This cross-sectional study reports the patterns of methamphetamine use (eg, with or without cocaine, frequency of use, and injected) among participants in the 2015 to 2019 National Survey on Drug Use and Health.
Key Points
Question
Are trends in methamphetamine use among populations with socioeconomic risk factors and comorbidities associated with increases in overdose mortality?
Findings
In this cross-sectional study of 195 711 respondents to a national survey from 2015 to 2019, methamphetamine use, frequent use, co-use with cocaine, and methamphetamine use disorder increased 43% to 105%. Methamphetamine use disorder without injection doubled overall and increased 10-fold among Black individuals, and risk factors included lower socioeconomic status factors, criminal justice involvement, and comorbidities.
Meaning
This study found riskier patterns of methamphetamine use and increased diversity in populations with methamphetamine use disorder risk (particularly those with socioeconomic risk factors and comorbidities) during a time of increasing overdose mortality.
Abstract
Importance
Mortality associated with methamphetamine use has increased markedly in the US. Understanding patterns of methamphetamine use may help inform related prevention and treatment.
Objective
To assess the national trends in and correlates of past-year methamphetamine use, methamphetamine use disorder (MUD), injection, frequent use, and associated overdose mortality from 2015 to 2019.
Design, Setting, and Participants
This cross-sectional study analyzed methamphetamine use, MUD, injection, and frequent use data from participants in the 2015 to 2019 National Surveys on Drug Use and Health (NSDUH). Mortality data were obtained from the 2015 to 2019 National Vital Statistics System Multiple Cause of Death files.
Exposures
Methamphetamine use.
Main Outcomes and Measures
Methamphetamine use, MUD, injection, frequent use, and overdose deaths.
Results
Of 195 711 NSDUH respondents aged 18 to 64 years, 104 408 were women (weighted percentage, 50.9%), 35 686 were Hispanic individuals (weighted percentage, 18.0%), 25 389 were non-Hispanic Black (hereafter, Black) individuals (weighted percentage, 12.6%), and 114 248 were non-Hispanic White (hereafter, White) individuals (weighted percentage, 60.6%). From 2015 to 2019, overdose deaths involving psychostimulants other than cocaine (largely methamphetamine) increased 180% (from 5526 to 15 489; P for trend <.001); methamphetamine use increased 43% (from 1.4 million [95% CI, 1.2-1.6 million] to 2.0 million [95% CI, 1.7-2.3 million]; P for trend = .002); frequent methamphetamine use increased 66% (from 615 000 [95% CI, 512 000-717 000] to 1 021 000 [95% CI, 860 000-1 183 000]; P for trend = .002); methamphetamine and cocaine use increased 60% (from 402 000 [95% CI, 306 000-499 000] to 645 000 [95% CI, 477 000-813 000]; P for trend = .001); and MUD without injection increased 105% (from 397 000 [95% CI, 299 000-496 000] to 815 000 [95% CI, 598 000-1 033 000]; P for trend = .006). The prevalence of MUD or injection surpassed the prevalence of methamphetamine use without MUD or injection in each year from 2017 to 2019 (60% to 67% vs 37% to 40%; P for trend ≤.001). Adults with MUD or using injection were more likely to use methamphetamine frequently (52.68%-53.84% vs 32.59%; adjusted risk ratio, 1.62-1.65; 95% CI, 1.35-1.94). From 2015 to 2019, the adjusted prevalence of MUD without injection more than tripled among heterosexual women (from 0.24% to 0.74%; P < .001) and lesbian or bisexual women (from 0.21% to 0.71%; P < .001) and more than doubled among heterosexual men (from 0.29% to 0.79%; P < .001) and homosexual or bisexual men (from 0.29% to 0.80%; P = .007). It increased over 10-fold among Black individuals (from 0.06% to 0.64%; P < .001), nearly tripled among White individuals (from 0.28% to 0.78%; P < .001), and more than doubled among Hispanic individuals (from 0.39% to 0.82%; P < .001). Risk factors for methamphetamine use, MUD, injection, and frequent use included lower educational attainment, lower annual household income, lack of insurance, housing instability, criminal justice involvement, comorbidities (eg, HIV/AIDS, hepatitis B or C virus, depression), suicidal ideation, and polysubstance use.
Conclusions and Relevance
This cross-sectional study found consistent upward trends in overdose mortality, greater risk patterns of methamphetamine use, and populations at higher risk for MUD diversifying rapidly, particularly those with socioeconomic risk factors and comorbidities. Evidence-based prevention and treatment interventions are needed to address surges in methamphetamine use and MUD.
Introduction
In the US, overdose deaths involving psychostimulants with abuse potential other than cocaine (ie, largely methamphetamine) increased in the past decade1,2 more than doubling from 2.4 to 5.0 per 100 000 population from 2016 to 2019 alone.1 Furthermore, based on provisional mortality data, the estimated national number of these psychostimulant-associated overdose deaths increased 46% from 16 011 during November 2018 to October 2019 to 23 352 during November 2019 to October 2020.3
By contrast, increases in methamphetamine use have been less dramatic. Among adults aged 26 years or older, the prevalence of past-year methamphetamine use increased 60% from 0.5% (1.1 million people) in 2016 to 0.8% (1.7 million people) in 2019.4 Prevalence of past-year methamphetamine use disorder (MUD) increased 33% from 0.3% (539 000 people) in 2016 to 0.4% (904 000 people) in 2019.4 Methamphetamine may serve as an opioid substitute or provide synergistic euphoria for those who co-use opioids.5,6 Currently, methamphetamine use is increasing among people who misuse opioids7 and those who are admitted for heroin treatment,8 whereas heroin use is increasing among people who are admitted into primary methamphetamine treatment.9 Fifty percent of psychostimulant-involved overdose deaths also involved opioids in 2017.10
In addition to increases in lethality associated with higher consumption of methamphetamine mixed with opioids,7,9 it is still unclear how trends in methamphetamine use among vulnerable populations and specific patterns of methamphetamine use (eg, with or without cocaine, frequent use, MUD, and injection) may be associated with greater risk for overdose mortality. Understanding changes in the patterns of methamphetamine use as functions of age, sex and sexual orientation, and race/ethnicity may help explain the increases in overdose deaths and inform prevention and treatment interventions. To address this knowledge gap, we conducted a cross-sectional study among US adults aged 18 to 64 years, the population at the highest risk for substance use and overdose mortality.2,4 Specifically, we assessed the national trends in and risk factors of past-year methamphetamine use, MUD, injection, frequent use, and associated overdose mortality.
Methods
Data Sources
We examined data from 195 711 individuals aged 18 to 64 years who participated in the National Survey on Drug Use and Health (NSDUH) from 2015 to 2019. These samples provided nationally representative data on methamphetamine use, frequency of use, MUD, and injection among the US civilian, noninstitutionalized populations aged 12 years or older. The NSDUH data collection protocol was approved by the US Office of Management and Budget and the institutional review board at the Research Triangle Institute International. This cross-sectional study received approval from the RTI Institutional Review Board. Oral informed consent was obtained from each NSDUH participant.4
The NSDUH was conducted by interviewers during in-person visits to households and noninstitutional group quarters. Additional details about the NSDUH methods are provided elsewhere.11 Audio computer-assisted self-administered interviewing was used to provide respondents with a private, confidential way to record answers. For the 2015 to 2019 NSDUH, the annual mean weighted screening response rate was 75.3%, and the annual mean weighted interview response rate was 67.3%.
In addition, we examined data from the 2015 to 2019 National Vital Statistics System Multiple Cause of Death files.12 Drug overdose deaths were those assigned an underlying cause of death with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes (X40-X44 [unintentional], X60-X64 [suicide], X85 [homicide], and Y10-Y14 [undetermined intent]). Overdose deaths that involved psychostimulants other than cocaine (largely methamphetamine) were those with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code T43.6.1
Measures
The NSDUH interviewers asked respondents about lifetime and past-year use of tobacco, alcohol, cannabis, cocaine, heroin, inhalants, methamphetamine, and hallucinogens as well as the number of days these substances were used in the past year. Frequent methamphetamine use was defined as 100 days or more in the past 12 months. Respondents were also asked about past-year injection of heroin, cocaine, and methamphetamine as well as lifetime and past-year misuse of prescription opioids, sedatives or tranquilizers, and stimulants.
Using diagnostic criteria specified in the DSM-IV,4,11,13 the NSDUH estimated the prevalence of specific substance use disorders (alcohol; cannabis; cocaine; heroin; methamphetamine; hallucinogens; and prescription opioids, tranquilizers or sedatives, and stimulants) in the past year. The NSDUH also assessed past-year major depressive episodes using the DSM-IV criteria11,14 and past-month nicotine dependence among cigarette smokers using the Nicotine Dependence Syndrome Scale.15 These measures of substance use and use disorders have demonstrated good validity and reliability.16,17,18
In addition to sociodemographic characteristics (age, sex, sexual orientation, race and ethnicity, educational attainment, employment status, annual household income, marital status, health insurance, and metropolitan statistical area), questions about medical diagnoses from a physician or other health care professional (lifetime diagnoses: hypertension, heart disease, diabetes, cancer, chronic obstructive pulmonary disease, asthma, hepatitis B or C virus [HBV or HCV], or HIV/AIDS; past-year diagnoses: any sexually transmitted infection) were also queried. Respondents were asked about past-year probation or parole status and the number of residential moves made in the past year (which is an indicator of housing instability). Adult respondents were asked about serious thoughts of suicide, suicide plan, and suicide attempt in the past year.19 The NSDUH respondents self-identified racial and ethnic origin (ie, Hispanic, non-Hispanic Asian [hereafter, Asian], non-Hispanic Black [hereafter, Black], non-Hispanic Native Hawaiian or Other Pacific Islander [hereafter, Native Hawaiian or Other Pacific Islander], non-Hispanic White [hereafter, White], non-Hispanic with more than 1 race or ethnicity) according to the classifications developed by the US Census Bureau.
Statistical Analysis
All analyses were conducted only for survey data from 2015 to 2019. We could not examine methamphetamine-related data from previous years because of NSDUH methods changes that resulted in trend breaks in 2015.
First, we performed descriptive analyses to examine linear, quadratic, cubic, and quartic trends in psychostimulant-involved overdose deaths with or without opioids or cocaine; methamphetamine use overall; methamphetamine use subgroups (use without MUD or injection; MUD or injection; MUD without injection, including symptoms such as compulsive methamphetamine-seeking behavior, continued use despite adverse consequences, loss of control over use, and inability to reduce or stop using20; comorbid mental disorders21 and other substance use disorders, all of which may be associated with increased risk of death22; injection, which is associated with unique high health risks such as septic shock with multiorgan failure, HIV/AIDS, HBV or HCV regardless of MUD status); and frequent methamphetamine use.
Second, given that previous research has shown the associations of methamphetamine use and MUD with socioenvironmental factors (eg, sociodemographic characteristics,2,3,7,8,9 housing instability,23,24 and criminal justice involvements24) and co-occurring conditions (eg, medical conditions,24 mental health status,21 and other substance use7,8,9,21,22), we applied bivariable and multivariable multinomial logistic regression models to simultaneously examine correlates (from these factors) of past-year methamphetamine use without MUD or injection, MUD without injection, and injection regardless of MUD.
Third, we applied bivariable and multivariable logistic regression models to examine correlates of frequent methamphetamine use among persons with past-year methamphetamine use.25 Multicollinearity and potential interaction effects were tested and were not found in final models.
For each analysis, a 2-tailed P < .05 was considered statistically significant. SUDAAN software, version 11.0.3 (RTI International) was used for all data analyses to account for the NSDUH’s complex sample design and sample weights. Data were analyzed from February 8 to March 8, 2021.
Results
Methamphetamine use, MUD, injection, and frequent use data from a total of 195 711 NSDUH respondents aged 18 to 64 years were analyzed. Of these individuals, 104 408 were women (weighted percentage, 50.9%), 91 303 were men (weighted percentage, 49.1%), 35 686 were Hispanic individuals (weighted percentage, 18.0%), 25 389 were Black individuals (weighted percentage, 12.6%), and 114 248 were White individuals (weighted percentage, 60.6%). Psychostimulant-involved overdose death data were examined among decedents aged 18 to 64 years from the National Vital Statistics System’s Multiple Cause of Death Files.12
Trends in Psychostimulant-Involved Overdose Deaths
Overdose deaths that involved psychostimulants other than cocaine (largely methamphetamine) increased substantially from 2015 to 2019. Overall, the number of overdose deaths increased 180% (from 5526 to 15 489; P for trend <.001). Specifically, overdose deaths involving psychostimulants with opioids increased 266% (from 2306 to 8438; P for trend <.001), psychostimulants with cocaine increased 379% (from 370 to 1772; P for trend = .007), psychostimulants without opioids increased 119% (from 3220 to 7051; P for trend <.001), psychostimulants without cocaine increased 166% (from 5156 to 13 717; P for trend <.001), and psychostimulants without opioids or cocaine increased 116% (from 3102 to 6698; P for trend <.001) (Table 1).
Table 1. Overdose Deaths Involving Psychostimulants Other Than Cocaine and Methamphetamine Use, Use Disorder, Injection, and Frequent Use Among US Adults Aged 18 to 64 Years.
| Variable | Year | P for trenda | ||||
|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | ||
| Overdose deaths involving psychostimulants other than cocaine, No.b | ||||||
| Overall | 5526 | 7301 | 10 029 | 12 203 | 15 489 | <.001 |
| With opioids | 2306 | 3345 | 5114 | 6269 | 8438 | <.001 |
| Without opioids | 3220 | 3956 | 4915 | 5934 | 7051 | <.001 |
| With cocaine | 370 | 690 | 1116 | 1433 | 1772 | .007 |
| Without cocaine | 5156 | 6662 | 8913 | 10 770 | 13 717 | <.001 |
| Without opioids or cocaine | 3102 | 3765 | 4665 | 5609 | 6698 | <.001 |
| Methamphetamine use, MUD, and methamphetamine injection, No. (95% CI), thousandsc | ||||||
| Any methamphetamine use | 1612 (1394-1829)d | 1381 (1193-1568)d | 1675 (1446-1903) | 1858 (1561-2155) | 1971 (1660-2282) | .002 |
| MUD | 741 (578-905)d | 672 (539-805)d | 965 (799-1132) | 1036 (809-1263) | 1091 (816-1365) | .003 |
| Injection | 321 (224-418) | 388 (277-498) | 472 (352-591) | 422 (303-541) | 365 (257-473) | .07e |
| MUD without injection | 549 (417-682) | 397 (299-496)d | 647 (502-792) | 730 (548-912) | 815 (598-1033) | .006 |
| Methamphetamine use without MUD or injection | 742 (631-852) | 596 (460-732) | 556 (428-684)d | 706 (540-871) | 790 (613-968) | .01e |
| Methamphetamine use and opioid misuse | 696 (556-836) | 696 (562-831) | 751 (606-896) | 881 (691-1072) | 865 (653-1077) | .03 |
| Methamphetamine use without opioid misuse | 916 (760-1071) | 685 (534-835)d | 924 (731-1116) | 977 (761-1192) | 1106 (895-1317) | .02 |
| Methamphetamine use and cocaine use | 402 (306-499)d | 420 (297-543)d | 565 (439-691) | 656 (500-813) | 645 (477-813) | .001 |
| Methamphetamine use without cocaine use | 1210 (1015-1404) | 961 (810-1112)d | 1109 (928-1291) | 1202 (977-1426) | 1326 (1100-1552) | .054e |
| Methamphetamine use without opioid misuse or cocaine use | 766 (622-911) | 527 (404-651)d | 674 (511-837) | 708 (533-883) | 833 (668-997) | .005e |
| Frequent (≥100 d in past 12 mo) methamphetamine use, No. (95% CI), thousandsc | ||||||
| Among adults with any methamphetamine use | 649 (551-747)d | 615 (512-717)d | 716 (584-848)d | 837 (705-968) | 1021 (860-1183) | .002 |
| Among adults with methamphetamine use but without MUD or injection | 157 (96-219)d | 196 (115-276) | 180 (117-244) | 251 (155-347) | 327 (235-419) | .01 |
| Among adults with MUD but without injection | 344 (286-402) | 203 (144-262)d | 271 (190-353)d | 373 (312-434) | 455 (365-544) | .02e |
| Among adults with injection regardless of MUD | 148 (97-199) | 216 (156-276) | 264 (210-318) | 213 (144-282) | 240 (195-284) | .15 |
Abbreviations: MUD, methamphetamine use disorder; NSDUH, National Survey on Drug Use and Health.
P values were calculated for linear trends (except where noted). Linear, quadratic, cubic, and quartic trends were tested, and neither a cubic trend nor a quartic trend was found in the measures used.
Data source: the 2015 to 2019 National Vital Statistics System Multiple Cause of Death files. Deaths may involve other drugs in addition to the referent drug, drugs involving more than 1 drug are counted in more than 1 total, and each estimate was statistically significantly different from the corresponding 2019 estimate (P < .001).
Data sources: the 2015 to 2019 NSDUH.4
The estimate was statistically significantly different from the corresponding 2019 estimate (P < .05).
P values were calculated for quadratic trends.
Trends in Methamphetamine Use, Co-Use, MUD, and Injection
The number of persons who reported past-year methamphetamine use increased from 2015 to 2019 (Table 1). Overall, we found a 43% increase (from 1.4 million [95% CI, 1.2-1.6 million] to 2.0 million [95% CI, 1.7-2.3 million]; P for trend = .002). Methamphetamine and opioid co-use showed an upward trend, but the 2019 estimate was similar to the 2015 to 2018 estimates. Cocaine co-use also increased 60% (from 402 000 [95% CI, 306 000-499 000] to 645 000 [95% CI, 477 000-813 000]; P for trend = .001). Methamphetamine use without opioids increased 61% (from 685 000 [95% CI, 534 000-835 000] to 1 106 000 [95% CI, 895 000-1 317 000]; P for trend = .02), as did methamphetamine use without opioids and cocaine by 58% (from 527 000 [95% CI, 404 000-651 000] to 833 000 [95% CI, 668 000-997 000]; P for trend = .005).
The number of adults with MUD increased 62% (from 672 000 [95% CI, 539 000-805 000] to 1 091 000 [95% CI, 816 000-1 365 000]; P for trend = .003), those with MUD without injection increased 105% (from 397 000 [95% CI, 299 000-496 000] to 815 000 [95% CI, 598 000-1 033 000]; P for trend = .006), and those with methamphetamine use but without MUD or injection increased 42% (from 556 000 [95% CI, 428 000-684 000] to 790 000 [95% CI, 613 000-968 000]; P for trend = .01). Among adults with past-year methamphetamine use, the prevalence of those with MUD or injection surpassed the prevalence of those with methamphetamine use without MUD or injection in each year from 2017 to 2019 (60% to 67% [1 118 000-1 181 000] vs 37% to 40% [556 000-790 000]; P for trend ≤.001).
Trends in Frequent Methamphetamine Use
From 2015 to 2019, the number of persons who reported frequent use of methamphetamine increased 66% (from 615 000 [95% CI, 512 000-717 000] to 1 021 000 [95% CI, 860 000-1 183 000]; P for trend = .002) (Table 1). Frequent use increased 108% (from 157 000 [95% CI, 96 000-219 000] to 327 000 [95% CI, 235 000-419 000]; P for trend = .01) for methamphetamine use without MUD or injection and increased 124% (from 203 000 [95% CI, 144 000-262 000] to 455 000 [95% CI, 365 000-544 000]; P for trend = .02) for MUD without injection.
Adjusted Prevalence and Correlates of Methamphetamine Use Without MUD or Injection
The multivariable multinomial logistic regression analysis showed that the adjusted prevalence of past-year methamphetamine use without MUD or injection was higher among homosexual men than heterosexual women (0.65% vs 0.32%; adjusted risk ratio [ARR], 2.02; 95% CI, 1.12-3.66) (Table 2 and Table 3). Bivariable multinomial logistic regression results are provided in the eTable in the Supplement. It was higher among American Indian or Alaska Native, Hispanic, and White individuals than among Black individuals (0.29%-0.50% vs 0.13%; ARR, 2.24-3.92; 95% CI, 1.40-7.32).
Table 2. Adjusted Prevalence of Past-Year Methamphetamine Use, Use Disorder, and Injection Among Adults Aged 18 to 64 Yearsa.
| Variable | Weighted % (95% CI) | ||
|---|---|---|---|
| Methamphetamine use without MUD or injection (n = 194 554) | MUD without injection (n = 194 465) | Injection regardless of MUD (n = 194 240) | |
| NSDUH year | |||
| 2015 | 0.38 (0.33-0.44) | 0.28 (0.22-0.35)b | 0.18 (0.13-0.23) |
| 2016 | 0.30 (0.23-0.38) | 0.20 (0.15-0.26)b | 0.18 (0.14-0.24) |
| 2017 | 0.28 (0.23-0.36)b | 0.33 (0.26-0.43) | 0.21 (0.17-0.27) |
| 2018 | 0.36 (0.29-0.45) | 0.37 (0.30-0.47) | 0.24 (0.18-0.32) |
| 2019 (Reference) | 0.40 (0.31-0.50) | 0.41 (0.32-0.52) | 0.19 (0.15-0.25) |
| Age group, y | |||
| 18-23 (Reference) | 0.24 (0.19-0.29) | 0.16 (0.13-0.19) | 0.07 (0.05-0.10) |
| 24-34 | 0.31 (0.26-0.37)b | 0.32 (0.27-0.39)b | 0.18 (0.15-0.22)b |
| 35-49 | 0.44 (0.38-0.52)b | 0.47 (0.38-0.57)b | 0.29 (0.24-0.36)b |
| 50-64 | 0.40 (0.32-0.50)b | 0.33 (0.23-0.47)b | 0.30 (0.22-0.42)b |
| Sex and sexual orientation | |||
| Homosexual men | 0.65 (0.38-1.10)b | 0.36 (0.19-0.69) | 0.55 (0.37-0.83)b |
| Lesbian women | 0.30 (0.15-0.61) | 0.20 (0.09-0.44) | 0.06 (0.03-0.13)b |
| Bisexual men | 0.55 (0.27-1.11) | 0.37 (0.23-0.59) | 0.15 (0.07-0.30) |
| Bisexual women | 0.30 (0.21-0.41) | 0.29 (0.22-0.38) | 0.25 (0.17-0.35)b |
| Men, unknown sexual orientation | 0.17 (0.07-0.43) | 0.63 (0.19-2.09) | 0.28 (0.11-0.74) |
| Women, unknown sexual orientation | 0.34 (0.14-0.80) | 0.17 (0.05-0.55) | 0.07 (0.02-0.31) |
| Heterosexual men | 0.35 (0.31-0.40) | 0.35 (0.30-0.41)b | 0.21 (0.18-0.25)b |
| Heterosexual women (Reference) | 0.32 (0.26-0.39) | 0.27 (0.22-0.33) | 0.15 (0.12-0.19) |
| Race and ethnicity | |||
| American Indian or Alaska Native | 0.50 (0.32-0.78)b | 0.86 (0.44-1.68)b | 0.32 (0.22-0.47)b |
| Asian | 0.18 (0.09-0.38) | 0.29 (0.12-0.70)b | 0.18 (0.04-0.70) |
| Black (Reference) | 0.13 (0.08-0.20) | 0.09 (0.05-0.15) | 0.06 (0.03-0.10) |
| Hispanic | 0.29 (0.21-0.39)b | 0.44 (0.34-0.57)b | 0.16 (0.11-0.24)b |
| Native Hawaiian or Other Pacific Islander | 0.23 (0.08-0.69) | 0.53 (0.23-1.23)b | 0.39 (0.13-1.12)b |
| White | 0.42 (0.37-0.47)b | 0.34 (0.29-0.40)b | 0.23 (0.20-0.26)b |
| Non-Hispanic, >1 race | 0.24 (0.15-0.38) | 0.30 (0.18-0.48)b | 0.24 (0.13-0.45)b |
| Educational attainment | |||
| <High school education | 0.44 (0.35-0.55)b | 0.40 (0.32-0.51)b | 0.23 (0.16-0.32)b |
| High school diploma | 0.40 (0.33-0.49)b | 0.37 (0.32-0.44)b | 0.22 (0.18-0.28)b |
| Some college courses | 0.32 (0.27-0.37) | 0.30 (0.25-0.37)b | 0.20 (0.16-0.24)b |
| ≥College degree (Reference) | 0.24 (0.17-0.34) | 0.14 (0.09-0.24) | 0.10 (0.06-0.18) |
| Annual household income, $ | |||
| <20 000 | 0.42 (0.33-0.53)b | 0.38 (0.32-0.45)b | 0.22 (0.18-0.27) |
| 20 000-49 999 | 0.35 (0.29-0.43) | 0.33 (0.26-0.41)b | 0.19 (0.16-0.24) |
| 50 000-74 999 | 0.29 (0.23-0.37) | 0.31 (0.21-0.45) | 0.20 (0.13-0.30) |
| ≥75 000 (Reference) | 0.28 (0.23-0.35) | 0.21 (0.16-0.28) | 0.18 (0.13-0.25) |
| Health insurance | |||
| Private only (Reference) | 0.25 (0.21-0.29) | 0.19 (0.15-0.25) | 0.15 (0.11-0.20) |
| Uninsured | 0.39 (0.32-0.49)b | 0.37 (0.30-0.46)b | 0.26 (0.21-0.33)b |
| Medicaid only | 0.46 (0.38-0.56)b | 0.49 (0.40-0.59)b | 0.22 (0.18-0.27) |
| Other | 0.46 (0.35-0.62)b | 0.29 (0.21-0.41) | 0.18 (0.13-0.26) |
| No. of times moved in past year | |||
| 0 (Reference) | 0.32 (0.28-0.37) | 0.29 (0.25-0.33) | 0.15 (0.12-0.18) |
| 1 | 0.41 (0.33-0.52) | 0.30 (0.23-0.40) | 0.23 (0.17-0.31)b |
| 2 | 0.35 (0.25-0.49) | 0.43 (0.33-0.58)b | 0.24 (0.18-0.33)b |
| 3 | 0.35 (0.26-0.47) | 0.45 (0.33-0.60)b | 0.45 (0.34-0.59)b |
| MSA status | |||
| Large MSA (Reference) | 0.32 (0.27-0.38) | 0.32 (0.26-0.39) | 0.15 (0.12-0.18) |
| Small MSA | 0.37 (0.31-0.44) | 0.34 (0.27-0.43) | 0.32 (0.25-0.40)b |
| Nonmetropolitan area | 0.37 (0.31-0.43) | 0.31 (0.26-0.37) | 0.20 (0.17-0.25)b |
| Probation or parole in past year | |||
| Yes | 0.65 (0.48-0.87)b | 1.09 (0.83-1.43)b | 0.45 (0.34-0.59)b |
| No (Reference) | 0.33 (0.29-0.36) | 0.26 (0.22-0.29) | 0.16 (0.14-0.19) |
| HIV/AIDS | |||
| Yes | 0.55 (0.17-1.74) | 1.40 (0.82-2.38)b | 0.65 (0.28-1.49)b |
| No (Reference) | 0.35 (0.31-0.38) | 0.31 (0.27-0.36) | 0.19 (0.17-0.22) |
| HBV or HCV | |||
| Yes | 0.65 (0.38-1.11)b | 0.32 (0.18-0.58) | 0.44 (0.30-0.63)b |
| No (Reference) | 0.33 (0.30-0.37) | 0.32 (0.28-0.37) | 0.18 (0.16-0.20) |
| STI in past year | |||
| Yes | 0.50 (0.34-0.74)b | 0.45 (0.31-0.66)b | 0.30 (0.21-0.44)b |
| No (Reference) | 0.34 (0.30-0.37) | 0.31 (0.27-0.36) | 0.19 (0.17-0.22) |
| MDE in past year | |||
| Yes | 0.30 (0.24-0.38) | 0.46 (0.35-0.60)b | 0.20 (0.15-0.28) |
| Did not answer | 0.50 (0.26-0.96) | 0.24 (0.08-0.70) | 0.49 (0.23-1.05)b |
| No (Reference) | 0.35 (0.31-0.40) | 0.29 (0.25-0.33) | 0.19 (0.17-0.23) |
| Serious thoughts of suicide in past year | |||
| Yes | 0.46 (0.35-0.61)b | 0.47 (0.34-0.64)b | 0.30 (0.23-0.40)b |
| Did not answer | 0.86 (0.42-1.74)b | 0.56 (0.18-1.76) | 0.15 (0.06-0.41) |
| No (Reference) | 0.32 (0.29-0.37) | 0.29 (0.24-0.34) | 0.18 (0.15-0.21) |
| Nicotine dependence in past month | |||
| Yes | 0.51 (0.43-0.61)b | 0.48 (0.40-0.58)b | 0.26 (0.22-0.31)b |
| No (Reference) | 0.27 (0.23-0.31) | 0.23 (0.19-0.29) | 0.14 (0.11-0.18) |
| Cannabis use disorder or daily/near daily use of cannabis in past year | |||
| Yes | 0.58 (0.46-0.73)b | 0.55 (0.44-0.68)b | 0.22 (0.17-0.28)b |
| No, but past year use | 0.62 (0.51-0.77)b | 0.56 (0.44-0.71)b | 0.30 (0.25-0.37)b |
| No past year use (Reference) | 0.19 (0.15-0.24) | 0.17 (0.13-0.23) | 0.14 (0.11-0.17) |
| Cocaine use in past year | |||
| Yes | 0.91 (0.68-1.20)b | 0.64 (0.48-0.85)b | 0.20 (0.15-0.27) |
| No (Reference) | 0.27 (0.24-0.30) | 0.27 (0.24-0.31) | 0.20 (0.17-0.24) |
| Hallucinogen use in past year | |||
| Yes | 0.56 (0.43-0.73)b | 0.42 (0.31-0.56)b | 0.36 (0.26-0.51)b |
| No (Reference) | 0.31 (0.28-0.35) | 0.31 (0.27-0.35) | 0.18 (0.15-0.20) |
| Heroin use or prescription opioid misuse in past year | |||
| Yes | 0.62 (0.49-0.80)b | 0.59 (0.48-0.73)b | 0.39 (0.30-0.52)b |
| No (Reference) | 0.29 (0.25-0.33) | 0.25 (0.21-0.30) | 0.12 (0.09-0.15) |
| Prescription tranquilizer or sedative misuse in past year | |||
| Yes | 0.44 (0.34-0.57) | 0.50 (0.39-0.63)b | 0.24 (0.18-0.32) |
| No (Reference) | 0.33 (0.29-0.37) | 0.29 (0.24-0.33) | 0.19 (0.16-0.22) |
| Prescription stimulant misuse in past year | |||
| Yes | 0.50 (0.39-0.64)b | 0.42 (0.31-0.58) | 0.37 (0.25-0.54)b |
| No (Reference) | 0.32 (0.29-0.36) | 0.31 (0.27-0.36) | 0.17 (0.15-0.20) |
| Heroin injection in past year | |||
| Yes | 0.40 (0.23-0.68) | 0.18 (0.08-0.41) | 1.38 (0.96-1.96)b |
| No (Reference) | 0.35 (0.32-0.38) | 0.33 (0.29-0.38) | 0.14 (0.12-0.16) |
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; MDE, major depressive episode; MSA, metropolitan statistical area; MUD, methamphetamine use disorder; NSDUH, National Survey on Drug Use and Health; STI, sexually transmitted infection.
Data source: 2015 to 2019 NSDUH.4 Bivariable multinomial logistic regression results are presented in the eTable in the Supplement.
Each estimate was statistically significantly different from the estimate of the reference group within the same cell. Each estimate was adjusted for the other covariates presented in this table.
Table 3. Correlates of Past-Year Methamphetamine Use, Use Disorder, and Injection Among Adults Aged 18-64 Yearsa.
| Correlate | ARR (95% CI) | ||
|---|---|---|---|
| Methamphetamine use without MUD or injection vs no methamphetamine use (n = 194 554) | MUD without injection vs no methamphetamine use (n = 194 465) | Injection regardless of MUD vs no methamphetamine use (n = 194 240) | |
| NSDUH year | |||
| 2015 | 0.95 (0.73-1.24) | 0.69 (0.48-0.98)b | 0.93 (0.65-1.33) |
| 2016 | 0.75 (0.54-1.03) | 0.50 (0.36-0.68)b | 0.97 (0.65-1.44) |
| 2017 | 0.72 (0.53-0.97)b | 0.83 (0.58-1.18) | 1.12 (0.80-1.57) |
| 2018 | 0.90 (0.65-1.26) | 0.92 (0.74-1.14) | 1.28 (0.85-1.94) |
| 2019 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Age group, y | |||
| 18-23 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 24-34 | 1.32 (1.05-1.67)b | 2.07 (1.57-2.73)b | 2.53 (1.83-3.52)b |
| 35-49 | 1.89 (1.43-2.48)b | 3.00 (2.20-4.10)b | 4.07 (2.84-5.83)b |
| 50-64 | 1.69 (1.24-2.31)b | 2.13 (1.39-3.27)b | 4.20 (2.62-6.71)b |
| Sex and sexual orientation | |||
| Homosexual men | 2.02 (1.12-3.66)b | 1.33 (0.67-2.61) | 3.66 (2.17-6.16)b |
| Lesbian women | 0.95 (0.45-2.02) | 0.73 (0.31-1.74) | 0.41 (0.18-0.91)b |
| Bisexual men | 1.73 (0.81-3.70) | 1.36 (0.82-2.26) | 0.98 (0.46-2.05) |
| Bisexual women | 0.93 (0.61-1.43) | 1.08 (0.78-1.48) | 1.64 (1.03-2.60)b |
| Men, unknown sexual orientation | 0.53 (0.20-1.45) | 2.34 (0.69-7.89) | 1.87 (0.73-4.83) |
| Women, unknown sexual orientation | 1.07 (0.45-2.50) | 0.62 (0.18-2.18) | 0.47 (0.11-2.14) |
| Heterosexual men | 1.10 (0.85-1.43) | 1.31 (1.04-1.64)b | 1.40 (1.07-1.83)b |
| Heterosexual women | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Race and ethnicityc | |||
| American Indian or Alaska Native | 3.92 (2.09-7.32)b | 9.98 (4.16-23.95)b | 5.49 (2.76-10.92)b |
| Asian | 1.45 (0.61-3.44) | 3.39 (1.07-10.72)b | 2.98 (0.60-14.70) |
| Black | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Hispanic | 2.24 (1.40-3.60)b | 5.13 (2.72-9.66)b | 2.71 (1.55-4.71)b |
| Native Hawaiian or Other Pacific Islander | 1.82 (0.57-5.88) | 6.15 (2.10-17.95)b | 6.56 (1.98-21.68)b |
| White | 3.29 (2.03-5.35)b | 3.98 (2.43-6.52)b | 3.80 (2.15-6.70)b |
| Non-Hispanic, >1 race | 1.87 (0.93-3.80) | 3.47 (1.65-7.30)b | 4.09 (1.83-9.12)b |
| Educational attainment | |||
| <High school education | 1.84 (1.22-2.79)b | 2.80 (1.48-5.32)b | 2.25 (1.13-4.47)b |
| High school diploma | 1.68 (1.10-2.58)b | 2.60 (1.46-4.63)b | 2.22 (1.19-4.13)b |
| Some college courses | 1.32 (0.88-1.97) | 2.10 (1.23-3.57)b | 1.97 (1.12-3.46)b |
| ≥College degree | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Annual household income, $ | |||
| <20 000 | 1.47 (1.05-2.06)b | 1.77 (1.28-2.45)b | 1.22 (0.82-1.80) |
| 20 000-49 999 | 1.25 (0.96-1.62) | 1.52 (1.07-2.18)b | 1.08 (0.73-1.60) |
| 50 000-74 999 | 1.02 (0.73-1.42) | 1.44 (0.95-2.16) | 1.08 (0.64-1.82) |
| ≥75 000 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Health insurance | |||
| Private only | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Uninsured | 1.60 (1.20-2.12)b | 1.93 (1.37-2.72)b | 1.76 (1.17-2.66)b |
| Medicaid only | 1.87 (1.44-2.46)b | 2.51 (1.76-3.58)b | 1.46 (0.97-2.19) |
| Other | 1.88 (1.40-2.54)b | 1.52 (0.97-2.38) | 1.21 (0.79-1.85) |
| No. of times moved in past year | |||
| 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1 | 1.27 (0.95-1.71) | 1.06 (0.82-1.36) | 1.54 (1.04-2.29)b |
| 2 | 1.07 (0.72-1.60) | 1.50 (1.14-1.98)b | 1.63 (1.15-2.33)b |
| 3 | 1.07 (0.79-1.47) | 1.55 (1.11-2.18)b | 3.02 (2.25-4.05)b |
| MSA status | |||
| Large MSA | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Small MSA | 1.15 (0.89-1.50) | 1.06 (0.82-1.38) | 2.10 (1.61-2.76)b |
| Nonmetropolitan area | 1.13 (0.89-1.45) | 0.97 (0.74-1.26) | 1.35 (1.01-1.79)b |
| Probation or parole in past year | |||
| Yes | 1.99 (1.45-2.72)b | 4.26 (3.25-5.58)b | 2.74 (2.02-3.72)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| HIV/AIDS | |||
| Yes | 1.60 (0.50-5.09) | 4.50 (2.60-7.80)b | 3.36 (1.45-7.79)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| HBV or HCV | |||
| Yes | 1.95 (1.12-3.42)b | 1.00 (0.55-1.84) | 2.46 (1.66-3.67)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| STI in past year | |||
| Yes | 1.49 (1.01-2.20)b | 1.45 (1.01-2.07)b | 1.56 (1.05-2.33)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| MDE in past year | |||
| Yes | 0.87 (0.65-1.15) | 1.58 (1.19-2.12)b | 1.04 (0.70-1.54) |
| Did not answer | 1.43 (0.73-2.83) | 0.82 (0.27-2.51) | 2.54 (1.15-5.62)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Serious thoughts of suicide in past year | |||
| Yes | 1.41 (1.02-1.97)b | 1.62 (1.09-2.41)b | 1.70 (1.20-2.40)b |
| Did not answer | 2.64 (1.26-5.51)b | 1.96 (0.60-6.45) | 0.85 (0.31-2.32) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Nicotine dependence in past month | |||
| Yes | 1.89 (1.49-2.38)b | 2.08 (1.56-2.78)b | 1.87 (1.37-3.54)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Cannabis use disorder or daily/near daily use of cannabis in past year | |||
| Yes | 3.02 (2.09-4.36)b | 3.18 (2.15-4.71)b | 1.58 (1.05-2.36)b |
| No, but past year use | 3.25 (2.31-4.59)b | 3.27 (2.17-4.93)b | 2.19 (1.61-2.98)b |
| No past year use | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Cocaine use in past year | |||
| Yes | 3.39 (2.43-4.73)b | 2.37 (1.76-3.18)b | 0.98 (0.65-1.49) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Hallucinogen use in past year | |||
| Yes | 1.79 (1.33-2.42)b | 1.36 (1.04-1.79)b | 2.05 (1.38-3.04)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Heroin use or prescription opioid misuse in past year | |||
| Yes | 2.18 (1.60-2.96)b | 2.31 (1.78-3.00)b | 3.40 (2.13-5.41)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Prescription tranquilizer or sedative misuse in past year | |||
| Yes | 1.34 (0.98-1.82) | 1.73 (1.30-2.32)b | 1.29 (0.90-1.85) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Prescription stimulant misuse in past year | |||
| Yes | 1.53 (1.16-2.03)b | 1.38 (0.98-1.94) | 2.12 (1.33-3.39)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Heroin injection in past year | |||
| Yes | 1.14 (0.66-1.94) | 0.55 (0.25-1.21) | 9.97 (6.43-15.47)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
Abbreviations: ARR, adjusted risk ratio; HBV, hepatitis B virus; HCV, hepatitis C virus; MDE, major depressive episode; MSA, metropolitan statistical area; MUD, methamphetamine use disorder; NSDUH, National Survey on Drug Use and Health; STI, sexually transmitted infection.
Data source: the 2015 to 2019 NSDUH.4 The final multivariable multinomial logistic regression model included the variables presented in this table. Alcohol use and use disorder were not associated with any of the outcomes and thus were removed from the final model. Bivariable multinomial logistic regression results are presented in the eTable in the Supplement.
Each estimate was statistically significantly different from the estimate of the reference group within the same cell.
Race and ethnicity was the NSDUH respondent’s self-classification of racial and ethnic origin based on the classifications developed by the US Census Bureau.
The adjusted prevalence of methamphetamine use without MUD or injection was higher among those with an educational level of high school or less vs those with a college degree (0.40%-0.44% vs 0.24%; ARR, 1.68-1.84; 95% CI, 1.10-2.79), those with an annual household income less than $20 000 vs those with an income of $75 000 or more (0.42% vs 0.28%; ARR, 1.47; 95% CI, 1.05-2.06), Medicaid-only beneficiaries and uninsured adults vs those with private-only insurance (0.39%-0.46% vs 0.25%; ARR, 1.60-1.87; 95% CI, 1.20-2.46), and those with past-year probation or parole status vs those without (0.65% vs 0.33%; ARR, 1.99; 95% CI, 1.45-2.72). It was also higher among those with vs those without HBV or HCV (0.65% vs 0.33%; ARR, 1.95; 95% CI, 1.12-3.42); those with past-year suicidal ideation vs those without (0.46% vs 0.32%; ARR, 1.41; 95% CI, 1.02-1.97); and those with nicotine dependence, cannabis use, cocaine use, hallucinogen use, opioid misuse, and prescription stimulant use vs those without (0.50%-0.91% vs 0.19%-0.32%; ARR, 1.53-3.39; 95% CI, 1.16-4.73).
Adjusted Prevalence and Correlates of MUD Without Injection
The adjusted prevalence of MUD without injection (Table 2 and Table 3) was lower in 2015 to 2016 than in 2019 (0.20%-0.28% vs 0.41%; ARR, 0.50-0.69; 95% CI, 0.36-0.98) and was higher among heterosexual men than heterosexual women (0.35% vs 0.27%; ARR, 1.31; 95% CI, 1.04-1.64); Hispanic, American Indian or Alaska Native, Asian, White, and Native Hawaiian or Other Pacific Islander individuals as well as those who reported being non-Hispanic individuals with more than 1 race vs Black individuals (0.29%-0.86% vs 0.09%; ARR, 3.47-9.98; 95% CI, 1.07-23.95); those who moved twice or more in the past year vs those who did not move (0.43%-0.45% vs 0.29%; ARR, 1.50-1.55; 95% CI, 1.11-2.18); and those with past-year probation or parole status vs without (1.09% vs 0.26%; ARR, 4.26; 95% CI, 3.25-5.58). The adjusted prevalence was higher among those with vs those without HIV/AIDS (1.40% vs 0.31%; ARR, 4.50; 95% CI, 2.60-7.80); past-year major depressive episode vs those without (0.46% vs 0.29%; ARR, 1.58; 95% CI, 1.19-2.12); past-year suicidal ideation vs those without (0.47% vs 0.29%; ARR, 1.62; 95% CI, 1.09-2.41); and those with nicotine dependence, cannabis use, cocaine use, hallucinogen use, opioid misuse, and prescription tranquilizer or sedative misuse vs those without (0.42%-0.64% vs 0.17%-0.31%; ARR, 1.36-3.27; 95% CI, 1.04-4.93).
Increases in Adjusted Past-Year Prevalence of MUD Without Injection by Age, Sex and Sexual Orientation, and Race and Ethnicity
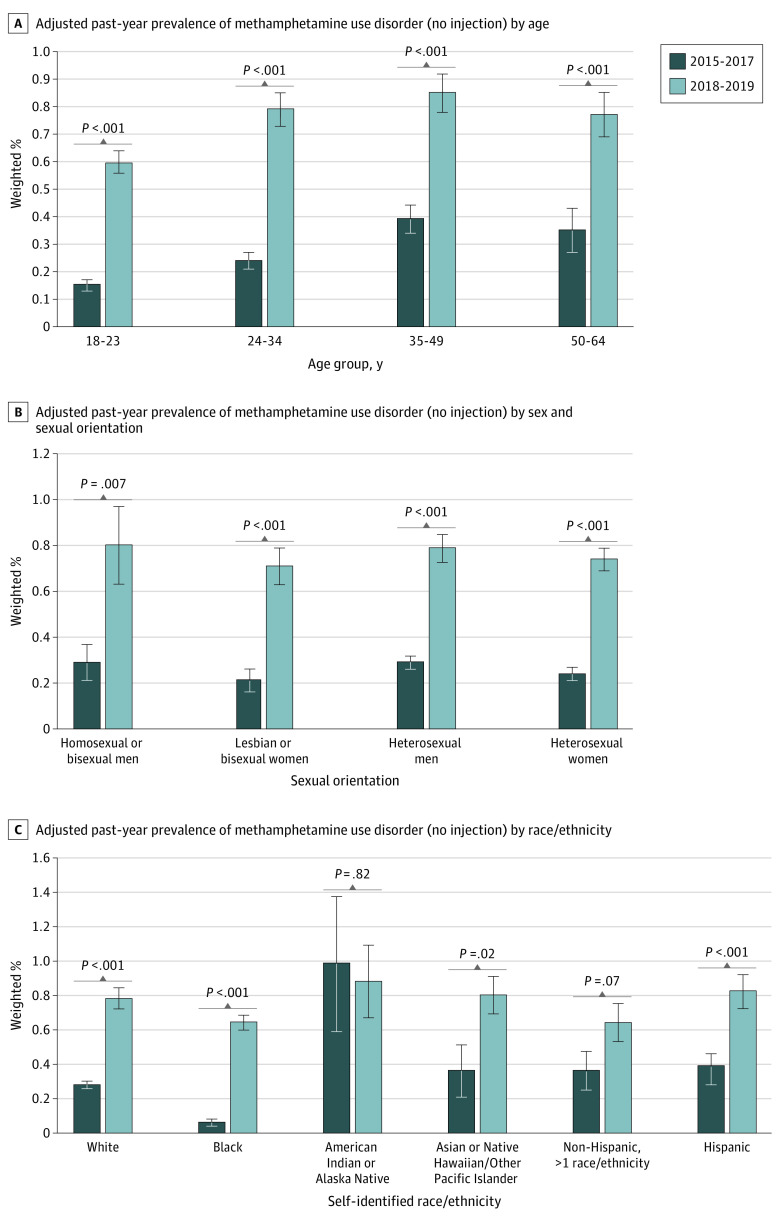
We combined years of data for reliable estimates. Between 2015 to 2017 and 2018 to 2019, the adjusted prevalence of MUD without injection increased 300% among those aged 18 to 23 years (from 0.15% to 0.60%; P < .001), 229% among those aged 24 to 34 years (from 0.24% to 0.79%; P < .001), 118% among those aged 35 to 49 years (from 0.39% to 0.85%; P < .001), and 120% among those aged 50 to 64 years (from 0.35% to 0.77%; P < .001) (Figure, A). The adjusted prevalence of MUD without injection also increased 176% among homosexual or bisexual men (from 0.29% to 0.80%; P = .007), 238% among lesbian or bisexual women (from 0.21% to 0.71%; P < .001), 172% among heterosexual men (from 0.29% to 0.79%; P < .001), and 208% among heterosexual women (from 0.24% to 0.74%; P < .001) (Figure, B). In addition, past-year prevalence increased 110% among Hispanic individuals (from 0.39% to 0.82%; P < .001), 122% among Asian or Native Hawaiian or Other Pacific Islander individuals (from 0.36% to 0.80%; P = .018), 179% among White individuals (from 0.28% to 0.78%; P < .001), and 967% among Black individuals (from 0.06% to 0.64%; P < .001) (Figure, C).
Figure. Methamphetamine Use Disorder Among US Adults Aged 18 to 64 Years.
Data were obtained from the 2015 to 2019 National Surveys on Drug Use and Health.4 Each estimate was adjusted for the following variables: age, sex and sexual orientation, self-reported race/ethnicity, educational attainment, annual household income, health insurance, housing instability, metropolitan statistical area status, probation or parole status, HIV/AIDS, hepatitis B or C virus, sexually transmitted infection, major depressive episode, serious thoughts of suicide, nicotine dependence, co-occurring use of other drugs and misuse of psychotherapeutic prescriptions, and heroin injection. Error bars indicate SEs.
Adjusted Prevalence and Correlates of Injection
The adjusted prevalence of methamphetamine injection was higher among homosexual men, heterosexual men, and bisexual women than among heterosexual women (0.21%-0.55% vs 0.15%; ARR, 1.40-3.66; 95% CI, 1.03-6.16) (Table 2 and Table 3). Adjusted prevalence was also higher among American Indian or Alaska Native, Hispanic, Native Hawaiian or Other Pacific Islander, and White individuals as well as non-Hispanic individuals who reported more than 1 race and ethnicity than among Black individuals (0.16%-0.39% vs 0.06%; ARR, 2.71-6.56; 95% CI, 1.55-21.68) and among those residing in small and nonmetropolitan statistical areas than among those residing in large metropolitan statistical areas (0.20%-0.32% vs 0.15%; ARR, 1.35-2.10; 95% CI, 1.01-2.76). The prevalence of injection was higher among those with vs without HIV/AIDS (0.65% vs 0.19%; ARR, 3.36; 95% CI, 1.45-7.79); those with past-year suicidal ideation vs those without (0.30% vs 0.18%; ARR, 1.70; 95% CI, 1.20-2.40); and those with nicotine dependence, cannabis use, hallucinogen use, opioid misuse, prescription stimulant misuse vs those without (0.22%-0.39% vs 0.12%-0.18%; ARR, 1.58-3.40; 95% CI, 1.05-5.41), and heroin injection vs those without (1.38% vs 0.14%; ARR, 9.97; 95% CI, 6.43-15.47).
Adjusted Prevalence and Correlates of Frequent Use
Among those with any past-year methamphetamine use, the adjusted prevalence of frequent methamphetamine use was lower in 2015 than in 2019 (41.56% vs 50.44%; ARR, 0.82; 95% CI, 0.68-0.99) (Table 4). The adjusted prevalence was higher among those aged 35 to 64 years (46.47%-55.74% vs 34.75%; ARR, 1.34-1.60; 95% CI, 1.09-2.08) compared with those aged 18 to 23 years, among those with HBV or HCV and those with sexually transmitted infection compared with those without such infections (56.76%-57.94% vs 43.69%-43.91%; ARR, 1.29-1.33; 95% CI, 1.09-1.60), and among those with hallucinogen use compared with those without (54.65% vs 42.70%; ARR, 1.28; 95% CI, 1.12-1.47). In addition, adjusted prevalence was higher among those with MUD or injection compared with those with methamphetamine use but without MUD or injection (52.68%-53.84% vs 32.59%; ARR, 1.62-1.65; 95% CI, 1.35-1.94).
Table 4. Correlates of Past-Year Frequent Methamphetamine Use Among Adults Aged 18-64 Yearsa .
| Correlate | Adjusted prevalence of frequent (≥100 d in past 12 mo) methamphetamine use, weighted % (95% CI) | Frequent (≥100 d in past 12 mo) methamphetamine use, ARR (95% CI) |
|---|---|---|
| NSDUH year | ||
| 2015 | 41.56 (25.55-47.83)b | 0.82 (0.68-0.99)b |
| 2016 | 43.90 (37.18-50.85) | 0.87 (0.71-1.06) |
| 2017 | 42.40 (35.15-49.99) | 0.84 (0.70-1.01) |
| 2018 | 45.97 (39.55-52.53) | 0.91 (0.76-1.10) |
| 2019 | 50.44 (43.09-57.76) | 1 [Reference] |
| Age group, y | ||
| 18-23 | 34.75 (28.41-41.68) | 1 [Reference] |
| 24-34 | 41.19 (36.34-46.22) | 1.19 (0.97-1.45) |
| 35-49 | 46.47 (41.13-51.89)b | 1.34 (1.09-1.64)b |
| 50-64 | 55.74 (46.10-64.96)b | 1.60 (1.24-2.08)b |
| HBV or HCV | ||
| Yes | 57.94 (47.65-67.58)b | 1.33 (1.10-1.60)b |
| No | 43.69 (39.78-47.68) | 1 [Reference] |
| STI in past year | ||
| Yes | 56.76 (48.29-64.85)b | 1.29 (1.09-1.54)b |
| No | 43.91 (39.83-48.08) | 1 [Reference] |
| MDE in past year | ||
| Yes | 40.04 (33.93-46.48)b | 0.84 (0.71-0.99)b |
| Did not answer | 30.89 (16.86-49.62) | 0.65 (0.38-1.10) |
| No | 47.56 (43.24-51.92) | 1 [Reference] |
| Alcohol use and use disorder in past year | ||
| Alcohol use disorder | 34.96 (28.38-42.18)b | 0.74 (0.60-0.92)b |
| No alcohol use disorder, but had alcohol use | 48.91 (44.23-53.60) | 1.04 (0.89-1.20) |
| No alcohol use | 47.19 (40.85-53.62) | 1 [Reference] |
| Cocaine use in past year | ||
| Yes | 33.48 (27.89-39.57)b | 0.66 (0.55-0.80)b |
| No | 50.45 (45.88-55.02) | 1 [Reference] |
| Hallucinogen use in past year | ||
| Yes | 54.65 (48.36-60.79)b | 1.28 (1.12-1.47)b |
| No | 42.70 (38.51-47.01) | 1 [Reference] |
| Methamphetamine use, MUD, or injection in past year | ||
| Use without MUD or injection | 32.59 (28.12-37.41) | 1 [Reference] |
| MUD without injection | 53.84 (47.82-59.76)b | 1.65 (1.42-1.92)b |
| Injection regardless of MUD | 52.68 (45.50-59.75)b | 1.62 (1.35-1.94)b |
Abbreviations: ARR, adjusted risk ratio; HBV, hepatitis B virus; HCV, hepatitis C virus; MDE, major depressive episode; MUD, methamphetamine use disorder; NSDUH, National Survey on Drug Use and Health; STI, sexually transmitted infection.
Data source: the 2015 to 2019 NSDUH.4
Each estimate was statistically significantly different from the estimate of the reference group within the same cell. The final multivariable multinomial logistic regression model included all of the variables presented in this table. Covariates shown in Table 2 and Table 3, but not in Table 4, were not associated with the outcome and were removed from the final model.
Discussion
Among adults aged 18 to 64 years from 2015 to 2019, we found a substantial increase (180%) in overdose deaths involving psychostimulants other than cocaine (largely methamphetamine), but this increase was considerably larger than the growth in the number of adults who reported past-year methamphetamine use (43%), indicating riskier patterns of methamphetamine use. Similar to previous reports of increases in the combined use of methamphetamine and opioids,5,23,26,27,28,29,30,31 the present study found increasing trends in the number of adults who used both. We also observed a 60% increase in individuals with combined methamphetamine and cocaine use, a 105% increase in those with MUD without injection, and a 66% increase in frequent methamphetamine use. Among those with past-year methamphetamine use, the prevalence of MUD or injection surpassed the prevalence of methamphetamine use without MUD or injection in each year from 2017 to 2019. Moreover, we found that adults with MUD or methamphetamine injection were more likely to use methamphetamine frequently.
Recent studies have reported riskier methamphetamine use patterns, such as injection with fentanyl or heroin,27 preference for fentanyl over heroin,27 and increases in use of heroin with methamphetamine (goofball), and associated morbidity and overdose.31,32 In addition, the increased presence in the illicit drug market of methamphetamine laced with fentanyl may expose people who use methamphetamine and have no tolerance to opioids, which could be a factor in the increase in overdose deaths.33,34 All of these changes in methamphetamine use patterns are associated with increased risk for overdose and other adverse outcomes. Thus, understanding the patterns of higher-risk methamphetamine use, as observed in this study and other recent studies,27,31,32,33,34 may help explain the marked increases in associated overdose deaths during the study periods.
The results also indicated that the populations who used methamphetamine diversified from 2015 to 2019. Many studies have reported a high prevalence of methamphetamine use among men who have sex with men,21,35,36,37 which is a major risk factor for HIV infection.38 Consistently, we found that, from 2015 to 2019, the adjusted prevalence of MUD without injection more than doubled among homosexual or bisexual men. However, this prevalence more than tripled among heterosexual women and lesbian or bisexual women and more than doubled among heterosexual men. Methamphetamine use has historically been prevalent among middle-aged White persons and has been low among Black persons. However, we observed a 300% increase in MUD without injection among those aged 18 to 23 years, an important period of brain development, and 118% to 229% increases among those aged 24 to 64 years; we also found a 10-fold increase in MUD without injection among Black persons. Increases in MUD without injection were observed among most racial and ethnic minority groups, nearly tripled among White persons, and more than doubled among Asian/Native Hawaiian or Other Pacific Islander persons as well as among Hispanic persons. The prevalence remained high but unchanged among non-Hispanic American Indian or Alaska Native persons.
Results from the present study help explain the more-than-doubled increase in psychostimulant-involved overdose deaths among adults aged 18 to 23 years and the approximately tripled increase among those in the 24- to 34-year, 35- to 49-year, and 50- to 64-year age groups during the study periods (from our additional analysis) as well as the results of a previous study that found Black men had the fastest increases in psychostimulant-involved overdose death rates among men during 2011 to 2018 and that rates increased for all examined racial/ethnic groups.2 These results were also consistent with increases in methamphetamine-associated treatment admissions among American Indian or Alaska Native, Black, Hispanic, and White patients from 2007 to 2018, with the fastest increase among Black patients.9
The results of the present study suggest that implementing evidence-based prevention and treatment interventions that target racially and ethnically diverse populations is urgently needed. In addition, given that fentanyl-contaminated methamphetamine is associated with the increase in methamphetamine overdose, prevention interventions that include access to drug-checking services, such as fentanyl test strips, may be useful.39
Understanding the correlates of methamphetamine use, frequent use, MUD, and injection is of value in guiding the strategies for addressing the root causes of the recent surge in methamphetamine overdose deaths. The results highlighted key risk factors, including lower educational attainment, lower annual household income, lack of insurance, housing instability, criminal justice involvement, comorbidities (eg, HIV/AIDS, HBV or HCV, sexually transmitted infection, or major depressive episode), suicidal ideation, and polysubstance use. Co-use of opioids (knowingly or unknowingly) is a particularly important factor given the increasing overlap of synthetic opioids (ie, fentanyl-related agents) with methamphetamine-involved overdose deaths.40
Given the indicators of the growth of methamphetamine use during the COVID-19 pandemic,41 the prevalence of MUD and injection may have further accelerated during 2020 to 2021. Moreover, estimates of overdose deaths did not include most people who died from methamphetamine-associated health problems (eg, stroke, myocardial infarction, pulmonary hypertension, HIV/AIDS, or HBV or HCV). Thus, methamphetamine-associated mortality and harms are likely to be markedly underestimated when considering only overdose deaths.
A major challenge in addressing the high rates of methamphetamine-associated morbidity and mortality is the lack of US Food and Drug Administration–approved medications for MUD treatment, highlighting the urgency for further research and investments in MUD medication development. Studies on implementation of evidence-based prevention interventions and on public policies are needed to inform the response to the surge in methamphetamine use and associated adverse outcomes. For example, expansion of community-based interventions to reduce injection drug use–associated harms and overdoses, such as comprehensive Syringe Services Programs, could help mitigate overdose risks and the additional spread of infectious diseases, such as HBV or HCV and HIV.
Limitations
This study has several limitations. First, the cross-sectional nature of NSDUH data precludes drawing causal inferences. Second, this study may have underestimated the prevalence of methamphetamine use, MUD, injection, and use frequency because the NSDUH excluded people who were experiencing homelessness and not living in shelters as well as those who were institutionalized (eg, in jail or prison) who tend to have more drug use and may have a higher risk of methamphetamine overdose deaths than the general population.42,43,44,45 Third, the NSDUH is a self-reported survey and thus is subject to recall and social desirability bias. Fourth, approximately 85% to 90% of death certificates involving psychostimulants other than cocaine mentioned methamphetamine.46 We may have underestimated the mortality rate because some overdose death certificates did not report the specific drugs involved (eg, 6% in 2019).1 When additional years of NSDUH data are available on adults with past-year methamphetamine use, further analyses are needed to examine the difference between persons with MUD or injection and persons with methamphetamine use without MUD or injection.
Conclusions
Among US adults aged 18 to 64 years during 2015 to 2019, we found upward trends in methamphetamine use and MUD as well as psychostimulant-involved overdose deaths with or without opioids or cocaine. The prevalence of MUD or methamphetamine injection surpassed the prevalence of methamphetamine use without MUD or injection in each year from 2017 to 2019. Adults with MUD or who injected methamphetamine were more likely to use methamphetamine frequently. We detected upward trends in frequent use that were driven by those with methamphetamine use (without MUD or injection) or with MUD (without injection). Subgroups showed notable trends, including increases in MUD without injection by heterosexual men and women, homosexual or bisexual men, and lesbian or bisexual women as well as by individuals with Hispanic and non-Hispanic Asian or Native Hawaiian or Other Pacific Islander, Black, or White race/ethnicity. Populations at higher risk for methamphetamine use diversified rapidly, particularly those with socioeconomic risk factors and more comorbidities. These changes in methamphetamine use patterns increase the risks for overdose and other adverse outcomes. Combating the surges in methamphetamine use, MUD, and associated mortality warrants the implementation of evidence-based prevention and treatment interventions.
eTable. Bivariable Multinomial Logistic Regression Results Show Correlates of Past-Year Methamphetamine Use, Use Disorder, and Injection Among Adults Aged 18-64 in the U.S. (N = 195,711)
References
- 1.Hedegaard H, Miniño AM, Warner M. Drug Overdose Deaths in the United States, 1999–2019. National Center for Health Statistics, Centers for Disease Control and Prevention. NCHS Data Brief, no 394. Accessed March 8, 2021. https://www.cdc.gov/nchs/products/databriefs/db394.htm
- 2.Han B, Cotto J, Etz K, Einstein EB, Compton WM, Volkow ND. Methamphetamine overdose deaths in the US by sex and race and ethnicity. JAMA Psychiatry. 2021;78(5):564-567. doi: 10.1001/jamapsychiatry.2020.4321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics, Centers for Disease Control and Prevention . Provisional drug overdose death counts. Accessed on April 15, 2021. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- 4.Han B. Key Substance Use and Mental Health Indicators in the United States: Results From the 2019 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. HHS Publication No. PEP20-07-01-001, NSDUH Series H-55.
- 5.Ellis MS, Kasper ZA, Cicero TJ. Twin epidemics: the surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend. 2018;193:14-20. doi: 10.1016/j.drugalcdep.2018.08.029 [DOI] [PubMed] [Google Scholar]
- 6.Mei DS, Cai YJ, Wang FM, et al. Reciprocal substitution between methamphetamine and heroin in terms of reinforcement effects in rats. Front Psychiatry. 2020;11:750. doi: 10.3389/fpsyt.2020.00750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palamar JJ, Han BH, Keyes KM. Trends in characteristics of individuals who use methamphetamine in the United States, 2015-2018. Drug Alcohol Depend. 2020;213:108089. doi: 10.1016/j.drugalcdep.2020.108089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones CM, Underwood N, Compton WM. Increases in methamphetamine use among heroin treatment admissions in the United States, 2008-17. Addiction. 2020;115(2):347-353. doi: 10.1111/add.14812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones CM, Olsen EO, O’Donnell J, Mustaquim D. Resurgent methamphetamine use at treatment admission in the United States, 2008-2017. Am J Public Health. 2020;110(4):509-516. doi: 10.2105/AJPH.2019.305527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003-2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388-395. doi: 10.15585/mmwr.mm6817a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration . National Survey on Drug Use and Health (NSDUH). Accessed February 21, 2021. https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health
- 12.National Center for Health Statistics . National Vital Statistics System: mortality statistics. Accessed March 8, 2021. https://www.cdc.gov/nchs/nvss/deaths.htm
- 13.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293-301. doi: 10.7326/M17-0865 [DOI] [PubMed] [Google Scholar]
- 14.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878. doi: 10.1542/peds.2016-1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shiffman S, Waters A, Hickcox M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6(2):327-348. doi: 10.1080/1462220042000202481 [DOI] [PubMed] [Google Scholar]
- 16.Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC. Discrepancies in estimates of prevalence and correlates of substance use and disorders between two national surveys. Addiction. 2007;102(4):623-629. doi: 10.1111/j.1360-0443.2007.01745.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C. A clinical validation of the National Survey on Drug Use and Health assessment of substance use disorders. Addict Behav. 2008;33(6):782-798. doi: 10.1016/j.addbeh.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 18.Substance Abuse and Mental Health Services Administration . Reliability of Key Measures in the National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration; 2010. Office of Applied Studies Methodology Series M-8. HHS Publication No. SMA 09-4425. [PubMed] [Google Scholar]
- 19.Han B, Compton WM, Gfroerer J, McKeon R. Prevalence and correlates of past 12-month suicide attempt among adults with past-year suicidal ideation in the United States. J Clin Psychiatry. 2015;76(3):295-302. doi: 10.4088/JCP.14m09287 [DOI] [PubMed] [Google Scholar]
- 20.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text revision. American Psychiatric Association; 2000. [Google Scholar]
- 21.Fletcher JB, Swendeman D, Reback CJ. Mental health and substance use disorder comorbidity among methamphetamine-using men who have sex with men. J Psychoactive Drugs. 2018;50(3):206-213. doi: 10.1080/02791072.2018.1447173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuo CJ, Liao YT, Chen WJ, Tsai SY, Lin SK, Chen CC. Causes of death of patients with methamphetamine dependence: a record-linkage study. Drug Alcohol Rev. 2011;30(6):621-628. doi: 10.1111/j.1465-3362.2010.00255.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shearer RD, Howell BA, Bart G, Winkelman TNA. Substance use patterns and health profiles among US adults who use opioids, methamphetamine, or both, 2015-2018. Drug Alcohol Depend. 2020;214:108162. doi: 10.1016/j.drugalcdep.2020.108162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howell BA, Bart G, Wang EA, Winkelman TNA. Service involvement across multiple sectors among people who use opioids, methamphetamine, or both, United States-2015-2018. Med Care. 2021;59(3):238-244. doi: 10.1097/MLR.0000000000001460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618-623. doi: 10.1093/aje/kwp440 [DOI] [PubMed] [Google Scholar]
- 26.Bonk R, Miller RJ, Lanter J, Niblo C, Kemp J, Shelton J. Accidental overdose deaths in Oklahoma, 2002-2017: opioid and methamphetamine trends. J Anal Toxicol. 2020;44(7):672-678. doi: 10.1093/jat/bkaa068 [DOI] [PubMed] [Google Scholar]
- 27.Daniulaityte R, Silverstein SM, Crawford TN, et al. Methamphetamine use and its correlates among individuals with opioid use disorder in a Midwestern U.S. city. Subst Use Misuse. 2020;55(11):1781-1789. doi: 10.1080/10826084.2020.1765805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strickland JC, Havens JR, Stoops WW. A nationally representative analysis of “twin epidemics”: rising rates of methamphetamine use among persons who use opioids. Drug Alcohol Depend. 2019;204:107592. doi: 10.1016/j.drugalcdep.2019.107592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McMahan VM, Kingston S, Newman A, Stekler JD, Glick SN, Banta-Green CJ. Interest in reducing methamphetamine and opioid use among syringe services program participants in Washington State. Drug Alcohol Depend. 2020;216:108243. doi: 10.1016/j.drugalcdep.2020.108243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Tayyib A, Koester S, Langegger S, Raville L. Heroin and methamphetamine injection: an emerging drug use pattern. Subst Use Misuse. 2017;52(8):1051-1058. doi: 10.1080/10826084.2016.1271432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glick SN, Klein KS, Tinsley J, Golden MR. Increasing heroin-methamphetamine (goofball) use and related morbidity among Seattle area people who inject drugs. Am J Addict. 2021;30(2):183-191. doi: 10.1111/ajad.13115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Glick SN, Burt R, Kummer K, Tinsley J, Banta-Green CJ, Golden MR. Increasing methamphetamine injection among non-MSM who inject drugs in King County, Washington. Drug Alcohol Depend. 2018;182:86-92. doi: 10.1016/j.drugalcdep.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tupper KW, McCrae K, Garber I, Lysyshyn M, Wood E. Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug Alcohol Depend. 2018;190:242-245. doi: 10.1016/j.drugalcdep.2018.06.020 [DOI] [PubMed] [Google Scholar]
- 34.Park JN, Rashidi E, Foti K, Zoorob M, Sherman S, Alexander GC. Fentanyl and fentanyl analogs in the illicit stimulant supply: results from U.S. drug seizure data, 2011-2016. Drug Alcohol Depend. 2021;218:108416. doi: 10.1016/j.drugalcdep.2020.108416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hussen SA, Camp DM, Jones MD, et al. Exploring influences on methamphetamine use among Black gay, bisexual and other men who have sex with men in Atlanta: a focus group study. Int J Drug Policy. 2021;90:103094. doi: 10.1016/j.drugpo.2020.103094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rivera AV, Harriman G, Carrillo SA, Braunstein SL. Trends in methamphetamine use among men who have sex with men in New York City, 2004-2017. AIDS Behav. 2021;25(4):1210-1218. doi: 10.1007/s10461-020-03097-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fletcher JB, Swendeman D, Reback CJ. Associations between major depressive episode, methamphetamine use disorder severity, and engagement in sexual risk-taking among methamphetamine-using men who have sex with men. AIDS Behav. 2018;22(5):1461-1466. doi: 10.1007/s10461-017-1974-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grov C, Westmoreland D, Morrison C, Carrico AW, Nash D. The crisis we are not talking about: one-in-three annual HIV seroconversions among sexual and gender minorities were persistent methamphetamine users. J Acquir Immune Defic Syndr. 2020;85(3):272-279. doi: 10.1097/QAI.0000000000002461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beaulieu T, Wood E, Tobias S, et al. Is expected substance type associated with timing of drug checking service utilization?: a cross-sectional study. Harm Reduct J. 2021;18(1):66. doi: 10.1186/s12954-021-00514-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010-2016. JAMA. 2018;319(17):1819-1821. doi: 10.1001/jama.2018.2844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wainwright JJ, Mikre M, Whitley P, et al. Analysis of drug test results before and after the US declaration of a national emergency concerning the COVID-19 outbreak. JAMA. 2020;324(16):1674-1677. doi: 10.1001/jama.2020.17694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Passaro RC, Ramsey K, Segura ER, et al. Speed kills: associations between methamphetamine use, HIV infection, tobacco use, and accelerated mortality among gay and bisexual men in Los Angeles, CA 20years after methamphetamine dependence treatment. Drug Alcohol Depend. 2019;195:164-169. doi: 10.1016/j.drugalcdep.2018.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Compton WM, Dawson D, Duffy SQ, Grant BF. The effect of inmate populations on estimates of DSM-IV alcohol and drug use disorders in the United States. Am J Psychiatry. 2010;167(4):473-474. doi: 10.1176/appi.ajp.2009.09081087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferguson KM, Bender K, Thompson SJ. Gender, coping strategies, homelessness stressors, and income generation among homeless young adults in three cities. Soc Sci Med. 2015;135:47-55. doi: 10.1016/j.socscimed.2015.04.028 [DOI] [PubMed] [Google Scholar]
- 45.Reuter P, Caulkins JP, Midgette G. Heroin use cannot be measured adequately with a general population survey. Addiction. Published online March 2, 2021. doi: 10.1111/add.15458 [DOI] [PubMed] [Google Scholar]
- 46.Drug Enforcement Administration, US Department of Justice . 2018. National Drug Threat Assessment. DEA-DCT-DIR-032-18. Accessed April 15, 2021. https://www.dea.gov/sites/default/files/2018-11/DIR-032-18%202018%20NDTA%20final%20low%20resolution.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Bivariable Multinomial Logistic Regression Results Show Correlates of Past-Year Methamphetamine Use, Use Disorder, and Injection Among Adults Aged 18-64 in the U.S. (N = 195,711)