The reported number of nationally notifiable sexually transmitted diseases decreased in March to April 2020 during the US COVID-19 pandemic; however, resurgence of some reported sexually transmitted disease cases occurred later in 2020.
Supplemental digital content is available in the text.
Background
To describe changes in reported sexually transmitted diseases (STDs) during the US coronavirus disease 2019 pandemic, we compared the weekly number of reported nationally notifiable STDs in 2020 to 2019.
Methods
We reviewed cases of chlamydia, gonorrhea, and primary and secondary (P&S) syphilis reported to the US National Notifiable Disease Surveillance System in 2020. For each STD, we compare the number of 2020 cases reported for a given Morbidity and Mortality Weekly Report (MMWR) week to the number of 2019 cases reported in the same week, expressing 2020 cases as a percentage of 2019 cases. We also calculated the percent difference between 2020 and 2019 cumulative case totals as of MMWR week 50 (week of December 9).
Results
During MMWR weeks 1 to 11 (week of December 29, 2019–March 11, 2020), the weekly number of cases of STDs reported in 2020 as a percentage of the cases in the same week in 2019 was similar. However, 2020 numbers were much lower than 2019 numbers in week 15 (week of April 8; chlamydia, 49.8%; gonorrhea, 71.2%; and P&S syphilis, 63.7%). As of week 50, the 2020 cumulative totals compared with 2019 were 14.0% lower for chlamydia, 7.1% higher for gonorrhea, and 0.9% lower for P&S syphilis.
Conclusions
During March–April 2020, national case reporting for STDs dramatically decreased compared with 2019. However, resurgence in reported gonorrhea and syphilis cases later in the year suggests STD reporting may have increased in 2020, underscoring the importance of continued STD prevention and care activities.
The first confirmed US case of coronavirus disease 2019 (COVID-19) was reported on January 20, 2020.1 Before the COVID-19 pandemic, rates of reported sexually transmitted diseases (STDs) in the US were increasing steadily.2 When a national emergency declaration was issued for the COVID-19 pandemic on March 13, 2020, states enacted various prevention measures such as stay-at-home orders, the closing of nonessential businesses, and flexible telework policies in the workplace to stem the COVID-19 spread.3–7 These measures potentially affected STD case reporting in several ways, including reduced STD-related screening and care opportunities from temporary clinic closures, changes in sexual behaviors related to social distancing, and decreases in case investigations due to reductions in state and local health department staff.8–14 To describe changes in reported STDs in the US during the COVID-19 pandemic, we compared the weekly number of reported chlamydia, gonorrhea, and primary and secondary (P&S) syphilis cases in 2020 with the number of cases reported in the same calendar week in 2019.
METHODS
We reviewed cases of chlamydia, gonorrhea, and P&S syphilis reported to the Centers for Disease Control and Prevention's (CDC) National Notifiable Diseases Surveillance System (NNDSS). Data on STD case are transmitted to NNDSS weekly by all 50 states and the District of Columbia.
We examined potential changes in STD case data by week. To be consistent with other diseases reported across the CDC, we based our classification on weeks according to the Morbidity and Mortality Weekly Report (MMWR) classification scheme, which starts with the first week of the year that has at least 4 days in the calendar year (e.g., MMWR week 1 begins on December 30, 2018, in 2019, and on December 29, 2019, in 2020).15 Jurisdictions assign a MMWR week for each reported case; published guidance for assigning MMWR week for STD cases prioritizes dates that best reflect date of disease onset, including date of specimen collection, laboratory result, or date of diagnosis.16 Thus, MMWR week is assumed to reflect the week of disease onset rather than the week reported to public health authorities. To use MMWR week as reported by the jurisdiction, we investigated this assumption by comparing the jurisdiction-assigned MMWR week with dates reflecting disease onset also provided for the case.
To quantify the COVID-19 pandemic's potential impact on reported STDs, we compared the number of 2020 cases reported for a given MMWR week with the number of cases reported in the same week in 2019. We expressed this comparison in terms of the percentage of the previous year's cases that were reported. Percentages lower than 100% denote when 2020 numbers were less than 2019 numbers, whereas percentages higher than 100% indicate when 2020 numbers were higher than 2019 numbers. For example, the weekly number of 2020 chlamydia cases in MMWR week 1 was 22,331 compared with 23,867 cases in 2019 (93.6%). In MMWR week 2, 36,385 chlamydia cases were reported in 2020, whereas 35,650 cases were reported in 2019 (102.1%). To examine variability during nonpandemic periods, we compared 2019 data with 2018 data using the same methods (Table, Supplemental Digital Content 1, http://links.lww.com/OLQ/A696). We also calculated the percent difference between the 2020 and 2019 cumulative case totals as of MMWR week 11 and week 50.
In addition, we conducted stratified analyses by age group (15–19, 20–24, 25–29, 30–34, 35–39, 40–44, and 45+ years), sex (male, female), selected racial/Hispanic ethnicity groups (non-Hispanic Black or African American, non-Hispanic White, Hispanic or Latino), selected diagnosing facility types (private physicians/health maintenance organizations [HMOs], STD clinic, and emergency room/urgent care), and by sex and sex of sex partners for P&S syphilis (men having sex with men [MSM], men having sex with women, women). Finally, to examine variability at the state level, we compared the number of reported 2020 with 2019 cases by disease for each state for two aggregate periods: April–June 2020 and July–September 2020. The April–June 2020 period reflects when states generally imposed various COVID-19 prevention measures, and the July–September 2020 period corresponds to when states subsequently eased the prevention measures.6
Based on data quality review of CDC STD data from previous years (CDC data, unpublished), more than 90% of cases are reported to CDC within 8 weeks of disease onset date; therefore, in this report, we included data reported to CDC up to 8 weeks prior (MMWR week 50—week of December 11, 2019; week of December 9, 2020) to the date of initial analysis (February 3, 2021).
This activity was reviewed by the CDC and was conducted consistent with applicable federal law and CDC policy.*
RESULTS
MMWR Week Assignment
A majority (75.5%) of STD case reports were assigned an MMWR week that reflected the disease onset date, whereas 6.0% had no disease onset date available for comparison. For cases using a date other than disease onset to assign MMWR week, 5.9% resulted in the same MMWR week that would have been assigned using disease onset date. For the remaining case reports (12.7%), the average difference between the date reflecting disease onset and the date used to assign MMWR week was less than 2 weeks.
Chlamydia
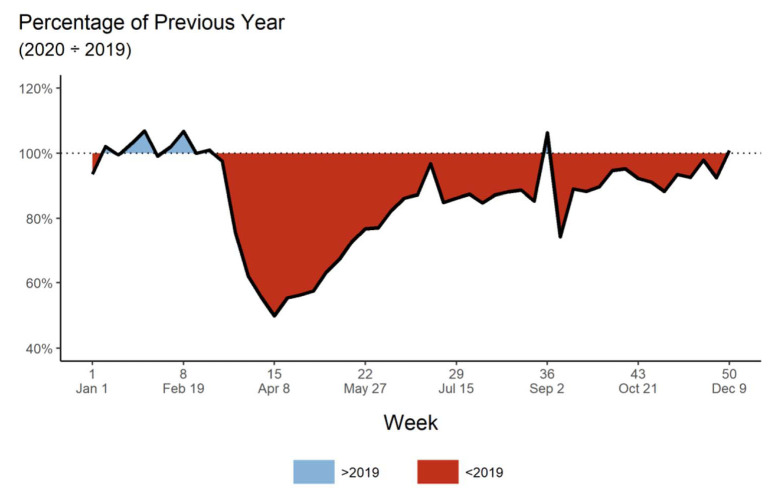
During MMWR week 1 to week 11 (week of March 11, 2020), the weekly number of chlamydia cases reported in 2020 as a percentage of the cases in the same week in 2019 ranged from 93.6% to 106.8% (Fig. 1 and Supplemental Digital Content 1, http://links.lww.com/OLQ/A696). As of MMWR week 11, the 2020 cumulative total of reported chlamydia cases (368,407 cases) was slightly higher than the 2019 cumulative total for the same number of weeks (364,130 cases).
Figure 1.
Reported* 2020 chlamydia cases as a percentage of 2019 by MMWR week†—United States. *Figure includes data reported to the CDC's NNDSS. †The MMWR is prepared by the CDC and is the agency's primary vehicle for scientific publication of timely, reliable, authoritative, accurate, objective, and useful public health information and recommendations. The MMWR week is the week of the epidemiologic year for which the NNDSS disease report is assigned by the reporting local or state health department for the purposes of MMWR disease incidence reporting and publishing.
In week 12 (week of March 18; the first full week of the emergency declaration for the COVID-19 pandemic), the weekly number of 2020 chlamydia cases was 75.8% of 2019 cases. Over the next several weeks, the difference between 2020 cases compared with 2019 cases increased, reaching its greatest point at week 15 (49.8%, week of April 8). Although 2020 cases began to slowly rise toward 2019 levels in week 16 (55.4%, week of April 15), reported 2020 chlamydia cases generally remained lower than the number reported in 2019 through week 50 (week of December 9). As of week 50, the 2020 cumulative total of chlamydia cases was 14.0% lower than for 2019 (1,357,611 and 1,578,286, respectively).
Gonorrhea
From MMWR week 1 to week 11, the number of reported 2020 gonorrhea cases was generally higher than the number of cases from the same weeks in 2019 (range, 99.2%–115.7%; Fig. 2 and Supplemental Digital Content 1, http://links.lww.com/OLQ/A696). By week 11, 130,006 gonorrhea cases had been reported in 2020, an 8.7% increase compared with the 2019 cumulative total of 119,585 gonorrhea cases.
Figure 2.
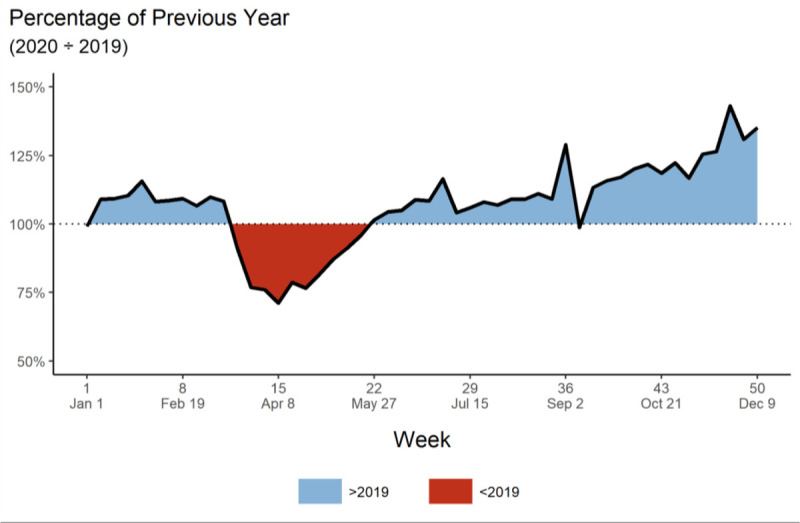
Reported* 2020 gonorrhea cases as a percentage of 2019 by MMWR week†—United States. *Figure includes data reported to the CDC's NNDSS. †The MMWR is prepared by the CDC and is the agency's primary vehicle for scientific publication of timely, reliable, authoritative, accurate, objective, and useful public health information and recommendations. The MMWR week is the week of the epidemiologic year for which the NNDSS disease report is assigned by the reporting local or state health department for the purposes of MMWR disease incidence reporting and publishing.
Decreases in the weekly number of reported 2020 cases compared with 2019 cases began in week 12 (91.1%), with the largest disparity at week 15 (71.2%). In week 18 (81.1%, week of April 29), 2020 cases began to steadily approach 2019 numbers until the number of 2020 cases surpassed the number reported in 2019 in week 22 (101.6%, week of May 27). Generally, from week 22 to week 50, the number of reported 2020 gonorrhea cases remained higher than the number of 2019 cases (range, 98.7%–143.1%).
The cumulative total of 2020 gonorrhea cases was 576,627, a 7.1% increase over the 2019 cumulative total (538,499) through week 50.
P&S Syphilis
During MMWR week 1 to week 10 (week of March 4), reported 2020 P&S syphilis cases were higher compared with 2019 (range, 100.0%–114.8%; Fig. 3 and Supplemental Digital Content 1, http://links.lww.com/OLQ/A696). As of week 11, the 2020 cumulative total of P&S syphilis cases was 5.6% higher compared with 2019 (8185 cases compared with 7748 cases, respectively). During week 11 to week 21 (week of May 20), the number of 2020 P&S syphilis cases remained lower than the number of reported 2019 cases, with the greatest difference at week 15 (63.7%). The number of reported 2020 cases relative to 2019 cases fluctuated from week 22 to week 50, ranging from 82.3% in week 30 (week of July 22) to 151.3% in week 50.
Figure 3.
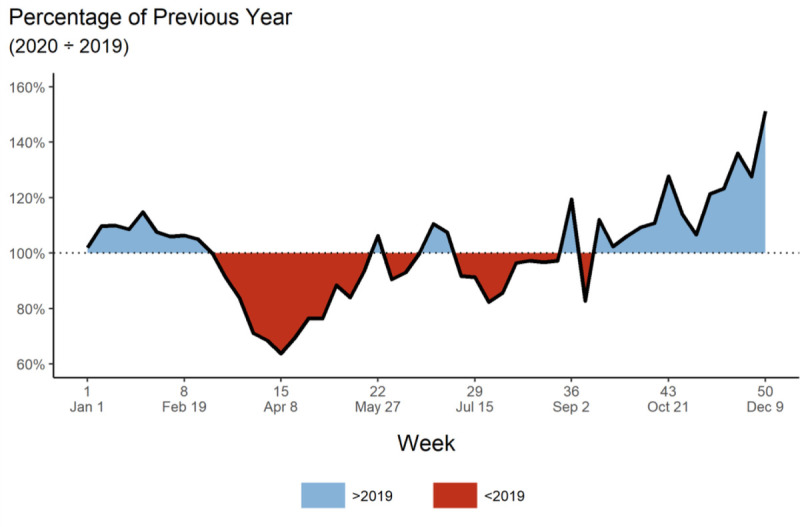
Reported* 2020 P&S syphilis cases as a percentage of 2019 by MMWR week†—United States. *Figure includes data reported to the CDC's NNDSS. †The MMWR is prepared by the CDC and is the agency's primary vehicle for scientific publication of timely, reliable, authoritative, accurate, objective, and useful public health information and recommendations. The MMWR week is the week of the epidemiologic year for which the NNDSS disease report is assigned by the reporting local or state health department for the purposes of MMWR disease incidence reporting and publishing.
By week 50, the cumulative total of 2020 P&S syphilis cases was 0.9% lower than the 2019 cumulative total (33,249 cases vs. 33,562 cases, respectively).
Age Group
When comparing 2020 cumulative totals with 2019 by age group, the decreases observed in March–April 2020 for chlamydia persisted in all age groups through week 50 (Supplemental Fig. 1, Supplemental Digital Content 2, http://links.lww.com/OLQ/A697). The cumulative total of 2020 gonorrhea cases was higher than 2019 among those aged 15 to 44 years (Supplemental Fig. 1, Supplemental Digital Content 2, http://links.lww.com/OLQ/A697). The cumulative total of 2020 P&S syphilis cases among those aged 30 to 44 years increased from 2019 (Supplemental Fig. 1, Supplemental Digital Content 2, http://links.lww.com/OLQ/A697).
Sex
When comparing 2020 with 2019 by week 50, the cumulative totals for male and female chlamydia cases were both lower (16.0% and 12.8%, respectively), whereas cumulative totals for male and female gonorrhea cases were both higher (3.9% and 11.7%, respectively; Supplemental Fig. 2, Supplemental Digital Content 3, http://links.lww.com/OLQ/A698). The 2020 cumulative total of male P&S syphilis cases was 3.2% lower than in 2019, whereas the cumulative total of female P&S syphilis cases was 10.0% higher (Supplemental Fig. 2, Supplemental Digital Content 3, http://links.lww.com/OLQ/A698).
Race/Hispanic Ethnicity
Examining trends by race/Hispanic ethnicity, the 2020 cumulative total cases among non-Hispanic White and Hispanic or Latino persons for all 3 diseases decreased compared with 2019 by week 50 (Supplemental Fig. 3, Supplemental Digital Content 4, http://links.lww.com/OLQ/A699). The 2020 cumulative total cases among non-Hispanic Black or African American persons compared with 2019 were higher in gonorrhea (10.3%) and P&S syphilis (2.4%), but 13.5% lower in chlamydia (Supplemental Fig. 3, Supplemental Digital Content 4, http://links.lww.com/OLQ/A699).
Diagnosing Facility Type
After comparing 2020 numbers with 2019 by diagnosing facility type, the cumulative total cases diagnosed at an emergency room or urgent care increased for all 3 diseases by week 50, whereas the cumulative total cases diagnosed at STD clinics decreased (Supplemental Fig. 4, Supplemental Digital Content 5, http://links.lww.com/OLQ/A700). Although the 2020 cumulative total of chlamydia cases diagnosed at private physicians/HMOs was 6.3% lower than in 2019, gonorrhea and P&S syphilis cases were 19.0% and 8.0% higher, respectively (Supplemental Fig. 4, Supplemental Digital Content 5, http://links.lww.com/OLQ/A700).
Sex of Sex Partners
Although there was no difference in the cumulative totals between 2020 and 2019 for men having sex with women, MSM experienced a 6.7% decrease in reported cases of P&S syphilis (Supplemental Fig. 5, Supplemental Digital Content 6, http://links.lww.com/OLQ/A701).
Jurisdictions
For each of the 51 jurisdictions (50 states and the District of Columbia), we examined the percentage of 2020 cases compared with 2019 cases reported in 2 periods: April–June 2020 and July–September 2020 (Supplemental Fig. 6, Supplemental Digital Content 7, http://links.lww.com/OLQ/A702). For chlamydia, 49 (96%) jurisdictions reported fewer cases during April–June 2020 compared with April–June 2019. The lower numbers continued in 45 (88%) jurisdictions for cases reported in July–September 2020 compared with the same period in 2019. For gonorrhea, 34 (67%) jurisdictions had decreased reported cases during April–June 2020, but only 23 (45%) jurisdictions had decreased numbers during July–September 2020. Similarly, 38 (75%) jurisdictions reported fewer P&S syphilis cases during April–June 2020 compared with 2019, whereas 23 (45%) jurisdictions reported fewer cases during July–September 2020.
In addition, the magnitude of the decreases or increases in case reporting varied by jurisdiction. For example, during July–September, 12 (23%) of jurisdictions had substantial increases (>125%) in gonorrhea when comparing 2020 cases with 2019 cases, whereas only 4 jurisdictions had substantial decreases (<50% of 2019 cases had been reported in 2020). There was no clear pattern by US region.
DISCUSSION
Before the implementation of widespread COVID-19 mitigation measures in the United States, the numbers of reported chlamydia, gonorrhea, and P&S syphilis case counts were all higher in 2020 compared with 2019. However, during March–April 2020, case reporting for all 3 diseases dramatically decreased. Later in the year, 2020 numbers for gonorrhea and syphilis were on track to match and surpass 2019 totals.
The observed decrease in case counts during March–April 2020 was not surprising. As COVID-19 shuttered businesses and workplaces including medical clinics, one likely explanation for the decline in 2020 cases is a decrease in STD screening and diagnosis. During this phase of the COVID-19 pandemic, many health care clinics either limited in-person visits to symptomatic cases or closed entirely.8–14 The STDs, particularly urogenital chlamydial infections among women and extragenital chlamydial and gonococcal infections, are often asymptomatic, and screening is necessary to identify infection.17 Furthermore, shortages of STD test kits and laboratory supplies, specifically for chlamydia and gonorrhea nucleic acid amplification tests, were reported.18 Likewise, it is possible that there was a reduction in other health care visits where STD screening is usually provided (e.g., annual reproductive health visits for young women or HIV preexposure prophylaxis prescription appointments).19–21 In addition, loss of health insurance due to increasing unemployment during the pandemic may have reduced access to health care visits.22 Lastly, individuals may have delayed or avoided routine health visits due to adherence with stay-at-home orders, reduced availability of public transportation, or fear of COVID-19 exposure.22,23 This could have had a further trickle-down effect as reduced diagnoses would preclude partner notification leading to further spread and additional missed opportunities for STD diagnoses. In addition, it is possible that an increase in presumptive treatment via telemedicine for symptomatic persons could have further reduced the number of diagnosed and reported STDs, as STDs were successfully treated in the absence of a confirmatory laboratory test result.9 Unfortunately, there are no nationally representative data available on STD screening coverage, so it is not possible to quantify changes in screening at the national level. However, data from one large commercial laboratory suggest that the number of STD tests performed decreased during shelter-in-place orders.24 Because of the combined impact of all of these factors, the COVID-19 pandemic's disruptive effects on health care clinic capacity and patient's access to screening and testing may have greatly reduced the number of STD cases reported.
Although a reduction in STD screening could result in a drop in diagnosed and reported cases, independent of changes in incidence, it is also possible that the reduction in 2020 reported cases during the shelter-in-place orders occurred because of a true decrease in STD incidence. At the beginning of the pandemic, the majority of the US came under stay-at-home orders, which restricted people from leaving their homes for anything other than essential activities.3 Social distancing was also encouraged to limit people's contact with individuals outside their immediate household.25 COVID-19 can be spread during in-person sexual contact through inhalation of respiratory droplets or respiratory secretions.26,27 Studies conducted among MSM indicate a decrease in sexual behaviors and the number of sexual partners to decrease COVID-19 transmission, at least in the beginning of the COVID-19 pandemic.10,11 Thus, the preventive measures aimed at reducing people's contact with each other to curtail COVID-19 spread may have also resulted in changes in sexual behaviors that reduced STD spread.
In addition, the observed decreases in 2020 case counts may be due to delays in state and local health department processing of STD cases. As COVID-19 cases began to increase, many state and local health department STD staff were redirected from routine STD responsibilities to COVID-19 activities.9,12–14 Consequently, many staff were placed on administrative leave or forced to work from home, which may have affected access to information technology systems necessary to manage STD case data. However, we determined that most cases were assigned to a MMWR week corresponding to the date of diagnosis, suggesting that the resurgence in counts later in 2020 was not simply a result of entering a backlog of cases. Still, it is possible that in some jurisdictions, routine data quality activities that would affect weekly reported cases (e.g., de-duplication of chlamydia cases) were postponed during STD staff redirection and will be completed before 2020 data close out. As state and local health departments can continue to enter, clean, and report cases diagnosed in 2020 until national data are finalized, it is possible the observed differences during the shelter-in-place orders could change as reporting of 2020 cases becomes more complete; an update of this analysis using final 2020 data is planned.
The competing priorities placed on STD staff from COVID-19 may be most strongly felt by disease intervention specialists (DISs), specially trained staff who are essential for identifying and facilitating testing and treatment of index patients and sexual partners, especially for syphilis cases.28 From the very beginning of the pandemic, the case investigation and contact tracing expertise of DIS were leveraged to trace COVID-19 case contacts and ultimately, slow transmission. However, as surges in COVID-19 cases continue, the drop in P&S syphilis cases at the national level may reflect the limited availability and difficulty of DIS staff to maintain syphilis caseloads. However, the preliminary deficit in P&S syphilis cases in 2020 compared with 2019 was quite small, and P&S syphilis numbers were actually higher in 2020 for females, non-Hispanic Black or African American persons, those aged 30 to 44 years, and cases diagnosed at private physicians/HMOs. Furthermore, when examining P&S syphilis numbers by jurisdiction, the number of jurisdictions that reported fewer P&S syphilis cases in 2020 compared with the same period in 2019 earlier in 2020 decreased later in the year. The resurgence of P&S syphilis cases implies that case reports may match and possibly surpass 2019 total nationally.
Chlamydia experienced the largest decreases of the 3 STDs analyzed; reflected at the national level and in the age, sex, race/Hispanic ethnicity, and diagnosing facility type stratified analyses. Even at the jurisdiction level, the deficits from April to June 2020 persisted in July to September 2020 in most jurisdictions. One potential reason for the large decrease in numbers may relate to CDC guidance provided to the jurisdictions in reaction to limited STD resources; guidance directed state and local health departments to prioritize the diagnosis and treatment of syphilis and gonorrhea cases.29 As reflected in the lower number of chlamydia cases diagnosed at private physicians/HMOs, the decrease in STD screenings and limited services to symptomatic cases may continue to disproportionately affect detection of chlamydia cases, as most cases are identified from asymptomatic screening and routine preventive care visits.22,23
Although numbers of reported gonorrhea cases dropped below 2019 levels in March–April 2020, 2020 cases ultimately exceeded 2019 counts. The increase in gonorrhea is seen in both male and female cases, non-Hispanic Black or African American persons, those aged 15 to 44 years, and cases diagnosed at private physicians/HMOs. The same trend can be seen at the state level as the number of states reporting deficits in 2020 gonorrhea cases compared with 2019 dropped later in 2020. The increase in gonorrhea cases seen later in 2020 may reflect increased service utilization as health care clinics reopened services. Furthermore, clinics may have continued targeting services to patients most likely to be infected, therefore increasing the number of cases identified and ultimately reported.12,29
The decrease in cases diagnosed at STD clinics for all 3 STDs may relate to the shuttering of STD clinics at the beginning of the COVID-19 pandemic and the limiting of STD clinics services that continues today.12–14 Conversely, the surge in cases diagnosed at an emergency room or urgent care for all 3 STDs may reflect patients seeking STD care at emergency departments that remained open throughout the pandemic even when access to STD clinics and other health facilities was restricted.
This analysis is subject to several limitations. Factors unrelated to COVID-19 may have influenced the weekly reporting of data to CDC. Some jurisdictions reported issues with the information technology systems used to transmit STD data to CDC before the COVID-19 pandemic. Such issues may have persisted during the pandemic, causing decreases in reporting. However, by using disease onset date to designate MMWR week, we tried to minimize the effect reporting delays may have had on the data. In addition, surveillance data do not include social factors essential to fully understanding the complex interplay between COVID-19, the underlying STD transmission of before the pandemic, and patient demographics.10,11
Clearly, the COVID-19 pandemic has introduced uncertainty and difficulty in interpreting the 2020 case counts. The case reports reported in the nonpandemic years of 2018 and 2019 highlight the striking and anomalous nature of the 2020 drop in STD case reports. As of June 9, 2021, the CDC reported 33,224,075 total COVID-19 cases and 595,625 total deaths.30 Although the introduction of vaccines has decreased COVID-19 cases and deaths, the effects of the protracted pandemic may impair our ability to obtain an accurate picture of the STD epidemic in the US beyond 2020.21,31s
As the COVID-19 pandemic continues to demand state and local public health resources, understaffed STD programs are forced to limit services to a public threatened by an ongoing STD epidemic. Studies have shown that the sexual risk reduction strategies exhibited at the beginning of the pandemic waned as stay-at-home orders lifted and adherence to strict COVID-19 mitigation behaviors declined.3,10,11 One modeling study reported that a higher STD incidence would result if STD service interruptions persisted without a corresponding reduction in sexual activity.32s As the lack of opportunities for STD screening and testing precipitate delays in diagnosis and treatment of index cases, the impact on the health sequelae resulting from more advanced and complicated STDs, such as pelvic inflammatory disease or disseminated gonococcal infection, remains to be seen. Adverse pregnancy outcomes, neonatal infections, and increased HIV infections may also emerge in the future.22 The deleterious effects of such delays in STD diagnosis and treatment are compounded as infected individuals continue to spread STDs for longer durations to a greater number of partners. As DIS continue to bear a heavy burden responding to the COVID-19 pandemic, contact tracing efforts for STDs are reduced.9 Resurgence in gonorrhea and P&S syphilis cases suggests STDs may have increased in 2020, underscoring the importance of continued STD prevention and care activities even in the face of the COVID-19 pandemic.
For further references, please see “Supplemental References,” http://links.lww.com/OLQ/A703.
See, for example, 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
Conflict of Interest and Sources of Funding: None declared.
CDC Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
Contributor Information
Jeremy Grey, Email: yej7@cdc.gov.
Elizabeth Torrone, Email: igf0@cdc.gov.
Kristen Kreisel, Email: ltq1@cdc.gov.
Mark Stenger, Email: zpl4@cdc.gov.
Hillard Weinstock, Email: hsw2@cdc.gov.
REFERENCES
- 1.Holshue ML DeBolt C Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382:929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . Sexually Transmitted Disease Surveillance 2018. 2019. Available at: https://www.cdc.gov/std/stats18/default.htm. Accessed January 3, 2021.
- 3.Moreland A Herlihy C Tynan MA, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—United States, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1198–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czeisler M Tynan MA Howard ME, et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5–12, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention . Guidance for Businesses and Employers Responding to Coronavirus Disease 2019 (COVID-19). 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html. Accessed January 3, 2021.
- 6.Centers for Disease Control and Prevention . COVID-19. 2020. Available at: https://ephtracking.cdc.gov/DataExplorer/. Accessed January 3, 2021. [PubMed]
- 7.Executive Office of the President . Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak, Proclamation. Vol. 85, No. 53, March 18, 2020, 15337–15338. Available at: https://www.federalregister.gov/. Accessed January 3, 2021.
- 8.Napoleon SC Maynard MA Almonte A, et al. Considerations for STI clinics during the COVID-19 pandemic. Sex Transm Dis 2020; 47:431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nagendra G Carnevale C Neu N, et al. The potential impact and availability of sexual health services during the COVID-19 pandemic. Sex Transm Dis 2020; 47:434–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pampati S Emrick K Siegler AJ, et al. Changes in sexual behavior, PrEP adherence, and access to sexual health services due to the COVID-19 pandemic among a cohort of PrEP-using MSM in the South. J Acquir Immune Defic Syndr 2021; 87:639–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanchez TH Zlotorzynska M Rai M, et al. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav 2020; 24:2024–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Coalition of STD Directors . COVID-19 & the State of the STD Field. 2020. Available at: https://www.ncsddc.org/wp-content/uploads/2020/05/STD-Field.Survey-Report.Final_.5.13.20.pdf. Accessed January 3, 2021.
- 13.National Coalition of STD Directors . COVID-19 & the State of the STD Field: Phase II. 2020. Available at: https://www.ncsddc.org/wp-content/uploads/2020/08/STD-Field.Survey-Report.II_.Final-8.6.20.pdf. Accessed January 3, 2021.
- 14.National Coalition of STD Directors . COVID-19 & the State of the STD Field: Phase III. 2021. Available at: https://www.ncsddc.org/wp-content/uploads/2021/01/COVID19-State-of-STD-Field-Phase-III-Report-1.28.21-FINAL-1.pdf. Accessed January 3, 2021.
- 15.Centers for Disease Control and Prevention . MMWR Week. 2019. Available at: https://wwwn.cdc.gov/nndss/document/MMWR_Week_overview.pdf. Accessed January 3, 2021.
- 16.Centers for Disease Control and Prevention . Guidance on classifying STD case reports into MMWR week. 2018. Available at: https://www.cdc.gov/std/program/MMWR-week-guidance_2018January.pdf. Accessed January 3, 2021.
- 17.Stamm W. Chlamydia trachomatis infections in the adult. In: Holmes K Sparling P Stamm W, et al., eds. Sexually Transmitted Diseases. Vol 4th. New York, NY: McGraw-Hill, 2008:575–606. [Google Scholar]
- 18.Bachmann LH, Bolan G. Dear Colleague Letter: DSTDP Lab and Drug Shortages. 2020. Available at: https://www.cdc.gov/std/general/DCL-Diagnostic-Test-Shortage.pdf. Accessed January 3, 2021.
- 19.Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64(Rr-03):1–137. [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention . US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. 2018. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed January 3, 2021.
- 21.Berzkalns A Thibault CS Barbee LA, et al. Decreases in reported sexually transmitted infections during the time of COVID-19 in King County, WA: Decreased transmission or screening? Sex Transm Dis 2021; 48(8S):S44–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ogunbodede OT, Zablotska-Manos I, Lewis DA. Potential and demonstrated impacts of the COVID-19 pandemic on sexually transmissible infections. Curr Opin Infect Dis 2021; 34:56–61. [DOI] [PubMed] [Google Scholar]
- 23.Czeisler M Marynak K Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1250–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinstock H Grey J Stenger M, et al. Impact of COVID-19 on STD Incidence [conference presentation]. 2020 STD Prevention Conference, Virtual. 2020. Available at: https://s6.goeshow.com/ncsd/prevention/2020/conference_schedule.cfm.
- 25.Centers for Disease Control and Prevention . Social Distancing. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html. Accessed January 3, 2021.
- 26.Turban JL, Keuroghlian AS, Mayer KH. Sexual health in the SARS-CoV-2 era. Ann Intern Med 2020; 173:387–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cipriano M, Giacalone A, Ruberti E. Sexual behaviors during COVID-19: The potential risk of transmission. Arch Sex Behav 2020; 49:1431–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cope AB Mobley VL Samoff E, et al. The changing role of disease intervention specialists in modern public health programs. Public Health Rep 2019; 134:11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention . Public Health Activity Guidance. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-covid-19-client-interaction.html#appendix. Accessed January 3, 2021.
- 30.Centers for Disease Control and Prevention . COVID Data Tracker. 2021. Available at: https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days. Accessed June 3, 2021.