1. Introduction
About 13% of American adults currently have an alcohol use disorder (AUD), including 12% of Latinos (Grant et al., 2017). AUD, marked by uncontrolled alcohol use and significant alcohol-related distress or problems, is associated with a number of poor health outcomes (Rehm et al., 2014; Room et al., 2005). The U.S.-Mexico border region, including within 100km of the international border (Office of Global Affairs (OGA), 2017), has unique alcohol use patterns and risk factors, including increased availability of alcohol due to its proximity to Mexico (Caetano et al., 2013), permissive alcohol norms, and border-related social stressors (Zemore et al., 2016).
Practitioners can implement treatment for AUD across a variety of clinical settings, from inpatient hospitalization to care delivered in primary care and other outpatient settings. Alcohol treatment can decrease alcohol use, decrease AUD symptoms, and promote abstinence among Latinos when implemented in an accessible and culturally sensitive way (Marsh et al., 2009). For those with AUD, research recommends specialty alcohol treatment (i.e., treatment provided at a specialty facility, including hospital, rehabilitation facility, or mental health center; Weisner et al., 2003). However, rates of alcohol treatment utilization, including in specialty care, are very low for all Americans (Cohen et al., 2007).
Utilization of specialty care is particularly limited among Latinos (Guerrero, Marsh, Duan, et al., 2013; Guerrero, Marsh, Khachikian, et al., 2013). Across the U.S., about 19% of Latinos with alcohol dependence reported lifetime receipt of alcohol-related care, with only 6% receiving treatment in a specialty alcohol treatment program (Zemore et al., 2009, 2014). Even among those linked with care within a healthcare system—the Veterans Health Administration—less than one-third of Latinos with AUD received specialty treatment within six months of diagnosis (Bensley et al., 2017). However, access to treatment among Latinos in the U.S. is not uniform and may be geographically determined, with some Latino communities having less access to care than others. In the U.S.-Mexico border region access to healthcare is often limited (Ortiz et al., 2004; Su et al., 2011, 2014), including access to alcohol treatment. In one representative study of treatment utilization in the U.S.-Mexico border region, those on the border with a lifetime history of alcohol and drug problems were about half as likely to receive alcohol treatment as those living in nonborder communities (Wallisch et al., 2017). Differences in treatment ecology may explain the differences between treatment utilization for those residing within and outside of the border region.
Treatment ecology, or the physical or social neighborhood characteristics related to treatment seeking, can affect treatment utilization by increasing travel burden or influencing norms about treatment seeking (Jacobson, 2004). These characteristics often create barriers even when treatment is available in a community by limiting accessibility of care. Distance to treatment has been negatively associated with retention in outpatient drug treatment (Beardsley et al., 2003) and with receipt of aftercare following inpatient alcohol treatment (Fortney et al., 1995; Schmitt et al., 2003). While treatment accessibility is broadly related to receipt of healthcare, no studies have specifically assessed whether density of treatment facilities is broadly associated with treatment receipt. Particularly in the U.S.-Mexico border region, given unique alcohol risk factors and differences in receipt of alcohol-related care (Wallisch et al., 2017), alcohol treatment accessibility may help to explain differences observed in receipt of alcohol related care.
Availability of specific types of treatment that improve accessibility, including services offered in Spanish or with fee assistance, may also help to explain differences in treatment utilization in the border region. A study in Los Angeles County examining treatment accessibility for Latinos found that SUD services in Spanish were often located far from Latino neighborhoods (Guerrero et al., 2011; Guerrero, Kao, & Perron, 2013), but we do not know if Spanish-language treatment services in proximity to Latino residents varies between those who reside in communities in the border region relative to nonborder communities. A dearth of treatment options offered in Spanish could help to explain low treatment utilization. Also, for low-income populations, fees associated with treatment may be a barrier to care. In a previous study, low receipt of care on the U.S.-Mexico border was strongly associated with reduced consideration of getting help for alcohol use (Wallisch et al., 2017). However, we do not know whether these differences in treatment accessibility explain border disparities in treatment utilization. Thus, disparities in treatment utilization may be due to differences in proximity to and density of alcohol treatment services within and outside of the border region.
The U.S.-Mexico Study of Alcohol and Related Conditions (UMSARC) surveyed Mexican Americans in two cities in the border region and one city not in the border region in Texas, providing an ideal context in which to study this issue. Texas has a low absolute number of treatment sites and lower relative treatment availability compared to other states (Perron et al., 2010). In this study, we assessed whether differences in treatment utilization between Mexican Americans living in the U.S.-Mexico border region and in a nonborder city were mediated by treatment accessibility We expected to find that spatial accessibility would mediate this association, particularly in the border region. To assess this, we estimated the bivariate association in border status and consideration or receipt of alcohol treatment. For those with significant bivariate association, we tested whether spatial treatment accessibility (i.e., proximity to and density of treatment) mediated differences in consideration or receipt of treatment for those residing within and outside of the border region. We also describe differences between border cities, and associations between covariates and receipt of care outcomes that may explain some of the differences that we found in this study. This paper explores a key explanatory factor describing disparities in alcohol-treatment utilization in Texas and on the U.S.-Mexico border among Mexican Americans.
2. Material and methods
2.1. The UMSARC
We used U.S. data from the UMSARC, a study of Mexican-origin adults surveyed between 2011 and 2013 in three communities in Texas. The UMSARC was the first large-scale survey to assess alcohol and drug use in “sister cities” on the U.S. and Mexico side of the border simultaneously. The Public Policy Institute at Texas A&M University collected surveys in Texas through face-to-face interviews conducted in English or Spanish, with Mexican-origin adults ages 18–65. We used a multistage, area-probability sampling design with stratification by city to select census blocks and then to randomly select respondents within them. We included 792 Mexican American survey participants with lifetime AUD in this study. Participants included respondents from the border cities of Laredo (n = 751) and McAllen/Brownsville (n = 814), and the nonborder city of San Antonio (n = 771). In this paper, we refer to Laredo as Border City A, McAllen/Brownsville as Border City B, and San Antonio as the Non-Border City. All three cities are major metropolitan areas in southern Texas. We compared the two cities in the border region with the one nonborder city, which we used as the referent group, as well as describe differences between the cities in the border region. We have previously published more detailed descriptions of this study and cities used in this study (Cherpitel et al., 2015; Wallisch et al., 2017; Zemore et al., 2016). Our sample included only UMSARC participants with a lifetime history of AUD (see below; n=792).
2.2. Alcohol-related measures
We assessed AUD using self-reported experience of the eleven diagnostic criteria for a DSM-5 diagnosis in one’s lifetime (American Psychiatric Association, 2013). We define AUD as endorsement of 2 or more symptoms (Hasin et al., 2013). We used two dichotomous lifetime measures of self-reported treatment utilization in this study: 1) considering getting help for an alcohol problem and 2) receipt of alcohol treatment. To assess considering getting help, we asked participants, “Have you ever had a problem with your alcohol or drug use for which you thought about getting help?” To assess receipt of treatment, we asked participants, “Have you ever gone to anyone—a physician, AA, a treatment agency, anyone at all—for a problem related in any way to your drinking or drug use?” Because this latter question referred to both receipt of alcohol and drug treatment, we also asked the participants responding “yes” whether treatment was for alcohol use, drug use, or both. Receipt of treatment included participants who reported that they had received treatment for both alcohol and drugs or for alcohol alone. Given the broad nature of the questions that we used to assess consideration of help and treatment receipt, we refer to any kind of help as treatment in this study.
2.3. Predisposing and need characteristics
We considered several factors as covariates because they may confound the associations between border status and alcohol receipt of care outcomes. We selected candidate variables based on a modified version of Andersen’s Behavioral Model of Health Services (Andersen, 1995) that was used in a previous study of treatment disparities in the UMSARC data (Wallisch et al., 2017), including predisposing (e.g., demographics), enabling (e.g., health insurance), and need (e.g., AUD severity) characteristics. A supplementary figure is available online with covariates included as candidates. We then empirically tested associations between candidate variables and receipt of care outcomes using bivariate analyses, with p<0.05 constituting our cutoff for inclusion. We excluded conceptually important variables that were not associated with outcomes in bivariate analyses from the primary models.
The predisposing characteristics that we included in the final model were sex (male or female) and age (18–29, 30–39, 40–49, 50–59, or 60+). Enabling characteristics included marital status (single, married/living together, or separated/divorced/widowed), health insurance (yes or no), annual household income (under $15,000, $15,000–$30,000, $30,000–$60,000, or more than $60,000). There were missing data for health insurance (n=28) and annual household income (n=45) so we created missing categories for these two variables to retain cases in this analysis, due to small sample size. We also included two measures of need in the final model: lifetime AUD severity (mild, with 2–3 symptoms endorsed; moderate, with 4–5 symptoms endorsed; or severe, with 6+ symptoms endorsed), and lifetime drug abuse symptoms based on DSM-IV (no symptoms, 1 symptom, or 2 symptoms) alcohol and drug use disorder criteria (American Psychiatric Association, 2013).
2.4. Spatial accessibility mediating factors
We measured spatial accessibility to treatment by density of treatment and proximity to outpatient treatment. We focused on outpatient treatment, including partial hospitalization or day treatment and other outpatient services. We did not consider inpatient treatment, as there were only a few inpatient treatment facilities in each city and thus accessibility of inpatient treatment did not vary much between participants within each city.
First, we geocoded treatment facilities from the SAMHSA National Directory of Drug and Alcohol Abuse Treatment Facilities and UMSARC participant residence locations. We defined participant residence as the centroid of the census block group including the participant’s residence as reported in the UMSARC survey. Next, we calculated proximity to treatment by estimating travel time using Network Analysis in ArcGIS/ArcMap to the facility nearest to the participant’s residence. This calculated time to nearest outpatient treatment followed roads and took street type into account (e.g., travel time is faster on a highway than on a city street). We measured density of treatment by the number of facilities within a 20-mile radius of the participant’s residence. To decrease bias, we compared each border city independently to the nonborder city.
We evaluated two additional subtypes of treatment options, which we measured in the same way as proximity to and density of outpatient treatment. These two types of treatment were: 1) fee-assisted treatment, including any treatment facilities with programs offering payment assistance, a sliding pay scale, or no-cost access to recovery programs; and 2) Spanish-language treatment, including any facilities offering treatment services provided in Spanish.
2.5. Analysis
Broadly, we assessed whether receipt of care outcomes differed for those with a lifetime history of AUD living in border cities compared to the nonborder city, and whether the association between residing in the border region and receipt of care outcomes were mediated by spatial accessibility of treatment. First, we desbribed demographic factors and AUD severity for the overall sample. Second, we compared prevalence of considering getting help across demographic factors and AUD severity using chi-square tests. Third, for those with a significant overall effect, we assessed indirect effects of each border city on the outcomes mediated through spatial accessibility using a multilevel mediation model with the predictor and mediator measured at the community level and each outcome measured at the individual level (a 2–1-1 model) (Krull & MacKinnon, 2001); we weighted models for sampling and nonresponse and adjusted for all covariates. In these models, we specified the logit link function for the two dichotomous outcomes, and we estimated a generalized structural equation model. We separately fit mediation models for each of the three types of treatment (outpatient, fee-assisted, Spanish-speeking) and each receipt of care outcome. Finally, based on this estimation, we used the product of coefficients approach and the delta method to calculate the standard errors for indirect effect evaluation.
We conducted two sensitivity analyses to assess the robustness of findings. In the first sensitivity analysis, we reran the models with complete-case analysis (i.e., dropping participants who had missing health insurance or missing income data instead of including a category for missing). In the second sensitivity analysis, we additionally adjusted for factors that were not associated with alcohol treatment in bivariate analyses but are conceptually important. This includes two measures derived from the U.S. Census for each census block group: neighborhood disadvantage (a scaled item created using 6 measures of neighborhood disadvantage), and percent of the neighborhood that was Hispanic; and two self-reported measures derived from UMSARC: nativity and interview language preference (English or Spanish). We conducted all analyses using Stata 15 (StataCorp, 2017).
3. Results
Table 1 displays participant characteristics and predictors of consideration of getting help for an AUD and treatment receipt. Table 1 shows the weighted percent of individuals receiving treatment, accounting for sampling design. Of all participants with lifetime AUD, 20.8% had ever considered getting help, and 10.2% reported receipt of any treatment. Men were more likely than women to receive treatment (12.1% vs. 5.3%). Further, participants who were older, separated/divorced/widowed, lower on income, and more severe on lifetime AUD and drug problem measures were more likely to both consider getting help and to receive treatment than their counterparts. Health insurance status was not associated with considering getting help but was associated negatively with receiving treatment. Dropping the missing category, the comparison of having health insurance was not significant for both consideration of getting help (P = .353) and receipt of treatment (P = .060).
Table 1.
Associations between demographic factors and receipt of care outcomes compared using Chi-square tests.
| Overall (N=792) | Considered Getting Help (N=174) | P | Received Treatment (N=87) | P | |
|---|---|---|---|---|---|
|
| |||||
| N | % | % | |||
| Overall | 792 | 20.8 | 10.1 | ||
| Gender | |||||
| Female | 226 | 16.2 | 0.066 | 5.3 | 0.002 |
| Male | 566 | 22.8 | 12.1 | ||
| Age | |||||
| 18–29 | 283 | 14.5 | 0.001 | 5.2 | <0.001 |
| 30–39 | 224 | 20.3 | 7.6 | ||
| 40–49 | 148 | 26.2 | 15.4 | ||
| 50–59 | 101 | 23.9 | 12.7 | ||
| 60+ | 36 | 40.4 | 33.6 | ||
| Marital Status | |||||
| Single | 259 | 13.5 | <0.001 | 6.5 | <0.001 |
| Married/Living Together | 381 | 18.4 | 8.7 | ||
| Separated/Divorced/Widowed | 152 | 39.4 | 19.7 | ||
| Health Insurance | |||||
| No | 453 | 22.3 | 0.129 | 11.9 | 0.021 |
| Yes | 311 | 19.6 | 8.3 | ||
| Missing | 28 | 10.2 | 2.9 | ||
| Annual Household Income | |||||
| Under $15,000 | 225 | 28.5 | <0.001 | 15.4 | <0.001 |
| $15,000 - $30,000 | 209 | 24.9 | 12.7 | ||
| $30,000 - $60,000 | 217 | 15.6 | 5.8 | ||
| Over $60,000 | 96 | 10.9 | 4.8 | ||
| Missing | 45 | 16.0 | 7.7 | ||
| Lifetime AUD Severity | |||||
| Mild (2–3 symptoms) | 382 | 7.5 | <0.001 | 2.2 | <0.001 |
| Moderate (4–5 symptoms) | 193 | 16.8 | 7.3 | ||
| Severe (6+ symptoms) | 217 | 48.6 | 27.0 | ||
| Lifetime Drug Dependence Symptoms | |||||
| No symptoms | 484 | 13.0 | <0.001 | 5.7 | <0.001 |
| 1 symptom | 207 | 23.0 | 10.9 | ||
| 2 symptoms | 101 | 58.1 | 32.3 | ||
N = number of observations
Row percentages weighted to account for sampling design
P = P-values based on chi-square tests for independence comparing prevalence of considering getting help and receiving treatment across demographic groups
Table 2 displays border-related differences in considering getting help between those on and away from the border. Those living on the border in Border City A and B were less likely to report considering getting help relative to those residing outside of the border region in the Non-Border City (p = 0.003 for both border cities combined). However, receipt of treatment did not significantly vary across cities (p = 0.256). Given a lack of association between residing in the border region and receipt of treatment, we do not include analysis of potential mediating influence of spatial accessibility measures on residing in the border region for receipt of treatment and instead we focus only on considering getting help in the mediation analyses.
Table 2.
Prevalence of considering getting help and receiving treatment across cities.
| Overall (N=792) | Considered Getting Help (N=174) | P | Received Treatment (N=87) | P | |
|---|---|---|---|---|---|
|
| |||||
| N | % | % | |||
| Non-Border City | 282 | 27.3 | ref | 12.1 | ref |
| Border City A | 266 | 16.9 | 0.006 | 8.5 | 0.100 |
| Border City B | 244 | 17.4 | 0.016 | 9.4 | 0.304 |
N = number of observations
Row percentages weighted to account for sampling design
P = P-values based on chi-square tests for independence comparing prevalence of considering getting help and receiving treatment across demographic groups
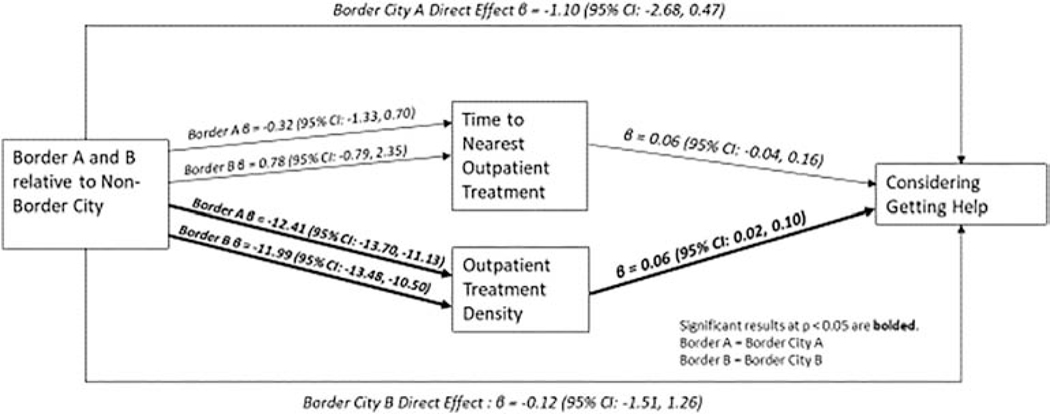
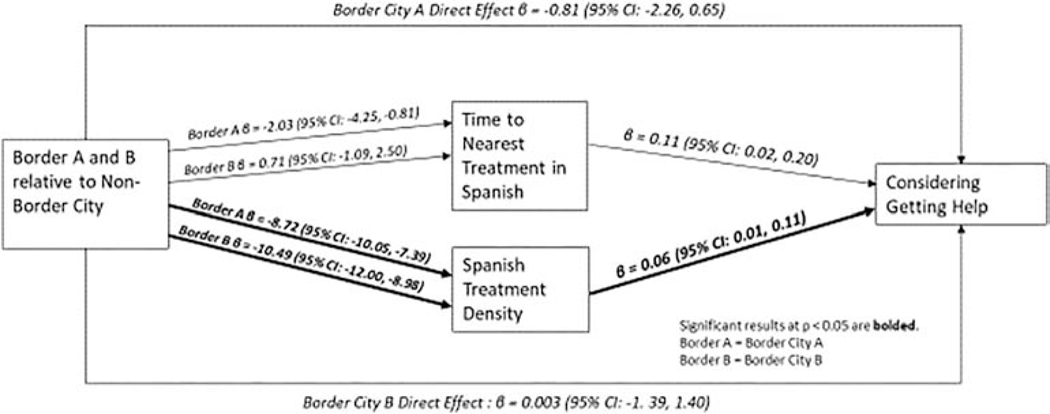
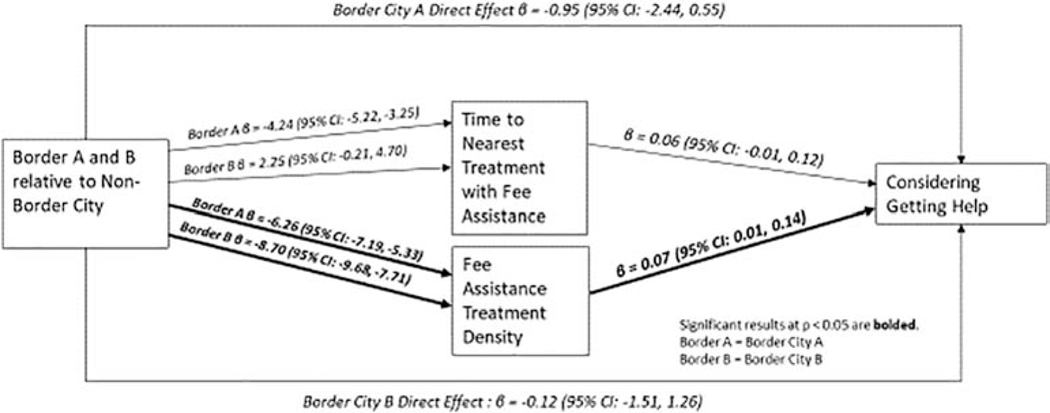
We found several significant indirect pathways between border cities and considering getting help, indicating the ways in which spatial accessibility mediates the association between residing in the border region and considering getting help, through both direct and indirect effects. These are shown in Table 3 and Figures 1–3. Table 3 also shows indirect effects of city (both on and off border) on considering getting help through each spatial accessibility measure. For both cities in the border region there is a statistically significant negative indirect effect of border city through spatial accessibility. Additionally, there is a significant negative indirect effect of Border City A (relative to the Non-Border City) on proximity to treatment for Spanish-speaking services only.
Table 3:
Adjusted indirect effect through specific spatial accessibility mediators of each border city (vs. the nonborder city) on considering getting help.
| Beta coefficient (95% CI) | p-value | |
|---|---|---|
| All Outpatient Treatment | ||
|
| ||
| Border City A – treatment proximity | −0.02 (−0.09, 0.05) | 0.618 |
| Border City B – treatment proximity | 0.04 (−0.07, 0.16) | 0.460 |
|
| ||
| Border City A – treatment density | −0.76 * (−1.29, −0.22) | 0.005 |
| Border City B – treatment density | −0.73 * (−1.25, −0.21) | 0.006 |
|
| ||
| Fee assisted Outpatient Treatment | ||
|
| ||
| Border City A – fee-assisted treatment proximity | −0.24 (−0.52, 0.03) | 0.086 |
| Border City B – fee-assisted treatment proximity | 0.13 (−0.06, 0.32) | 0.175 |
|
| ||
| Border City A -- fee-assisted treatment density | −0.47 * (−0.86, −0.07) | 0.021 |
| Border City B – fee-assisted treatment density | −0.65 * (−1.20, −0.10) | 0.022 |
|
| ||
| Spanish-language Outpatient Treatment | ||
|
| ||
| Border City A – Spanish-language treatment proximity | −0.21 * (−0.43, −0.003) | 0.047 |
|
| ||
| Border City B – Spanish-language treatment proximity | 0.07 (−0.13, 0.28) | 0.471 |
|
| ||
| Border City A – Spanish-language treatment density | −0.53 * (−0.96, −0.11) | 0.014 |
|
| ||
| Border City B – Spanish-language treatment density | −0.64 * (−1.16, −0.12) | 0.016 |
Each model adjusted for age, gender, marital status, annual household income, insurance status, lifetime AUD severity, and lifetime of drug dependence symptoms
indicates significance at p < 0.05
Figure 1:
Direct and Indirect Effects of Border Cities (relative to the Non-Border City) on Considering Getting Help, Mediated by Time to Nearest Outpatient Treatment and Outpatient Treatment Density
Figure 3:
Direct and Indirect Effects of Border Cities (relative to the Non-Border City) on Considering Getting Help, Mediated by Timeto Nearest Treatment offered in Spanish and Spanish Treatment Density
All significant indirect effect estimates with the mediator of treatment density are negative (Table 3). As shown in the figures, while treatment density was associated with increased consideration of getting help for all three types of treatment (outpatient, fee assistance, and Spanish-speaking), treatment density was also significantly lower in both border cities relative to the Non-Border City, leading to negative indirect effects. The largest effect sizes for the indirect effect of border city on considering getting help through the mediator of treatment density is for outpatient treatment density, with β = –0.76 [95% Confidence Interval (CI) = –1.29, –0.22] for Border City A relative to the Non-Border City, and β = –0.73 (95% CI: –1.25, –0.21) for Border City B relative to the Non-Border City. As shown in the figures, lower density of treatment in the Non-Border City helps to explain decreased likelihood of considering getting help in both Border Cities relative to the Non-Border City, although the magnitude of the differences is small.
Notably, treatment density did not mediate receipt of treatment for any of the treatment types—outpatient, fee assistance, Spanish-speaking (data available upon request). Time to nearest treatment only significantly mediated the effect of residing in a border city in Border City A, with time to nearest treatment with fee assistance mediating considering getting help (Figure 3). We found no differences in mediation results in the sensitivity analyses (i.e., in complete-case analysis and adjusting for additional conceptually important variables).
4. Discussion
In this study, Mexican American adults with AUD residing in the U.S.-Mexico border region were less likely to consider getting help for alcohol problems but had similar reported treatment receipt relative to those living in the Non-Border City. Treatment density helps to explain this difference: in both border cities, treatment density was a mediator of residing in the border region on considering getting help. However, proximity to treatment was only significant for Border City A, and, unexpectedly, indicated that increased distance to treatment with fee assistance was associated with increased report of considering getting help. These findings give important insight into the ways in which spatial accessibility mediates the association between living in the border region and receipt of care for Mexican Americans.
We found spatial accessibility to be a significant mediator for explaining the effect of residing in the border region on considering getting help. The significance of proximity to care and density of treatment options to increasing treatment receipt has been well documented in the literature (Beardsley et al., 2003; Fortney et al., 1995; Jacobson, 2004). The current study builds on this prior work by suggesting that fewer treatment options (lower density of treatment) can help to explain the observed disparity in considering getting help for treatment on the U.S.-Mexico border.
Treatment density may help to explain differences by border city in receipt of care, as we found that treatment density was a significant mediator of residing in a border region on considering getting help. This finding was robust for all three types of treatment assessed. This suggests that having multiple treatment options may increase visibility, acceptability, and, ultimately, utilization. However, this finding may be unique to alcohol-related care and not generalizable for all types of substance use disorder treatment. In another study of Mexican American current and former heroin injecting men age 45 and older living in a U.S. city away from the border (Houston, TX), the authors found that neither proximity to nor density of treatment was associated with either treatment seeking or treatment receipt (Kao et al., 2014). A previous study among Hispanics in the United States found that among Spanish-speaking Hispanics, barriers to seeking treatment were higher than English-speaking Hispanics, including perceived anonymity, language barriers, and not knowing where to go for help (Zemore et al., 2009), suggesting that increasing density of services offering Spanish speakers may be particularly important on the border to increase the number of people with AUD who consider getting help.
There are also interesting differences between the border cities we included in this study. Our findings suggest that shorter travel time to nearest treatment with fee assistance in Border City A was associated with lower likelihood of considering getting help. Findings unique to Border City A were not wholly unexpected. Previous data also show heterogeneity in cities in the border region related to AUD risk among men—in Border City A, lower family support and more permissive drinking norms mediated the association between border city and prevalence of AUD, although drug availability and violence/crime were found to be mediators for both Border City A and Border City B (Zemore et al., 2016). Our finding suggests that the treatment ecology may vary between these two border cities. The direction of the significant association in Border City A was surprising, as most previous research suggests that shorter distances encourage treatment utilization. However, broadly, research in Latino populations suggests that there is increased stigma about seeking care and individuals cite worries about anonymity as a barrier to seeking alcohol treatment (Pinedo et al., 2018). It may be that treatment options in Border City A are too close to one’s home or community and thus those with AUD feel that this threatens anonymity. Given differences in social norms around alcohol use in communities in the U.S.-Mexico border region relative to communities farther from the border, it may be that norms around alcohol use also act as a barrier to seeking treatment closer to home. Future research is needed to better understand if this is unique to Border City A or exists across other cities in the border region, as we did not find this to be true in Border City B.
Finally, study findings build on previous research on treatment utilization, showing bivariate associations between covariates and considering getting help and treatment receipt on and away from the border. Like this study, a previous study using data for UMSARC also found that considering getting help was lower in border communities in the United States (Wallisch et al., 2017). The current study builds on this prior work by examining receipt of care outcomes only among those with AUD, rather than anyone with lifetime substance use. We also found in bivariate analyses that being older and having higher AUD severity were associated with being more likely to consider getting help or receive treatment. This makes sense as severity of AUD is a strong predictor of treatment utilization (Spence et al., 2007; Wallisch et al., 2017), and using a lifetime measure, it is not surprising that those who were older were also more likely to consider or receive treatment. Interestingly, we also found that the proportion of those considering getting help and receiving treatment was higher in low-income communities. This suggests that that those most likely to access care are those most likely to experience harms related to alcohol use.
There are several key limitations to this study. There may be limitations to the generalizability of our findings, as we included only a limited number of border communities (two in the border region, one outside the border region), limiting generalizability to the whole border region. These cities may not be representative of all nonborder cities, nor all cities within the border region. Importantly, another study comparing Mexican Americans in other communities in the border region to those in large U.S. cities not proximal to the border found no difference in alcohol treatment utilization between those residing within or outside of the border region (Reingle Gonzalez et al., 2014), suggesting there may be variability within border communities. There were also temporal issues that prevent causal conclusions to the mediation analysis. Receipt of care outcomes were lifetime measures while we determined city by location when participants completed the survey, and spatial accessibility measures were determined in 2013. There is a possibility for residual confounding not captured by the covariates that we included in this analysis, including drug availability, community resources, and restorative quality of the neighborhood. Finally, like any study using self-reported alcohol use measures, there may be response or recall bias from survey participants.
This study makes a valuable contribution to the literature about the reasons Mexican Americans residing on the U.S.-Mexico border indicate less likelihood of considering getting help for alcohol use. Future interventions should focus on increasing treatment options along the U.S.- Mexico border. These findings support the hypothesis that increased treatment density, or more treatment options, may be more important than decreasing distance to care, particularly in urban areas on the U.S.-Mexico border. Future work should assess whether these factors are important for non–Mexican Americans who reside in the U.S.-Mexico border region, assess the causality of this association, and assess whether increasing treatment density is an effective way to increase the likelihood of Mexican Americans considering getting help, and ultimately receiving treatment, in the U.S.-Mexico border region.
Supplementary Material
Figure 2:
Direct and Indirect Effects of Border Cities (relative to the Non-Border City) on Considering Getting Help, Mediated by Time to Nearest Treatment with Fee Assistance and Fee Assistance Treatment Density
Highlights:
Mexican Americans in US-Mexico border region are less likely to consider getting alcohol-related care
Treatment density mediates the observed border differences in alcohol care consideration
Additional treatment locations within communities may improve care utilization
Density of fee-assistance and Spanish-language services are important in the border region
Acknowledgements, Funding, and Disclaimer
This study was supported by funding from the National Institute on Alcohol Abuse and Alcoholism under T32AA007240, P50AA005595, and R01AA01836540). An earlier version of this paper was presented at the 41st Annual Research Society on Alcoholism Scientific Meeting in San Diego, CA, June 16–20, 2018. Thank you to Deidre Patterson, geocoder at the Alcohol Research Group, for geocoding substance use treatment facilities. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association (Ed.). (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed). American Psychiatric Association. [Google Scholar]
- Andersen RM (1995). Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? Journal of Health and Social Behavior, 36(1), 1. 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- Beardsley K, Wish ED, Fitzelle DB, O’Grady K, & Arria AM (2003). Distance traveled to outpatient drug treatment and client retention. Journal of Substance Abuse Treatment, 25(4), 279–285. 10.1016/S0740-5472(03)00188-0 [DOI] [PubMed] [Google Scholar]
- Bensley KM, Harris AHS, Gupta S, Rubinsky AD, Jones-Webb R, Glass JE, & Williams EC (2017). Racial/ethnic differences in initiation of and engagement with addictions treatment among patients with alcohol use disorders in the veterans health administration. Journal of Substance Abuse Treatment, 73, 27–34. 10.1016/j.jsat.2016.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Mills BA, & Vaeth PAC (2013). Alcohol use among Mexican American U.S.–Mexico border residents: Differences between those who drink and who do not drink in Mexico. Addictive Behaviors, 38(4), 2026–2031. 10.1016/j.addbeh.2013.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Zemore SE, Borges G, & Greenfield TK (2015). Border effects on DSM-5 alcohol use disorders on both sides of the U.S.–Mexico border. Drug and Alcohol Dependence, 148, 172–179. 10.1016/j.drugalcdep.2015.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, & Kranzler HR (2007). Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 86(2–3), 214–221. 10.1016/j.drugalcdep.2006.06.008 [DOI] [PubMed] [Google Scholar]
- Fortney JC, Booth BM, Blow FC, & Bunn JY (1995). The effects of travel barriers and age on the utilization of alcoholism treatment aftercare. The American Journal of Drug and Alcohol Abuse, 21(3), 391–406. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A, & Hasin DS (2017). Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry, 74(9), 911. 10.1001/jamapsychiatry.2017.2161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Kao D, & Perron BE (2013). Travel distance to outpatient substance use disorder treatment facilities for Spanish-speaking clients. International Journal of Drug Policy, 24(1), 38–45. 10.1016/j.drugpo.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Marsh JC, Duan L, Oh C, Perron B, & Lee B. (2013). Disparities in Completion of Substance Abuse Treatment between and within Racial and Ethnic Groups. Health Services Research, 48(4), 1450–1467. 10.1111/1475-6773.12031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Marsh JC, Khachikian T, Amaro H, & Vega WA (2013). Disparities in Latino substance use, service use, and treatment: Implications for culturally and evidence-based interventions under health care reform. Drug and Alcohol Dependence, 133(3), 805–813. 10.1016/j.drugalcdep.2013.07.027 [DOI] [PubMed] [Google Scholar]
- Guerrero EG, Pan KB, Curtis A, & Lizano EL (2011). Availability of substance abuse treatment services in Spanish: A GIS analysis of Latino communities in Los Angeles County, California. Substance Abuse Treatment, Prevention, and Policy, 6(1), 21. 10.1186/1747-597X-6-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, & Grant BF (2013). DSM-5 criteria for substance use disorders: recommendations and rationale. The American Journal of Psychiatry, 170(8), 834–851. 10.1176/appi.ajp.2013.12060782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson JO (2004). Place and Attrition from Substance Abuse Treatment. Journal of Drug Issues, 34(1), 23–49. 10.1177/002204260403400102 [DOI] [Google Scholar]
- Kao D, Torres LR, Guerrero EG, Mauldin RL, & Bordnick PS (2014). Spatial accessibility of drug treatment facilities and the effects on locus of control, drug use, and service use among heroin-injecting Mexican American men. International Journal of Drug Policy, 25(3), 598–607. 10.1016/j.drugpo.2013.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krull JL, & MacKinnon DP (2001). Multilevel Modeling of Individual and Group Level Mediated Effects. Multivariate Behavioral Research, 36(2), 249–277. 10.1207/S15327906MBR3602_06 [DOI] [PubMed] [Google Scholar]
- Marsh JC, Cao D, Guerrero E, & Shin H-C (2009). Need-service matching in substance abuse treatment: Racial/ethnic differences. Evaluation and Program Planning, 32(1), 43–51. 10.1016/j.evalprogplan.2008.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Global Affairs (OGA). (2017, December13). The U.S.-Mexico Border Region [Text]. HHS.Gov. https://www.hhs.gov/about/agencies/oga/about-oga/what-we-do/international-relations-division/americas/border-health-commission/us-mexico-border-region/index.html [Google Scholar]
- Ortiz L, Arizmendi L, & Cornelius LJ (2004). Access to Health Care Among Latinos of Mexican Descent in Colonias in Two Texas Counties. The Journal of Rural Health, 20(3), 246–252. 10.1111/j.1748-0361.2004.tb00035.x [DOI] [PubMed] [Google Scholar]
- Perron BE, Gillespie DF, Alexander-Eitzman B, & Delva J. (2010). Availability of Outpatient Substance Use Disorder Treatment Programs in the United States. Substance Use & Misuse, 45(7–8), 1097–1111. 10.3109/10826080903443602 [DOI] [PubMed] [Google Scholar]
- Pinedo M, Zemore S, & Rogers S. (2018). Understanding barriers to specialty substance abuse treatment among Latinos. Journal of Substance Abuse Treatment, 94, 1–8. 10.1016/j.jsat.2018.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Dawson D, Frick U, Gmel G, Roerecke M, Shield KD, & Grant B. (2014). Burden of disease associated with alcohol use disorders in the United States. Alcoholism, Clinical and Experimental Research, 38(4), 1068–1077. 10.1111/acer.12331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reingle Gonzalez JM, Caetano R, Mills BA, & Vaeth PAC (2014). An assessment of individual-level factors associated with alcohol treatment utilization among Mexican Americans. Journal of Substance Abuse Treatment, 47(5), 347–352. 10.1016/j.jsat.2014.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Room R, Babor T, & Rehm J. (2005). Alcohol and public health. Lancet (London, England), 365(9458), 519–530. 10.1016/S0140-6736(05)17870-2 [DOI] [PubMed] [Google Scholar]
- Schmitt SK, Phibbs CS, & Piette JD (2003). The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addictive Behaviors, 28(6), 1183–1192. 10.1016/S0306-4603(02)00218-6 [DOI] [PubMed] [Google Scholar]
- Spence R, Wallisch L, & Smith S. (2007). Treatment Seeking in Populations in Urban and Rural Settings on the Border. Alcoholism: Clinical and Experimental Research, 31(6), 1002–1011. 10.1111/j.1530-0277.2007.00362.x [DOI] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata Statistical Software: Release 15. StataCorp LLC. [Google Scholar]
- Su D, Pratt W, Stimpson JP, Wong R, & Pagán JA (2014). Uninsurance, Underinsurance, and Health Care Utilization in Mexico by US Border Residents. Journal of Immigrant and Minority Health, 16(4), 607–612. 10.1007/s10903-013-9828-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su D, Richardson C, Wen M, & Pagán JA (2011). Cross-border utilization of health care: evidence from a population-based study in south Texas. Health Services Research, 46(3), 859–876. 10.1111/j.1475-6773.2010.01220.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallisch L, Zemore SE, Cherpitel CJ, & Borges G. (2017). Wanting and Getting Help for Substance Problems on Both Sides of the US-Mexico Border. Journal of Immigrant and Minority Health, 19(5), 1174–1185. 10.1007/s10903-016-0442-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Matzger H, & Kaskutas LA (2003). How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction (Abingdon, England), 98(7), 901–911. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Cherpitel CJ, Ye Y, Borges G, Li L, & Wallisch LS (2016). Factors Explaining Variation in Alcohol Use Disorder Prevalence Across Border and Nonborder Communities in Texas. Alcoholism: Clinical and Experimental Research, 40(8), 1707–1716. 10.1111/acer.13124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Mulia N, Ye Y, Borges G, & Greenfield TK (2009). Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three National Alcohol Surveys. Journal of Substance Abuse Treatment, 36(4), 446–456. 10.1016/j.jsat.2008.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Murphy RD, Mulia N, Gilbert PA, Martinez P, Bond J, & Polcin DL (2014). A Moderating Role for Gender in Racial/Ethnic Disparities in Alcohol Services Utilization: Results from the 2000 to 2010 National Alcohol Surveys. Alcoholism: Clinical and Experimental Research, 38(8), 2286–2296. 10.1111/acer.12500 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.