Highlights
-
•
A bidirectional relationship exists between physical activity and mental health.
-
•
During COVID-19, physical activity and mental health status varied by demographic.
-
•
Physical activity can be a protective factor against deteriorating mental health.
Keywords: COVID-19, Physical activity, Mental health, Rural health
Abstract
The objectives of this paper are to investigate: 1) how the COVID-19 pandemic influenced both physical activity practices and mental health status, and 2) to assess the relationship between the two. Our mixed-methods study draws on 4,026 online survey responses collected between April – September 2020 across five states (Louisiana, Montana, North Carolina, Oregon and West Virginia). Logistic regression models were run for two outcome variables (physical activity and mental health status (measured using the Kessler Psychological Distress scale)). Researchers controlled for race/ethnicity, household income/size, gender, urbanicity, education, employment, use of government assistance and presence of chronic health conditions. Qualitative analysis was applied to open-ended survey responses to contextualize quantitative findings. Household income was significant in predicting difficulty maintaining pre-pandemic physical activity levels; pre-pandemic physical activity levels were associated with increased psychological distress levels during COVID-19; and race/ethnicity, income status and urbanicity were significantly associated with deteriorating mental health status and physical activity levels during COVID-19. Data suggests that a bi-directional, cyclical relationship between physical activity and mental health exists. Policy implications should include physical activity promotion as a protective factor against declining mental health.
1. Introduction
On March 11, 2020, the World Health Organization declared the novel coronavirus (COVID-19) outbreak a global pandemic. COVID-19 upended daily life and presented the world with ongoing physical and mental health (MH) challenges. In the U.S, by April 2020, 43 states had implemented stay-at-home orders as nationwide average cases were on the rise (on April 10, 2020 for example, the US experienced a new high of 33,473 new COVID-19 cases per day) (Jordan, 2021, Sen et al., 2020). To limit the spread of COVID-19 and protect the public’s health, these orders closed schools, businesses, organizations, and even parks.
Shortly after stay-at-home orders were implemented, studies reported declining MH outcomes for U.S. adults. A cross-sectional survey in June 2020 observed that 41% of adults reported at least 1 adverse mental or behavioral health condition (Czeisler et al., 2020). These outcomes were higher among young adults (74.9%), Hispanic/Latino populations (52.1%), those without a high school diploma (66.2%), and essential workers (54.0%). COVID-19 has had a deleterious impact on MH, with particularly harmful outcomes for historically oppressed groups (Czeisler et al., 2020, Liu and Modir, 2006, Chen et al., 2020).
Research has demonstrated that physical activity (PA) could be protective for MH. PA (Jordan, 2021) is linked with antidepressant effects and a relationship to improved MH (Schuch et al., 2018, Kandola et al., 2019, White et al., 2017). MH is defined as a positive state of well-being, allowing individuals to realize their potential, experience positive emotions, cope with stress, contribute as citizens, maintain interpersonal relationships, and work productively (White et al., 2017). Additionally, there is a dose–response relationship between PA and MH, where those with motivation to engage in higher levels of PA had a lower likelihood of developing depression, regardless of gender and geographic location (Schuch et al., 2018).
Given pre-pandemic research on the connections between PA and MH, this study investigated how COVID-19 influenced both PA practices and MH status, and assessed the relationship between the two. This mixed-methods study investigated the directionality of this relationship as well as how and why changes have occurred. Researchers have increasingly called for intersectional approaches to public health research and practice, recognizing that health is shaped by a convergence of factors, including histories of oppression, experiences of discrimination, poverty, and social location (Tipirneni, 2021, Andress et al., 2020, Bowleg, 2020, Cook et al., 2014, Meyer et al., 2014). Given this context, the relationship between PA and MH should be examined for intersections between location, time, access, and identities (Tipirneni, 2021).
2. Methods
The COVID-19 Food Security Survey, designed by researchers at Montana State University with input from research team members, was administered electronically using Qualtrics across five states (Louisiana, Montana, North Carolina, Oregon, West Virginia) from April – September 2020. Within this timeframe, US COVID-19 deaths passed the 100,000 mark (on May 28, 2020), while the total number of infections surpassed 3 million (on July 7, 2020); vaccines had not yet been approved, but Moderna, Pfizer and BioNTech were in the process of their Phase 3 Trials (July – September 2020). States were selected based on geographic diversity, racial/ethnic breakdown, political leaning, persistent poverty, and SNAP participation rates.
The survey had 52 questions and included a mix of multiple choice, matrix, Likert scale, and open-ended. There were five categories of questions: demographics, economic security, food security, health conditions, and health behaviors. A cross-sectional convenience sample was utilized to recruit participants over 18 years of age, drawing on partnerships with organizations like Cooperative Extension, SNAP-Ed, health departments, and WIC. Participation incentives varied by state.
Quantitative analysis focused on two unique outcome variables: 1) the change in participants’ PA levels before and during the pandemic and 2) the change in participants’ psychological distress levels before and during the pandemic. For the first variable, survey respondents were asked, “The COVID-19 pandemic has made it _____________ for me to get the same amount of physical activity as before.” Response options included: 1) A little more challenging than usual, 2) A lot more challenging than usual, 3) Less challenging than usual, 4) No more challenging than usual, and 5) Prefer not to answer. The second outcome variable describes the change in distress levels before and during the pandemic using the Kessler Psychological Distress (K6) scale. Respondents were asked to think about the K6 questions retrospectively to gauge their level of distress before the pandemic, while their level of distress during the pandemic was measured at the point (between April 2020 and September 2020) that they took the survey. K6 is a brief screening tool for psychological distress in adults (Furukawa et al., 2003, Kessler et al., 2002, Kessler et al., 2003) and is a strong predictor of serious MH issues (Kessler et al., 2002, Kessler et al., 2003).
Researchers controlled for race/ethnicity, household income and size, gender, urbanicity (using Rural Urban Commuting Area codes) (USDA ERS - Rural-Urban Commuting Area Codes. Accessed April 12, 2021), educational attainment, employment status, receipt of government assistance, and presence of chronic health conditions (overweight/obesity, hypertension, pre-diabetes, type 1, II and/or gestational diabetes, metabolic syndrome, heart disease, lung disease or moderate/severe asthma, kidney disease, liver disease, and immunocompromised). This research received IRB approval from Montana State University (CBS042420-EX).
2.1. Quantitative analysis
Researchers analyzed demographics overall and stratified by state. Descriptive statistics were calculated for average K6 scores before and during COVID-19 and average change in score (K6 during COVID-19 - K6 before COVID-19). Logistic regression models were run for the two unique outcome variables to assess the presence of a bi-directional relationship. These models are utilized to describe the three phases below.
Phase 1: The Impact of Psychological Distress on Maintaining Pre-COVID Physical Activity Levels
A logistic regression model was used to estimate whether participants’ K6 scale during COVID-19 was associated with difficulty maintaining pre-pandemic PA levels. In this equation, difficulty maintaining PA level (more difficult versus same or less difficult) is the outcome of interest, represented by y. The primary predictor (K6 scale during COVID-19) and covariates (race/ethnicity, household income, number of household members, gender, urbanicity, education level, employment status, use of government assistance, and chronic health conditions) are included as independent variables, represented by × in the model below. Survey responses that chose “prefer not to answer” were dropped from the study’s model.
Model 1: y (PhysicalActivityLevel) = β0 + β1Race/Ethnicity + β2HouseholdIncome + β2HouseholdMembers + β3Gender + β4Geography (Urban/Rural) + β5EducationLevel + β6EmploymentStatus + β7GovermentAssistance + β8HealthChronicCondition + β9Kessler Score during COVID-19 + ε
Phase 2: The Impact of Lower Physical Activity Levels During COVID on Psychological Distress
Next, because studies have shown a negative feedback loop between PA and MH status, researchers modeled the association between changes in psychological distress levels and PA levels using the same covariates as in Model 1. In this model, the difference in K6 score (K6 score during COVID-19 subtracted by K6 score before COVID-19) is the primary outcome, represented by y. The primary predictor (difficulty maintaining PA levels during COVID-19 -- more difficult versus same or less difficult):
Model 2: y (Change in Kessler Score) = β0 + β1Race/Ethnicity + β2HouseholdIncome + β2HouseholdMembers + β3Gender + β4Geography (Urban/Rural) + β5EducationLevel + β6EmploymentStatus + β7GovermentAssistance + β8HealthChronicCondition + β9PhysicalActivityLevels + ε
Phase 3: The Impact of Negative Change in Psychological Distress (During COVID) on Further Deterioration of Physical Activity Levels
Last, researchers modeled the association between change in K6 score (K6 score during COVID-19 subtracted by K6 score before COVID-19) with difficulty maintaining pre-pandemic PA levels, using the same logistic regression model as described above (Model 1), replacing K6 score during COVID-19 (β9) with change in K6.
Model 3: y (PhysicalActivityLevel) = β0 + β1Race/Ethnicity + β2HouseholdIncome + β3HouseholdMembers + β4Gender + β5Geography (Urban/Rural) + β6EducationLevel + β7EmploymentStatus + β7GovermentAssistance + β8HealthChronicCondition + β9Change in Kessler Score + ε
2.2. Qualitative analysis
Open-ended response questions in the survey were treated as qualitative data. Researchers (xx, xx) analyzed responses to the question, “the reasons that physical activity has or has not been challenging.” Researchers used an iterative process to create a codebook, which included deductive codes based on a review of relevant literature about COVID-19, MH, and barriers/facilitators to PA. Definitions were developed for both inductive and deductive codes. Dedoose software was used by two researchers (xx,xx) (Dedoose Version, 2018, USDA ERS - Rural-Urban Commuting Area Codes. Accessed April 12, 2021) to code the data and generate code frequencies. Illustrative quotes are used to substantiate each of the themes mentioned most often, as well as to contextualize quantitative findings related to the relationship between MH and PA.
3. Results
3.1. Quantitative results
4,026 individuals across five states completed the online survey (see Table 1 for demographic details).
Table 1.
Participant Demographics, Overall and by State.
| All States (n = 4,026) |
Louisiana (n = 875) |
Montana (n = 1,944) |
North Carolina (n = 383) |
Oregon (n = 303) |
West Virginia (n = 521) |
|
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||||
| Female | 3466 (86.37%) | 73 (76.04%) | 1704 (88.02%) | 320 (83.77%) | 272 (89.77%) | 465 (89.25%) |
| Male | 527 (13.13%) | 23 (23.96%) | 222 (11.47%) | 61 (15.97%) | 30 (9.90%) | 53 (10.17%) |
| Other | 20 (0.50%) | 0 (0.00%) | 10 (0.52%) | 1 (0.26%) | 1 (0.33%) | 3 (0.58%) |
| Race | ||||||
| Non-Hispanic White | 3238 (81.32%) | 54 (56.25%) | 1761 (91.43%) | 235 (62.17%) | 159 (54.45%) | 491 (95.16%) |
| Hispanic | 141 (3.54%) | 3 (3.13%) | 25 (1.3%) | 16 (4.23%) | 68 (23.29%) | 3 (0.58%) |
| Non-Hispanic Black | 284 (7.13%) | 21 (21.88%) | 8 (0.42%) | 104 (27.51%) | 9 (3.08%) | 9 (1.74%) |
| Multi-racial | 140 (3.52%) | 5 (5.21%) | 62 (3.22%) | 19 (5.03%) | 23 (7.88%) | 9 (1.74%) |
| Other race | 179 (4.50%) | 13 (13.54%) | 70 (3.63%) | 4 (1.06%) | 33 (11.30%) | 4 (0.78%) |
| Age | ||||||
| 18 to 24 | 376 (9.65%) | 12 (13.95%) | 137 (7.22%) | 19 (5.37%) | 91 (31.16%) | 20 (3.96%) |
| 25 to 34 | 819 (21.01%) | 29 (33.72%) | 339 (17.87%) | 77 (21.75%) | 63 (21.58%) | 100 (19.8%) |
| 35 to 44 | 966 (24.78%) | 23 (26.74%) | 480 (25.30%) | 60 (16.95%) | 59 (20.21%) | 135 (26.73%) |
| 45 to 54 | 675 (17.32%) | 9 (10.47%) | 341 (17.98%) | 67 (18.93%) | 41 (14.04%) | 111 (21.98%) |
| 55 to 64 | 637 (16.34%) | 10 (11.63%) | 382 (20.14%) | 67 (18.93%) | 24 (8.22%) | 80 (15.84%) |
| 65 plus | 425 (10.90%) | 3 (3.49%) | 218 (11.49%) | 64 (18.08%) | 14 (4.79%) | 59 (11.68%) |
| Education | ||||||
| Less than high school | 42 (1.05%) | 3 (3.23%) | 8 (0.41%) | 3 (0.79%) | 13 (4.36%) | 3 (0.58%) |
| Completed high school | 295 (7.39%) | 10 (10.75%) | 107 (5.54%) | 23 (6.05%) | 37 (12.42%) | 55 (10.62%) |
| Some college, but no degree | 705 (17.67%) | 14 (15.05%) | 317 (16.42%) | 52 (13.68%) | 105 (35.23%) | 86 (16.60%) |
| Completed 2-year college or trade school | 464 (11.63%) | 5 (5.38%) | 196 (10.15%) | 80 (21.05%) | 50 (16.78%) | 73 (14.09%) |
| Completed 4-year college or higher | 2484 (62.26%) | 61 (65.59%) | 1303 (67.48%) | 222 (58.42%) | 93 (31.21%) | 301 (58.11%) |
| Household Income | ||||||
| $5,000 or less per year | 122 (3.24%) | 6 (7.06%) | 29 (1.58%) | 10 (2.98%) | 24 (8.54%) | 17 (3.48%) |
| $5,001–15,000 per year | 259 (6.89%) | 8 (9.41%) | 95 (5.16%) | 12 (3.57%) | 53 (18.86%) | 21 (4.30%) |
| $15,001–25,000 per year | 301 (8.01%) | 13 (15.29%) | 124 (6.74%) | 15 (4.46%) | 46 (16.37%) | 27 (5.53%) |
| $25,001–35,000 per year | 377 (10.03%) | 10 (11.76%) | 173 (9.4%) | 38 (11.31%) | 42 (14.95%) | 46 (9.43%) |
| $35,001–45,000 per year | 362 (9.63%) | 3 (3.53%) | 184 (9.99%) | 37 (11.01%) | 31 (11.03%) | 49 (10.04%) |
| $45,001–50,000 per year | 323 (8.59%) | 6 (7.06%) | 175 (9.51%) | 29 (8.63%) | 14 (4.98%) | 50 (10.25%) |
| More than $50,000 per year | 2016 (53.62%) | 39 (45.88%) | 1061 (57.63%) | 195 (58.04%) | 71 (25.27%) | 278 (56.97%) |
| Employment Status | ||||||
| Not employed- not looking for work | 205 (5.13%) | 9 (9.57%) | 103 (5.34%) | 14 (3.68%) | 15 (4.98%) | 29 (5.59%) |
| Not employed- looking for work | 88 (2.20%) | 2 (2.13%) | 25 (1.30%) | 11 (2.89%) | 22 (7.31%) | 11 (2.12%) |
| Not employed- retired, disabled, homemaker, or full-time student | 369 (9.23%) | 7 (7.45%) | 171 (8.86%) | 47 (12.37%) | 6 (1.99%) | 65 (12.52%) |
| Yes- employed in a temporary/seasonal job | 159 (3.98%) | 4 (4.26%) | 84 (4.35%) | 11 (2.89%) | 23 (7.64%) | 3 (0.58%) |
| Yes- employed year-round in a job for 1–10 h per week. | 149 (3.73%) | 3 (3.19%) | 63 (3.26%) | 8 (2.11%) | 34 (11.3%) | 5 (0.96%) |
| Yes- employed year-round in a job for 11–29 h per week. | 460 (11.51%) | 14 (14.89%) | 222 (11.5%) | 35 (9.21%) | 60 (19.93%) | 39 (7.51%) |
| Yes- employed year-round in a job for more than 30 h per week. | 2374 (59.41%) | 54 (57.45%) | 1139 (59.02%) | 238 (62.63%) | 128 (42.52%) | 350 (67.44%) |
| Other employment status | 192 (4.80%) | 1 (1.06%) | 123 (6.37%) | 16 (4.21%) | 13 (4.32%) | 17 (3.28%) |
| Number of Children in Household | ||||||
| Before COVID-19 (Mean, SD) | 0.85 (1.23) | 0.9 (1.34) | 0.83 (1.21) | 0.74 (1.08) | 0.89 (1.38) | 0.88 (1.13) |
| During COVID-19 (Mean, SD) | 0.86 (1.26) | 0.94 (1.45) | 0.84 (1.22) | 0.72 (1.06) | 0.89 (1.31) | 0.89 (1.13) |
| Number of Adults in Household | ||||||
| Before COVID-19 (Mean, SD) | 1.29 (1.5) | 1.43 (2.77) | 1.2 (0.85) | 1.27 (0.87) | 1.6 (1.18) | 1.22 (0.82) |
| During COVID-19 (Mean, SD) | 1.35 (1.65) | 1.48 (2.76) | 1.27 (0.93) | 1.34 (0.94) | 1.63 (1.19) | 1.34 (1.88) |
| Urbanicity1 | ||||||
| Urban | 1756 (47.55%) | 642 (83.27%) | 472 (25.88%) | 170 (48.02%) | 198 (74.72%) | 274 (57.2%) |
| Rural | 1937 (52.45%) | 129 (16.73%) | 1352 (74.12%) | 184 (51.98%) | 67 (25.28%) | 205 (42.8%) |
| Relied on Social Services/Government Assistance | ||||||
| Before COVID-19 | 1179 (29.28%) | 263 (30.06%) | 495 (25.46%) | 107 (27.94%) | 149 (49.17%) | 165 (31.67%) |
| During COVID-19 | 1189 (29.73%) | 259 (29.94%) | 503 (26.01%) | 94 (24.8%) | 157 (51.82%) | 176 (33.91%) |
| Presence of Chronic Health Conditions | ||||||
| Overweight or obese | 1297 (34.03%) | 261 (32.71%) | 557 (29.75%) | 149 (40.38%) | 90 (32.49%) | 240 (48.48%) |
| High blood pressure or hypertension | 842 (22.09%) | 190 (23.81%) | 329 (17.57%) | 117 (31.71%) | 52 (18.77%) | 154 (31.11%) |
| Pre diabetes | 295 (7.74%) | 42 (5.26%) | 329 (17.57%) | 45 (12.2%) | 30 (10.83%) | 55 (11.11%) |
| High blood sugar, Type 1 diabetes, Type II diabetes | 213 (5.59%) | 39 (4.89%) | 78 (4.17%) | 31 (8.4%) | 1 (12.00%) | 53 (10.71%) |
| Gestational diabetes / diabetes during pregnancy | 98 (2.57%) | 19 (2.38%) | 38 (2.03%) | 15 (4.07%) | 6 (2.17%) | 20 (4.04%) |
| Metabolic syndrome | 75 (1.97%) | 18 (2.26%) | 36 (1.92%) | 6 (1.63%) | 4 (1.44%) | 11 (2.22%) |
| Heart condition such as a heart attack, angina, or congestive heart failure | 98 (2.57%) | 21 (2.63%) | 39 (2.08%) | 10 (2.71%) | 6 (2.17%) | 22 (4.44%) |
| Chronic lung disease or moderate to severe asthma | 250 (6.56%) | 45 (5.64%) | 140 (7.48%) | 19 (5.15%) | 16 (5.78%) | 30 (6.06%) |
| Chronic kidney disease | 27 (0.71%) | 8 (1.00%) | 10 (0.53%) | 4 (1.08%) | 1 (0.36%) | 4 (0.81%) |
| Chronic liver disease | 18 (0.47%) | 6 (0.75%) | 2 (0.11%) | 2 (0.54%) | 3 (1.08%) | 5 (1.01%) |
| Immunocompromised | 200 (5.25%) | 33 (4.14%) | 101 (5.40%) | 17 (4.61%) | 10 (3.61%) |
|
As defined by Rural Urban Commuting Area (RUCA) codes.
Prior to COVID-19, respondents’ average psychological distress scale score was 9.69. During COVID-19, this score increased to 13.51, indicating that respondents’ psychological distress levels worsened during COVID-19.
Table 2 presents results from logistic regressions modeling the association between psychological distress during COVID-19 and perceived difficulty of maintaining pre-pandemic PA levels. Model 1 illustrates that during COVID-19, the K6 scale was negatively associated with PA levels (p < 0.01). Every 1 unit increase in K6 score resulted in a 1.11 greater odds of experiencing difficulty maintaining pre-pandemic PA levels during COVID-19 (p < 0.01). The only statistically significant variable in this model was household income prior to COVID-19; respondents with an annual income of $45,001-$50,000 had 1.35 greater odds of experiencing difficulty maintaining PA levels (p < 0.05) compared to households making more than $50,000 per year.
Table 2.
Logistic regression estimates modeling odds of experiencing difficulty maintaining previous physical activity levels during COVID-19 per one-unit increase in Kessler score during COVID-19, controlling for race/ethnicity, household income, sex urbanicity, education, employment status, use of social services, and presence of chronic health conditions.
| Variable | Odds Ratio | 95% CI1 | P-value | |
|---|---|---|---|---|
| Race/Ethnicity | White vs non-White | 0.71 | (0.45, 1.12) | 0.14 |
| Hispanic vs non-Hispanic | 0.73 | (0.43, 1.24) | 0.25 | |
| Black vs non-Black | 0.88 | (0.51, 1.53) | 0.65 | |
| Asian vs non-Asian | 2.05 | (0.97, 4.34) | 0.06 | |
| American Indian/Alaskan Native vs non-American Indian/Alaskan Native | 0.69 | (0.36, 1.31) | 0.26 | |
| Middle Eastern vs non-Middle Eastern | 0.64 | (0.17, 2.38) | 0.50 | |
| Hawaiian/Pacific Islander vs non-Hawaiian/Pacific Islander | 1.37 | (0.11, 17.82) | 0.81 | |
| Multi-racial vs non-multi-racial | 0.76 | (0.39, 1.49) | 0.42 | |
| Other race vs non-other race | 0.85 | (0.32, 2.29) | 0.75 | |
| Household income | $5,000 or less per year vs more than $50,000 per year | 0.85 | (0.48, 1.49) | 0.56 |
| $5,001–15,000 per year vs more than $50,000 per year | 1.17 | (0.81, 1.70) | 0.41 | |
| $15,001–25,000 per year vs more than $50,000 per year | 0.80 | (0.58, 1.11) | 0.19 | |
| $25,001–35,000 per year vs more than $50,000 per year | 1.22 | (0.92, 1.63) | 0.17 | |
| $35,001–45,000 per year vs more than $50,000 per year | 0.99 | (0.75, 1.30) | 0.94 | |
| $45,001–50,000 per year vs more than $50,000 per year | 1.35 | (1.01, 1.80) | 0.04 | |
| Sex | Female vs male | 0.81 | (0.64, 1.03) | 0.09 |
| Other sex vs male | 1.14 | (0.30, 4.38) | 0.85 | |
| Urbanicity2 | Rural vs urban | 0.89 | (0.76, 1.04) | 0.13 |
| Education | Less than high school vs completed 4-year college or higher | 1.08 | (0.32, 3.66) | 0.90 |
| Completed high school vs completed 4-year college or higher | 0.89 | (0.63, 1.24) | 0.48 | |
| Some college, but no degree vs completed 4-year college or higher | 0.98 | (0.79, 1.23) | 0.88 | |
| Completed 2-year junior or community college or trade school vs completed 4-year college or higher | 0.90 | (0.69, 1.16) | 0.41 | |
| Employment status | Not employed- not looking for work vs employed- full time | 1.21 | (0.81, 1.82) | 0.35 |
| Not employed- looking for work vs employed- full time | 0.88 | (0.49, 1.56) | 0.65 | |
| Not employed- retired, disabled, homemaker, or full-time student vs employed- full time | 1.26 | (0.95, 1.68) | 0.11 | |
| Employed- 1–10 h per week vs employed- full time | 1.08 | (0.71, 1.64) | 0.73 | |
| Employed- 11–29 h per week vs employed- full time | 1.14 | (0.87, 1.48) | 0.34 | |
| Employed- temporary or seasonal job vs employed- full time | 1.32 | (0.86, 2.04) | 0.21 | |
| Other employment status vs employed- full time | 1.11 | (0.77, 1.59) | 0.57 | |
| Use of social services/government assistance | Yes (received assistance) vs no (did not receive assistance) | 1.16 | (0.97, 1.38) | 0.12 |
| Presence of chronic health condition(s) | Presence of one or more chronic health conditions vs no chronic health conditions | 1.09 | (0.93, 1.28) | 0.27 |
| Kessler Score during COVID-19 | Per one unit increase in Kessler score | 1.11 | (1.09, 1.13) | <0.01 |
95% Confidence Interval.
As defined by Rural Urban Commuting Area (RUCA) codes.
For model 2, researchers examined the association between changes in maintaining pre-pandemic PA levels and psychological distress levels. Difficulty maintaining pre-COVID-19 PA levels was associated with an increase in K6 score during the pandemic. More specifically, challenge maintaining prior PA levels during COVID-19 was associated with a 1.73 point higher increase in K6 score, on average, compared to those who experienced equal or less challenge maintaining PA levels (p < 0.01). Additionally, rural zip codes were significantly associated (p < 0.05) with a 0.37 point lower increase in K6 score, on average, compared to those living in urban zip codes.
Lastly, researchers examined the association between K6 score change with difficulty maintaining pre-pandemic PA levels (Model 3). When comparing changes in K6 scores before and during COVID-19, the odds of experiencing difficulty maintaining PA levels increased by a factor of 1.13 for every 1 unit increase in K6 score (p < 0.01). Additionally, race/ethnicity, income status, and urbanicity were all significantly associated with difficulty maintaining PA levels. Respondents who self-identified as Asian had a 2.35 greater odds of experiencing difficulty maintaining pre-pandemic PA levels (p < 0.05) than those not identifying as Asian. Respondents whose household income was $45,001-$50,000 per year also had 1.46 greater odds of experiencing difficulty maintaining PA levels (p = 0.01) compared to households making more than $50,000 per year. Lastly, respondents living in urban zip codes had a 1.22 greater odds of experiencing difficulty maintaining PA levels (p < 0.05) than respondents living in rural areas (Table 3).
Table 3.
Logistic regression estimates modeling odds of experiencing difficulty maintaining previous physical activity levels during COVID-19 per one-unit change in Kessler score during COVID-19, controlling for race/ethnicity, household income, sex urbanicity, education, employment status, use of social services, and presence of chronic health conditions.
| Variable | Odds Ratio | 95% CI1 | P-value | |
|---|---|---|---|---|
| Race/Ethnicity | White vs non-White | 0.74 | (0.46, 1.18) | 0.21 |
| Hispanic vs non-Hispanic | 0.70 | (0.41, 1.20) | 0.20 | |
| Black vs non-Black | 0.86 | (0.49, 1.51) | 0.60 | |
| Asian vs non-Asian | 2.35 | (1.10, 5.02) | 0.03 | |
| American Indian/Alaskan Native vs non-American Indian/Alaskan Native | 0.72 | (0.38, 1.39) | 0.33 | |
| Middle Eastern vs non-Middle Eastern | 0.63 | (0.17, 2.34) | 0.49 | |
| Hawaiian/Pacific Islander vs non-Hawaiian/Pacific Islander | 0.88 | (0.07, 11.77) | 0.93 | |
| Multi-racial vs non-multi-racial | 0.92 | (0.46, 1.84) | 0.82 | |
| Other race vs non-other race | 0.74 | (0.28, 1.98) | 0.54 | |
| Household income | $5,000 or less per year vs more than $50,000 per year | 1.07 | (0.61, 1.87) | 0.81 |
| $5,001–15,000 per year vs more than $50,000 per year | 1.31 | (0.90, 1.91) | 0.15 | |
| $15,001–25,000 per year vs more than $50,000 per year | 0.93 | (0.67, 1.28) | 0.64 | |
| $25,001–35,000 per year vs more than $50,000 per year | 1.34 | (1.01, 1.79) | 0.05 | |
| $35,001–45,000 per year vs more than $50,000 per year | 1.04 | (0.79, 1.36) | 0.79 | |
| $45,001–50,000 per year vs more than $50,000 per year | 1.46 | (1.09, 1.96) | 0.01 | |
| Sex | Female vs male | 0.82 | (0.65, 1.04) | 0.11 |
| Other sex vs male | 1.38 | (0.36, 5.32) | 0.64 | |
| Urbanicity2 | Rural vs urban | 0.82 | (0.70, 0.96) | 0.02 |
| Education | Less than high school vs completed 4-year college or higher | 1.43 | (0.42, 4.80) | 0.57 |
| Completed high school vs completed 4-year college or higher | 0.81 | (0.57, 1.14) | 0.22 | |
| Some college, but no degree vs completed 4-year college or higher | 0.97 | (0.77, 1.21) | 0.77 | |
| Completed 2-year junior or community college or trade school vs completed 4-year college or higher | 0.81 | (0.63, 1.05) | 0.11 | |
| Employment status | Not employed- not looking for work vs employed- full time | 1.22 | (0.81, 1.84) | 0.35 |
| Not employed- looking for work vs employed- full time | 0.90 | (0.51, 1.60) | 0.73 | |
| Not employed- retired, disabled, homemaker, or full-time student vs employed- full time | 1.11 | (0.84, 1.48) | 0.46 | |
| Employed- 1–10 h per week vs employed- full time | 1.05 | (0.69, 1.60) | 0.82 | |
| Employed- 11–29 h per week vs employed- full time | 1.20 | (0.92, 1.57) | 0.18 | |
| Employed- temporary or seasonal job vs employed- full time | 1.37 | (0.89, 2.13) | 0.16 | |
| Other employment status vs employed- full time | 1.10 | (0.77, 1.58) | 0.61 | |
| Use of social services/government assistance during COVID-19 | Yes (received assistance) vs no (did not receive assistance) | 1.19 | (1.00, 1.43) | 0.05 |
| Presence of chronic health condition(s) | Presence of one or more chronic health conditions vs no chronic health conditions | 1.16 | (0.99, 1.36) | 0.06 |
| Difference in Kessler Score (during COVID-19 - score before COVID-19) | Per one unit increase in Kessler score difference | 1.13 | (1.1, 1.15) | <0.01 |
95% Confidence Interval.
As defined by Rural Urban Commuting Area (RUCA) codes.
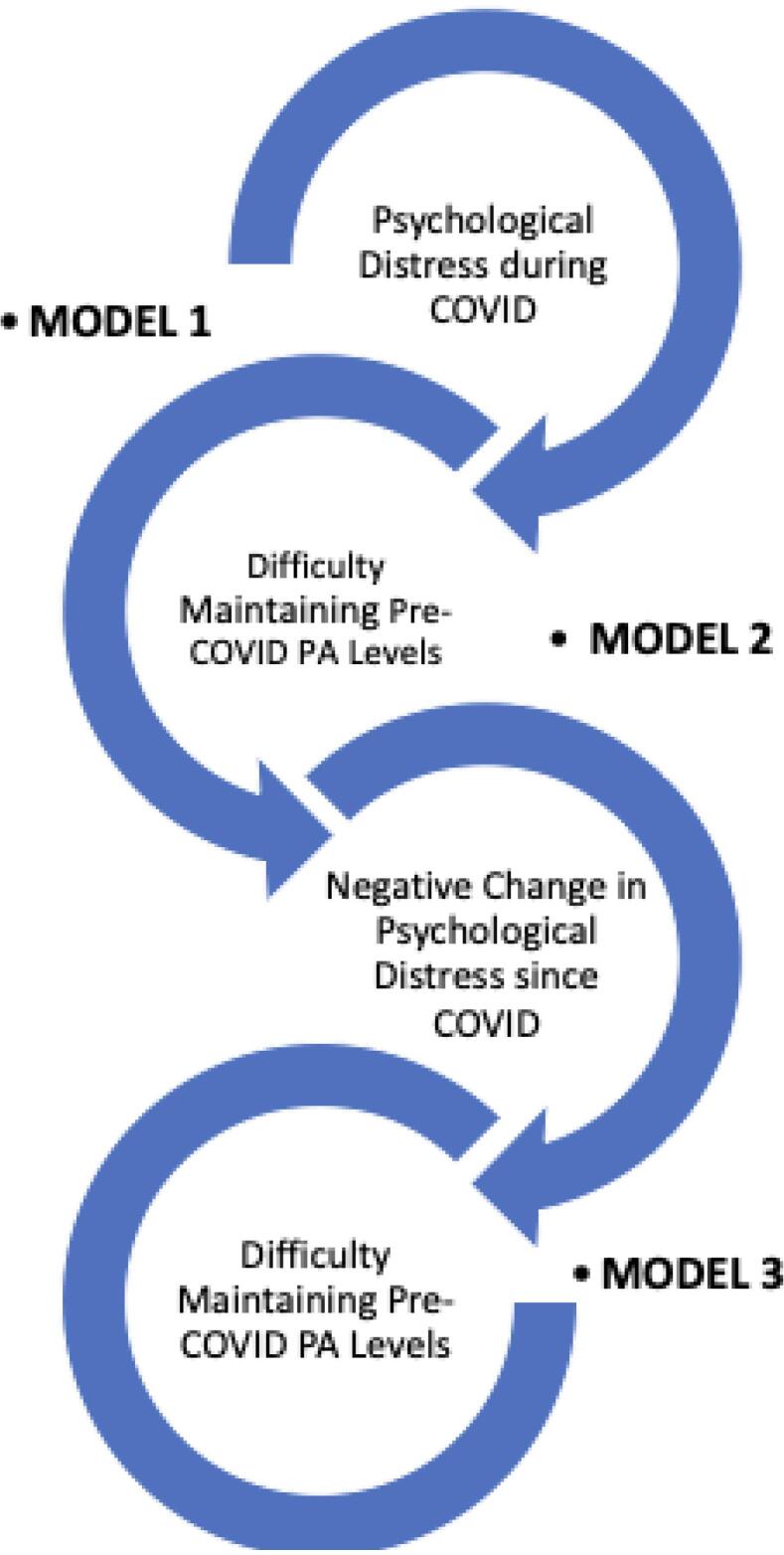
The regression model results show a bi-directional relationship between PA and MH during COVID-19. Additionally, this relationship is cyclical: psychological distress is related to PA, which is in turn related to further decreases in psychological distress, which again is related to PA levels (Fig. 1).
Fig. 1.
Illustration of the bi-directional, cyclical relationship between physical activity and mental health during COVID-19.* Data was collected between April – September of 2020.
3.2. Qualitative results
Many participants indicated that COVID-19 stay-at-home orders directly affected their ability to engage in PA (n = 538). For some participants, stay-at-home orders increased PA levels. As one participant explained, “[I have] more time at home; able to work outside; quarantine [is] forcing me to cancel plans/stay at home so no excuse not to exercise” (Louisiana P28). For other residents, living in a rural location meant that they felt safer being active outdoors. As a participant stated, “I walk around the neighborhood. I live in a rural area and I feel like I can walk safely since there are few people out when I am walking” (North Carolina P306).
However, for many others, COVID-19 closures were an obstacle to PA. As one participant noted, “gym is closed, worried to go outside to workout” (North Carolina P253). Numerous respondents feared going outside, or were not able to due to park closures. “The stay-at-home order meant I couldn’t access trails” (Oregon P58). Many respondents who were additionally caring for children and/or older adults cited that stay-at-home orders made PA even more difficult (n = 192).
Qualitative data can also contextualize the bi-directional, cyclical relationship between MH and PA reported quantitatively.
Phase 1: The Impact of Psychological Distress on Maintaining Pre-COVID Physical Activity Levels
Numerous participants cited that feelings of distress impacted their PA levels (Quantitative results, Model 1). According to one participant, “My mental health has decreased and that has influenced my desire to get exercise” (Oregon P173). For other respondents, MH impacted their PA routines because of lack of childcare and continued (or increased) workloads. As one participant noted, “My children have been home since March, and we have not had childcare until recently. I have to prioritize work, housework, and childcare over self-care” (Louisiana P634). These new responsibilities led to exhaustion, which made PA difficult and kept participants from other forms of self-care that might have facilitated PA. As another participant shared, “I have been caring for my baby while working from home, so I sometimes feel like I don't have time or energy at the end of the day because of the distractions during the workday” (Montana P168). Another summed this up by sharing, “I'm mentally exhausted and overwhelmed” (Montana P1794).
Phase 2: The Impact of Lower Physical Activity Levels During COVID on Psychological Distress
Other statements from participants indicated that difficulty maintaining PA during COVID-19 led to further deterioration of MH (Quantitative results, Model 2). As one participant explained, “while it would seem that being at home provides more time to exercise, it is not as motivating. [The] workday now has to be completed along with housework and homework all at home. [I] have lost the ability to go to my exercise class that was scheduled twice a week. Losing that firm spot for fitness has been difficult” (West Virginia P7). According to another participant, “It is hard to keep up with my level of physical activity I sustained before with no gym and poor mental health” (Louisiana P193).
Phase 3: The Impact of Negative Change in Psychological Distress (During COVID) on Further Deterioration of Physical Activity Levels
Finally, the relationship between MH and PA is described by those who reported that the presence of psychological distress further deteriorated PA levels (Quantitative results, Model 3). Several participants described diagnosed MH issues that either emerged or worsened during the pandemic, including depression. For some, this was connected to stress around contracting COVID-19:
“I am less motivated due to my depression and anxiety (diagnosed by a psychiatrist) being heightened during this time. I have autoimmune conditions not known to increase risk of covid but it always makes me more worried about going to work or the grocery store. It usually results with a full-blown anxiety attack before entering.” (Louisiana P509).
For some, depression was tied to motivation to be active (or lack thereof). Some participants talked about feeling “hopeless” about the future or fears of leaving the house because they were susceptible to COVID-19. For others, lack of social support because of stay-home orders increased depression. As one participant said, “I usually exercise with friends. COVID has also been a grief\depression trigger for me. When I’m depressed it is challenging for me to do things like exercise” (Montana P1011). Additionally, MH impacts like exhaustion, stress, and depression shaped whether or how participants could be active during COVID-19. As one participant stated, “I have felt a bit hopeless and down and out… feeling a bit like there's no point if we will just be sentenced to our own homes for the foreseeable future” (Montana P1063).
Overall, participants noted how stay-at-home orders and increased caregiving kept them from PA. The additional stressors of life during a pandemic also worsened MH challenges faced by those who were already struggling to get by.
4. Discussion
The COVID-19 pandemic has exacerbated MH challenges and led to a rise in mental illness diagnoses, substance misuse, and feelings of worry, stress, anxiety, hopelessness, and in some cases, job satisfaction (Liu and Modir, 2006, Chen et al., 2020, Capasso et al., 2021, Magnavita et al., 2021). This has been intensified by the necessity of social distancing. While a successful mitigation strategy for COVID-19 transmission, it has negatively impacted people’s well-being due to the loss of social support and increased feelings of loneliness and isolation (Hwang et al., 2020). This echoes previous research on viral diseases and their impacts on MH (DiGiovanni et al., 2004). This study contributes to the literature by exploring how virus-related MH experiences relate to PA. While over the years numerous studies have evaluated physical activity in relation to mental health in other contexts (Taylor et al., 1985, Fox, 1999, Harris, 2018), the literature on this relationship during the COVID-19 pandemic is limited, but growing (Violant-Holz et al., 2020, Silva et al., 2020).
Pre-pandemic research shows that PA serves as a protective factor for MH and well-being. Therefore, it is imperative to consider the relationship between PA and MH, both during and after the pandemic. Based on the aforemenioned logistic regression models, this study reveals that an increase in psychological distress led to a decrease in PA levels during COVID-19 (Phase 1), which led to further decreases in psychological distress (Phase 2), which led to even further decreases in PA (Phase 3). This bi-directional, cyclical relationship is an important finding since PA has been well documented as a key strategy to help support positive MH (Schuch et al., 2018, Kandola et al., 2019, White et al., 2017).
Surprisingly, most variables in Model 1 comparing changes in PA before and during COVID-19 were not statistically significant (with the exception of household income). Model 2, however, illustrated that difficulty maintaining pre-COVID-19 PA levels was associated with an increase in K6 score during COVID-19. Contrary to previous studies that have shown rural residents at an increased risk for diminished MH in comparison to urban residents (Silva et al., 2020) our study suggests that rural respondents experienced a smaller increase in their K6 score during COVID-19 compared to those living in urban areas. We infer that rural residents perceived their outdoor spaces as less risky for contracting COVID-19 and felt comfortable being outdoors. Alternatively, it is possible that PA for rural residents did not decrease because their regular PA activities were already mostly outdoors (Silva et al., 2020, Singh et al., 2017).
Lastly, when comparing changes in K6 scores before and during COVID-19 and the odds of experiencing difficulty maintaining PA levels (Model 3), respondents who self-identified as Asian had greater difficulty maintaining pre-COVID-19 PA levels during the pandemic, as did those households whose income was $45,001-$50,000 per year, and/or those who lived in urban areas. Violence and discrimination against Asian and Asian-Americans has increased rapidly during the COVID-19 pandemic (Chen et al., 2020). The results related to difficulty maintaining PA during COVID-19 for Asian and Asian-American participants may speak to a recent surge “of anti-Asian racism and “othering” practices during the COVID-19 pandemic,” which have “exposed the marginalization and conditional status of Asian Americans” in the United States (Liu and Modir, 2006).
The spread of COVID-19, like other epidemics, is greatly influenced by a population’s social and emotional response to the virus (Cullen et al., 2020). Decreases in MH during the pandemic offers lessons in the intersections of MH and physical health (Cullen et al., 2020, Pfefferbaum and North, 2020). This includes the need to prioritize interventions and support for those with established MH conditions as they are at greatest risk for decreases in PA that could lead to further deterioration of health (Czeisler et al., 2020, Cullen et al., 2020). Next, documented increases in depression, emotional and physical isolation, and anxiety during infectious disease outbreaks means that interventions should be implemented swiftly to address the reciprocal nature of mental and physical health (Sallis et al., 2020).
This research demonstrates the need for opportunities to engage people in a variety of cost effective, stay-at-home activities including video gaming, dancing, and using safe, natural features around the neighborhood for activity such as parks, beaches, or fields (Hammami et al., 2020). Lastly, COVID-19 presents a robust research agenda for the future including examining the impacts of residential density and the health impacts of walkable communities with equitable access to parks, playgrounds, bike trails and sidewalks (Sallis et al., 2020).
4.1. Limitations
The online survey distribution presents a limitation, as individuals lacking internet access were excluded from the sample, thus impacting sample size and generalizability. There may be a seasonality effect to the PA findings, as this survey was distributed in the summer, when people may have been more likely to be active outdoors due to longer hours of daylight and warmer weather (Wagner et al., 2019). Additionally, the duration of participants’ PA was not measured directly- rather, participants self-reported this. Numerous other potentially stress-inducing matters (e.g. persistent racial injustices, politically-driven civil unrest) that took place during the time of data collection could have impacted respondents’ reported MH status. This study also did not directly ask survey respondents whether they engaged in activities that could have had a beneficial effect on their mental health, such as mindfulness, meditation and/or prayer. Accordingly, observed attenuated or smaller decreases in positive mental health might possibly be attributed to these practices based on other literature (Hofmann et al., 2010, Ferguson et al., 2010). Lastly, these findings explain respondents’ behavior and sentiment as it relates to physical activity and mental health within a short timeframe during the beginning of the COVID-19 pandemic and should not be taken out of temporal context.
5. Public health implications
Given that this study has highlighted a bidirectional, cyclical relationship between PA and MH during the COVID-19 pandemic, it supports existing literature that cites PA as a protective factor against MH issues that should be addressed for the current and future pandemics.
First, since rural residents were more likely to keep their pre-COVID-19 PA routines, especially considering that MH issues tend to impact those in rural areas more, is hopeful. For example, between 2001 and 2015 the suicide rate was nearly 1.5 times higher in rural areas than in urban (Jensen et al., 2020, Summers-Gabr, 2020, Ivey-Stephenson et al., 2017). With the advent of COVID-19, MH problems in rural areas have worsened due to isolation and anxiety, in addition to the fact that assistance resources, have, in many rural areas, diminished (Summers-Gabr, 2020, Monteith et al., 2020). PA could be one protective factor to focus on in rural areas to improve and promote mental and physical health (Rural, 2004).
Beyond rural populations, PA can be protective and mitigate negative impacts of social isolation. Since numerous respondents cited “time” as a barrier to engaging in PA (n = 515), resources for home-based PA that can be accomplished in short amounts of time should be widely disseminated. Furthermore, since caregiving made it more difficult to maintain PA, programs to support PA in the home through online educational platforms should be explored (Hammami et al., 2020). These resources should be provided at no to low-cost, given that respondents with lower household incomes had greater odds of experiencing difficulty maintaining PA levels. Finally, information regarding the benefits of PA on MH should be widely disseminated, not only to the individuals, but to businesses as well, as this could motivate them to provide employees flextime for PA. This strategy would be especially helpful for those at higher risk of suffering from MH consequences of pandemics, such as frontline and shift workers. Moreover, this strategy could act as one avenue to prevent MH deterioration.
While these interventions could support individuals and organizations in adopting or maintaining PA as a protective factor against deteriorating psychological distress caused by the pandemic, they must be met with structural changes that recognize the intersections of inequities that shape whether or how people have access to PA or MH resources before, during, or after a pandemic.
Funding
This work was supported by the National Institutes of Health [grant number P20GM104417].
Credit authorship contribution statement
Michelle Grocke-Dewey: Conceptualization, Methodology, Formal analysis, Writing – original draft. Annie Hardison-Moody: Conceptualization, Methodology, Writing – review & editing. Lindsey Haynes-Maslow: Conceptualization, Methodology, Writing – review & editing. Shelly Maras: Writing – review & editing. Eliza Webber: Writing – review & editing. Lauri Andress: Writing – review & editing. Bailey Houghtaling: Writing – review & editing. Megan Patton-Lopez: Writing – review & editing. Justin Shanks: Writing – review & editing. Carmen Byker-Shanks: Funding acquisition, Conceptualization, Methodology, Formal analysis, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Michelle Grocke-Dewey, Email: michelle.grocke@montana.edu.
Annie Hardison-Moody, Email: amhardis@ncsu.edu.
Lindsey Haynes-Maslow, Email: lhmaslow@ncsu.edu.
Shelly Maras, Email: samaras2@ncsu.edu.
Eliza Webber, Email: eliza.webber@montana.edu.
Lauri Andress, Email: laandress@hsc.wvu.edu.
Bailey Houghtaling, Email: bhoughtaling@agcenter.lsu.edu.
Megan Patton-Lopez, Email: pattonlm@mail.wou.edu.
Justin Shanks, Email: jstnshanks@gmail.com.
Carmen Byker-Shanks, Email: cbykershanks@montana.edu.
References
- A. Jordan. Coronavirus in the U.S.: Latest Map and Case Count. The New York Times. https://www.nytimes.com/interactive/2021/us/covid-cases.html. Published July 15, 2021. Accessed July 15, 2021.
- Sen S., Karaca-Mandic P., Georgiou A. Association of Stay-at-Home Orders With COVID-19 Hospitalizations in 4 States. JAMA. 2020;323(24):2522–2524. doi: 10.1001/jama.2020.9176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S.R., Modir S. The outbreak that was always here: Racial trauma in the context of COVID-19 and implications for mental health providers. Psychological Trauma: Theory, Research, Practice, and Policy. 2006;12(5):439. doi: 10.1037/tra0000784. [DOI] [PubMed] [Google Scholar]
- Chen Justin A., Zhang Emily, Liu Cindy H. Potential Impact of COVID-19–Related Racial Discrimination on the Health of Asian Americans. Am. J. Public Health. 2020;110(11):1624–1627. doi: 10.2105/AJPH.2020.305858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F.B., Vancampfort D., Firth J., Rosenbaum S., Ward P.B., Silva E.S., Hallgren M., Ponce De Leon A., Dunn A.L., Deslandes A.C., Fleck M.P., Carvalho A.F., Stubbs B. Physical activity and incident depression: a meta-analysis of prospective cohort studies. AJP. 2018;175(7):631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- Kandola A., Ashdown-Franks G., Hendrikse J., Sabiston C.M., Stubbs B. Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 2019;107:525–539. doi: 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- White R.L., Babic M.J., Parker P.D., Lubans D.R., Astell-Burt T., Lonsdale C. Domain-Specific Physical Activity and Mental Health: A Meta-analysis. Am. J. Prev. Med. 2017;52(5):653–666. doi: 10.1016/j.amepre.2016.12.008. [DOI] [PubMed] [Google Scholar]
- Tipirneni R. A Data-Informed Approach to Targeting Social Determinants of Health as the Root Causes of COVID-19 Disparities. Am. J. Public Health. 2021;111(4):620–622. doi: 10.2105/AJPH.2020.306085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andress L., Purtill M.P., Ewen H.H. Shifting the gaze of the physician from the body to the body in a place: A qualitative analysis of a community-based photovoice approach to teaching place-health concepts to medical students. PLoS One. 2020;15(2):e0228640. doi: 10.1371/journal.pone.0228640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L. Evolving Intersectionality Within Public Health: From Analysis to Action. Am. J. Public Health. 2020;111(1):88–90. doi: 10.2105/AJPH.2020.306031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook J.E., Purdie-Vaughns V., Meyer I.H., Busch J.T.A. Intervening within and across levels: A multilevel approach to stigma and public health. Soc. Sci. Med. 2014;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- Meyer O.L., Castro-Schilo L., Aguilar-Gaxiola S. Determinants of Mental Health and Self-Rated Health: A Model of Socioeconomic Status, Neighborhood Safety, and Physical Activity. Am. J. Public Health. 2014;104(9):1734–1741. doi: 10.2105/AJPH.2014.302003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T.A., Kessler R.C., Slade T., Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol. Med. 2003;33(2):357–362. doi: 10.1017/S0033291702006700. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L.-T., Walters E.E., Zaslavsky A.M. Short Screening Scales to Monitor Population Prevalences and Trends in Non-Specific Psychological Distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.-L., Manderscheid R.W., Walters E.E., Zaslavsky A.M. Screening for Serious Mental Illness in the General Population. Arch. Gen. Psychiatry. 2003;60(2):184. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- USDA ERS - Rural-Urban Commuting Area Codes. Accessed April 12, 2021. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/.
- Dedoose Version 8.0.35, web application for managing, analyzing, and presenting qualitative and mixed method research data (2018). Los Angeles, CA: SocioCultural Research Consultants, LLC www.dedoose.com.
- Capasso A., Jones A.M., Ali S.H., Foreman J., Tozan Y., DiClemente R.J. Increased alcohol use during the COVID-19 pandemic: The effect of mental health and age in a cross-sectional sample of social media users in the U.S. Prev. Med. 2021;145:106422. doi: 10.1016/j.ypmed.2021.106422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnavita N., Soave P.M., Antonelli M. Prolonged Stress Causes Depression in Frontline Workers Facing the COVID-19 Pandemic—A Repeated Cross-Sectional Study in a COVID-19 Hub-Hospital in Central Italy. Int. J. Environ. Res. Public Health. 2021;18(14):7316. doi: 10.3390/ijerph18147316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang T.-J., Rabheru K., Peisah C., Reichman W., Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020:1–4. doi: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGiovanni C., Conley J., Chiu D., Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror. 2004;2(4):265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- Taylor C.B., Sallis J.F., Needle R. The relation of physical activity and exercise to mental health. Public Health Rep. 1985;100(2):195–202. [PMC free article] [PubMed] [Google Scholar]
- Fox K.R. The influence of physical activity on mental well-being. Public Health Nutr. 1999;2(3a):411–418. doi: 10.1017/S1368980099000567. [DOI] [PubMed] [Google Scholar]
- Harris M.A. The relationship between physical inactivity and mental wellbeing: Findings from a gamification-based community-wide physical activity intervention. Health Psychol. Open. 2018;5(1) doi: 10.1177/2055102917753853. 2055102917753853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Violant-Holz V., Gallego-Jiménez M.G., González-González C.S., et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int. J. Environ. Res. Public Health. 2020;17(24) doi: 10.3390/ijerph17249419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva L.R.B., Seguro C.S., de Oliveira C.G.A., Santos P.O.S., de Oliveira J.C.M., de Souza Filho L.F.M., de Paula Júnior C.A., Gentil P., Rebelo A.C.S. Physical Inactivity Is Associated With Increased Levels of Anxiety, Depression, and Stress in Brazilians During the COVID-19 Pandemic: A Cross-Sectional Study. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.565291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G., Daus G., Allender M., Ramey C., Martin E., Perry C., Reyes A., Vedamuthu I. Social Determinants of Health in the United States: Addressing Major Health Inequality Trends for the Nation, 1935–2016. Int. J. MCH AIDS. 2017;6(2) doi: 10.21106/ijma10.21106/ijma.V6.N210.21106/ijma.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen W., Gulati G., Kelly B.D. Mental health in the COVID-19 pandemic. QJM: An Int. J. Med. 2020;113(5):311–312. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Hammami A., Harrabi B., Mohr M., Krustrup P. Physical activity and coronavirus disease 2019 (COVID-19): specific recommendations for home-based physical training. Managing Sport and Leisure. 2020:1–6. doi: 10.1080/23750472.2020.1757494. [DOI] [Google Scholar]
- Sallis J.F., Adlakha D., Oyeyemi A., Salvo D. An international physical activity and public health research agenda to inform coronavirus disease-2019 policies and practices. J. Sport Health Sci. 2020;9(4):328–334. doi: 10.1016/j.jshs.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner A.L., Keusch F., Yan T., Clarke P.J. The impact of weather on summer and winter exercise behaviors. J. Sport Health Sci. 2019;8(1):39–45. doi: 10.1016/j.jshs.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann S.G., Sawyer A.T., Witt A.A., Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson J.K., Willemsen E.W., Castañeto M.V. Centering Prayer as a Healing Response to Everyday Stress: A Psychological and Spiritual Process. Pastoral Psychol. 2010;59(3):305–329. doi: 10.1007/s11089-009-0225-7. [DOI] [Google Scholar]
- Jensen E.J., Wieling E., Mendenhall T. A phenomenological study of clinicians’ perspectives on barriers to rural mental health care. Journal of Rural Mental Health. 2020;44(1):51–61. doi: 10.1037/rmh0000125. [DOI] [Google Scholar]
- Summers-Gabr N.M. Rural–urban mental health disparities in the United States during COVID-19. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S222–S224. doi: 10.1037/tra0000871. [DOI] [PubMed] [Google Scholar]
- Ivey-Stephenson A.Z., Crosby A.E., Jack S.P.D., Haileyesus T., Kresnow-Sedacca M. Suicide Trends Among and Within Urbanization Levels by Sex, Race/Ethnicity, Age Group, and Mechanism of Death — United States, 2001–2015. MMWR Surveill Summ. 2017;66(18):1–16. doi: 10.15585/mmwr.ss6618a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteith L.L., Holliday R., Brown T.L., Brenner L.A., Mohatt N.V. Preventing suicide in rural communities during the COVID-19 pandemic. J. Rural. Health. 2020 doi: 10.1111/jrh.12448. Published online May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rural H.D. Rural health disparities, population health, and rural culture. Am. J. Public Health. 2004;94(10):1675–1678. doi: 10.2105/AJPH.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]