Abstract
Background Prognosis of metastatic colorectal cancer (mCRC) is poor and goal of treatment is mainly palliative unless there is limited metastatic disease which is surgically resectable. Here, we report a case series of long-term survivors treated predominantly with chemotherapy.
Methods This is a single-center retrospective analysis of patients of mCRC. Records of metastatic colorectal cancer patients registered at Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, between the year 2005 and 2015 were retrieved and reviewed. Inclusion criteria were patients who survived 5 years or more, treated mainly by chemotherapy, with either initial presentation as metastatic disease or those who progressed after initial surgery with or without adjuvant therapy. The details about the patient characteristics, treatment, and outcome were collected. The data were censored on September 30, 2020.
Results Records of 370 mCRC patients were reviewed. Thirty-one patients with all the available details fulfilled the criteria for inclusion in the study. Median age was 53 years (range, 22–74 years). Sixteen were women (51.6%). Twenty-four (77%) were newly diagnosed cases with initial presentation as metastatic disease. Commonest site of primary was on the left (21, 67.6%) followed by right side and transverse colon in 5 patients each. Liver was the most common site of metastasis ( n = 18, 58.06%). In metastatic setting, the most common chemotherapy regimen used in the first line was CAPOX ( n = 11, 35.48%). Only three patients could undergo metastatectomy. Monoclonal antibodies could be used only in 14 patients. Median overall survival (OS) of this cohort is 81.6 months (95% confidence interval [CI], 69.73–117.9).
Conclusion A small but significant proportion of mCRC patients may achieve and maintain durable responses and long term survival with use of combination of chemotherapy with or without biologics.
Keywords: metastatic colorectal cancer, long-term survivors, chemotherapy, India

Atul Sharma
Introduction
As per Globocan 2018 data colorectal cancer (CRC) is the third most common cancer (10.2%) and the second most common cause of cancer-related death among all cancer cases. 1 Metastatic colorectal cancer (mCRC) has dismal outcomes, with the 5-year survival rate of less than 10%. The median survival time of patients with untreated mCRC is approximately 5 months. 2 The goal of treatment in majority of cases remain palliative unless there is limited metastatic disease which is resectable, as surgery is the only curative treatment option. 3 However, the landscape of treatment of mCRC has significantly evolved over the past two decades with the availability of newer chemotherapeutic, targeted agents. 4 A better understanding of the administration of combination chemotherapy (oxaliplatin and irinotecan) with use of biological agents (bevacizumab, cetuximab, and panitumumab), molecular biology of the disease, approval of newer agents (regorafenib, Her2neu inhibitor) immune checkpoint inhibitors, and improvement in supportive care delivery have largely revolutionized the outcomes of metastatic patients. 5 A small subset of these patients may have durable responses and survival even without surgery. The data regarding this subset are lacking from the Indian as well as South East Asian subcontinent regarding long-term survivors. Here we report a case series from India, of long-term survivors of mCRC mainly treated with chemotherapy.
Methods
This is a single-center retrospective analysis of patients of mCRC registered at Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, from the year 2005 to 2015. Main inclusion criteria were mCRC patients who were treated at the centre mainly with chemotherapy, who had either initial presentation as metastatic disease or those who progressed after initial surgery with or without adjuvant therapy, and those who survived for 5 or more years. Data were retrieved from the hospital-based record system. Demographic details including age, sex, Eastern cooperative oncology group (ECOG)performance status, primary and metastatic sites stage, and various treatment lines including biologics received by the patient were documented in a structured proforma. Treatment response and current status of the patient were obtained telephonically and from case records. Common terminology criteria for adverse events (CTCAE) 4.0 was used to document toxicities. Median and range were used to describe quantitative variables. Kaplan–Meier curve was used for survival analyses. Cox proportional hazards model was used to assess the association of clinical variables with survival. P values of <0.05 were considered statistically significant. Statistical analysis was done using STATA software (ver13 StataCorp, College Station, Texas, United States). Data were censored on September 30, 2020.
Results
Patient Characteristics
In the duration extending from year 2005 to 2015, records of 370 mCRC patients were identified and reviewed. Thirty-eight patients fulfilled the criteria of survival beyond 5 years. However, details of treatment, evaluable response, and complete records were available for 31 patients. Median age was 53 years (range, 22–74 years). Sixteen patients were women (51.6%). Out of the 31 patients, 13 (41.9%) patients had comorbidities like diabetes, hypertension, or hypothyroidism. Twenty-eight (90.3%) patients had ECOG PS 1 and two (6.4%) patients presented with PS 2. Twenty-one (67.7%) patients had left-sided colon cancer, whereas 5 patients (16.1%) had right-sided colon cancer. Five (16.1%) patients had involvement of transverse colon. The commonest histopathology grade was moderately differentiated adenocarcinoma (87%); only one patient had mucinous histology. Liver was the most common predominant site of metastasis ( n = 18, 58%), followed by peritoneum ( n = 6, 19.3%), and lung ( n = 4, 12.9%). Multiple unresectable liver metastases (defined as >3) were seen in 6 patients. Two patients had family history of gastrointestinal (GI) cancers without further details. Baseline median CEA (carcino embryonic antigen) was 6 ng/mL (range 2-900). RAS status was not available in all cases. K RAS status was available for 15 patients NRAS available in 3 patients and BRAF in one. Eleven patients were RAS wild type whereas one patient was documented as RAS mutated ( Table1 ).
Table 1. Patient characteristics.
| Characteristics |
N
= 31
( N )% |
|---|---|
| Median age | 53 (22–74) |
| Sex | |
| Male | 15 (48.39) |
| Female | 16 (51.61) |
| ECOG PS | |
| 0 | 1 (3.23) |
| 1 | 28 (90.32) |
| 2 | 2 (6.45) |
| Sidedness | |
| Right | 5 (16.13) |
| Left | 21 (67.74) |
| Transverse colon | 5 (16.13) |
| Mutation status available | |
| K RAS | 15 (48.38) |
| N RAS | 3 (9.67) |
| BRAF | 1 (3.2) |
| No. of previous lines received | |
| 1 | 14 (45.16) |
| 2 | 8 (25.81) |
| 3 | 3 (9.68) |
| 4 | 1 (3.23) |
| 5 | 5 (16.13) |
| No. of metastatic sites | |
| 1 | 27 (87.1) |
| 2 | 4 (12.9) |
| Site of metastasis | |
| Liver | 18 (58.06) |
| Lung | 4 (12.9) |
| Peritoneum | 6 (19.35) |
| Distant nodal | 5 (16.13) |
| Biochemical parameters mean (range) | |
| CEA levels (ng/dL) | 6 (2–900) |
| Hemoglobin (g/dL) | 11.7 (6–16.4) |
| Total leucocyte count (10 9 /L) | 7,600 (4,500–15,500) |
| Platelets (10 9 /L) | 2.47 (1.01–6.09) |
| Serum albumin (g/dL) | 3.9 (2.7–5.3) |
Treatment Characteristics
Twenty-four (77%) of the patients presented as upfront metastatic disease. Seven (22.5%) progressed as metastatic disease following previous curative resection with or without chemotherapy and radiotherapy. Median time to relapse was 484 days. Three patients were stage II and did not receive any adjuvant therapy. Remaining three patients received modified folinic acid, oxaliplatin, fluorouracil–based combination (FOLFOX) ( n = 3) and one patient (rectal cancer) received adjuvant Chemoradiation. Twenty patients (64.5) received oxaliplatin-based first-line therapy. The most common regimen used as first line in palliative metastatic setting was capecitabine and oxaliplatin (CAPOX) ( n = 11, 35.48%) followed by mFOLFOX ( n = 9, 29.03%) and folinic acid, irinotecan, fluorouracil–based combination (FOLFIRI) ( n = 5, 16.13%). Only three patients underwent surgery for metastatic disease (pulmonary metastetectomy and hepatic resection.). The number of lines of chemotherapy given in metastatic setting were one ( n = 14, 45.16%), two ( n = 8, 25.81%), three ( n = 3, 9.68%), four ( n = 1, 3.23%), and five ( n = 5, 13%). Total of 14 patients received monoclonal antibodies of which 11 patients received in first line, 10 in second line, and 5 in third line setting. The most common biologic agent used was cetuximab ( n = 12) followed by bevacizumab ( n = 1) and panitumumab (only 1). Three patients received both anti–epidermal growth factor receptor (EGFR) and anti–vascular endothelial growth factor (VEGF) targeting biological therapies.
Adverse Events
The most common adverse event profile CTCAE) grades 3 and 4 from long-term exposure to multiple lines of chemotherapy were hematological toxicity ( n = 8) and peripheral neuropathy ( n = 2). Two patients had grades 3 and 4 diarrhea and febrile neutropenia. Other less common grades 3 and 4 adverse events included rash and hand foot syndrome ( n = 1) patient. No death was reported due to toxicity.
Outcomes
At the time of analysis, 10 patients are currently surviving. Six patients are maintaining radiological complete response. Three patients were lost to follow-up. Median overall survival (OS) of this cohort is 81.6 months (95% confidence interval [CI], 69.73–117.9) ( Fig. 1 ) and median progression-free survival (PFS) to first line therapy was 17.23 months (95% CI 13–46.8).
Fig. 1.
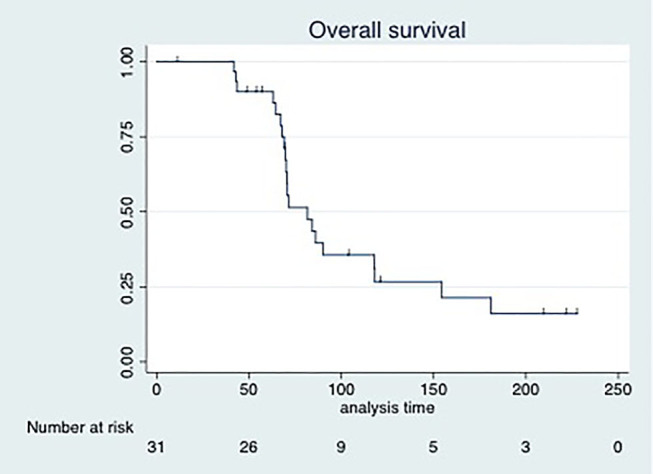
Overall survival of metastatic colorectal cancers (long term survivors).
Factors Predicting Survival
We performed regression analysis to determine the factors that predicted survival. The variables considered in our study were age, sex, sidedness, number of chemotherapy lines received, upfront metastatic presentation, and use of biologic agents. Female gender was the only factor found significant ( p = 0.031) in univariate analysis; however, the significance was not seen on multivariate regression analysis ( Table 2 ).
Table 2. Treatment characteristics.
| Characteristics | ( N )% |
|---|---|
| Chemotherapy regimens in first line | |
| FOLFOX | 9 (29.03) |
| FOLFIRI | 5 (16.13) |
| Cap-OX | 11 (35.48) |
| Cap IRI | 2 (6.45) |
| IFL | 4 (12.9) |
| Biological agents received | |
| Yes | 14 (45.16) |
| No | 17 (54.8) |
| Progression free survival (first line) | 17.23 months(13.0–46.8) |
| Median overall survival | 81.6 months(69.73–117.9) |
Table 3. Factors predicting overall survival.
| Factors | Univariate ( p -value) | Multivariate ( p -value) |
|---|---|---|
| Age (57 or less vs. more than 57) | 0.981 | – |
| Sex | 0.031 | 0.174 |
| Sidedness | 0.244 | – |
| Upfront metastatic presentation | 0.48 | – |
| Number of lines used (< or equal to 2) | 0.084 | 0.721 |
| Use of biologics | 0.057 | 0.148 |
Discussion
Long-term survivors of mCRC in literature has been defined conventionally as survival more than 5 years. mCRC has a median survival of 6 to 10 months with time-tested single agents like 5 FU. 6 Advent of doublet chemotherapeutic regimen including oxaliplatin and irinotecan has further contributed to the armamentarium against this disease. 7 8 The new era of biologicals and targeted therapy has ushered in changes in the outcomes and there is still uncertainty on how and to what extent these agents have an impact on survival. In the metastatic setting, “cure” per se has been a rare occurrence in colorectal cancers. However, in recent times long-term follow ups of various large multicenter trials have demonstrated a significant rise in patient population who have survived beyond the 5-year mark. 9 10 Evolution in surgical techniques like hepatic resection of metastasis has also contributed to prolongation in survival as reported in various studies. 11 Addressing the most common site of metastasis with improved infusional chemotherapy as well as newer surgical techniques has resulted in improvement of disease outcomes. 12 13 Concrete data to substantiate correlations of factors to long-term survival and actual magnitude of patient population who are achieving cure in real life is not much reported. Till date, only two large studies, MD Anderson Cancer Center 9 and NCCTG, 10 have addressed these patients and their characteristics. No data from India cohort are currently available which can provide us with the prevalence of prolonged survivors in our population.
In our study, 77% of patients presented to us as upfront metastatic disease. This analysis demonstrates that only a small proportion of our patients (10%) underwent metastatectomy and majority received chemotherapy only as part of therapy. Hence, our analysis highlights good and durable response achieved with chemotherapy alone. Presently six patients are maintaining complete response. This is somewhat comparable to the large retrospective study of mCRC by Ferrarrato et al from MD Anderson Cancer Centre, 9 where they reported six patients in CR on chemotherapy alone. Majority of our patients presented with left-sided colon cancer which now we know has a better prognosis. 14 The most common used biologic in our study was cetuximab. However, as the current evidence of use of cetuximab according to sidedness of the colon cancer was not available at the time of institution of biologics in our patients, the response correlation according to primary tumor location needs to be assessed in a larger cohort. 15
Toxicity is also a concern in long-term survivors and adverse effects like neuropathy can be disabling and have a bearing on quality of life. 16 Seven percent of our patients had residual grade III peripheral neuropathy. 17 Quality of life also takes precedence in analysis of long-term survivors and very few studies are available in literature to highlight this aspect. Our study did not include quality of life analysis.
It is hard to overlook the concepts of precision medicine and tailoring of therapy in subsequent lines. The approved agents like bevacizumab, cetuximab, and panitumumab have shown promise in prolongation of survival. 18 Our study almost 50% patients received at least one biologic agent. Genetic determinants of prolonged survival can be further analyzed in retrospective manner from bedside to the bench by tissue preservation and subjecting sample to specific of molecular and genetic testing.
The limitations of our study is its retrospective nature, less number of patients ( n = 31), limited number of patients exposed to all available options, and unavailability of MSI (microsattelite instability) and RAS (RA\at sarcoma virus gene) status in majority of the patients.
Survival data on newer regimens are sparse owing to heterogeneous nature or retrospective nature of studies. Addition of biologics may have a contribution to patients achieving and maintaining complete and partial responses beyond 5 years and needs to be examined in detail.
Conclusion
The term “cure” might not be a remote possibility in mCRC. A close scrutiny needs to be maintained on all the large multicenter trials and their long-term follow-ups to ascertain and validate these data. Although the patient number is small, durable responses achieved with chemotherapy and biological agents alone in a metastatic setting is encouraging and possible. Analysis from large institutional database should be carried out.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Fact Sheets by Cancer. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed April 27, 2018
- 2.Zacharakis M, Xynos I D, Lazaris A et al. Predictors of survival in stage IV metastatic colorectal cancer. Anticancer Res. 2010;30(02):653–660. [PubMed] [Google Scholar]
- 3.Chow FC-L, Chok KS-H. Colorectal liver metastases: an update on multidisciplinary approach. World J Hepatol. 2019;11(02):150–172. doi: 10.4254/wjh.v11.i2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kemeny N E. Treatment of metastatic colon cancer: “the times they are A-changing”. J Clin Oncol. 2013;31(16):1913–1916. doi: 10.1200/JCO.2013.49.4500. [DOI] [PubMed] [Google Scholar]
- 5.Heinemann V, Douillard J Y, Ducreux M, Peeters M. Targeted therapy in metastatic colorectal cancer—an example of personalised medicine in action. Cancer Treat Rev. 2013;39(06):592–601. doi: 10.1016/j.ctrv.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Perez N, Tournigand C, Mabro M et al. Long term survival in metastatic colorectal cancer treated with leucovorin and 5-fluoro-uracil chemotherapy. Rev Med Interne. 2004;25(02):124–128. doi: 10.1016/s0248-8663(03)00214-5. [DOI] [PubMed] [Google Scholar]
- 7.Sanoff H K, Sargent D J, Campbell M E et al. Five-year data and prognostic factor analysis of oxaliplatin and irinotecan combinations for advanced colorectal cancer: N9741. J Clin Oncol. 2008;26(35):5721–5727. doi: 10.1200/JCO.2008.17.7147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masi G, Loupakis F, Pollina L et al. Long-term outcome of initially unresectable metastatic colorectal cancer patients treated with 5-fluorouracil/leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) followed by radical surgery of metastases. Ann Surg. 2009;249(03):420–425. doi: 10.1097/SLA.0b013e31819a0486. [DOI] [PubMed] [Google Scholar]
- 9.Ferrarotto R, Pathak P, Maru D et al. Durable complete responses in metastatic colorectal cancer treated with chemotherapy alone. Clin Colorectal Cancer. 2011;10(03):178–182. doi: 10.1016/j.clcc.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 10.Dy G K, Hobday T J, Nelson G et al. Long-term survivors of metastatic colorectal cancer treated with systemic chemotherapy alone: a north central cancer treatment group review of 3811 patients, n0144. Clin Colorectal Cancer. 2009;8(02):88–93. doi: 10.3816/CCC.2009.n.014. [DOI] [PubMed] [Google Scholar]
- 11.Kopetz S, Chang G J, Overman M J et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27(22):3677–3683. doi: 10.1200/JCO.2008.20.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giacchetti S, Itzhaki M, Gruia G et al. Long-term survival of patients with unresectable colorectal cancer liver metastases following infusional chemotherapy with 5-fluorouracil, leucovorin, oxaliplatin and surgery. Ann Oncol. 1999;10(06):663–669. doi: 10.1023/a:1008347829017. [DOI] [PubMed] [Google Scholar]
- 13.Dattatreya S. Metastatic colorectal cancer-prolonging overall survival with targeted therapies. South Asian J Cancer. 2013;2(03):179–185. doi: 10.4103/2278-330X.114152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baran B, Mert Ozupek N, Yerli Tetik N, Acar E, Bekcioglu O, Baskin Y. Difference between left-sided and right-sided colorectal cancer: a focused review of literature. Gastroenterol Res. 2018;11(04):264–273. doi: 10.14740/gr1062w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holch J W, Ricard I, Stintzing S, Modest D P, Heinemann V. The relevance of primary tumour location in patients with metastatic colorectal cancer: a meta-analysis of first-line clinical trials. Eur J Cancer. 2017;70:87–98. doi: 10.1016/j.ejca.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Van L oon, K, Venook A P. Curable patient with metastatic colorectal cancer: balancing effective therapies and toxicities. J Clin Oncol. 2014;32(10):991–996. doi: 10.1200/JCO.2013.53.5195. [DOI] [PubMed] [Google Scholar]
- 17.Weickhardt A, Wells K, Messersmith W. Oxaliplatin-induced neuropathy in colorectal cancer [e-pub ahead of print] J Oncol. 2011;2011:201593. doi: 10.1155/2011/201593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.López-Gómez M, Merino M, Casado E. Long-term treatment of metastatic colorectal cancer with panitumumab. Clin Med Insights Oncol. 2012;6:125–135. doi: 10.4137/CMO.S5055. [DOI] [PMC free article] [PubMed] [Google Scholar]


