(4):e14999. 10.1111/dth.14999
Contributor Information
Nina Wyss, Email: n97wyss@gmail.com.
Laurence Imhof, Email: laurence.imhof@usz.ch.
DATA AVAILABILITY STATEMENT
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1.Ngaage M, Agius M. The psychology of scars: a mini‐review. Psychiatr Danub. 2018;30(7):633‐638. [PubMed] [Google Scholar]
- 2.Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150(2):187‐193. [DOI] [PubMed] [Google Scholar]
- 3.Baca ME, Neaman KC, Rapp DA, Burton ME, Mann RJ, Renucci JD. Reduction of post‐surgical scarring with the use of ablative fractional CO2 lasers: a pilot study using a porcine model. Lasers Surg Med. 2017;49(1):122‐128. [DOI] [PubMed] [Google Scholar]
- 4.Cervelli V, Gentile P, Spallone D, et al. Ultrapulsed fractional CO2 laser for the treatment of post‐traumatic and pathological scars. J Drugs Dermatol. 2010;9(11):1328‐1331. [PubMed] [Google Scholar]
- 5.Ibrahim SM, Saudi WM, Abozeid MF, Elsaie ML. Early fractional carbon dioxide laser intervention for postsurgical scars in skin of color. Clin Cosmet Investig Dermatol. 2019;12:29‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shumaker PR, Kwan JM, Landers JT, Uebelhoer NS. Functional improvements in traumatic scars and scar contractures using an ablative fractional laser protocol. J Trauma Acute Care Surg. 2012;73(1):116‐121. [DOI] [PubMed] [Google Scholar]
- 7.Sobanko JF, Vachiramon V, Rattanaumpawan P, Miller CJ. Early postoperative single treatment ablative fractional lasing of Mohs micrographic surgery facial scars: a split‐scar, evaluator‐blinded study. Lasers Surg Med. 2015;47(1):1‐5. [DOI] [PubMed] [Google Scholar]
- 8.Weiss ET, Chapas A, Brightman L, et al. Successful treatment of atrophic postoperative and traumatic scarring with carbon dioxide ablative fractional resurfacing: quantitative volumetric scar improvement. Arch Dermatol. 2010;146(2):133‐140. [DOI] [PubMed] [Google Scholar]
- 9.Lee SH, Zheng Z, Roh MR. Early postoperative treatment of surgical scars using a fractional carbon dioxide laser: a split‐scar, evaluator‐blinded study. Dermatol Surg. 2013;39(8):1190‐1196. [DOI] [PubMed] [Google Scholar]
- 10.Laubach HJ, Manstein D. Fractional photothermolysis. Hautarzt. 2007;58(3):216‐218. [DOI] [PubMed] [Google Scholar]
- 11.Heston TF, King JM. Predictive power of statistical significance. World J Methodol. 2017;7(4):112‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hothorn T, Hornik K. exactRankTests: Exact Distributions for Rank and Permutation Tests. R package version 0.8–31. 2019.
- 13.Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria 2019. Available from https://www.R-project.org/.
- 14.Yoshida K.tableone: Create ‘Table 1’ to Describe Baseline Characteristics. R package version 0.10.0. 2019 Available from: https://CRAN.R-project.org/package=tableone.
- 15.Arnholt A, Evans B. BSDA: Basic Statistics and Data Analysis. R package version 1.2.0. 2017. Available from https://CRAN.R-project.org/package=BSDA.
- 16.Raulin C, Syrus K. Lasertherapie der Haut. Berlin‐Heidelberg: Springer‐Verlag; 2013. [Google Scholar]
- 17.Choi JE, Oh GN, Kim JY, Seo SH, Ahn HH, Kye YC. Ablative fractional laser treatment for hypertrophic scars: comparison between Er:YAG and CO2 fractional lasers. J Dermatolog Treat. 2014;25(4):299‐303. [DOI] [PubMed] [Google Scholar]
- 18.Datz E, Schonberger C, Zeman F, et al. Fractional carbon dioxide laser resurfacing of skin grafts: long‐term results of a prospective, randomized, split‐scar, evaluator‐blinded study. Lasers Surg Med. 2018;50(10):1010‐1016. [DOI] [PubMed] [Google Scholar]
- 19.Tawfic SO, El‐Tawdy A, Shalaby S, et al. Evaluation of fractional CO2 versus long pulsed Nd:YAG lasers in treatment of hypertrophic scars and keloids: a randomized clinical trial. Lasers Surg Med. 2020;52:959‐965. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Patient 3: pre‐treatment photograph.
Figure S2 Patient 3: post‐treatment photograph.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.


