BACKGROUND
Traumatic pediatric cervical spine injury can be challenging to diagnose, and the clinical algorithms meant to aid physicians differ from adult trauma protocols. Despite the existence of standardized guidelines, imaging decisions may vary according to physician education, subjective assessment, and experience with pediatric trauma patients. Our study investigates the rates of pediatric posttraumatic cervical spine imaging across trauma centers, hypothesizing that more specialized centers will have lower rates of advanced cervical spine imaging.
METHODS
The 2015 to 2016 Trauma Quality Improvement Program database was reviewed for patients younger than 18 years- to assess rates of cervical spine imaging on presentation across different trauma centers. Propensity stratification logistic regression was performed controlling for patient- and center-specific variables. p Values less than 0.05 were considered significant.
RESULTS
Of 110,769 pediatric trauma patients, 35.2% were female, and the average age was 9.6 years. Overall, 3.6% had cervical spine computed tomography (CT) and less than 1% had cervical spine MRI or X-ray. Compared with all others, Level I trauma centers were significantly less likely to use cervical spine CT for the initial evaluation of younger (≤14 years) but not older trauma patients (adjusted odds ratio [AOR], 0.89; 95% confidence interval [CI], 0.80–0.99; AOR, 0.97; 95% CI, 0.87–1.09); Level I centers had higher odds of cervical spine MRI use, but only for patients 14 years or younger (AOR, 1.63; 95% CI, 1.09–2.44). Pediatric-designated trauma centers had significantly lower odds of cervical spine CT (≤14 years: AOR, 0.70; 95% CI, 0.63–0.78; >14 years: AOR, 0.67; 95% CI, 0.67–0.75) and higher odds of cervical spine X-ray (≤14 years: AOR, 4.75; 95% CI, 3.55–6.36; >14 years: AOR, 4.50; 95% CI, 2.72–7.45) for all ages, but higher odds of cervical spine MRI for younger patients only (≤14 years: AOR, 2.10; 95% CI, 1.38–3.21).
CONCLUSION
Level I and pediatric designations were associated with lower rates of cervical spine CT. Pediatric centers were also more likely to use cervical spine X-ray. This variability of imaging use further supports the need to disseminate and educate providers on pediatric-specific cervical spine evaluation guidelines.
LEVEL OF EVIDENCE
Prognostic and epidemiological, level III.
KEY WORDS: Traumatic cervical spine injury, pediatric trauma, cervical spine imaging, variations of care
Traumatic cervical spine injury (CSI) is a devastating condition associated with substantial morbidity and mortality. Prompt, accurate evaluation of patients with possible or suspected CSI is crucial. For pediatric trauma patients this obligation holds even more true. As a result, there is a greater sense of urgency to diagnose these injuries in children. This may lead to increased advanced cervical spine imaging, which is associated with heightened risks for the pediatric population, as well as substantial healthcare costs, that trauma providers must consider when caring for seriously injured children.
Effectively diagnosing CSI in pediatric trauma patients is complicated by a variety of factors and can be challenging for providers. For one, pediatric CSI is relatively rare and estimated to occur in less than 2% of all pediatric trauma patients, compared with 2% to 4% of adult trauma patients.1–4 Hence, even the busiest trauma providers are unlikely to have frequent exposure to pediatric CSI. Moreover, as the cervical spine anatomy is not “mature” until 8 years to 10 years of age, CSI presentations not only vary between pediatric and adult patients but also within the pediatric population.5,6 Differing head-to-body ratios, ligamentous laxity, incomplete ossification, muscle strength, and vertebral morphology (e.g., facet orientation), among other biomechanical and anatomic factors, partially explain why CSIs move caudally with increasing age (i.e., patients <8 tend to have upper CSI while patients >8 have lower CSI).1,5–8 Further, propensity for different mechanisms of injury also contributes to varying CSI presentations. Motor vehicle accidents (MVAs) are responsible for most pediatric CSI in general, but infants and toddlers are uniquely susceptible to nonaccidental trauma, and sport injuries are responsible for a roughly equal share of CSI in older adolescents. In contrast, adult CSI is most often associated with MVAs or falls.8,9 Lastly, young age also often lends to barriers in communication, resulting in an unreliable history and a further complicated physical examination.10 Even for older children with more advanced language skills, examination findings may be confounded by high levels of anxiety and fear of their surroundings and the situation.10
As a result of the aforementioned complexities and differences between pediatric and adult CSI, the validated imaging-decision algorithms created for adults are not reliably applicable to children.11–13 Thus, pediatric-specific algorithms have been developed to guide imaging for this unique patient population.6,10,13–18 However, there remain variations in practice. This discrepancy is exacerbated by the fact that children present to trauma centers staffed by both adult and/or dedicated pediatric providers; some providers at adult centers might use adult algorithms in the context of pediatric trauma cases, especially if the child is older. Missing or misdiagnosing a pediatric CSI can have grave neurological consequences and there has thus been a trend toward overimaging even at specialized, pediatric-capable centers, which can lead to unnecessary radiation exposure, increased hospital costs and, in some instances, a need for sedation.4–6,10,15,19,20 Accordingly, the goal of our study is to accurately quantify the difference in imaging rates after controlling for several patient, presentation, and trauma center factors. Our study assesses variations in cervical spine imaging at trauma centers across the United States for pediatric trauma victims. We hypothesized that more specialized centers would have lower rates of advanced cervical spine imaging, such as cervical spine computed tomography scan or cervical spine magnetic resonance imaging.
PATIENTS AND METHODS
Data Source and Study Population
The UCLA Institutional Review Board (IRB 19-000831) exempted this study. A retrospective review was performed of the 2015 and 2016 American College of Surgeons Trauma Quality Improvement Program (ACS TQIP) participant use file for all included patients younger than 18 years who presented to a trauma center after injury. The ACS TQIP database consists of an annual collection of quality data from over 850 participating US trauma centers of all levels.21 The accompanying participant use file contains deidentified data for research and quality improvement purposes.
Study Variables
Our primary outcomes were the performance of any cervical spine imaging within 24 hours of presentation, including cervical spine computed tomography (cervical spine CT), cervical spine magnetic resonance imaging (cervical spine MRI), and/or cervical spine radiography (cervical spine X-ray). Imaging performance data were extracted from the database using DRG International Classification of Diseases—10th Rev.—Clinical Modification codes: BR20ZZZ, BR201ZZ, BR200ZZ, and BR20YZZ for cervical spine CT; BR30ZZZ, BR30Y0Z, and BR30YZZ for cervical spine MRI, and BR00ZZZ and BR00ZZ1 for cervical spine X-Ray. Independent variables included hospital trauma level (labeled as I, II, or III/IV/other/not reported, according to either state or ACS designation) and pediatric specialty center status. Additional variables were also extracted, including patient age and sex, region of the country, injury severity (including Injury Severity Score [ISS] and Abbreviated Injury Severity Scale), Glascow Coma Scale (GCS), vital signs, method of injury, presence of a confounding comorbidity, and whether the presentation immediately followed an injury (initial presentation) or corresponded to an interfacility transfer. Vital signs were dichotomized as either normal or abnormal based on the patient’s age group. The method of injury was categorized according to DRG International Classification of Diseases—10th Rev.—Clinical Modification codes as either a fall, gunshot wound, other penetrating injury, MVA, pedestrian versus motor vehicle (peds vs. MVA), cycling injury, motorcycle accident, sport related injury, other blunt injury, crush accident, child abuse, explosion, animal bite, burn, environmental accident, boating accident, drowning/suffocation, poison or “other.” Comorbidities controlled for included those that may confound a physician’s decision to obtain imaging, namely the presence of an attention deficit/hyperactivity disorder, any major psychiatric illness, congenital anomalies, functionally dependent health status, bleeding disorder, history of cerebrovascular accident, dementia, drug, alcohol or steroid use.
Statistical Analysis
Univariate analyses to compare patient demographics, presentation characteristics, and cervical spine imaging utilization by trauma level and pediatric specialty designation were performed using Pearson χ2 tests and analysis of variance. Propensity stratification logistic regression was used for adjusted comparisons of cervical spine imaging used by trauma center characteristics. For these multivariate analyses, we first dichotomized our data according to the age of the patient (14 years and younger; older than 14 years). We further restricted both subsets to include only those patients who were presenting to a trauma center immediately following injury; that is, observations corresponding to presentation following interfacility transfer were excluded. A flow diagram is provided to show final participant inclusion. Next, we calculated for both age subsets, using multivariable logistic regression, four probabilities of presentation: (1) to any Level I trauma center (vs. any other center), (2) to any pediatric-only designated center (vs. any adult center), and (3) to a pediatric-only Level I trauma center (vs. adult Level I). Each model (six in total) incorporated GCS score, method of injury, ISS, region of country, sex and race of patient, presence of comorbid conditions, and vital signs. Cases missing any of these covariates were excluded. Note that whereas the use of five strata has previously been considered standard of practice, current research suggests that meaningful reductions in bias can be achieved using upwards of 12.22,23 Accordingly, we iteratively compared the balance of models (with up to 12 strata) using the reported standardized mean differences; we selected the smallest model to have all standardized mean differences of 0.2 or less. Lastly, we used logistic regression weighted with the appropriate stratification weights to estimate the marginal treatment effect with regular robust standard errors.
All analyses were performed using R Statistical Computing (R Foundation for Statistical Computing, Vienna, Austria) version 3.6.3.24 Odds ratios are reported along with 95% confidence intervals (95% CI). p Values less than 0.05 were considered statistically significant. Results are reported following the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.25
RESULTS
Demographics and Basic Information
We identified 110,769 patients younger than 18 years who presented to a trauma center after injury in the 2015 to 2016 ACS TQIP database. Table 1 shows that the average age was 9.6 years and 35.2% of patients were female. Compared with those who presented to Adult-only Level I centers, children who presented to Pediatric Level I centers after injury were younger (mean age, 8.71 years vs. 10.89 years; p < 0.001) and less likely to be White (64.23% vs. 66.46%; p < 0.001). A significantly higher proportion of children presenting to adult-only Level I centers had confounding comorbidities compared with those who presented to pediatric Level I or other level center (12.75% (adult-only Level I) versus 8.84% (pediatric Level I) and 8.41% (all others), p < 0.001). Similarly, a greater proportion of patients presenting to adult-only Level I centers had abnormal vital signs upon presentation (63.03% [adult-only Level I] vs. 59.98% [pediatric Level I] and 62.27% [all others], p < 0.001). Lastly, pediatric Level I centers were more likely to receive a patient as a transfer from another facility than any other center (48.89% [pediatric Level I] vs. 33.18% [adult-only Level I] vs. 19.99% [all others], p < 0.001) (Table 1).
TABLE 1.
Demographics and Characteristics of Study Patients by Trauma Center Designation (N = 110,769)
| Variables | All Trauma Centers (N = 110,769) | Pediatric Level I (n = 53,272) | Adult-Only Level I (n = 21,716) | All Others (n = 34,603) | p |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | |||||
| Mean (SD) | 9.64 (5.21%) | 8.71 (4.98%) | 10.89 (5.38%) | 10.24 (5.19%) | <0.001 |
| 14 y and younger, n (col. %) | 28,208 (25.47%) | 9,094 (17.07%) | 8,362 (38.51%) | 10,352 (29.92%) | <0.001 |
| Older than 14 y | 82,561 (74.53%) | 44,178 (82.93%) | 13,354 (61.49%) | 24,251 (70.08%) | |
| Sex | |||||
| Male | 71,743 (64.78%) | 33,807 (63.47%) | 14,412 (66.37%) | 22,727 (65.69%) | <0.001 |
| Race | |||||
| White | 71,411 (66.56%) | 33,053 (64.23%) | 13,968 (66.46%) | 23,576 (70.02%) | <0.001 |
| Black or African American | 19,564 (18.23%) | 10,676 (20.75%) | 4,101 (19.51%) | 4,548 (13.51%) | |
| Asian | 2,016 (1.88%) | 1,063 (2.07%) | 379 (1.80%) | 567 (1.68%) | |
| American Indian | 1,245 (1.16%) | 370 (0.72%) | 232 (1.10%) | 631 (1.87%) | |
| Native Hawaiian or Other Pacific Islander | 318 (0.30%) | 94 (0.18%) | 37 (0.18%) | 182 (0.54%) | |
| Other race | 12,742 (11.88%) | 6,205 (12.06%) | 2,299 (10.94%) | 4,164 (12.37%) | |
| Presence of comorbidity | 10,466 (9.45%) | 4,707 (8.84%) | 2,769 (12.75%) | 2,909 (8.41%) | <0.001 |
| Region | |||||
| Midwest | 29,112 (26.36%) | 14,985 (28.16%) | 4,533 (21.13%) | 8,976 (25.94%) | <0.001 |
| Northeast | 16,314 (14.77%) | 8,611 (16.18%) | 4,178 (19.47%) | 3,448 (9.96%) | |
| South | 47,706 (43.20%) | 22,705 (42.67%) | 9,439 (44.00%) | 15,146 (43.77%) | |
| West | 17,290 (15.66%) | 6,904 (12.98%) | 3,304 (15.40%) | 7,033 (20.32%) | |
| Presentation | |||||
| Initial | 70,430 (63.60%) | 27,226 (51.11%) | 14,509 (66.82%) | 27,668 (80.01%) | <0.001 |
| Transfer | 40,314 (36.40%) | 26,046 (48.89%) | 7,206 (33.18%) | 6,912 (19.99%) | |
| Presence of abnormal vital signs | 67,932 (61.33%) | 31,955 (59.98%) | 13,687 (63.03%) | 21,548 (62.27%) | <0.001 |
| GCS | |||||
| 15 | 90,096 (88.11%) | 43,290 (89.13%) | 17,460 (84.83%) | 28,429 (88.71%) | <0.001 |
| 12–14 | 5,263 (5.15%) | 2,163 (4.45%) | 1,291 (6.27%) | 1,742 (5.44%) | |
| 8–11 | 1,809 (1.77%) | 811 (1.67%) | 443 (2.15%) | 529 (1.65%) | |
| Below 8 | 5,086 (4.97%) | 2,305 (4.75%) | 1,388 (6.74%) | 1,347 (4.20%) | |
| ISS | |||||
| 1–25 | 105,129 (96.51%) | 50,678 (96.50%) | 20,194 (94.97%) | 33,116 (97.44%) | <0.001 |
| 26–50 | 3,549 (3.26%) | 1,714 (3.26%) | 1,002 (4.71%) | 804 (2.37%) | |
| 51–75 | 258 (0.24%) | 125 (0.24%) | 68 (0.32%) | 65 (0.19%) | |
| Method of injury | |||||
| Cycling | 4,815 (4.35%) | 2,329 (4.37%) | 853 (3.93%) | 1,598 (4.62%) | <0.001 |
| Falls | 30,959 (27.95%) | 16,413 (30.81%) | 4,590 (21.14%) | 9,666 (27.93%) | |
| MVA | 18,534 (16.73%) | 7,541 (14.16%) | 4,756 (21.90%) | 6,031 (17.43%) | |
| Other | 42,560 (38.42%) | 20,766 (38.98%) | 8,848 (40.74%) | 12,443 (35.96%) | |
| Ped vs. MVA | 4,272 (3.86%) | 2,045 (3.84%) | 1,002 (4.61%) | 1,190 (3.44%) | |
| Sports | 9,629 (8.69%) | 4,178 (7.84%) | 1,667 (7.68%) | 3,675 (10.62%) | |
Cervical Spine Imaging Utilization
Across all included trauma centers, cervical spine CT scans were performed on 3.55% of children, while fewer than 1% of patients received either cervical spine MRI (0.38%) or X-ray (0.77%) (Table 2). Although pediatric Level I trauma centers evaluated 2.4 times the number of patients as adult Level I centers, and 1.5 times the number as all other trauma centers, pediatric Level I trauma centers used cervical spine CT the least (1133 [2.13%] vs. 1250 [5.76%] vs. 1503 [4.34%], respectively; Table 2). Conversely, pediatric Level I centers had higher rates of cervical spine X-ray at 1.15% of patients who presented, while adult Level I centers X-rayed 0.24% and all other centers X-rayed 0.51% (Table 2). Adult Level I centers used cervical spine MRI on the greatest proportion of patients (0.51% vs. 0.34% (pediatric Level I) vs. 0.35% (all others), p < 0.001; Table 2).
TABLE 2.
Cervical Spine Imaging Utilization by Trauma Center Designation
| Variables | Overall (N = 109,591) | Pediatric Level I (n = 52,139) | Adult-Only Level I (n = 21,716) | All Others (n = 34,603) | p |
|---|---|---|---|---|---|
| CS CT | 3886 (3.55%) | 1133 (2.13%) | 1250 (5.76%) | 1503 (4.34%) | <0.001 |
| CS MRI | 414 (0.38%) | 183 (0.34%) | 111 (0.51%) | 120 (0.35%) | 0.002 |
| CS X-Ray | 843 (0.77%) | 614 (1.15%) | 53 (0.24%) | 176 (0.51%) | <0.001 |
Adjusted Analyses Sample
Of the patients 14 years or younger, 49,402 were initial presentations (59.8%; Fig. 1). Among these patients, 42,518 (86.1%) had complete information about the trauma center’s level, and 43,117 (87.2%) had complete information regarding the trauma center’s pediatric designation. Combined, 26,056 were eligible for analyses restricted to Level I trauma centers. Of the patients older than 14 years, 21,028 were initial presentations (74.5%, Fig. 1). Of these, 18,806 (89.4%) had both a complete set of covariates along with the level of the trauma center they presented to, and 19,115 (90.9%) had a complete set of covariates and the trauma center’s pediatric designation. Ultimately, 10,794 patients older than 14 years were included in analyses restricted to Level I centers.
Figure 1.
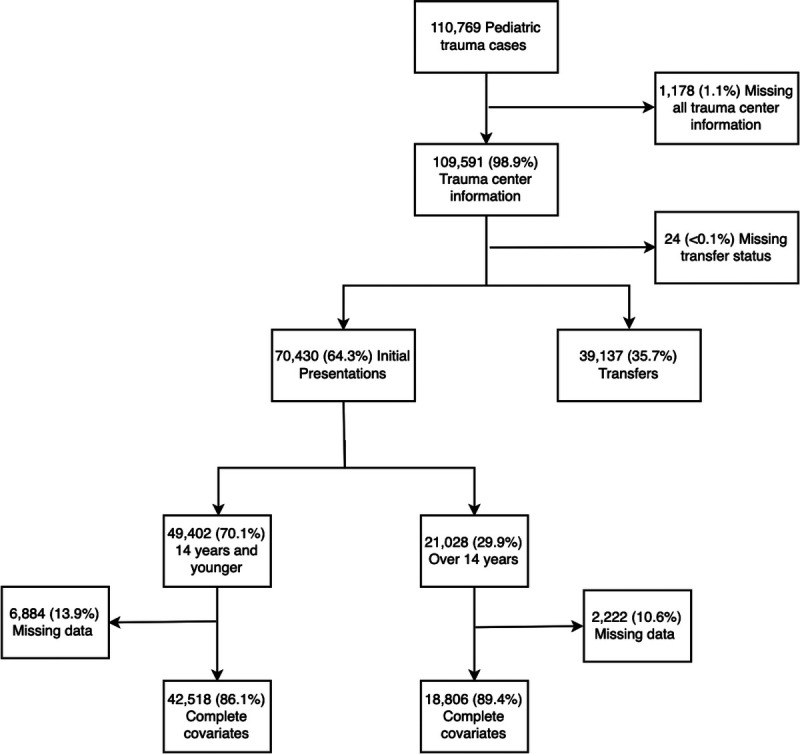
Flowchart for inclusion in propensity stratification logistic regression analyses.
Any Level I vs. All Others
In our multivariate analyses controlling for patient demographics, injury severity, and hospital level covariates, we found that patients 14 years or younger, presenting to any Level I trauma center had significantly decreased odds of cervical spine CT (odds ratio [OR], 0.89; 95% confidence interval [95% CI], 0.80–0.99), and significantly increased odds of cervical spine MRI (OR, 1.63; 95% CI, 1.09–2.44) and X-ray (OR, 2.10; 95% CI, 1.67–2.63) (Table 3). However, children older than 14 years only had significantly increased odds of cervical spine X-ray (OR, 1.59; 95% CI, 1.05–2.42), while cervical spine CT and X-ray utilization were equivocal (Table 3).
TABLE 3.
Adjusted ORs, Adjusted Using Propensity-Stratification, for Cervical Spine Imaging by Age Group Upon Initial Presentation*
| CT | MRI | X-ray | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Any Level I trauma center vs. all others | ||||||
| 14 y and younger (n = 42,518) | 0.89 (0.80–0.99) | 0.034 | 1.63 (1.09–2.44) | 0.017 | 2.10 (1.67–2.63) | <0.001 |
| Older than 14 y (n = 18,806) | 0.97 (0.87–1.09) | 0.647 | 0.99 (0.66–1.47) | 0.949 | 1.59 (1.05–2.42) | 0.030 |
| Any pediatric designated trauma center vs. all others | ||||||
| 14 y and Younger (n = 43,117) | 0.70 (0.63–0.78) | <0.001 | 2.10 (1.38–3.21) | <0.001 | 4.75 (3.55–6.36) | <0.001 |
| Older than 14 years (n = 19,115) | 0.67 (0.60–0.75) | <0.001 | 1.27 (0.85–1.89) | 0.240 | 4.50 (2.72–7.45) | <0.001 |
| Pediatric level i vs. adult level I | ||||||
| 14 y and younger (n = 26,056) | 0.53 (0.46–0.60) | <0.001 | 0.94 (0.60–1.47) | 0.777 | 4.27 (2.95–6.17) | <0.001 |
| Older than 14 y (n = 10,794) | 0.53 (0.45–0.61) | <0.001 | 0.69 (0.41–1.17) | 0.165 | 6.55 (3.05–14.07) | <0.001 |
*Immediately following injury; therefore, children who were presenting as a transfer from another trauma center were excluded.
Pediatric Specialty Designation
Again adjusting for patient demographics, injury severity, and hospital level covariates, our analyses showed that pediatric specialty trauma centers were significantly less likely to perform cervical spine CT scans on children 14 years or younger than trauma centers without a pediatric specialty designation (OR, 0.70; 95% CI, 0.63–0.78) (Table 3). Pediatric specialty centers were also significantly more likely to use cervical spine MRI (OR, 2.10; 95% CI, 1.38–3.21) and cervical spine X-ray (OR, 4.75; 95% CI, 3.55–6.36) in this age group. For patients older than 14 years, pediatric specialty centers were still significantly less likely to use cervical spine CT (OR, 1.67; 95% CI, 0.60–0.75) and significantly more likely to use cervical spine X-ray (OR, 4.50; 95% CI, 2.72–7.45]); however, pediatric and nonpediatric specialty centers used MRI equally (Table 3).
In subanalyses comparing the effect of pediatric specialty designation among Level I centers exclusively (i.e., pediatric Level I vs. adult-only Level I), significant differences in cervical spine imaging emerged. Pediatric Level I centers were significantly less likely to use cervical spine CT and significantly more likely to use cervical spine X-ray: a finding true for both the younger (CT: OR, 0.53; 95% CI, 0.46–0.60; X-ray: OR, 4.27; 95% CI, 2.95–6.17) and older (CT: OR, 0.53; 95% CI, 0.45–0.61; X-ray: OR, 6.55; 95% CI, 3.05–14.07) pediatric patients (Table 3). However, cervical spine MRI use was not significantly different for either age group.
DISCUSSION
Our analyses showed that CSI practices at the time of initial pediatric trauma evaluation varied significantly according to the patient’s age group and the trauma center’s ACS/state level and pediatric capabilities. Our propensity adjusted analyses showed that Level I trauma centers were significantly less likely to use cervical spine CT imaging in the evaluation of younger (≤14 years) but not older (>14 years) trauma patients when compared with all other trauma centers. Conversely, Level I centers were significantly more likely than all others to use cervical spine X-ray in the evaluation of both younger and older pediatric patients and cervical spine MRI in the evaluation of younger patients. In the evaluation of younger patients, centers with a pediatric designation were significantly less likely to use cervical spine CT and more likely to use both cervical spine MRI and X-ray compared with nonpediatric centers. Similarly, these centers were significantly less likely to use cervical spine CT in the evaluation of older pediatric trauma patients, but only used cervical spine X-ray (and not MRI) significantly more often. To isolate the effect of level versus pediatric designation, we compared pediatric Level I centers with nonpediatric Level I centers, finding significantly less cervical spine CT utilization for both younger and older pediatric trauma patients by pediatric Level I centers, as well as significantly more alternative imaging for both age groups by these pediatric Level I centers (X-ray for both younger and older, MRI for only younger patients).
Cervical spine injury is rare in the pediatric trauma patient but also particularly difficult to diagnose and devastating when missed. We found that less than 4% of pediatric trauma patients included in the TQIP database received any cervical spine imaging but that when it was performed, the most common modality was a cervical spine CT. Despite validated protocols intended to guide cervical spine imaging decisions in the care of pediatric trauma patients, our findings substantiated the hypothesis that there is persistent variation in the use of cervical spine imaging in the initial evaluation of these children.4,6,10,13–18
Our findings should be contextualized with respect to the established algorithms intended to guide clinicians toward the best practice for initial cervical spine imaging of pediatric (and adult) trauma patients. While a single gold standard does not exist, the American College of Radiology does release their annually updated Appropriateness Criteria for Suspected Spinal Trauma in the Child.14 This comprehensive report, which reviews the latest literature and draws upon the validated NEXUS, PECARN, and Pierretti-Vanmarcke clinical decision rules, as well as the expert opinion of a multidisciplinary panel when evidence is lacking or conflicted, promulgates the appropriateness of each imaging modality for various presenting characteristics of trauma patients.12,14,15,17 Notably, plain radiography is the only modality with a favorable risk-to-benefit ratio established for nearly all clinical scenarios warranting cervical spine imaging.14
While cervical spine CT is the most sensitive and, hence, preferred imaging modality for suspected adult CSI, its utility for the pediatric population is debated.14,26 Pediatric trauma patients who are obtunded, experienced polytrauma, or were injured by a high-risk mechanism are likely to benefit from cervical spine CT.5 As older pediatric patients have cervical spine anatomy, physiology, and biomechanics more similar to adults, clinicians may opt more often for cervical spine CT in these patients as well.5,27 It is important to note, however, that negative cervical spine CT scans, like negative cervical spine plain radiography, cannot exclude all cervical spine injuries. In particular, spinal cord injury without radiographic abnormality (SCIWORA) presents without fracture nor dislocation on both radiography and CT, and is more common in pediatric patients, particularly those younger than 8 years.28 Because of this, clinicians are urged to have a low threshold for cervical spine MRI use—MRI’s superior soft tissue and bone visualization capabilities are better suited for the cervical spine anatomy (e.g., ligamentous laxity) and injury patterns of the pediatric population; indeed, MRI has the highest sensitivity and specificity for acute pediatric CSI.5,6,14,15
Our study showed the cervical spine imaging practices of specialized trauma centers (ACS and state designated Level I and pediatric Level I) align more closely with the published algorithms for pediatric cervical spine imaging (e.g., ACR Appropriateness Criteria) than do the practices of less specialized trauma centers.5,11,14,15 These findings could imply that providers at specialized centers have greater familiarity with the standardized imaging protocols. However, our findings still suggest excess utilization of cervical spine CT regardless of trauma level designation. For example, although pediatric Level I trauma centers were four and a half times as likely to use cervical spine radiography compared with all other trauma centers, perhaps indicating a better appreciation for the utility of plain cervical spine x-ray, they were still about half as likely to utilize CT. And, finally, despite MRI’s superior capabilities for detecting and ruling out CSI in pediatric trauma patients, especially in cases of SCIWORA, it was consistently the least frequently used modality across all trauma centers.
Nonetheless, variability in imaging performance is to be expected to a certain extent, and our findings should not be interpreted as an indictment on inadequate guideline adherence. Each of the published algorithms allow for subjective clinical assessment, physician suspicion, and physician experience to factor into individual imaging decisions. Given the gravity of missing CSI in children, physicians, especially those at less specialized centers who are also less accustomed to caring for pediatric trauma patients, may be taking a “better safe than sorry” diagnostic approach.4 Another important possibility to consider, especially in the context of older pediatric trauma patients, is that providers might have been using adult cervical spine clearance algorithms; and, unfortunately, it is likely that this issue persists today. In 2016, Duane et al.29 published the findings from a decade long study to determine the best practice for clearance of the cervical spine in the setting of adult trauma patients meeting the Center of Disease Control trauma team alert criteria. The authors declared that any adult trauma patient meeting the Center of Disease Control trauma team alert should undergo a CT scan which captures the cervical spine. Hence, providers at adult trauma centers today who immediately request cervical spine CT scans for the initial evaluation of a pediatric trauma patients might actually be following guidelines (in)appropriately because they either lack familiarity with the pediatric specific protocols or believe the pediatric patient is old enough to meet adult criteria. Nonetheless, there are significant harms to such an approach, as children need to be treated differently than adults for several reasons. Not only is cervical spine anatomy different in children and adults (as previously discussed), the longer expected life span of children allows for a longer latency period for the adverse effects of ionizing radiation to manifest.19,28
It is important to note, too, that actually performing cervical spine plain radiography in pediatric trauma care is challenging for several reasons, namely that it requires cooperation on the part of the patient. Similarly, performing MRI is a complicated, expensive procedure, and younger patients often require sedation; furthermore, many centers might not have ready access to MRI machines. Accordingly, some physicians may elect to avoid these arduous processes and use cervical spine CT first line. Again, however, taking such an approach has been shown to be associated with increased harm, as cervical spine CT is not only associated with greater radiation exposure and higher costs, it may also yield false reassurance in cases of SCIWORA.19,28
Given the risks associated with advanced imaging in combination with the fact that CSI is, in general, less common in younger patients, our study supports that education on, and greater dissemination of these standardized guidelines are desperately needed.1,2,5 Previous studies have shown that following a protocol leads to a more judicious use of imaging with similar outcomes.1,2,5,10 Our findings illustrate the extent to which variation in cervical spine imaging practices exists across trauma level designations and resource availability. Universally distributed algorithms and continuing education on their use are likely to standardize care and reduce the variation observed in our study. While CSI is a grave and serious condition, trauma centers must work to minimize the cost and harms associated with advanced imaging modalities, especially CT.
Our study is subject to certain limitations similar to those of prior studies using National Trauma Data Bank (NTDB) TQIP data. For example, given that observations in retrospective trauma studies are influenced by many factors including subjective clinical judgments, it possible that undocumented confounding factors persist beyond adjustment and bias results. To address this, however, we controlled for several observed covariates and used propensity stratification for multivariate regression adjustment. Propensity score models have become increasingly popular in observational medical treatment studies as they effectively and robustly reduce bias attributable to differential covariate distribution between the treatment groups.22,30 Further, like other studies using NTDB TQIP data, our data are subject to coding inaccuracies and nonrandom missingness.31–33 More, the NTDB TQIP is not a census of trauma centers in the United States and likely disproportionately represents high volume and academic centers. While these three limitations are common to any project using the NTDB TQIP, previous authors have taken varied approaches to limiting potential bias; our approach excluding observations missing data was not dissimilar to the majority of NTDB research published.33 Although imperfect, the NTDB is the largest and most comprehensive trauma registry, and as such it is best suited to compare trauma centers between each other, particularly those designated Level I (95% of which participate).33 Finally, our study lacked many clinical variables and observations, such as subjective patient complaints. As such, we could not apply published guidelines, such as the NEXUS, PECARN, and Pierretti-Vanmarcke clinical decision rules, to individual observations to compare performance across trauma centers.12,15,17 However, the focus of our study was not to comment on the quality of individual patient care at various trauma centers, specifically in the context of CSI, but rather to explore how imaging use varies by trauma center designation and pediatric capabilities. As guidelines are revised, more widely distributed, and familiarized by trauma providers at all centers, future studies might reevaluate and compare cervical spine imaging utilization to the baseline we have described herein.
In conclusion, despite validated clinical decision algorithms promoting cervical spine X-ray as the preferred cervical spine imaging modality for pediatric trauma patients with suspected CSI, our study found that cervical spine CT remains the most common cervical spine imaging modality in the care of pediatric trauma patients. Level I trauma centers were significantly less likely to use CT and more likely to use X-ray for the initial evaluation of younger but not older pediatric trauma patients. Pediatric specialty trauma centers were significantly less likely to use cervical spine CT and more likely to use cervical spine X-ray for pediatric patients of any age (also significantly more likely to use MRI for younger patients.) Compared with nonpediatric Level I centers, pediatric Level I centers were significantly less likely to use CT and more likely to use X-ray for the initial evaluation of both pediatric age groups, but no significant differences were found for cervical spine MRI use. Better dissemination of and education on appropriateness criteria for evaluation of pediatric CSI may lead to improved outcomes of pediatric spinal injury with decreased cost and radiation exposure at a population level.
AUTHORSHIP
R.M. and H.C.-H.J. participated in the conception and method design of the study. R.M., H.C.-H.J., T.D., and C.-H.T. performed the database review. T.D., C.-H.T. and J.W. performed the statistical analyses. R.M. drafted the initial article. J.W. and H.C.-H.J. critically revised and finalized the article.
DISCLOSURE
The authors declare no funding or conflicts of interest.
Footnotes
Published online: July 6, 2021.
This study was presented at the American Pediatric Surgical Association (APSA) 2020.
Contributor Information
Roxanne Massoumi, Email: rmassoumi@mednet.ucla.edu.
Joseph Wertz, Email: jwertz@mednet.ucla.edu.
Tuyen Duong, Email: hcjen13@gmail.com.
Chi-Hon Tseng, Email: ctseng@mednet.ucla.edu.
REFERENCES
- 1.Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN. Spinal injuries in children. J Pediatr Surg. 2004;39(4):607–612. [DOI] [PubMed] [Google Scholar]
- 2.Mohseni S, Talving P, Branco BC, Chan LS, Lustenberger T, Inaba K, Bass M, Demetriades D. Effect of age on cervical spine injury in pediatric population: a National Trauma Data Bank review. J Pediatr Surg. 2011;46(9):1771–1776. [DOI] [PubMed] [Google Scholar]
- 3.Milby AH, Halpern CH, Guo W, Stein SC. Prevalence of cervical spinal injury in trauma. Neurosurg Focus. 2008;25(5):E10. [DOI] [PubMed] [Google Scholar]
- 4.Viccellio P Simon H Pressman BD Shah MN Mower WR Hoffman JR, NEXUS Group . A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):E20. [DOI] [PubMed] [Google Scholar]
- 5.McAllister AS, Nagaraj U, Radhakrishnan R. Emergent imaging of pediatric cervical spine trauma. Radiographics. 2019;39(4):1126–1142. [DOI] [PubMed] [Google Scholar]
- 6.Egloff AM, Kadom N, Vezina G, Bulas D. Pediatric cervical spine trauma imaging: a practical approach. Pediatr Radiol. 2009;39(5):447–456. [DOI] [PubMed] [Google Scholar]
- 7.Jones TM, Anderson PA, Noonan KJ. Pediatric cervical spine trauma. J Am Acad Orthop Surg. 2011;19(10):600–611. [DOI] [PubMed] [Google Scholar]
- 8.Leonard JR, Jaffe DM, Kuppermann N, Olsen CS, Leonard JC. Cervical spine injury patterns in children. Pediatrics. 2014;133(5):e1179–e1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hasler RM, Exadaktylos AK, Bouamra O, Benneker LM, Clancy M, Sieber R, Zimmermann H, Lecky F. Epidemiology and predictors of cervical spine injury in adult major trauma patients: a multicenter cohort study. J Trauma Acute Care Surg. 2012;72(4):975–981. [DOI] [PubMed] [Google Scholar]
- 10.Lee SL, Sena M, Greenholz SK, Fledderman M. A multidisciplinary approach to the development of a cervical spine clearance protocol: process, rationale, and initial results. J Pediatr Surg. 2003;38(3):358–362. [DOI] [PubMed] [Google Scholar]
- 11.Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, Laupacis A, Schull M, McKnight RD, Verbeek R. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841–1848. [DOI] [PubMed] [Google Scholar]
- 12.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343(2):94–99. [DOI] [PubMed] [Google Scholar]
- 13.Browne GJ, Lam LT, Barker RA. The usefulness of a modified adult protocol for the clearance of paediatric cervical spine injury in the emergency department. Emerg Med. 2003;15(2):133–142. [DOI] [PubMed] [Google Scholar]
- 14.Kadom N, Palasis S, Pruthi S, Biffl WL, Booth TN, Desai NK, Falcone RA, Jr., Jones JY, Joseph MM, Kulkarni AV. ACR Appropriateness Criteria® Suspected Spine Trauma-Child. J Am Coll Radiol. 2019;16(5):S286–S299. [DOI] [PubMed] [Google Scholar]
- 15.Pieretti-Vanmarcke R, Velmahos GC, Nance ML, Islam S, Falcone RA, Jr., Wales PW, Brown RL, Gaines BA, McKenna C, Moore FO. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the American Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2009;67(3):543–550. [DOI] [PubMed] [Google Scholar]
- 16.Jaffe DM, Binns H, Radkowski MA, Barthel MJ, Engelhard HH, III. Developing a clinical algorithm for early management of cervical spine injury in child trauma victims. Ann Emerg Med. 1987;16(3):270–276. [DOI] [PubMed] [Google Scholar]
- 17.Leonard JC, Kuppermann N, Olsen C, Babcock-Cimpello L, Brown K, Mahajan P, Adelgais KM, Anders J, Borgialli D, Donoghue A. Factors associated with cervical spine injury in children after blunt trauma. Ann Emerg Med. 2011;58(2):145–155. [DOI] [PubMed] [Google Scholar]
- 18.Laham JL, Cotcamp DH, Gibbons PA, Kahana MD, Crone KR. Isolated head injuries versus multiple trauma in pediatric patients: do the same indications for cervical spine evaluation apply? Pediatr Neurosurg. 1994;21(4):221–226. [DOI] [PubMed] [Google Scholar]
- 19.Goodman TR, Mustafa A, Rowe E. Pediatric CT radiation exposure: where we were, and where we are now. Pediatr Radiol. 2019;49(4):469–478. [DOI] [PubMed] [Google Scholar]
- 20.Flynn JM, Closkey RF, Mahboubi S, Dormans JP. Role of magnetic resonance imaging in the assessment of pediatric cervical spine injuries. J Pediatr Orthop. 2002;22(5):573–577. [PubMed] [Google Scholar]
- 21.Committee on Trauma ACoS . TQP PUF Version X.X. Chicago, IL: Committee on Trauma ACoS; 2015–2016. [Google Scholar]
- 22.Neuhäuser M, Thielmann M, Ruxton GD. The number of strata in propensity score stratification for a binary outcome. Arch Med Sci. 2018;14(3):695–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79(387):516–524. [Google Scholar]
- 24.R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. [Google Scholar]
- 25.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. [DOI] [PubMed] [Google Scholar]
- 26.Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma Acute Care Surg. 2005;58(5):902–905. [DOI] [PubMed] [Google Scholar]
- 27.Fesmire FM, Luten RC. The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med. 1989;7(2):133–142. [DOI] [PubMed] [Google Scholar]
- 28.Pang D, Pollack IF. Spinal cord injury without radiographic abnormality in children—the SCIWORA syndrome. J Trauma Acute Care Surg. 1989;29(5):654–664. [DOI] [PubMed] [Google Scholar]
- 29.Duane TM Young AJ Vanguri P, et al. Defining the cervical spine clearance algorithm: a single-institution prospective study of more than 9,000 patients. J Trauma Acute Care Surg. 2016;81(3):541–547. [DOI] [PubMed] [Google Scholar]
- 30.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roudsari B, Field C, Caetano R. Clustered and missing data in the US National Trauma Data Bank: implications for analysis. Inj Prev. 2008;14(2):96–100. [DOI] [PubMed] [Google Scholar]
- 32.Dowd B, Bernal E, Boneva D, Hai S, Mark McKenney MDM. The National Trauma Data Bank Data Consistency: Can We Do Better? Am Surg. 2018;84(11):E492. [PubMed] [Google Scholar]
- 33.Haider AH. Improving the quality of science arising from the NTDB: We can do this! LWW; 2013. [DOI] [PubMed] [Google Scholar]


