Abstract
The majority of chronic conditions that plague the USA are modifiable by lifestyle change. Lifestyle interventions that incorporate family members for social support and that use game design elements to engage family members have the potential to improve upon traditional interventions, which have largely been unsustainable. Determining the populations where family member support in a lifestyle intervention are present and the extent of gamification of lifestyle intervention components that engage these family members is an important and underexplored area of work. A systematic review of lifestyle interventions involving family members were reviewed for game design elements using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework. Game design elements related to engaged learning and motivational affordances from previous literature were included. Sixty-one studies met inclusion criteria. These studies reported on 50 independent interventions that were reviewed. Thirty-one of these interventions addressed lifestyle in those with a chronic condition, and 19 addressed lifestyle in those at high risk for chronic conditions. The majority of the lifestyle interventions included at least one game design element, yet overall there were limited elements utilized together. Compared with successful gamified programs that have greatly impacted a population’s health behaviors, there were relatively a limited number of elements reported, particularly those that support social relatedness, such as meaningful storylines. Meaningfulness of the game design elements chosen and their arrangement was not apparent. Technology was under-utilized as a potential modality for intervention component delivery. Developing products to train researchers to properly apply game design elements to intervention components, as well as test their effectiveness, are areas for future research.
Keywords: Game design, Gamification, Lifestyle intervention, Family member, Chronic conditions
Introduction
Over half of Americans live with at least one chronic condition, yet the majority are preventable with healthy lifestyle behaviors (Prevention, 2019). Lifestyle interventions, defined as any intervention that includes exercise, diet, and other behavioral components (Sumamo et al., 2011), can make an impact on health behavior change (Gillies et al., 2007; Hu et al., 2016). However, their effectiveness and sustainability have been elusive (Chesla et al., 2003; Fisher & Weihs, 2000; Gupta et al., 2019), with a lack of motivation to engage as a known barrier (Touyz et al., 2019). Lifestyle interventions, which seek to impact multiple behaviors, have begun to incorporate family members, recognizing lifestyle choices are made in the context of family. As Family system theory purports, choices and functioning of one family member impact other family members (Kerr, 1981). Family members have influence in the lived environment, and social support of participants can have a positive impact for change (Christakis & Fowler, 2013; Miller & Dimatteo, 2013). Additionally, family members can have a significant impact on a person’s ability and desire to change behaviors (Institute of Medicine (US) Committee on Health and Behavior: Research; Monden et al., 2003), and family member inclusion in behavioral intervention components positively assists participants to stay involved in the program (Gupta et al., 2019). Despite the known benefits of family support, strategic inclusion of family members in lifestyle interventions has been limited (Aschbrenner et al., 2015).
Strategically engaging individuals in interventions means optimizing their motivation to be involved by addressing their psychological needs. The Self-Determination Theory (SDT) purports that individuals have three psychological needs for optimal motivation: autonomy, perceived competence, and relatedness to others (Patrick & Williams, 2012). Changes in an individual’s environment can lead to fulfillment of these needs and foster motivation (Deci & Vansteenkiste, 2004). The fulfillment of these psychological needs can be found in previously identified strategies used to motivate family members in behavioral intervention. A review of family-based interventions for child physical activity found a handful of strategies used to motivate family member engagement (Brown et al., 2016). The strategies included goal-setting, recording or affirmation of performance, and rewards for achievement (Brown et al., 2016), which meet the psychological needs of autonomy and perceived competence. However, the extent of strategies incorporated to engage family members in lifestyle interventions, which seek to prevent and manage chronic conditions, has not been examined.
Traditional methods of engaging participants and family members in behavior change are intensive, in-person, and commonly delivered at one point in time, such as motivational interviews at the outset of a study (Burgess et al., 2017; Ingoldsby, 2010). However, sustaining motivation of family members, the social support system for individuals to maintain behavior change, require novel strategies that impact the same psychological needs as traditional interventions, yet are able to be delivered pragmatically for continual reach. One promising approach for sustained engagement of family members is the use of gamification. Gamification, the use of game design elements in non-game contexts (Deterding et al., 2011), seeks to motivate individuals to engage in a behavior over a period of time. Gamification has been used to motivate specific behaviors using intentionally arranged game building blocks, or game design elements, to impact the participant’s motivation (Deterding et al., 2011). Game design elements can be used to impact the psychological needs identified for optimal motivation (Sailer et al., 2017) and have done so in both the gaming context and in behavioral medicine (Edwards et al., 2016; Miller et al., 2016; Ryan et al., 2006). Gamification has been successful in engaging individuals in behavior change interventions. However, it is not known if game design elements have been used in lifestyle intervention components to motivate family members to engage.
While the use of gamification in facilitating the self-management of chronic conditions has been examined recently (Sola et al., 2015), there is a paucity of research that studies the impact of gamification on familial support. Determining the extent of gamification to engage the family, spouses and caregivers of those at high risk for chronic conditions or those that have chronic conditions is of particular interest. The use and potential benefits of gamification techniques amongst families in this highly prevalent population remain to be explored.
Because of these gaps in our understanding of family engagement in lifestyle intervention components using gamification for chronic condition prevention or management, we sought to answer the following:
How often and for what chronic disease conditions or prevention has gamification been used to increase family member engagement in lifestyle interventions?
Among studies that used gamification to increase family member engagement, what core elements of gamification were present?
Methods
Gamification is relatively new in the medical literature. We will describe our literature review process, as well as our theoretical framework that elucidates the theoretical underpinnings of the game design strategies and elements included in the review.
Data Collection
Initial searches for gamification in lifestyle interventions and those that involve family members were limited. We decided to cast a wider net for lifestyle interventions that involved family initially and search full text descriptions of intervention components for gamification elements. Due to our interest in lifestyle interventions for chronic condition prevention or management and to capture interventions that have been or will be tested in these populations, avoiding prototype or usability-only tested work, we focused our search on medical literature. PubMed, a resource from the National Center for Biotechnology and the National Library of Medicine with citations and abstracts from medicine, nursing, dentistry, health care systems and more, was used as our database (Williamson & Minter, 2019). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used to report the process (Moher et al., 2010).
Search Terms
We used search terms to capture studies on lifestyle interventions and family members or caregivers.
Lifestyle interventions AND (family[title/abstract] OR spouse[title/abstract] OR caregiver[title/abstract])
The full term “gamification” or truncated term “gamif*” were not used in the search term as previous gamification searches have done due to the limited literature captured during initial searches. The term gamification is relatively new, and the term’s use may not be widely utilized, yet the elements of gamification may be present. Therefore, we broadly captured lifestyle interventions that include family members, then sought to determine components of gamification by full study review.
Title and Abstract Review
The titles of the articles from the database search were reviewed for indication of lifestyle or chronic condition prevention. Family did not need to be mentioned in the title. Then, abstracts were reviewed to see if family were potentially involved in the lifestyle or chronic condition management or prevention effort. Inclusion Criteria. We included clinical trials, feasibility studies, implementation trials, protocol papers or reviews that had a lifestyle or refer to a chronic condition-prevention intervention, or a health behavior in the title. Exclusion Criteria. Because of our focus on gamification elements in intervention, we did not keep studies that did not focus on the lifestyle intervention itself, including qualitative-only analyses and cross-sectional studies that did not add any additional information about the intervention or its use. We excluded abstracts that solely included “family history” or “family practice,” as they did not refer to family members being a part of an intervention.
Full Text Review
Once family members were determined to be involved in a lifestyle intervention in some capacity, a full text review of studies was performed to determine (1) the type of family involvement in interventions and (2) which (if any) gamification elements included in intervention components. Inclusion Criteria. Studies with a description of intervention components or a reference to an article describing intervention components were included. Exclusion Criteria. Studies were excluded if (1) full text was not available, (2) the intervention was not described and there was no reference to a source for a description, or (3) family involvement was not mentioned. We removed ancillary or secondary studies of trials if they did not provide pertinent or additional information on the intervention and involvement of family members from original/primary or protocol papers.
Constructed Matrix
Data from the final studies included were extracted into a matrix, including sample, study design, components of intervention, type of family involved, extent of family involvement, and gamification elements.
Theoretical Framework
To guide our identification of gamification elements, we constructed a theoretical framework. Gamification strategies can help with the problem of motivation for sustained engagement by enhancing intrinsic motivation for engagement through external influence or modification of the environment (Vansteenkiste et al., 2010). The Self-Determination Theory (SDT), a theory of motivation, purports three psychological needs that are necessary for optimal motivation to be developed: relatedness to others, autonomy, and perceived competence (Patrick & Williams, 2012). Gamification strategies have been shown to meet these basic needs using motivational theory (Sailer et al., 2017). In addition, educational frameworks have informed gamification design strategies, including the Theory of Intrinsically motivated instruction and the “Working on the Work” framework, for continual learner engagement (Dickey, 2005; Schlechty, 2011). Briefly, as instructors design work or activities for learners to engage in to meet learners’ needs, the quality of design influences the level of engagement from learners. Learner engagement can be enhanced by the type of design inserted into the work or activity—such as including qualities that are most likely to appeal to learners’ values, interests and needs (Schlechty, 2011). Game design element qualities can fulfill learners’ interests and reflect these qualities (Dickey, 2005). Our theoretical framework is modeled in Fig. 1.
Fig. 1.
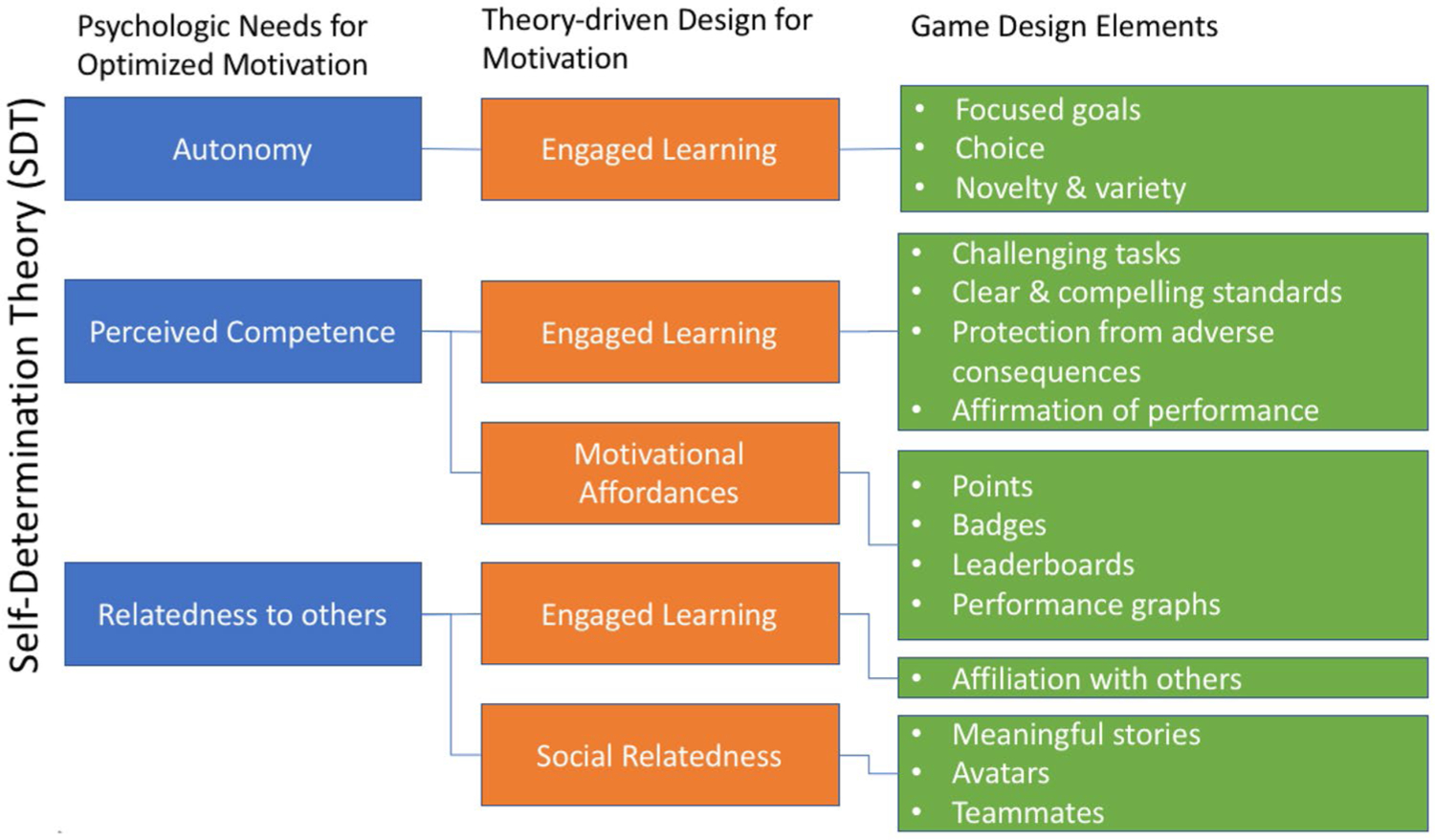
Motivation for sustained engagement theoretical framework
Briefly, game elements based on educational and motivational theory are designed to meet basic psychologic needs for optimized motivation. Autonomy can be promoted with psychological freedom to make choices on one’s values and interests, and volition to achieve one’s goals (Deci & Ryan, 2012). Game design elements derived from engaged learning strategies support autonomy through a chosen goal and providing choices, and even better—providing novel or a variety of—choices. Perceived competence can be promoted by feelings of efficiency and success, even in game design (Rigby & Ryan, 2011). Game design elements informed by engaged learning strategies promote learning with challenging tasks and clear standards, along with feelings of success using protection and affirmation. Motivational affordances using points, badges, leaderboards, and performance graphs can help with continual engagement by earning and viewing success. Social relatedness, or feeling belonging, attachment and care with others—beyond oneself—is fulfilled in both engaged learning and social relatedness (Deci & Vansteenkiste, 2004). Game design element affiliation with others promotes relatedness through engaged learning together. Further, social relatedness can be promoted through stories that are meaningful to the participants, avatars that are alike to or meaningful to the participants, or teammates that share a goal or common experience.
Identifying Gamification Elements
Gamification can take many forms using a combination of different game design elements to create the environment for learning and activation (Sailer et al., 2017). To determine the degree of gamification present in intervention components, we included previously identified categories of game design elements to use in our review (see Framework). We searched for game design elements that reflect engaged learning strategies, which were utilized for the engagement of participants and family members in intervention components. These elements included focused goals, challenging tasks, clear and compelling standards, protection from adverse consequences, affirmation of performance, affiliation with others, novelty and variety, and choice (Dickey, 2005). Additionally, we searched for game design elements that are known motivational affordances and were utilized for participant or family member action related to intervention components or behavior change. These included elements of points, achievements/badges, leaderboards, and performance graphs, as they impact competence and perceived task meaningfulness (Sailer et al., 2017). Additionally, elements of meaningful stories, avatars, and teammates were admitted, as these influence experiences of social relatedness (Sailer et al., 2017). Upon review of an intervention, we identified details in component descriptions that mirror these elements and extracted this information into a matrix. For each intervention, we have reported the number and type of game design elements present in the studies reviewed.
Inter‑rater Reliability
After the interventions were organized in a matrix, we conducted inter-rater reliability of game element coding for each independent intervention following a standard approach for systematic reviews (Belur et al., 2018). Selecting a random sample of interventions (using an online random sample generator), two team members coded independently and then came together to discuss coding and resolve differences by consensus. Overall, there were five rounds of coding and discussion, with three sessions examining 5 interventions (10% each session, 30% overall), then two sessions examining 10 interventions (20% each session, 40% overall). During each review, we discussed our definitions of game elements and made minor clarifying adjustments. We present our final definitions in Table 1. We calculated inter-rater reliability (IRR) on the presence or absence of game elements in each intervention and present our percent agreement and the kappa statistic for each session. Once our K statistic exceeded the threshold of 0.6 in several sessions (McHugh, 2012), we were confident in our coding reliability and game element definitions. One team member continued coding the remaining 15 interventions independently. We report our IRR results in Table 2.
Table 1.
Game element definitions
| Game element | Psychological need | Definition |
|---|---|---|
| Motivational affordances (Sailer et al., 2017) | ||
| Points | Perceived competence | A basic element of games, they are often numeric and the reward for successful accomplishment of specified activities and allow behavior to be measured. |
| Badges | Perceived competence | Visual representation of achievements, and can be earned by achieving goals, rewarding progress or completing tasks in the intervention. This is opposed to tracking progress, as done in affirmation of performance. |
| Leaderboards | Perceived competence | A system of ranking individuals based on their success by comparing individuals’ performance with that of others’ performance. This system is continually updated for individual’s viewing, and not a one-time assessment, in order to motivate over time. |
| Performance graphs | Perceived competence | Evaluation of individual’s performance over time by comparing individuals’ current performance to their previous performance. Visual representation of performance is used to motivate change. |
| Social relatedness (Sailer et al., 2017) | ||
| Meaningful stories | Relatedness to others | A narrative that gives meaning or context to tasks, activities or performance, moving motivation beyond the achievement of points or goals. The narrative can be simple or complex and can involve individuals as characters or not. |
| Avatars | Relatedness to others | Visual representations of players or story characters, which range in complexity and inter-activeness. |
| Teammates | Relatedness to others | Clearly designated individuals to partner with the individual toward a goal. These individuals can be selected or assigned, real or virtual, and are designed to support performance, whether through inducing conflict, competition or cooperation toward a shared goal. |
| Engaged learning strategies (Dickey, 2005; Schlechty, 2011) | ||
| Design qualities of context | ||
| Focused goals | Autonomy | Defined, measurable results or achievements the individual aims to complete or succeed in by participating. These may be structured tasks or activities that link learning to some product, performance, or exhibition—such as a change in behavior—to which the individual attaches personal value. |
| Challenging tasks | Perceived competence | Structured tasks that are sufficiently difficult so that the individual needs to put forth effort for achievement—typically beyond a standard approach, and ideally believe they will accomplish something of worth by completing them. |
| Clear and compelling standards | Perceived competence | The extent to which individuals are clear about what standards will be applied to evaluate their performance, typically determined by an outside authority (i.e., national guidelines) and how much value individuals attach to the standards that are to be used, ideally seeing them as personally compelling. |
| Protection from adverse consequences | Perceived competence | The extent to which the task is designed so individuals feel free to try without fear that initial failures will bring them humiliation, implicit punishment, or negative sanctions. |
| Design qualities of choice | ||
| Affirmation of performance | Perceived competence | The design of tasks and activities so that the individuals’ performance is made visible to themselves and/or others who are likely to, or instructed to, provide feedback. |
| Affiliation with others | Relatedness to others | The design of tasks so that individuals are provided the opportunity to participate in the activity with others—typically a group, so as it is done together. Others can be peers, family, outside experts, or more, but not the creators or implementers of the tasks. This differs from teammates, where an individual is specifically assigned or chosen to partner with the individual to reach a goal. |
| Novelty and variety | Autonomy | Providing individuals the opportunity to employ a wide range of media and approaches when engaged in the activities assigned and encouraged. The approaches should diverge from or are in addition to standard approaches, ideally being unique or place a twist on standard approaches. |
| Choice | Autonomy | The design of tasks and activities so that individuals can exercise choice either in what they are to achieve or how they go about their achievement. |
Definitions are modified for non-educational context and for behavior change.
Table 2.
Game design element coding inter-rater reliability by session
| First session IRR |
Second session IRR |
Third session IRR |
Fourth session IRR |
Fifth session IRR |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Interventions | 5 | 100 | 5 | 100 | 5 | 100 | 10 | 100 | 10 | 100 |
| Gamification elements coded | 75 | 100 | 75 | 100 | 75 | 100 | 150 | 100 | 150 | 100 |
| Individual coding—agreement | 48 | 64.0 | 18 | 76.0 | 67 | 89.3 | 127 | 84.7 | 132 | 88.0 |
| Agreement after discussion | 75 | 100 | 75 | 100 | 75 | 100 | 150 | 100 | 150 | 100 |
| K | Std. error | K | Std. error | K | Std. error | K | Std. error | K | Std. error | |
| K statistic* | 0.24 | 0.08 | 0.26 | 0.11 | 0.65 | 0.12 | 0.54 | 0.08 | 0.65 | 0.08 |
All p < 0.05
Results
We identified 267 papers from the medical literature, with 264 from the database search and 3 from additional sources. Of these, 109 were removed by title review, and 63 by abstract review. Of the 95 articles included in full text review, 34 were removed for the following reasons: family involvement in an intervention was not mentioned (n = 9), ancillary or secondary analyses that did not provide any additional information or were irrelevant (n = 8), descriptive or commentary articles that did not provide any information on family involvement (n = 6), full text was not available from the institution (n = 5), study targets the family member only (n = 3), and family were not involved in the intervention (n = 3). Sixty-one studies were included, with 56 studies reporting on 50 independent interventions and 5 literature reviews. Data from the 50 lifestyle interventions reported on by 56 studies were extracted to a matrix (available online). Five reviews based on family and lifestyle interventions were included and were examined for additional studies for inclusion. Studies in reviews were either already included from the database search (Admiraal et al., 2013; Bhopal et al., 2014) or did not meet inclusion criteria (Babamoto et al., 2009; Becker et al., 2005; Chiang & Sun, 2009; Woodruff et al., 2002). Our process is reported using PRISMA (Fig. 2).
Fig. 2.
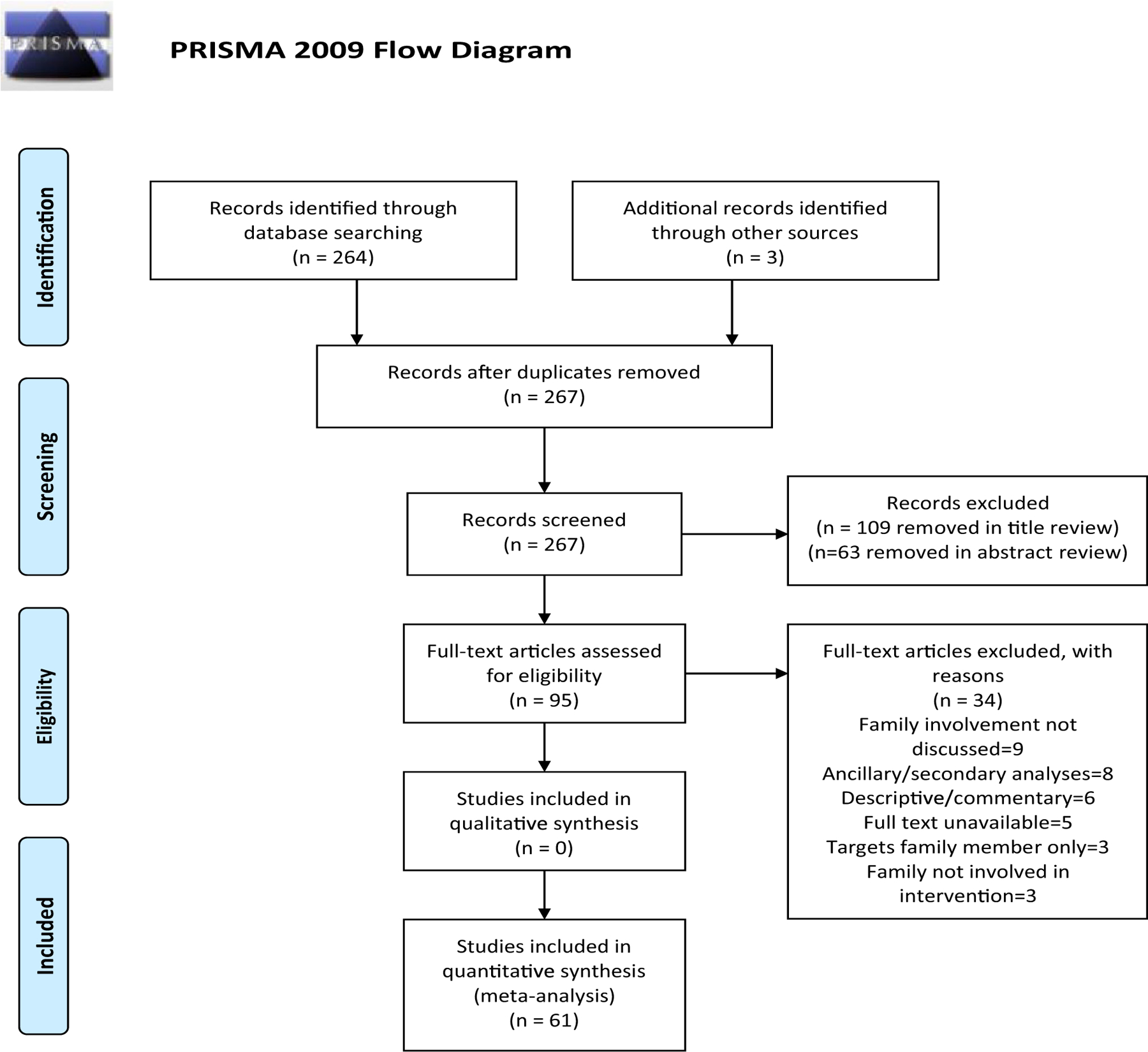
PRISMA flow diagram
We found lifestyle interventions were designed to either manage chronic conditions (n = 31) or to prevent the onset of chronic conditions for at-risk populations (n = 19) (Table 3). For lifestyle interventions designed for chronic condition management (n = 31), obesity was by far the most common chronic condition targeted (n = 25/31; 81%) and nearly all of these included children (n = 21/25, 88%), followed by adolescents (n = 5/25, 20%), and adults (n = 1/25, 4%). Parents or guardians were a part of every intervention for obesity, with two additionally including other members of the family, such as siblings. Interventions for diabetes management (n = 4/31; 13%) included whole communities (n = 2/4; 50%), adult daughters and mothers (n = 1/4, 25%), and youth (n = 1/4, 25%). Lastly, one intervention addressed high blood pressure in children and young adults in a middle eastern country (n = 1/31; 3%) and one addressed asthma management in children (n = 1/31; 3%). The majority of studies reviewed were clinical trials (n = 16/36; 44%), followed by protocol papers (n = 9/36, 25%), preliminary or secondary analyses (n = 6/36, 17%), and pilot or feasibility studies (n = 5/36, 14%).
Table 3.
Description of included lifestyle interventions
| Populations addressed | Interventions, n (%) |
|---|---|
| Interventions for populations with chronic conditions | 31 (100) |
| Population | |
| Obesity or overweight | 25 (81) |
| Diabetes | 4 (13) |
| Cardiovascular disease | 1 (3) |
| Asthma | 1 (3) |
| Age group | |
| Children or adolescents | 26 (84) |
| Adults or whole family/community | 5 (16) |
| Interventions for populations with chronic conditions | 19 (100) |
| Population | |
| Obesity or overweight | 9 (47) |
| Diabetes | 7 (37) |
| Cardiovascular disease | 3 (16) |
| Age group | |
| Children or adolescents | 10 (53) |
| Adults or whole family/community | 9 (47) |
Lifestyle interventions to prevent chronic conditions (n = 19) were more balanced in population type, with almost half addressing adults or communities (n = 9/19, 47%). Obesity was still the most commonly addressed chronic condition—but for prevention (n = 9/19, 47%), with the majority of these targeting children (7/9, 79%), one for Latino mother-daughter dyads (n = 1/9, 11%), and one for people with serious mental illness (n = 1/9, 11%). Diabetes prevention interventions (n = 7/19, 37%) targeted both adults or communities (n = 4/7, 57%) and children (n = 3/7, 43%). Cardiovascular disease prevention interventions (n = 3/19, 16%) targeted whole families at risk (n = 1/2, 50%) and adults (n = 1/2, 50%). There were a similar amount of studies reporting clinical trials for lifestyle interventions for prevention (n = 11/21, 52%), but more pilot or feasibility studies (n = 5/21, 24%) and protocol papers (n = 4/21, 19%), and one secondary analysis (n = 1/21, 5%).
Many gamification elements related to engaged learning were prevalent in the interventions examined (Table 4). Affiliation with others was the most common element reported (n = 33), followed by focused goals (n = 29), novelty and variety (n = 22), affirmation of performance (n = 20), clear and compelling standards (n = 19), choice (n = 17), and challenging tasks (n = 13). Protection from adverse consequences for initial failures was under-used. Motivational affordances were not commonly employed, with teammates (n = 10) and performance graphs/levels (n = 7) used occasionally, and meaningful stories, badges, points, and leaderboards rarely used. Avatars were not mentioned at all. No clear pattern of lifestyle interventions favoring a particular psychological need addressed by the game elements was noted. While affiliation with others was the most frequent game element, all other game elements fulfilling the psychological need of relatedness to others were used infrequently.
Table 4.
Gamification elements included in lifestyle interventions involving family members
| Gamification element | Psychological need | Number of interventions with element | Examples of element from interventions included |
|---|---|---|---|
| Game design elements reflecting engaged learning | |||
| Affiliation with others | Relatedness to others | 33 | • Facebook support group for caregivers (Ling, 2018) • Web social support (Po’e, 2013) |
| Focused goals | Autonomy | 29 | • Goals set between parents and children (Waling, 2012) • Spouses support and focus on participant’s goals, avoiding criticism (King, 2014) |
| Novelty and variety | Autonomy | 22 | • Online synchronous meetings on website with coach and families (Hingle, 2019) • Child sends parent “letter” over FB messenger with food would like to try in next month (Ling, 2018) |
| Affirmation of performance | Perceived competence | 20 | • Real-time assessments based on sensors (Fedele, 2019; Espinoza, 2017) • Support for those not making goals (Bock, 2014) |
| Clear and compelling standards | Perceived competence | 19 | • Follow national recommendations on diet (Graziano, 2017, Diaz, 2010) |
| Choice | Autonomy | 17 | • Type of physical activity, with indoor sports tickets and exercise equipment offered (Viitasalo, 2016) |
| Challenging tasks | Perceived competence | 13 | • Modify recipes (Savoye, 2011) • Assignments and activities related to health behaviors for parents and children between sessions (Waling, 2012, Brennan, 2013) |
| Protection from adverse consequences for initial failures | Perceived competence | 3 | • “Power time” interactive lab between parents and children to try new snacks (Smith, 2013) • Practice problem solving (Fenner, 2016) • Work together on workbook activities (Catenacci, 2014) |
| Game design elements reflecting motivational affordances | |||
| Teammates | Relatedness to others | 10 | • Partners had shared goals and tracking (Aschbrenner, 2015) • Children and parents work as team to modify family recipes (Savoye, 2011) |
| Performance graphs/Levels | Perceived competence | 7 | • Sensor data downloaded and tracked at doctor’s office (Espinoza, 2017) or posted to FB (Ling, 2018) |
| Meaningful stories | Relatedness to others | 3 | • Culturally-specific stories written on living with and managing diabetes (Gilliland, 2002) |
| Badges | Perceived competence | 2 | • Spouse identifies reward for progress toward goals (King, 2014) |
| Points | Perceived competence | 2 | • Points awarded for reaching goals, translate into family-provided rewards (TODAY 2010) |
| Leaderboard | Perceived competence | 1 | • Teams were placed in order of success toward goals (Martin, 2009) |
| Avatars | Relatedness to others | 0 | |
There were several differences in game design elements utilized between interventions for chronic condition management and for chronic condition prevention (Table 5). Interventions for condition management were more likely to use clear and compelling standards (52% v. 16% of interventions for prevention) for engagement, while interventions for prevention were more likely to use novelty and variety (63% v. 32% of interventions for management) and performance graphs or levels (21% v. 10% of management) (Table 6).
Table 5.
Proportion of gamification elements included in interventions for populations with chronic conditions and interventions for disease prevention in populations at risk
| Gamification element | Psychological need | Number of interventions with element | Population type |
|
|---|---|---|---|---|
| Condition management (N = 31) | Condition prevention (N = 19) | |||
| N (%) | N (%) | |||
| Total interventions | 31 (100) | 19 (100) | ||
| Game design elements reflecting engaged learning | ||||
| Affiliation with others | Relatedness to others | 33 | 20 (64) | 13 (68) |
| Focused goals | Autonomy | 29 | 17 (55) | 12 (63) |
| Novelty and variety | Autonomy | 22 | 10 (32) | 12 (63) |
| Affirmation of performance | Perceived competence | 20 | 13 (42) | 7 (37) |
| Clear and compelling standards | Perceived competence | 19 | 16 (52) | 3 (16) |
| Choice | Autonomy | 17 | 12 (39) | 5 (26) |
| Challenging tasks | Perceived competence | 13 | 8 (26) | 5 (26) |
| Protection from Adverse consequences for initial failures | Perceived competence | 3 | 2 (6) | 1 (5) |
| Game design elements reflecting motivational affordances | ||||
| Teammates | Relatedness to others | 10 | 7 (22) | 3 (16) |
| Performance graphs | Perceived competence | 7 | 3 (10) | 4 (21) |
| Meaningful stories | Relatedness to others | 3 | 2 (6) | 1 (5) |
| Badges | Perceived competence | 2 | 1 (3) | 1 (5) |
| Points | Perceived competence | 2 | 2 (6) | 0 (0) |
| Leaderboard | Perceived competence | 1 | 1 (3) | 0 (0) |
| Avatars | Relatedness to others | 0 | 0 (0) | 0 (0) |
Table 6.
Proportion of gamification elements included in interventions for populations with chronic conditions and interventions for disease prevention in populations at risk by chronic condition type
| Condition management (N = 31) |
Condition prevention (N = 19) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Gamification element | Number of interventions with element | Obesity or overweight | Diabetes | Cardiovascular disease | Asthma | Obesity or overweight | Diabetes | Cardiovascular disease |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Total interventions | 25 (100) | 4 (100) | 1 (100) | 1 (100) | 9 (100) | 7 (100) | 3 (100) | |
| Game design elements reflecting engaged learning | ||||||||
| Affiliation with others | 33 | 15 (60) | 3 (75) | 1 (100) | 1 (100) | 5 (56) | 6 (86) | 2 (67) |
| Focused goals | 29 | 14 (56) | 2 (50) | 0 (0) | 1 (100) | 6 (67) | 4 (57) | 2 (67) |
| Novelty and variety | 22 | 8 (32) | 1 (25) | 0 (0) | 1 (100) | 5 (56) | 6 (86) | 1 (33) |
| Affirmation of performance | 20 | 11 (44) | 1 (25) | 0 (0) | 1 (100) | 4 (44) | 3 (43) | 0 (0) |
| Clear and compelling standards | 19 | 13 (52) | 1 (25) | 1 (100) | 1 (100) | 1 (11) | 2 (28) | 0 (0) |
| Choice | 17 | 9 (36) | 2 (50) | 0 (0) | 1 (100) | 3 (33) | 1 (14) | 1 (33) |
| Challenging tasks | 13 | 7 (28) | 1 (25) | 0 (0) | 0 (0) | 4 (44) | 1 (14) | 0 (0) |
| Protection from adverse consequences for initial failures | 6 | 2 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (33) |
| Game design elements reflecting motivational affordances | ||||||||
| Teammates | 10 | 6 (24) | 1 (25) | 0 (0) | 0 (0) | 2 (22) | 0 (0) | 0 (0) |
| Performance graphs | 7 | 3 (12) | 0 (0) | 0 (0) | 0 (0) | 3 (33) | 1 (14) | 0 (0) |
| Meaningful stories | 3 | 1 (4) | 1 (25) | 0 (0) | 0 (0) | 1 (11) | 0 (0) | 0 (0) |
| Badges | 2 | 0 (0) | 1 (25) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (33) |
| Points | 2 | 1 (4) | 1 (25) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Leaderboard | 1 | 1 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Avatars | 0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Game Elements by Chronic Condition Type
High use of affiliation with others across all conditions (range 56 to 100%) commonly facilitated by sharing experiences in group sessions. Focused goals were also highly prevalent for the majority of conditions (range 50 to 100%, except for cardiovascular management), typically with family members creating specific behavioral goals with participants. Diabetes prevention had a high amount of novelty and variety in their interventions (86%), including cooking demonstrations, food sampling, and supermarket tours. Almost half of obesity prevention interventions (44%) included challenging tasks, like homework, or intensive physical activity.
Game Elements by Age Group
Management interventions for children were more likely to use points (n = 2), badges (n = 1), and leaderboards (n = 1) than management interventions for adults. There were not any differences in game elements used between children or adolescents and adults for preventive interventions.
Discussion
While nearly two out of three lifestyle interventions to prevent or manage chronic medical conditions used at least one element of gamification, the overall use of game elements was relatively limited compared with well-known, successful games that have had a large impact on behavior change on a population level (Baranowski & Lyons, 2019). Our study highlights the potential to integrate multiple gamification elements into lifestyle interventions that involve family members to enhance motivation. We will discuss the populations that currently have family members included in lifestyle interventions, the amount and meaningfulness of the gamification elements found, and areas for future work.
Management and Prevention of Chronic Conditions
Chronic condition management lifestyle interventions are further along in the evolution than prevention interventions, with more interventions trialed and a number of recent protocols written. These interventions appeared more focused in the guidelines used for participants to make their goals and used affirmation as these goals were being achieved. Prevention studies for high risk populations are important and a budding area for research. Interventions for prevention currently have a heavier focus on participant competence and perceived task meaningfulness, along with building social support from a broader community (i.e., Facebook group or classmates with similar goals). Additionally, only a handful of conditions were identified by our review. These conditions, obesity, diabetes, and heart disease, are of major interest in public health and primary care specialties. Other chronic conditions, such as cancer survivors, were not found. For cancer survivorship, this is likely due to a lack of focus on family member inclusion in interventions, yet family social support has been found to be a major factor on the road to behavior change in the cancer survivor population (Blok et al., 2017; Green et al., 2015). There is a clear opportunity to expand gamified lifestyle interventions targeting family members to other chronic conditions.
Game Design Elements
Focused goals were the most common element found, with both the participant and the family member creating the goal together. This was not a surprising finding, as lifestyle interventions are commonly upfront with participants that their purpose is to make a change happen in areas of behavior, and create programs or activities that assist participants in achieving behavior goals. A goal to initiate a change in behavior was commonly the first step, followed by other game elements to enhance goal-directed behaviors. We noted intervention use of some elements that build external motivation (such as challenging tasks, affirmation of performance, badges), but failed to include multiple elements that build this motivation over time (points and leaderboards), likely limiting its impact. The Organismic Integration Theory suggests a continuum between external and internal motivators (Dickey, 2005). Game design elements are created to work together for the development of motivation (Werbach, 2014). For example, when using the element of affirmation of progress toward a goal, linking an external goal of scoring points and competing on a leaderboard with others can motivate participants to continue to reach for this goal, in turn building internal motivation and practice with a new behavior over time.
While game elements are the building blocks of gamification, there is a question of to what extent the use of individual game elements can be considered “meaningful gamification” (Deterding et al., 2011)? We noted that none of the elements included are there solely as feedback or an end to themselves. As the primary goal of a lifestyle intervention is to change a participant’s behavior, each component of the intervention is designed to work toward that goal. Therefore, each element applied in a lifestyle intervention context is inherently there to motivate a participant’s behaviors to improve their health; its intention is to woo the participant into being engaged for a longer period of time and evoke a sense of purpose for change. Each of these elements can be considered gamification in a lifestyle change context. However, multiple areas that assist in building gamification were not found in this review. These include the relative absence of gamification elements that promote social relatedness, a lack of meaningful selection and integration of elements, and technology use.
Social Relatedness
Chronic condition management or prevention interventions almost entirely ignored elements that build social relatedness. Meaningful stories were used only three times, and leaderboards, where competition inspires a higher level of engagement, were not used at all. Teammates were used solely in cooperation, as opposed to infusing competition between participants and family members in behavior change. Autonomy using choice was minimal considering the variety of ways diet and activity can be modified, and avatars, or visual representations of players, were not included. Story-telling has been a recent phenomena in self-management of chronic conditions and is ripe for integration into lifestyle interventions (Frank et al., 2015). A smartphone game with an elaborate storyline which was recently tested increased the steps per day of participants with type 2 diabetes (Höchsmann et al., 2019). Lifestyle interventions are ripe to harness social reference and autonomy in inspiring motivation for behavior change.
Meaningful Selection
While the interventions overall were built on theoretical foundations, the purposeful selection and integration of the game elements themselves were not commonly apparent. Gamification does not only consider the game design elements themselves, but how they work together for motivation (Werbach, 2014). Many interventions incorporated a variety of elements, but they did not appear intentional in their selection in how they work together to motivate. Commonly coupled elements, such as points, badges and leaderboards, were not found present together (Werbach & Hunter, 2012). This is likely due to the lack of familiarity and training of interventionists in gamification principles. However, this may be needed, as working with children and families, there needs to be significant effort in engaging them early on and long enough to inspire lasting change. Further interventional work, such as testing the combination of different elements for behavior change, is needed.
Technology Use
Technology was also not commonly found to be a modality utilized for lifestyle intervention in this review. Technologies for behavior change that incorporate gamificiation principles may be just beginning to be developed, such as the Nutriscience Project, a web-based gamified program for nutrition literacy in families just reported earlier this year (Azevedo et al., 2019). Technology is also a low-cost way to deliver lifestyle interventions, leading to the potential for further reach and engagement of participants and family members (Orji & Moffatt, 2016). Family members, unlike gaming “communities,” do care about the participant’s success in lifestyle change for disease prevention or management. Creation of games with design elements embedded in technology to assist in positive interactions participants and family members for behavior change is an imminent area of research.
Limitations
This review, while the first to examine this topic, relied on a relatively limited number of databases for the identification of potentially eligible studies. However, the 5 systematic reviews in our results did not report any additional studies cited in them that fit our criteria support, strengthening our belief that PubMed captured the relevant literature to answer our research questions. Additionally, the assessment of study quality was limited due to the objectives of determining gamification use and core elements present in current literature. While we were able to determine the presence of game elements, we were not commonly able to determine the logic for the use of a particular game element. Future work on determining logic models behind intervention design decisions using program manuals and supplemental elicitation from intervention developers would add to the literature.
Conclusion
The majority of chronic conditions that plague the USA are modifiable by lifestyle change. Lifestyle interventions that incorporate family members and engage them using game design elements have the potential to improve upon traditional interventions without these elements. Determining the extent of gamification of lifestyle intervention components that seek to engage family members is an important and underexplored area of work. We found the majority of lifestyle interventions that include family members use at least one game design element. Yet, compared with other successful gamified programs, lifestyle interventions targeted at family member engagements tended to have a more limited number of elements reported, particularly in those that support social relatedness, such as meaningful storylines. This suggests that these lifestyle interventions under-utilized technology as a potential modality to create engagement and for intervention component delivery.
Acknowledgements
We thank Clarice E. Hibbard, BAS, for her contribution in testing the inter-rater reliability, or consensus, of our review.
Funding
The preparation of this paper was supported by the Department of Veterans Affairs Center for Clinical Management Research (CCMR), the University of Michigan School of Nursing’s Systems, Populations and Leadership Department, the National Institues of Health (K23HL140165), and the Agency for Healthcare Research and Quality (AHRQ R01HS028038).
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s11121-021-01214-x.
Code availability PRISMA was used to guide the review. The search code is located in the methods section of the manuscript.
Declarations
Ethics Approval This review of the literature did not required approval from an ethics committee.
Informed Consent This review did not require recruitment of human subjects.
Conflict of Interest The authors declare that they have no conflict of interest.
Standards of Reporting This review did use the recommended reporting for systematic reviews; the Preferred reporting items for systematic reviews and meta-analyses (PRISMA).
References
- Admiraal WM, Vlaar EM, Nierkens V, Holleman F, Middelkoop BJ, Stronks K, & van Valkengoed IG (2013). Intensive lifestyle intervention in general practice to prevent type 2 diabetes among 18 to 60-year-old South Asians: 1-year effects on the weight status and metabolic profile of participants in a randomized controlled trial. PLoS One, 8, e68605. 10.1371/journal.pone.0068605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner K, Mueser K, Bartels S, Carpenter-Song E, Pratt S, Barre L, et al. (2015). The other 23 hours: a qualitative study of fitness provider perspectives on social support for health promotion for adults with mental illness. Health & Social Work, 40, 91–99. 10.1093/hsw/hlv006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azevedo J, Padrão P, Gregório MJ, Almeida C, Moutinho N, Lien N, & Barros R (2019). A web-based gamification program to improve nutrition literacy in families of 3- to 5-year-old children: The nutriscience project. Journal of Nutrition Education and Behavior, 51, 326–334. 10.1016/j.jneb.2018.10.008 [DOI] [PubMed] [Google Scholar]
- Babamoto KS, Sey KA, Camilleri AJ, Karlan VJ, Catalasan J, & Morisky DE (2009). Improving diabetes care and health measures among hispanics using community health workers: Results from a randomized controlled trial. Health Education & Behavior, 36, 113–126. 10.1177/1090198108325911 [DOI] [PubMed] [Google Scholar]
- Baranowski T, & Lyons EJ (2019). Scoping Review of Pokémon Go: Comprehensive assessment of augmented reality for physical activity change. Games for Health Journal 10.1089/g4h.2019.0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker DM, Yanek LR, Johnson WR, Garrett D, Moy TF, Reynolds SS, et al. (2005). Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation, 111, 1298–1304. 10.1161/01.CIR.0000157734.97351.B2 [DOI] [PubMed] [Google Scholar]
- Belur J, Tompson L, Thornton A, & Simon M (2018). Interrater reliability in systematic review methodology: Exploring variation in coder decision-making. Sociological methods & research, 0049124118799372.
- Bhopal RS, Douglas A, Wallia S, Forbes JF, Lean ME, Gill JM, et al. (2014). Effect of a lifestyle intervention on weight change in south Asian individuals in the UK at high risk of type 2 diabetes: A family-cluster randomised controlled trial. Lancet Diabetes Endocrinol, 2, 218–227. 10.1016/s2213-8587(13)70204-3 [DOI] [PubMed] [Google Scholar]
- Blok AC, Blonquist TM, Nayak MM, Somayaji D, Crouter SE, Hayman LL, et al. (2017). Feasibility and acceptability of “healthy directions” a lifestyle intervention for adults with lung cancer. Psychooncology 10.1002/pon.4443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock DE, Robinson T, Seabrook JA, Rombeek M, Norozi K, Filler G, Rauch R, & Clarson CL (2014). The Health Initiative Program for Kids (HIP Kids): effects of a 1-year multidisciplinary lifestyle intervention on adiposity and quality of life in obese children and adolescents--a longitudinal pilot intervention study. BMC Pediatrics, 14, 296. 10.1186/s12887-014-0296-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan L, Walkley J, Wilks R, Fraser SF, & Greenway K (2013). Physiological and behavioural outcomes of a randomised controlled trial of a cognitive behavioural lifestyle intervention for overweight and obese adolescents. Obesity research & clinical practice, 7(1), e23–41. 10.1016/j.orcp.2012.02.0102012.02.010 [DOI] [PubMed] [Google Scholar]
- Brown HE, Atkin AJ, Panter J, Wong G, Chinapaw MJ, & van Sluijs EM (2016). Family-based interventions to increase physical activity in children: A systematic review, meta-analysis and realist synthesis. Obesity Reviews, 17, 345–360. 10.1111/obr.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess E, Hassmén P, Welvaert M, & Pumpa KL (2017). Behavioural treatment strategies improve adherence to lifestyle intervention programmes in adults with obesity: A systematic review and meta-analysis. Clinical Obesity, 7, 105–114. 10.1111/cob.12180 [DOI] [PubMed] [Google Scholar]
- Catenacci VA, Barrett C, Odgen L, Browning R, Schaefer CA, Hill J, & Wyatt H (2014). Changes in physical activity and sedentary behavior in a randomized trial of an internet-based versus workbook-based family intervention study. Journal of Physical Activity and Health, 11(2), 348–358. 10.1123/jpah.2012-00432012-004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesla CA, Fisher L, Skaff MM, Mullan JT, Gilliss CL, & Kanter R (2003). Family predictors of disease management over one year in Latino and European American patients with type 2 diabetes. Family Process, 42, 375–390. [DOI] [PubMed] [Google Scholar]
- Chiang CY, & Sun FK (2009). The effects of a walking program on older Chinese American immigrants with hypertension: A pretest and posttest quasi-experimental design. Public Health Nursing, 26, 240–248. 10.1111/j.1525-1446.2009.00776.x [DOI] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2013). Social contagion theory: Examining dynamic social networks and human behavior. Statistics in Medicine, 32, 556–577. 10.1002/sim.5408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, & Ryan RM (2012). Motivation, personality, and development within embedded social contexts: An overview of self-determination theory
- Deci EL, & Vansteenkiste M (2004). Self-determination theory and basic need satisfaction: Understanding human development in positive psychology. Ricerche di psicologia
- Deterding S, Sicart M, Nacke L, O’Hara K, & Dixon D (2011). Gamification: Using game design elements in non-gaming contexts. ACM CHI Conference on Human Factors in Computing Systems. [Google Scholar]
- Diaz RG, Esparza-Romero J, Moya-Camarena SY, Robles-Sardin AE, & Valencia ME (2010). Lifestyle intervention in primary care settings improves obesity parameters among Mexican youth. Journal of the American Dietetic Association, 110(2), 285–290. 10.1016/j.jada.2009.10.0422009.10.042 [DOI] [PubMed] [Google Scholar]
- Dickey MD (2005). Engaging by design: How engagement strategies in popular computer and video games can inform instructional design. Educational Technology Research and Development, 53, 67–83. [Google Scholar]
- Edwards EA, Lumsden J, Rivas C, Steed L, Edwards LA, Thiyagarajan A, et al. (2016). Gamification for health promotion: systematic review of behaviour change techniques in smartphone apps. BMJ Open, 6, e012447. 10.1136/bmjopen-2016-012447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinoza J, Chen A, Orozco J, Deavenport-Saman A, & Yin L (2017). Effect of personal activity trackers on weight loss in families enrolled in a comprehensive behavioral family-lifestyle intervention program in the Federally Qualified Health Center setting: a randomized controlled trial. Contemporary clinical trials communications, 7, 86–94. 10.1016/j.conctc.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedele D, Lucero R, Janicke D, Abu-Hasan M, McQuaid E, Moon J, Fidler A, Wallace Farquharson T, & Lindberg D (2019). Protocol for the Development of a Behavioral Family Lifestyle Intervention Supported by Mobile Health to Improve Weight Self-Management in Children With Asthma and Obesity. JMIR Research Protocol, 8(6), e13549. 10.2196/13549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenner AA, Howie EK, Davis MC, & Straker LM (2016). Relationships between psychosocial outcomes in adolescents who are obese and their parents during a multi-disciplinary family-based healthy lifestyle intervention: One-year follow-up of a waitlist controlled trial (Curtin University’s Activity, Food and Attitudes Program). Health and quality of life outcomes, 14(1), 100. 10.1186/s12955-016-0501-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L, & Weihs KL (2000). Can addressing family relationships improve outcomes in chronic disease? Report of the National Working Group on Family-Based Interventions in Chronic Disease. The Journal of Family Practice, 49(6), 561–566. [PubMed] [Google Scholar]
- Frank LB, Murphy ST, Chatterjee JS, Moran MB, & Baezconde-Garbanati L (2015). Telling stories, saving lives: Creating narrative health messages. Health Communication, 30(2), 154–163. 10.1080/10410236.2014.974126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, & Khunti K (2007). Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ, 334(7588), 299. 10.1136/bmj.39063.689375.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliland SS, Azen SP, Perez GE, & Carter JS (2002). Strong in body and spirit: lifestyle intervention for Native American adults with diabetes in New Mexico. Diabetes Care, 25(1), 78–83. 10.2337/diacare.25.1.78 [DOI] [PubMed] [Google Scholar]
- Graziano PA, Garcia A, & Lim CS (2017). Summer Healthy-Lifestyle Intervention Program for Young Children Who Are Overweight: Results from a Nonrandomized Pilot Trial. Journal of Developmental & Behavioral Pediatrics, 38(9), 723–727. 10.1097/dbp.0000000000000499 [DOI] [PubMed] [Google Scholar]
- Green AC, Hayman LL, & Cooley ME (2015). Multiple health behavior change in adults with or at risk for cancer: A systematic review. American Journal of Health Behavior, 39(3), 380–394. 10.5993/AJHB.39.3.11 [DOI] [PubMed] [Google Scholar]
- Gupta L, Khandelwal D, Lal PR, Gupta Y, Kalra S, & Dutta D (2019). Factors determining the success of therapeutic lifestyle interventions in diabetes—Role of partner and family support. European endocrinology, 15, 18–24. 10.17925/ee.2019.15.1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingle MD, Turner T, Going S, Ussery C, Roe DJ, Saboda K, Kutob R, & Stump C (2019). Feasibility of a family-focused YMCA-based diabetes prevention program in youth: The E.P.I.C. Kids (Encourage, Practice, and Inspire Change) Study. Preventive medicine reports, 14, 100840. 10.1016/j.pmedr.2019.100840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu R, Cancela J, Arredondo Waldmeyer MT, Cea G, Vlachopapadopoulou EA, Fotiadis DI, & Fico G (2016). OB CITY—Definition of a family-based intervention for childhood obesity supported by information and communication technologies. IEEE Journal of Translational Engineering in Health and Medicine, 4, 2200114. 10.1109/JTEHM.2016.2526739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höchsmann C, Müller O, Ambühl M, Klenk C, Königstein K, Infanger D, et al. (2019). Novel smartphone game improves physical activity behavior in type 2 diabetes. American Journal of Preventive Medicine, 57, 41–50. 10.1016/j.amepre.2019.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingoldsby EM (2010). Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies, 19, 629–645. 10.1007/s10826-009-9350-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Health and Behavior: Research, P., and Policy. Health and behavior: The interplay of biological, behavioral, and societal influences. Washington (DC): National Academies Press (US); 2001. 5, Individuals and Families: Models and Interventions https://www.ncbi.nlm.nih.gov/books/NBK43749/ [PubMed] [Google Scholar]
- Kerr ME (1981). Family systems theory and therapy. Handbook of family therapy, 1, 226–264. [Google Scholar]
- King HA, Jeffreys AS, McVay MA, Coffman CJ, & Voils CI (2014). Spouse health behavior outcomes from a randomized controlled trial of a spouse-assisted lifestyle change intervention to improve patient low-density lipoprotein cholesterol. Journal of behavioral medicine, 37(6), 1102–1107. 10.1007/s10865-014-9559-4 [DOI] [PubMed] [Google Scholar]
- Ling J, Robbins LB, Zhang N, Kerver JM, Lyons H, Wieber N, & Zhang M (2018). Using Facebook in a Healthy Lifestyle Intervention: Feasibility and Preliminary Efficacy. Western journal of nursing research, 40(12), 1818–1842. 10.1177/0193945918756870 [DOI] [PubMed] [Google Scholar]
- Martin LJ, Burke SM, Shapiro S, Carron AV, Irwin JD, Petrella R, Prapavessis H, & Shoemaker K (2009). The use of group dynamics strategies to enhance cohesion in a lifestyle intervention program for obese children. BMC Public Health, 9, 277. 10.1186/1471-2458-9-277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: The kappa statistic. Biochemical Medicine (Zagreb), 22, 276–282. [PMC free article] [PubMed] [Google Scholar]
- Miller AS, Cafazzo JA, & Seto E (2016). A game plan: Gamification design principles in mHealth applications for chronic disease management. Health Informatics Journal, 22, 184–193. 10.1177/1460458214537511 [DOI] [PubMed] [Google Scholar]
- Miller TA, & Dimatteo MR (2013). Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metabolic Syndrome and Obesity, 6, 421–426. 10.2147/DMSO.S36368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8, 336–341. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Monden CW, de Graaf ND, & Kraaykamp G (2003). How important are parents and partners for smoking cessation in adulthood? An event history analysis. Prev Med, 36, 197–203. [DOI] [PubMed] [Google Scholar]
- Orji R, & Moffatt K (2016). Persuasive technology for health and wellness: State-of-the-art and emerging trends. Health Informatics Journal 10.1177/1460458216650979 [DOI] [PubMed] [Google Scholar]
- Patrick H, & Williams GC (2012). Self-determination theory: its application to health behavior and complementarity with motivational interviewing. The International Journal of Behavioral Nutrition and Physical Activity, 9, 18. 10.1186/1479-5868-9-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Po’e EK, Heerman WJ, Mistry RS, & Barkin SL (2013). Growing Right Onto Wellness (GROW): a family-centered, community-based obesity prevention randomized controlled trial for preschool child-parent pairs. Contemporary clinical trials, 36(2), 436–449. 10.1016/j.cct.2013.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevention, C. f. D. C. a. (2019). National Center for Chronic Disease Prevention and Health Promotion https://www.cdc.gov/chronicdisease/index.htm
- Rigby S, & Ryan RM (2011). Glued to games: How video games draw us in and hold us spellbound: How video games draw us in and hold us spellbound AbC-CLIo. [Google Scholar]
- Ryan RM, Rigby CS, & Przybylski A (2006). The motivational pull of video games: A self-determination theory approach. Motivation and emotion, 30, 344–360. [Google Scholar]
- Sailer M, Hense JU, Mayr SK, & Mandl H (2017). How gamification motivates: An experimental study of the effects of specific game design elements on psychological need satisfaction. Computers in Human Behavior, 69, 371–380. 10.1016/j.chb.2016.12.033 [DOI] [Google Scholar]
- Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, O’Malley G, Serrecchia JB, Tamborlane WV, & Caprio S (2011). Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics, 127(3), 402–410. 10.1542/peds.2010-0697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlechty PC (2011). Engaging students: The next level of working on the work John Wiley & Sons. [Google Scholar]
- Smith LR, Chadwick P, Radley D, Kolotourou M, Gammon CS, Rosborough J, & Sacher PM (2013). Assessing the short-term outcomes of a community-based intervention for overweight and obese children: The MEND 5–7 programme. BMJ Open, 3(5). 10.1136/bmjopen-2013-002607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sola D, Couturier J, & Voyer B (2015). Unlocking patient activation in chronic disease care. British Journal of Healthcare Management, 21, 220–225. [Google Scholar]
- Sumamo E, Ha C, Korownyk C, Vandermeer B, & Dryden DM (2011). Lifestyle interventions for four conditions: Type 2 diabetes, metabolic syndrome, breast cancer, and prostate cancer In. 10.1002/NBK254022 [DOI] [PubMed] [Google Scholar]
- Touyz LM, Cohen J, Cohn RJ, Garnett SP, Anazodo A, Gohil P, Grech AM, Ng A, & Wakefield CE (2019). Childhood cancer survivors report preferring lifestyle interventions delivered in person rather than online: An adolescent and parent perspective. Pediatr Blood Cancer, e27922. 10.1002/pbc.27922 [DOI] [PubMed] [Google Scholar]
- Vansteenkiste M, Niemiec CP, & Soenens B (2010). The development of the five mini-theories of self-determination theory: An historical overview, emerging trends, and future directions. In The decade ahead: Theoretical perspectives on motivation and achievement Emerald Group Publishing Limited. [Google Scholar]
- Viitasalo A, Eloranta AM, Lintu N, Vaisto J, Venalainen T, Kiiskinen S, Karjalainen P, Peltola J, Lampinen EK, Haapala EA, Paananen J, Schwab U, Lindi V, & Lakka TA (2016). The effects of a 2-year individualized and family-based lifestyle intervention on physical activity, sedentary behavior and diet in children. Preventive medicine, 87, 81–88. 10.1016/j.ypmed.2016.02.027 [DOI] [PubMed] [Google Scholar]
- Waling M, Backlund C, Lind T, & Larsson C (2012). Effects on metabolic health after a 1-year-lifestyle intervention in overweight and obese children: a randomized controlled trial. Journal of nutrition and metabolism, 2012, 913965. 10.1155/2012/913965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werbach K (2014). (Re) defining gamification: A process approach. International conference on persuasive technology, [Google Scholar]
- Werbach K, & Hunter D (2012). For the win: How game thinking can revolutionize your business Wharton Digital Press. [Google Scholar]
- Williamson PO, & Minter CIJ (2019). Exploring PubMed as a reliable resource for scholarly communications services. Journal of the Medical Library Association, 107, 16–29. 10.5195/jmla.2019.433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodruff SI, Talavera GA, & Elder JP (2002). Evaluation of a culturally appropriate smoking cessation intervention for Latinos. Tobacco Control, 11, 361–367. 10.1136/tc.11.4.361 [DOI] [PMC free article] [PubMed] [Google Scholar]


