Abstract
Physical exercise is a promising rehabilitative strategy for acute ischemic stroke. Preclinical trials suggest that exercise restores cerebral blood circulation and re-establishes the blood–brain barrier’s integrity with neurological function and motor skill improvement. Clinical trials demonstrated that exercise improves prognosis and decreases complications after ischemic events. Due to these encouraging findings, early exercise rehabilitation has been quickly adopted into stroke rehabilitation guidelines. Unfortunately, preclinical trials have failed to warn us of an adverse effect. Trials with very early exercise rehabilitation (within 24 h of ischemic attack) found an inferior prognosis at 3 months. It was not immediately clear as to why exercise was detrimental when performed very early while it was ameliorative just a few short days later. This review aimed to explore the potential mechanisms of harm seen in very early exercise administered to acute ischemic stroke patients. To begin, the mechanisms of exercise’s benefit were transposed onto the current understanding of acute ischemic stroke’s pathogenesis, specifically during the acute and subacute phases. Then, exercise rehabilitation’s mechanisms were compared to that of remote ischemic conditioning (RIC). This comparison may reveal how RIC may be providing clinical benefit during the acute phase of ischemic stroke when exercise proved to be harmful.
Keywords: Acute stroke, autoregulation, dysautoregulation, neuroprotection, stroke rehabilitation, subacute stroke
Introduction
Stroke is a leading cause of mortality and morbidity worldwide.[1,2] As life expectancy around the world increases, the global lifetime risk of stroke has also increased.[3] Of the various categories of strokes that plague the elderly, acute ischemic stroke comprises the largest portion.[4] And yet, treatment of acute ischemic stroke is currently limited to thrombolysis and, for a limited few, clot retrieval.[5] Despite improvements in recanalization rates and broadening of treatment eligibility criteria,[6] the rate of disability among survivors remains at a staggering rate of 50%.[7] Development of new treatment modalities with broad indications is necessary to relieve the tremendous disease burden of acute ischemic stroke.
Physical exercise is a promising rehabilitative strategy for acute ischemic stroke patients. Preclinical trials suggest that exercise rehabilitation can help to restore cerebral blood circulation[8,9] and re-establish the blood-brain barrier’s integrity[10] with improvements of neurological functions[11,12] and motor skills.[13] Clinical trials have demonstrated that exercise improves prognosis, decreases complications after ischemic events,[14] and improves motor function.[15] Due to these encouraging findings, early exercise rehabilitation has been quickly adopted into stroke rehabilitation guidelines.[16] Unfortunately, preclinical trials have failed to warn us of an adverse effect. Trials that started very early exercise rehabilitation (i.e. within 24 h of ischemic attack) found an inferior prognosis at 3 months.[17] It was not immediately clear as to why exercise was detrimental when performed very early while it was ameliorative just a few short days later. Furthermore, exercise has proven to be challenging to implement in stroke patients due to morbidities, instability, and disabilities after ischemic events.[18]
Another form of stroke rehabilitation is ischemic conditioning. In ischemic conditioning, sublethal hypoxia is induced on the body to coerce endogenous production of signaling molecules to aid in recovery from hypoxic damage.[19,20] RIC is one of the various forms of ischemic conditioning that is currently being explored.[21,22] It is currently being used for neuroprotection in other contexts such as symptomatic intracranial arterial stenosis (SIAS)[23] and carotid artery stent placements.[24] The sublethal dose of hypoxia is achieved on a distal limb with a blood pressure cuff and released to permit the beneficial signaling cascades to travel to the hypoxia-damaged tissue.[25,26,27] In preclinical studies, RIC was efficacious in stroke therapy[28,29,30] and acted synergistically with exercise in stroke therapy.[31,32] Furthermore, unlike exercise, it is a convenient therapy that is easy to administer on sick, recovering stroke patients.[26,33]
This review aims to explore the potential mechanisms of harm seen in very early exercise administered to acute ischemic stroke patients. To begin, the mechanisms of exercise’s benefit will be transposed onto the current understanding of acute ischemic stroke’s pathogenesis, specifically during the subacute phase. Then, we will explore exercise rehabilitation’s effect on the human body and how it may interact with the pathogenesis of ischemic stroke during the acute phase. Throughout the discussion, we will compare exercise rehabilitation’s mechanisms to that of RIC. This comparison may reveal how RIC may potentially provide clinical benefit during the acute phase of ischemic stroke, the same time frame in which exercise proved to be harmful. This review will focus on the acute and subacute phases of stroke, as the rehabilitative strategies that will be discussed have been prescribed within hours to days of the ischemic events in the studies that we are considering.
Acute and Subacute Phases of Stroke
The pathogenesis of acute ischemic stroke has been described extensively by Kurisu and Yenari.[34] They divide the pathogenesis of acute ischemic stroke into three phases: acute, subacute, and chronic. The time frames for these phases are minutes to hours, hours to days, and weeks to months, respectively. The acute phase of stroke is precipitated primarily due to alteration of blood flow. Ischemia resulting from an embolus, thrombus, or severe hypotension initiates a cascade of metabolic disequilibrium. Energy storing capacity quickly becomes impaired, leaving the neuron to depend on anerobic respiration, a considerably inefficient method of ATP generation compared to oxidative phosphorylation. Anerobic respiration generates lactic acid and inevitably acidosis. Inadequate ATP stores lead to cellular ion pump failure and loss of ion gradients across the membrane; these result in receptor activation from significant calcium influx and membrane insufficiency from hyperemia. The combination of cellular excitotoxicity from receptor activation and mitochondrial failure from membrane insufficiency ultimately ends with neuronal death.
The subacute phase relies on slower molecular signaling pathways for its tale of neuronal apoptosis to unfold. Its fate is determined by an interplay between proapoptotic and antiapoptotic molecules. Apoptosis can be divided into intrinsic and extrinsic pathways. The intrinsic pathway involves proapoptotic molecules of BCL-2-associated X (BAX), protein kinase Cδ, and cytochrome C, which are antagonized by antiapoptotic molecules, such as BCL-2 and PKCε. The extrinsic pathway involves the proapoptotic signaling pathway initiated by FAS-ligand-induced FAS activation. Both pathways ultimately end with caspase activation and subsequent apoptosis.
In summary, as depicted by Figure 1, the acute phase of stroke is progressed by the immediate consequences of interruptions to circulation within minutes to hours of the onset. The subacute phase of stroke counts on molecular cascades and marker expressions that are induced within hours to days. Exercise therapy should have underlying physiological mechanisms affected by time frames of acute and subacute phases of stroke. Understanding the mechanisms could help elucidate how the intended clinical amelioration occurs and how in other times they cause unintended harm instead.
Figure 1.
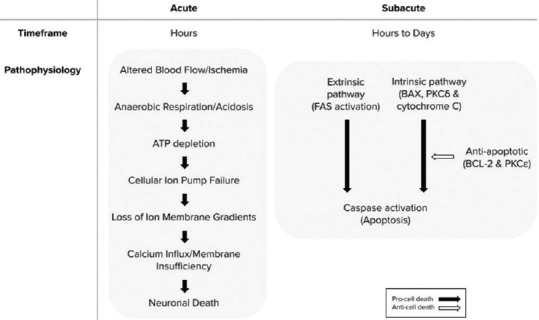
Pathophysiology of acute and subacute phases of stroke
Therapies and Subacute Phase of Stroke
Exercise and remote ischemic conditioning
As mentioned in the introduction, exercise rehabilitation has demonstrated its ameliorative effects in stroke patients by improving neurological function[6] and outcomes,[16] granted that it is not prescribed within 24 h of the ischemic event.[35] Exercise helps to maintain the blood–brain barrier[8,10] and prevent neuronal death,[8,9] which supports the associated observations of mitigated neurological impairment[11] and memory loss.[12]
RIC is a lesser-known method of postischemic stroke conditioning. RIC is based on an intrinsic process, named ischemic preconditioning, in which ischemia of short duration protects internal organs against subsequent ischemia. Ischemic preconditioning can be experimentally induced with a blood pressure cuff that creates a transient blood flow blockage at a distal limb. This procedure instigates endogenously protective effects on important internal organs from lethal ischemic damage.[25] RIC has also been induced through hypobaric and normobaric chambers.[36,37] This treatment method has been used for protection after myocardial infarction,[38] during carotid artery stent placements,[24] prophylactically for SIAS,[23] global cerebral ischemia,[20] and subcortical ischemic vascular dementia.[39] RIC has been reported to improve outcomes in chronic stroke as well.[40]
Exercise has been found to have very similar neuroprotective effects of RIC as it pertains to the subacute phase of acute ischemic stroke.[31] It supports neuroprotection[41] and regeneration by enhancing angiogenesis,[42] cerebral perfusion, cerebral collateral formation, and cerebral ischemia tolerance.[43,44] Further neuroprotection is established by reducing nerve injury,[45] promoting nerve remodeling,[42] and restoring function of paralyzed limbs.[31,40]
Therapies and mechanism of amelioration in the subacute phase
Hinted by their similar neuroprotective effects, it has been found that exercise and RIC have many overlaps in their ameliorative mechanism of action during the subacute phase of acute ischemic stroke [Figure 2]. Exercise and RIC protect brain tissue against injury by preventing apoptosis, modulating neuroplasticity regulation, and securing resources through angiogenesis.
Figure 2.
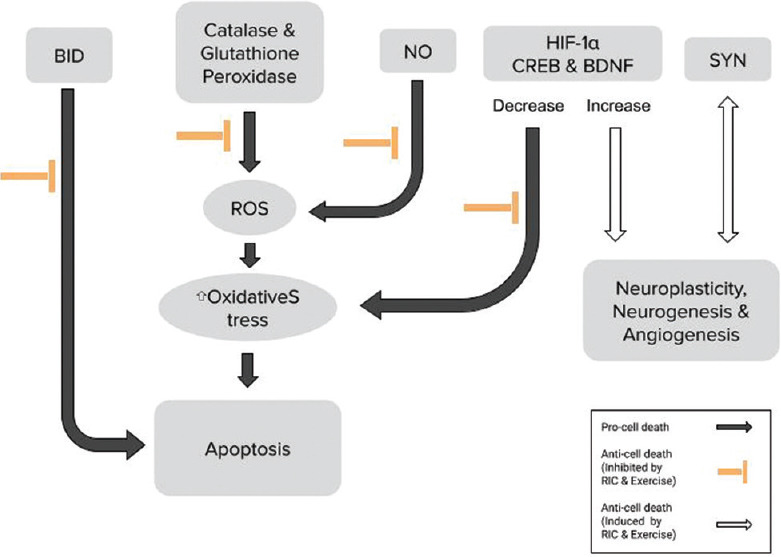
Subacute phase of stroke and the mechanism of exercise rehabilitation and remote ischemic conditioning
Apoptosis, as described above, is regulated through a fine balance between the pro and antiapoptotic pathways. Apoptosis is prevented through Bcl-2 interacting-domain death agonist inhibition by RIC[46] and exercise.[47] Increases in the Bcl-2/Bax ratio are favorable for neuron survival and are upregulated by RIC[48] and exercise.[49] ROS causes apoptosis through oxidative stress.[50] Exercise decreases oxidative stress by increasing catalase[51] and glutathione peroxidase.[52] RIC also increases antioxidant activity through glutathione,[53] catalase, and SOD.[54] NO scavenges ROS to prevent apoptosis;[55] exercise[56] and RIC[57] increase NO production.
Neuroplasticity can be assessed with many molecular markers. Synaptogenesis plays a critical role in neuroplasticity and can be measured with synaptophysin (SYN), a marker of synaptic plasticity in cerebral ischemia and damage.[58] Interestingly, SYN is increased by ischemic conditioning[59] and exercise.[60] In addition, neuroplasticity is regulated by cAMP response element-binding protein (CREB), brain-derived neurotrophic factor (BDNF), and tropomyosin receptor kinase B (TrkB), which act in coordination.[61,62] Ischemic conditioning[21] and exercise[60,63] increase CREB as well as BDNF.[21,64]
CREB supports neurogenesis[65] by encouraging functional recovery and increases circuit plasticity after stroke.[66] It also activates antioxidants and antiapoptotic proteins[38] to augment cell survival. The presence of BDNF indicates neuronal survival and synaptic plasticity; BDNF works with TrkB[67,68] to trigger an intracellular signaling cascade to mediate neuronal survival and differentiation,[69] angiogenesis,[70] and neuroplasticity.[71]
HIF-1α is a marker that is upregulated in hypoxic conditions and helps to mediate hypoxia by inducing vascular endothelial growth factor (VEGF), erythropoietin (EPO), and the respective receptors.[72,73] Through downstream effects of VEGF and EPO induction, HIF-1α ensures O2[74] and glucose[75] supplies to the brain. VEGF accelerates cognitive rehabilitation.[72] Ischemic conditioning[76] and exercise[77] are reported to increase HIF-1α. Preclinical trials have suggested that exercise and RIC, through HIF-1α, augment the BDNF/TrkB/CREB pathway in its amelioration of ischemic stroke.[32,78]
Therapies and Acute Phase of Ischemic Stroke
Cerebral autoregulation in the acute phase of ischemic stroke
Tissue death and injury in the acute phase of ischemic stroke are precipitated by inadequate blood supply due to a thrombus, emboli, or severe hypotension. In a healthy individual, perfusion of the cerebrum is supplemented by cerebral autoregulation through myogenic, neurogenic, metabolic, and endothelial mechanisms.[79] However, cerebral blood perfusion can still be insufficient following reperfusion. Various injuries to the head, such as traumatic brain injury,[80] hemorrhagic stroke,[81] and ischemic stroke,[82] can lead to autoregulation impairment, known as cerebral dysautoregulation. Inability to control blood flow to the brain may lead to both hypo and hyperperfusion. Cerebral dys-autoregulation results in hemorrhagic transformation and cerebral edema, which are often associated with a poor prognosis. The mechanism of these complications is hyperreperfusion, in which dys-autoregulation permits low vascular resistance and high blood flow velocity to the brain.[83] Studies have stressed the importance of maintaining cerebral autoregulation, which is associated with less atrophy and better neurological function in chronic ischemic infarctions.[84] At times, dys-autoregulation has been found to spread to the contralateral side of the injury as well, which was unsurprisingly associated with poor outcomes.[85]
Clinical studies have found that vascular recanalization helps to preserve the function of autoregulation, but the extent of its preservation is not well understood and requires more investigation.[86,87] Interestingly, animal studies have found rt-PA to cause dys-autoregulation.[88,89] Ma et al. discuss in their clinical trial that the superior autoregulation in the recanalized population may be because the patients with milder ischemia were eligible for the recanalization treatment, acting as a confounding variable.[86] Furthermore, cerebral dys-autoregulation has been observed from as early as 22 h[90] to as late as 6 months[91] following an ischemic event, making it relevant to our discussion.
Exercise and dys-autoregulation
Exercise induces changes to the hemodynamics of blood flow in the body. For instance, as skeletal muscles demand greater blood flow, other organs compete to maintain their critical perfusion levels to avoid ischemic damage. To supply both sides of the competition, heart rate and stroke volume increase to boost the overall cardiac output. Normal cardiac output is around 5 L/min for a resting adult human. With exercise, it can go up to 20 L/min for an average adult or to 40 L/min for athletes. Organs that are not directly involved in exercise, such as the kidneys and liver, have their blood flow redirected to skeletal and cardiac muscle tissue, decreasing their perfusion to ~25% of the flow at rest. The exception to this compensatory mechanism is the brain in a healthy individual, which maintains the same blood flow of 0.75 L/min both at rest and exercise.[92] In addition to the changes to the blood flow during exercise, the chemical composition of blood changes due to the increased metabolism in muscle tissues. Cerebral autoregulation must take these chemical changes into account in addition to the changes of the cardiac output to ensure consistent blood flow to the brain – the mechanism of which has been reviewed by Smith and Ainslie.[93]
Patients in the acute phase of ischemic stroke are unable to regulate cerebral blood flow during exercise because of cerebral dys-autoregulation. Brain tissues of patients with acute stroke can be overstressed by the changes of the cerebral blood flow’s hemodynamics, intracranial pressure, and intra- and extracellular chemistry while undergoing exercise rehabilitation. The brain can be hyperperfused or hypoperfused, depending on the specific regimen of the exercise and posture of the patient. Exercise during the acute phase of ischemic stroke may worsen prognosis by tempering blood supply to the brain during its vulnerable moments of dys-autoregulation [Figure 3].
Figure 3.
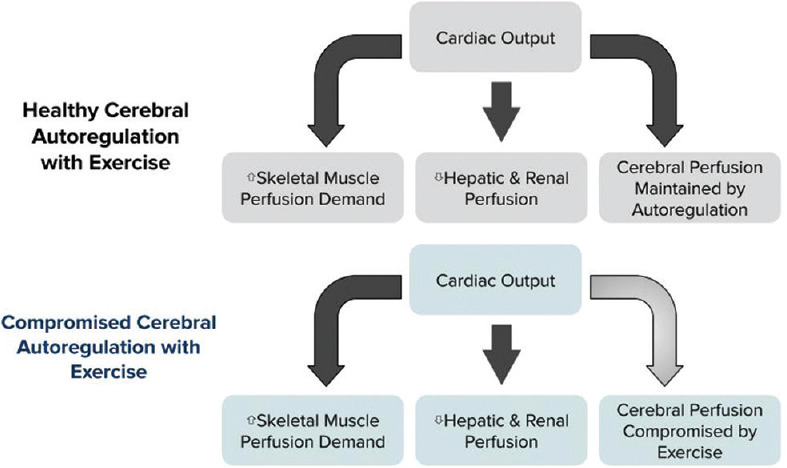
Acute phase of stroke and the mechanism of exercise
Remote ischemic conditioning in the acute phase of ischemic stroke
Those who are unfamiliar with RIC may express concerns for potential damage to the ischemic site and consequent cardiopulmonary response, which may potentially worsen cerebral perfusion.[94] It has been reported that up to 3 h of remote ischemia will not cause muscle damage to the ischemic site,[95] and concern for reperfusion damage is only necessary from 1 h of ischemia onward.[96] Because RIC protocols in ischemic tissue amelioration typically induce ischemia for only minutes at a time, ischemic tissue damage is not significant.
RIC has been demonstrated to be safe in a variety of contexts. As a preconditioning method, it has proven its safety and efficacy in pulmonary dysfunction[97] without damage to remote organs.[98] As a postconditioning method, its usage has been proven for spinal cord ischemia[99] and vascular endothelial dysfunction.[100] Finally, RIC is safe in acute ischemic stroke[101] as well as other cranial injuries, such as intracranial atherosclerosis,[102] carotid stenting, endarterectomy,[24] cerebral small vessel disease,[103] and aneurysm subarachnoid hemorrhage.[26]
As further reassurance, RIC in acute ischemic stroke has shown its efficacy with stable blood pressure, heart rate, intracranial pressure, cranial perfusion pressure, and peak velocity of middle cerebral artery.[101] Despite the brain’s inability to autoregulate in the context of acute ischemic stroke, the cerebral perfusion remains intact as RIC does not disturb the body’s circulatory dynamics. Stable cerebral perfusion is an important advantage of RIC because it does not occur with exercise rehabilitation. If the deleterious effects of exercise in the acute phase of stroke are primarily due to the instability of cerebral blood flow, RIC can be an excellent adjunct therapy. Exercise may not be able to induce clinical amelioration and prevent acute stroke damage within the first 24 h but RIC could [Figure 4].
Figure 4.
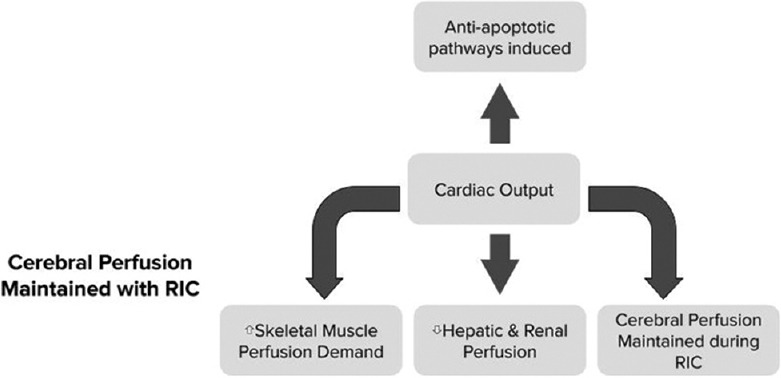
Acute phase of stroke and the mechanism of remote ischemic conditioning
Additional considerations for exercise therapy
Although this review has focused on dys-autoregulation as a possible source of exercise’s detriment in the very early stages of acute ischemic stroke, the reality is likely more complex. Calcium overload[104] and ATP depletion[105] after exercise are clearly counterproductive to acute ischemic stroke therapy. Glutamate excitotoxicity is also a detrimental consequence of exercise to stroke patients;[106,107] however, these were observed only in intense exercise,[108,109] while mild exercise proved to decrease glutamate levels.[110,111,112] ROS production with exercise contributes to oxidative damage,[113,114] but counterintuitively the same oxidative stress is seen to benefit patients with neurodegenerative diseases.[115] Moderate exercise decreases pro-inflammatory cytokines such as tumor necrosis factor-alpha, interleukin-6 (IL-6), IL-1 beta (IL-1 β), and C-reactive protein, while intense exercise increased them.[116] On a similar note, muscle damage increases both inflammation and white blood cell recruitment,[117] which was believed to be only detrimental. However, recent evidence points to microglia/macrophage polarization, in which some populations contribute to the tissue damage, while others assist in clearing cellular debris and facilitate neuronal restoration.[118]
As more research is conducted to better understand exercise’s role in acute ischemic stroke therapy, improved models of its interaction with the damaged and recovering brain are beneficial for discovering alternative treatment modalities and understanding stroke pathophysiology.
Conclusion
Although exercise has proven to be therapeutic for patients with acute ischemic stroke, it is harmful when implemented within 24 h of the ischemic event. RIC is another stroke therapy that is not used as widely. Exercise and RIC both induce ameliorative effects through similar mechanisms during the subacute phase of stroke, primarily through promoting neuroprotection, angiogenesis, and apoptosis inhibition. During the acute phase, tissue death and injury are caused by the ischemic event initiating a series of events consequent to lack of perfusion and ATP depletion. Injury during the acute phase may be aggravated by cerebral dys-autoregulation, a phenomenon observable in many types of injuries to the cranium. Exercise perturbs the cardiovascular physiology, causing hyper or hypoperfusion of the brain during cerebral dys-autoregulation. This combination may explain the reason for exercise’s deleterious effect during the first 24 h following the ischemic event. Meanwhile, RIC does not cause significant changes to the brain’s circulation during its dys-autoregulation. Because RIC is therapeutic through the same mechanisms as exercise without causing harm, RIC may be the suitable candidate for stroke therapy during the first 24 h following an ischemic event, followed by exercise therapy several days afterward. Together, RIC and exercise therapy may induce additive, if not synergistic, amelioration for acute ischemic stroke patients.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Yuchuan Ding is an Associate Editor of Brain Circulation. The article was subject to the journal’s standard procedures, with peer review handled independently of this Editor and their research groups.
Acknowledgment
The authors thank Yoke Ping Khoo Lee for formatting the figures.
References
- 1.Knecht T, Borlongan C, Dela Peña I. Combination therapy for ischemic stroke: Novel approaches to lengthen therapeutic window of tissue plasminogen activator. Brain Circ. 2018;4:99–108. doi: 10.4103/bc.bc_21_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma Y, Liu Y, Zhang Z, Yang GY. Significance of complement system in ischemic stroke: A comprehensive review. Aging Dis. 2019;10:429–62. doi: 10.14336/AD.2019.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen G, Cercy K, Johnson CO, Alam T, et al. GBD 2016 Lifetime Risk of Stroke Collaborators; Feigin VL. Global, Regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379:2429–37. doi: 10.1056/NEJMoa1804492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: A report from the American Heart Association. Circulation. 2021;143:e254–743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 5.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 6.Rabinstein AA. Update on treatment of acute ischemic stroke. Continuum (Minneap Minn) 2020;26:268–86. doi: 10.1212/CON.0000000000000840. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults – United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–6. [PubMed] [Google Scholar]
- 8.Zhang P, Zhang Q, Pu H, Wu Y, Bai Y, Vosler PS, et al. Very early-initiated physical rehabilitation protects against ischemic brain injury. Front Biosci (Elite Ed) 2012;4:2476–89. doi: 10.2741/e559. [DOI] [PubMed] [Google Scholar]
- 9.Anthony SS, Date I, Yasuhara T. Limiting exercise inhibits neuronal recovery from neurological disorders. Brain Circ. 2017;3:124–9. doi: 10.4103/bc.bc_16_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Y, Zhang P, Shen X, Tian S, Wu Y, Zhu Y, et al. Early exercise protects the blood-brain barrier from ischemic brain injury via the regulation of MMP-9 and occludin in rats. Int J Mol Sci. 2013;14:11096–112. doi: 10.3390/ijms140611096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terashi T, Otsuka S, Takada S, Nakanishi K, Ueda K, Sumizono M, et al. Neuroprotective effects of different frequency preconditioning exercise on neuronal apoptosis after focal brain ischemia in rats. Neurol Res. 2019;41:510–8. doi: 10.1080/01616412.2019.1580458. [DOI] [PubMed] [Google Scholar]
- 12.Pan X, Jiang T, Zhang L, Zheng H, Luo J, Hu X. Physical exercise promotes novel object recognition memory in spontaneously hypertensive rats after ischemic stroke by promoting neural plasticity in the entorhinal cortex. Front Behav Neurosci. 2017;11:185. doi: 10.3389/fnbeh.2017.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hatem SM, Saussez G, Della Faille M, Prist V, Zhang X, Dispa D, et al. Rehabilitation of motor function after stroke: A multiple systematic review focused on techniques to stimulate upper extremity recovery. Front Hum Neurosci. 2016;10:1–22442. doi: 10.3389/fnhum.2016.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pin-Barre C, Laurin J. Physical exercise as a diagnostic, rehabilitation, and preventive tool: Influence on neuroplasticity and motor recovery after stroke. Neural Plast 2015. 2015 doi: 10.1155/2015/608581. 608581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang F, Zhang S, Zhou F, Zhao M, Zhao H. Early physical rehabilitation therapy between 24 and 48h following acute ischemic stroke onset: A randomized controlled trial. Disabil Rehabil. 2021;44:1–6. doi: 10.1080/09638288.2021.1897168. [doi: 10.1080/09638288.2021.1897168] [DOI] [PubMed] [Google Scholar]
- 16.Correction to: Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e440–1. doi: 10.1161/STR.0000000000000215. [DOI] [PubMed] [Google Scholar]
- 17.AVERT Trial Collaboration group. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): A randomised controlled trial. Lancet. 2015;386:46–55. doi: 10.1016/S0140-6736(15)60690-0. [DOI] [PubMed] [Google Scholar]
- 18.Saunders DH, Greig CA, Mead GE. Physical activity and exercise after stroke: Review of multiple meaningful benefits. Stroke. 2014;45:3742–7. doi: 10.1161/STROKEAHA.114.004311. [DOI] [PubMed] [Google Scholar]
- 19.Moretti A, Ferrari F, Villa RF. Neuroprotection for ischaemic stroke: Current status and challenges. Pharmacol Ther. 2015;146:23–34. doi: 10.1016/j.pharmthera.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Zhu T, Zhan L, Liang D, Hu J, Lu Z, Zhu X, et al. Hypoxia-inducible factor 1α mediates neuroprotection of hypoxic postconditioning against global cerebral ischemia. J Neuropathol Exp Neurol. 2014;73:975–86. doi: 10.1097/NEN.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 21.Ramagiri S, Taliyan R. Remote limb ischemic post conditioning during early reperfusion alleviates cerebral ischemic reperfusion injury via GSK-3β/CREB/BDNF pathway. Eur J Pharmacol. 2017;803:84–93. doi: 10.1016/j.ejphar.2017.03.028. [DOI] [PubMed] [Google Scholar]
- 22.Rapisarda V, Ledda C, Matera S, Fago L, Arrabito G, Falzone L, et al. Absence of t (14;18) chromosome translocation in agricultural workers after short-term exposure to pesticides. Mol Med Rep. 2017;15:3379–82. doi: 10.3892/mmr.2017.6385. [DOI] [PubMed] [Google Scholar]
- 23.Meng R, Ding Y, Asmaro K, Brogan D, Meng L, Sui M, et al. Ischemic conditioning is safe and effective for Octo- and nonagenarians in stroke prevention and treatment. Neurotherapeutics. 2015;12:667–77. doi: 10.1007/s13311-015-0358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao W, Meng R, Ma C, Hou B, Jiao L, Zhu F, et al. Safety and efficacy of remote ischemic preconditioning in patients with severe carotid artery stenosis before carotid artery stenting: A proof-of-concept, randomized controlled trial. Circulation. 2017;135:1325–35. doi: 10.1161/CIRCULATIONAHA.116.024807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Randhawa PK, Bali A, Jaggi AS. RIPC for multiorgan salvage in clinical settings: Evolution of concept, evidences and mechanisms. Eur J Pharmacol. 2015;746:317–32. doi: 10.1016/j.ejphar.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 26.Koch S, Katsnelson M, Dong C, Perez-Pinzon M. Remote ischemic limb preconditioning after subarachnoid hemorrhage: A phase Ib study of safety and feasibility. Stroke. 2011;42:1387–91. doi: 10.1161/STROKEAHA.110.605840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Q, Wills M, Han Z, Geng X, Ding Y. Mini review (Part I): An experimental concept on exercise and ischemic conditioning in stroke rehabilitation. Brain Circ. 2020;6:242–7. doi: 10.4103/bc.bc_63_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L, Ren C, Li Y, Gao C, Li N, Li H, et al. Remote ischemic conditioning enhances oxygen supply to ischemic brain tissue in a mouse model of stroke: Role of elevated 2,3-biphosphoglycerate in erythrocytes. J Cereb blood flow Metab. 2020;41:1277–90. doi: 10.1177/0271678X20952264. [doi: 10.1177/0271678×20952264] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basalay MV, Wiart M, Chauveau F, Dumot C, Leon C, Amaz C, et al. Neuroprotection by remote ischemic conditioning in the setting of acute ischemic stroke: A preclinical two-centre study. Sci Rep. 2020;10:16874. doi: 10.1038/s41598-020-74046-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weir P, Maguire R, O’Sullivan SE, England TJ. A meta-analysis of remote ischaemic conditioning in experimental stroke. J Cereb Blood Flow Metab. 2021;41:3–13. doi: 10.1177/0271678X20924077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao W, Li S, Ren C, Meng R, Ji X. Chronic remote ischemic conditioning may mimic regular exercise: Perspective from clinical studies. Aging Dis. 2018;9:165–71. doi: 10.14336/AD.2017.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Geng X, Wang Q, Lee H, Huber C, Wills M, Elkin K, et al. Remote ischemic postconditioning vs. Physical exercise after stroke: An alternative rehabilitation strategy? Mol Neurobiol. 2021;58:3141–57. doi: 10.1007/s12035-021-02329-6. [doi: 10.1007/s12035-021-02329-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li S, Han C, Asmaro K, Quan S, Li M, Ren C, et al. Remote ischemic conditioning improves attention network function and blood oxygen levels in unacclimatized adults exposed to high altitude. Aging Dis. 2020;11:820–7. doi: 10.14336/AD.2019.0605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kurisu K, Yenari MA. Therapeutic hypothermia for ischemic stroke; pathophysiology and future promise. Neuropharmacology. 2018;134:302–9. doi: 10.1016/j.neuropharm.2017.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernhardt J, English C, Johnson L, Cumming TB. Early mobilization after stroke: Early adoption but limited evidence. Stroke. 2015;46:1141–6. doi: 10.1161/STROKEAHA.114.007434. [DOI] [PubMed] [Google Scholar]
- 36.Gamdzyk M, Makarewicz D, Słomka M, Ziembowicz A, Salinska E. Hypobaric hypoxia postconditioning reduces brain damage and improves antioxidative defense in the model of birth asphyxia in 7-day-old rats. Neurochem Res. 2014;39:68–75. doi: 10.1007/s11064-013-1191-0. [DOI] [PubMed] [Google Scholar]
- 37.Zhu P, Zhan L, Zhu T, Liang D, Hu J, Sun W, et al. The roles of p38 MAPK/MSK1 signaling pathway in the neuroprotection of hypoxic postconditioning against transient global cerebral ischemia in adult rats. Mol Neurobiol. 2014;49:1338–49. doi: 10.1007/s12035-013-8611-7. [DOI] [PubMed] [Google Scholar]
- 38.Staat P, Rioufol G, Piot C, Cottin Y, Cung TT, L’Huillier I, et al. Postconditioning the human heart. Circulation. 2005;112:2143–8. doi: 10.1161/CIRCULATIONAHA.105.558122. [DOI] [PubMed] [Google Scholar]
- 39.Liao Z, Bu Y, Li M, Han R, Zhang N, Hao J, et al. Remote ischemic conditioning improves cognition in patients with subcortical ischemic vascular dementia. BMC Neurol. 2019;19:206. doi: 10.1186/s12883-019-1435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Durand MJ, Boerger TF, Nguyen JN, Alqahtani SZ, Wright MT, Schmit BD, et al. Two weeks of ischemic conditioning improves walking speed and reduces neuromuscular fatigability in chronic stroke survivors. J Appl Physiol (1985) 2019;126:755–63. doi: 10.1152/japplphysiol.00772.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ren C, Wang P, Wang B, Li N, Li W, Zhang C, et al. Limb remote ischemic per-conditioning in combination with post-conditioning reduces brain damage and promotes neuroglobin expression in the rat brain after ischemic stroke. Restor Neurol Neurosci. 2015;33:369–79. doi: 10.3233/RNN-140413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esposito E, Hayakawa K, Maki T, Arai K, Lo EH. Effects of postconditioning on neurogenesis and angiogenesis during the recovery phase after focal cerebral ischemia. Stroke. 2015;46:2691–4. doi: 10.1161/STROKEAHA.115.009070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hougaard KD, Hjort N, Zeidler D, Sørensen L, Nørgaard A, Hansen TM, et al. Remote ischemic perconditioning as an adjunct therapy to thrombolysis in patients with acute ischemic stroke: A randomized trial. Stroke. 2014;45:159–67. doi: 10.1161/STROKEAHA.113.001346. [DOI] [PubMed] [Google Scholar]
- 44.Meng R, Asmaro K, Meng L, Liu Y, Ma C, Xi C, et al. Upper limb ischemic preconditioning prevents recurrent stroke in intracranial arterial stenosis. Neurology. 2012;79:1853–61. doi: 10.1212/WNL.0b013e318271f76a. [DOI] [PubMed] [Google Scholar]
- 45.Liu X, Sha O, Cho EY. Remote ischemic postconditioning promotes the survival of retinal ganglion cells after optic nerve injury. J Mol Neurosci. 2013;51:639–46. doi: 10.1007/s12031-013-0036-2. [DOI] [PubMed] [Google Scholar]
- 46.Gao X, Liu Y, Xie Y, Wang Y, Qi S. Remote ischemic postconditioning confers neuroprotective effects via inhibition of the BID-mediated mitochondrial apoptotic pathway. Mol Med Rep. 2017;16:515–22. doi: 10.3892/mmr.2017.6652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang P, Zhang Y, Zhang J, Wu Y, Jia J, Wu J, et al. Early exercise protects against cerebral ischemic injury through inhibiting neuron apoptosis in cortex in rats. Int J Mol Sci. 2013;14:6074–89. doi: 10.3390/ijms14036074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cheng Z, Li L, Mo X, Zhang L, Xie Y, Guo Q, et al. Non-invasive remote limb ischemic postconditioning protects rats against focal cerebral ischemia by upregulating STAT3 and reducing apoptosis. Int J Mol Med. 2014;34:957–66. doi: 10.3892/ijmm.2014.1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Song SH, Jee YS, Ko IG, Lee SW, Sim YJ, Kim DY, et al. Treadmill exercise and wheel exercise improve motor function by suppressing apoptotic neuronal cell death in brain inflammation rats. J Exerc Rehabil. 2018;14:911–9. doi: 10.12965/jer.1836508.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jang S, Yayeh T, Leem YH, Park EM, Ito Y, Oh S. Concanavalin a induces cortical neuron apoptosis by causing ROS accumulation and tyrosine kinase activation. Neurochem Res. 2017;42:3504–14. doi: 10.1007/s11064-017-2398-2. [DOI] [PubMed] [Google Scholar]
- 51.Lennon SL, Quindry J, Hamilton KL, French J, Staib J, Mehta JL, et al. Loss of exercise-induced cardioprotection after cessation of exercise. J Appl Physiol (1985) 2004;96:1299–305. doi: 10.1152/japplphysiol.00920.2003. [DOI] [PubMed] [Google Scholar]
- 52.Frasier CR, Moukdar F, Patel HD, Sloan RC, Stewart LM, Alleman RJ, et al. Redox-dependent increases in glutathione reductase and exercise preconditioning: role of NADPH oxidase and mitochondria. Cardiovasc Res. 2013;98:47–55. doi: 10.1093/cvr/cvt009. [DOI] [PubMed] [Google Scholar]
- 53.Morihira M, Hasebe N, Baljinnyam E, Sumitomo K, Matsusaka T, Izawa K, et al. Ischemic preconditioning enhances scavenging activity of reactive oxygen species and diminishes transmural difference of infarct size. Am J Physiol Heart Circ Physiol. 2006;290:H577–83. doi: 10.1152/ajpheart.00817.2004. [DOI] [PubMed] [Google Scholar]
- 54.Dong HL, Zhang Y, Su BX, Zhu ZH, Gu QH, Sang HF, et al. Limb remote ischemic preconditioning protects the spinal cord from ischemia-reperfusion injury: A newly identified nonneuronal but reactive oxygen species-dependent pathway. Anesthesiology. 2010;112:881–91. doi: 10.1097/ALN.0b013e3181d0486d. [DOI] [PubMed] [Google Scholar]
- 55.Pluta RM, Rak R, Wink DA, Woodward JJ, Khaldi A, Oldfield EH, et al. Effects of nitric oxide on reactive oxygen species production and infarction size after brain reperfusion injury. Neurosurgery. 2001;48:884–92. doi: 10.1097/00006123-200104000-00039. [DOI] [PubMed] [Google Scholar]
- 56.Hambrecht R, Adams V, Erbs S, Linke A, Kränkel N, Shu Y, et al. Regular physical activity improves endothelial function in patients with coronary artery disease by increasing phosphorylation of endothelial nitric oxide synthase. Circulation. 2003;107:3152–8. doi: 10.1161/01.CIR.0000074229.93804.5C. [DOI] [PubMed] [Google Scholar]
- 57.Liang Y, Li YP, He F, Liu XQ, Zhang JY. Long-term, regular remote ischemic preconditioning improves endothelial function in patients with coronary heart disease. Braz J Med Biol Res. 2015;48:568–76. doi: 10.1590/1414-431X20144452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang CJ, Wu Y, Zhang Q, Yu KW, Wang YY. An enriched environment promotes synaptic plasticity and cognitive recovery after permanent middle cerebral artery occlusion in mice. Neural Regen Res. 2019;14:462–9. doi: 10.4103/1673-5374.245470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hulsebosch CE, DeWitt DS, Jenkins LW, Prough DS. Traumatic brain injury in rats results in increased expression of Gap-43 that correlates with behavioral recovery. Neurosci Lett. 1998;255:83–6. doi: 10.1016/s0304-3940(98)00712-5. [DOI] [PubMed] [Google Scholar]
- 60.Liu W, Xue X, Xia J, Liu J, Qi Z. Swimming exercise reverses CUMS-induced changes in depression-like behaviors and hippocampal plasticity-related proteins. J Affect Disord. 2018;227:126–35. doi: 10.1016/j.jad.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 61.Sharma P, Kumar A, Singh D. Dietary flavonoids interaction with CREB-BDNF pathway: An unconventional approach for comprehensive management of epilepsy. Curr Neuropharmacol. 2019;17:1158–75. doi: 10.2174/1570159X17666190809165549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Almeida AA, Gomes da Silva S, Lopim GM, Vannucci Campos D, Fernandes J, Cabral FR, et al. Physical exercise alters the activation of downstream proteins related to BDNF-TrkB signaling in male Wistar rats with epilepsy. J Neurosci Res. 2018;96:911–20. doi: 10.1002/jnr.24196. [DOI] [PubMed] [Google Scholar]
- 63.Motaghinejad O, Motaghinejad M, Motevalian M, Rahimi-Sharbaf F, Beiranvand T. The effect of maternal forced exercise on offspring pain perception, motor activity and anxiety disorder: The role of 5-HT2 and D2 receptors and CREB gene expression. J Exerc Rehabil. 2017;13:514–25. doi: 10.12965/jer.1734992.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pietrelli A, Matković L, Vacotto M, Lopez-Costa JJ, Basso N, Brusco A. Aerobic exercise upregulates the BDNF-Serotonin systems and improves the cognitive function in rats. Neurobiol Learn Mem. 2018;155:528–42. doi: 10.1016/j.nlm.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 65.Luo CX, Jiang J, Zhou QG, Zhu XJ, Wang W, Zhang ZJ, et al. Voluntary exercise-induced neurogenesis in the postischemic dentate gyrus is associated with spatial memory recovery from stroke. J Neurosci Res. 2007;85:1637–46. doi: 10.1002/jnr.21317. [DOI] [PubMed] [Google Scholar]
- 66.Caracciolo L, Marosi M, Mazzitelli J, Latifi S, Sano Y, Galvan L, et al. CREB controls cortical circuit plasticity and functional recovery after stroke. Nat Commun. 2018;9:2250. doi: 10.1038/s41467-018-04445-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang J, Liu Z, Pei Y, Yang W, Xie C, Long S. MicroRNA-322 cluster promotes tau phosphorylation via targeting brain-derived neurotrophic factor. Neurochem Res. 2018;43:736–44. doi: 10.1007/s11064-018-2475-1. [DOI] [PubMed] [Google Scholar]
- 68.Ahn SM, Kim YR, Shin YI, Ha KT, Lee SY, Shin HK, et al. Therapeutic potential of a combination of electroacupuncture and TrkB-expressing mesenchymal stem cells for ischemic stroke. Mol Neurobiol. 2019;56:157–73. doi: 10.1007/s12035-018-1067-z. [DOI] [PubMed] [Google Scholar]
- 69.Tejeda GS, Díaz-Guerra M. Integral characterization of defective BDNF/TrkB signalling in neurological and psychiatric disorders leads the way to new therapies. Int J Mol Sci. 2017;18:268. doi: 10.3390/ijms18020268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kermani P, Hempstead B. Brain-derived neurotrophic factor: A newly described mediator of angiogenesis. Trends Cardiovasc Med. 2007;17:140–3. doi: 10.1016/j.tcm.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Waterhouse EG, Xu B. New insights into the role of brain-derived neurotrophic factor in synaptic plasticity. Mol Cell Neurosci. 2009;42:81–9. doi: 10.1016/j.mcn.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li S, Hafeez A, Noorulla F, Geng X, Shao G, Ren C, et al. Preconditioning in neuroprotection: From hypoxia to ischemia. Prog Neurobiol. 2017;157:79–91. doi: 10.1016/j.pneurobio.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Merelli A, Rodríguez JCG, Folch J, Regueiro MR, Camins A, Lazarowski A. Understanding the role of hypoxia inducible factor during neurodegeneration for new therapeutics opportunities. Curr Neuropharmacol. 2018;16:1484–98. doi: 10.2174/1570159X16666180110130253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sharp FR, Bernaudin M. HIF1 and oxygen sensing in the brain. Nat Rev Neurosci. 2004;5:437–48. doi: 10.1038/nrn1408. [DOI] [PubMed] [Google Scholar]
- 75.Guo Y, Feng L, Zhou Y, Sheng J, Long D, Li S, et al. Systematic review with meta-analysis: HIF-1α attenuates liver ischemia-reperfusion injury. Transplant Rev (Orlando) 2015;29:127–34. doi: 10.1016/j.trre.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 76.Hummitzsch L, Zitta K, Berndt R, Wong YL, Rusch R, Hess K, et al. Remote ischemic preconditioning attenuates intestinal mucosal damage: Insight from a rat model of ischemia-reperfusion injury. J Transl Med. 2019;17:136. doi: 10.1186/s12967-019-1885-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Halliday MR, Abeydeera D, Lundquist AJ, Petzinger GM, Jakowec MW. Intensive treadmill exercise increases expression of hypoxia-inducible factor 1α and its downstream transcript targets: A potential role in neuroplasticity. Neuroreport. 2019;30:619–27. doi: 10.1097/WNR.0000000000001239. [DOI] [PubMed] [Google Scholar]
- 78.Li F, Geng X, Huber C, Stone C, Ding Y. In search of a dose: The functional and molecular effects of exercise on post-stroke rehabilitation in rats. Front Cell Neurosci. 2020;14:186. doi: 10.3389/fncel.2020.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Armstead WM. Cerebral blood flow autoregulation and dysautoregulation. Anesthesiol Clin. 2016;34:465–77. doi: 10.1016/j.anclin.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rangel-Castilla L, Gasco J, Nauta HJ, Okonkwo DO, Robertson CS. Cerebral pressure autoregulation in traumatic brain injury. Neurosurg Focus. 2008;25:E7. doi: 10.3171/FOC.2008.25.10.E7. [DOI] [PubMed] [Google Scholar]
- 81.Prabhakaran S, Naidech AM. Ischemic brain injury after intracerebral hemorrhage: A critical review. Stroke. 2012;43:2258–63. doi: 10.1161/STROKEAHA.112.655910. [DOI] [PubMed] [Google Scholar]
- 82.Immink RV, van Montfrans GA, Stam J, Karemaker JM, Diamant M, van Lieshout JJ. Dynamic cerebral autoregulation in acute lacunar and middle cerebral artery territory ischemic stroke. Stroke. 2005;36:2595–600. doi: 10.1161/01.STR.0000189624.06836.03. [DOI] [PubMed] [Google Scholar]
- 83.Castro P, Azevedo E, Serrador J, Rocha I, Sorond F. Hemorrhagic transformation and cerebral edema in acute ischemic stroke: Link to cerebral autoregulation. J Neurol Sci. 2017;372:256–61. doi: 10.1016/j.jns.2016.11.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aoi MC, Hu K, Lo MT, Selim M, Olufsen MS, Novak V. Impaired cerebral autoregulation is associated with brain atrophy and worse functional status in chronic ischemic stroke. PLoS One. 2012;7:e46794. doi: 10.1371/journal.pone.0046794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Reinhard M, Rutsch S, Lambeck J, Wihler C, Czosnyka M, Weiller C, et al. Dynamic cerebral autoregulation associates with infarct size and outcome after ischemic stroke. Acta Neurol Scand. 2012;125:156–62. doi: 10.1111/j.1600-0404.2011.01515.x. [DOI] [PubMed] [Google Scholar]
- 86.Ma H, Guo ZN, Jin H, Yan X, Liu J, Lv S, et al. Preliminary study of dynamic cerebral autoregulation in acute ischemic stroke: Association with clinical factors. Front Neurol. 2018;9:1006. doi: 10.3389/fneur.2018.01006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Reinhard M, Wihler C, Roth M, Harloff A, Niesen WD, Timmer J, et al. Cerebral autoregulation dynamics in acute ischemic stroke after rtPA thrombolysis. Cerebrovasc Dis. 2008;26:147–55. doi: 10.1159/000139662. [DOI] [PubMed] [Google Scholar]
- 88.Armstead WM, Riley J, Yarovoi S, Higazi AA, Cines DB. Tissue-type plasminogen activator-A296-299 prevents impairment of cerebral autoregulation after stroke through lipoprotein-related receptor-dependent increase in cAMP and p38. Stroke. 2016;47:2096–102. doi: 10.1161/STROKEAHA.116.012678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Armstead WM, Riley J, Kiessling JW, Cines DB, Higazi AA. Novel plasminogen activator inhibitor-1-derived peptide protects against impairment of cerebrovasodilation after photothrombosis through inhibition of JNK MAPK. Am J Physiol Regul Integr Comp Physiol. 2010;299:R480–5. doi: 10.1152/ajpregu.00256.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Reinhard M, Roth M, Guschlbauer B, Harloff A, Timmer J, Czosnyka M, et al. Dynamic cerebral autoregulation in acute ischemic stroke assessed from spontaneous blood pressure fluctuations. Stroke. 2005;36:1684–9. doi: 10.1161/01.STR.0000173183.36331.ee. [DOI] [PubMed] [Google Scholar]
- 91.Hu K, Peng CK, Czosnyka M, Zhao P, Novak V. Nonlinear assessment of cerebral autoregulation from spontaneous blood pressure and cerebral blood flow fluctuations. Cardiovasc Eng. 2008;8:60–71. doi: 10.1007/s10558-007-9045-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Joyner MJ, Casey DP. Regulation of increased blood flow (hyperemia) to muscles during exercise: A hierarchy of competing physiological needs. Physiol Rev. 2015;95:549–601. doi: 10.1152/physrev.00035.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Smith KJ, Ainslie PN. Regulation of cerebral blood flow and metabolism during exercise. Exp Physiol. 2017;102:1356–71. doi: 10.1113/EP086249. [DOI] [PubMed] [Google Scholar]
- 94.Carmo-Araújo EM, Dal-Pai-Silva M, Dal-Pai V, Cecchini R, Anjos Ferreira AL. Ischaemia and reperfusion effects on skeletal muscle tissue: morphological and histochemical studies. Int J Exp Pathol. 2007;88:147–54. doi: 10.1111/j.1365-2613.2007.00526.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Day RL, Zale BW. The effect of tourniquets on muscle enzymes during foot and ankle surgery. J Foot Ankle Surg. 1993;32:280–5. [PubMed] [Google Scholar]
- 96.Estebe JP, Mallédant Y. Pneumatic tourniquets in orthopedics. Ann Fr Anesth Reanim. 1996;15:162–78. doi: 10.1016/0750-7658(96)85038-6. [DOI] [PubMed] [Google Scholar]
- 97.Lin LN, Wang LR, Wang WT, Jin LL, Zhao XY, Zheng LP, et al. Ischemic preconditioning attenuates pulmonary dysfunction after unilateral thigh tourniquet-induced ischemia-reperfusion. Anesth Analg. 2010;111:539–43. doi: 10.1213/ANE.0b013e3181e368d2. [DOI] [PubMed] [Google Scholar]
- 98.Kanoria S, Jalan R, Davies NA, Seifalian AM, Williams R, Davidson BR. Remote ischaemic preconditioning of the hind limb reduces experimental liver warm ischaemia-reperfusion injury. Br J Surg. 2006;93:762–8. doi: 10.1002/bjs.5331. [DOI] [PubMed] [Google Scholar]
- 99.Jiang X, Ai C, Shi E, Nakajima Y, Ma H. Neuroprotection against spinal cord ischemia-reperfusion injury induced by different ischemic postconditioning methods: Roles of phosphatidylinositol 3-kinase-Akt and extracellular signal-regulated kinase. Anesthesiology. 2009;111:1197–205. doi: 10.1097/ALN.0b013e3181bf1d93. [DOI] [PubMed] [Google Scholar]
- 100.Loukogeorgakis SP, Williams R, Panagiotidou AT, Kolvekar SK, Donald A, Cole TJ, et al. Transient limb ischemia induces remote preconditioning and remote postconditioning in humans by a K (ATP)-channel dependent mechanism. Circulation. 2007;116:1386–95. doi: 10.1161/CIRCULATIONAHA.106.653782. [DOI] [PubMed] [Google Scholar]
- 101.Zhao W, Che R, Li S, Ren C, Li C, Wu C, et al. Remote ischemic conditioning for acute stroke patients treated with thrombectomy. Ann Clin Transl Neurol. 2018;5:850–6. doi: 10.1002/acn3.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li S, Ma C, Shao G, Esmail F, Hua Y, Jia L, et al. Safety and feasibility of remote limb ischemic preconditioning in patients with unilateral middle cerebral artery stenosis and healthy volunteers. Cell Transplant. 2015;24:1901–11. doi: 10.3727/096368914X683520. [DOI] [PubMed] [Google Scholar]
- 103.Mi T, Yu F, Ji X, Sun Y, Qu D. The interventional effect of remote ischemic preconditioning on cerebral small vessel disease: A pilot randomized clinical trial. Eur Neurol. 2016;76:28–34. doi: 10.1159/000447536. [DOI] [PubMed] [Google Scholar]
- 104.Ding Y, Chang C, Xie L, Chen Z, Ai H. Intense exercise can cause excessive apoptosis and synapse plasticity damage in rat hippocampus through Ca2+overload and endoplasmic reticulum stress-induced apoptosis pathway. Chin Med J (Engl) 2014;127:3265–71. [PubMed] [Google Scholar]
- 105.Hargreaves M, Spriet LL. Exercise metabolism: Fuels for the fire. Cold Spring Harb Perspect Med. 2018;8:a029744. doi: 10.1101/cshperspect.a029744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mahmoud S, Gharagozloo M, Simard C, Gris D. Astrocytes maintain glutamate homeostasis in the CNS by controlling the balance between glutamate uptake and release. Cells. 2019;8:184. doi: 10.3390/cells8020184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lau A, Tymianski M. Glutamate receptors, neurotoxicity and neurodegeneration. Pflugers Arch. 2010;460:525–42. doi: 10.1007/s00424-010-0809-1. [DOI] [PubMed] [Google Scholar]
- 108.Guezennec CY, Abdelmalki A, Serrurier B, Merino D, Bigard X, Berthelot M, et al. Effects of prolonged exercise on brain ammonia and amino acids. Int J Sports Med. 1998;19:323–7. doi: 10.1055/s-2007-971925. [DOI] [PubMed] [Google Scholar]
- 109.Maddock RJ, Casazza GA, Fernandez DH, Maddock MI. Acute modulation of cortical glutamate and GABA content by physical activity. J Neurosci. 2016;36:2449–57. doi: 10.1523/JNEUROSCI.3455-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cheng A, Yang Y, Zhou Y, Maharana C, Lu D, Peng W, et al. Mitochondrial SIRT3 mediates adaptive responses of neurons to exercise and metabolic and excitatory challenges. Cell Metab. 2016;23:128–42. doi: 10.1016/j.cmet.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Goldshmit Y, Banyas E, Bens N, Yakovchuk A, Ruban A. Blood glutamate scavengers and exercises as an effective neuroprotective treatment in mice with spinal cord injury. J Neurosurg Spine. 2020;33:692–704. doi: 10.3171/2020.4.SPINE20302. [doi: 10.3171/2020.4.SPINE20302] [DOI] [PubMed] [Google Scholar]
- 112.Mourão FA, Leite HR, de Carvalho LE, Vieira TH, Pinto MC, de Castro Medeiros D, et al. Neuroprotective effect of exercise in rat hippocampal slices submitted to in vitro ischemia is promoted by decrease of glutamate release and pro-apoptotic markers. J Neurochem. 2014;131:65–73. doi: 10.1111/jnc.12786. [DOI] [PubMed] [Google Scholar]
- 113.Block ML, Zecca L, Hong JS. Microglia-mediated neurotoxicity: Uncovering the molecular mechanisms. Nat Rev Neurosci. 2007;8:57–69. doi: 10.1038/nrn2038. [DOI] [PubMed] [Google Scholar]
- 114.Huang B, Chen Q, Wang L, Gao X, Zhu W, Mu P, et al. Aflatoxin B1 induces neurotoxicity through reactive oxygen species generation, DNA damage, apoptosis, and S-phase cell cycle arrest. Int J Mol Sci. 2020;21:6517. doi: 10.3390/ijms21186517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Powers SK, Deminice R, Ozdemir M, Yoshihara T, Bomkamp MP, Hyatt H. Exercise-induced oxidative stress: Friend or foe? J Sport Health Sci. 2020;9:415–25. doi: 10.1016/j.jshs.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Paolucci EM, Loukov D, Bowdish DME, Heisz JJ. Exercise reduces depression and inflammation but intensity matters. Biol Psychol. 2018;133:79–84. doi: 10.1016/j.biopsycho.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 117.Paulsen G, Mikkelsen UR, Raastad T, Peake JM. Leucocytes, cytokines and satellite cells: What role do they play in muscle damage and regeneration following eccentric exercise? Exerc Immunol Rev. 2012;18:42–97. [PubMed] [Google Scholar]
- 118.Hu X, Leak RK, Shi Y, Suenaga J, Gao Y, Zheng P, et al. Microglial and macrophage polarization – New prospects for brain repair. Nat Rev Neurol. 2015;11:56–64. doi: 10.1038/nrneurol.2014.207. [DOI] [PMC free article] [PubMed] [Google Scholar]


