Abstract
Background and Purpose:
Walking activity in persons with Parkinson disease (PD) is important for preventing functional decline. The contribution of walking activity to home and community mobility in PD is poorly understood.
Methods:
Cross-sectional baseline data (n=69) were analyzed from a randomized controlled PD trial. The Life-Space Assessment (LSA) quantified the extent, frequency, and independence across five expanding levels of home and community mobility, producing individual subscores and a total score. Two additional summed scores were used to represent mobility within (Levels 1-3) and beyond (Levels 4-5) neighborhood limits. An accelerometer measured walking activity for seven days. Regression and correlation analyses evaluated relationships between daily steps and mobility scores. Mann-Whitney U tests secondarily compared differences in mobility scores between active and sedentary groups.
Results:
Walking activity contributed significantly to the summed Level 1-3 score (β=.001, p=.004) but not to the summed Level 4-5 (β=.001, p=.33) or total (β=.002, p=.07) scores. Walking activity was significantly related to Level 1 (ρ=.336, p=.005), Level 2 (ρ=.307, p=.010), and Level 3 (ρ=.314, p=.009) subscores. Only the summed Level 1-3 score (p=.030) was significantly different between active and sedentary groups.
Discussion and Conclusions:
Persons with PD who demonstrated greater mobility beyond the neighborhood were not necessarily more active; walking activity contributed moreso to home and neighborhood mobility. Compared to LSA total score, the Level 1-3 summed score may be a more useful participation-level measure for assessing the impact of changes in walking activity.
Video Abstract available:
for more insight from the authors (see Supplemental Digital Content 1)
Keywords: Parkinson disease, life-space, walking activity
Introduction
Walking is an important contributor to participation in community life.1,2 Declining walking activity in persons with Parkinson disease (PD) can precede limitations in other gait-dependent activities (e.g. housework, yard work, dressing, traveling) and has been associated with increasing disability.3,4 Interventions targeting walking, therefore, may have the greatest impact on slowing the progression of disability.3,5,6 Recently, interventions that promote a daily habit of sustained walking activity have been proposed as a means of slowing disability by preserving walking capacity.7 How such interventions might influence home and community mobility, defined as moving from one place to another on foot or by other forms of transportation,1 has yet to be studied. More fundamentally, the extent to which persons with PD might rely on walking for mobility in home and community environments is not well understood.
Physical therapists routinely seek to assess walking function in persons with PD across multiple domains of human functioning. Whereas locomotor physiologic systems, gait speed, and walking capacity are relatively easy to measure directly, the assessment of natural, “free-living” walking activity beyond the clinical spotlight (i.e., at home and in the community) often relies on patient self-report. Affirmative answers to questions directed at community mobility (e.g., Do you do your own grocery shopping? Do you work or volunteer outside the home?) may be interpreted as suggesting that a patient is relatively active; however, this assumption has not been formally tested.
Life-space mobility is a participation-level construct representing the extent to which a person moves, either actively (e.g., walking) or passively (e.g., motorized transportation), through their environment.8,9 Life-space has been defined conceptually using a series of progressively expanding environments, or “levels,” representing rooms in the home, areas immediately outside the home (e.g., yard or driveway), the neighborhood, the town, and beyond town (Fig 1).8,9 For older adults, mobility excursions into more widely ranging life-spaces (i.e., greater total life-space) have been associated with engagement in meaningful activities, community participation, and overall health.10-18 Restrictions in life-space, in contrast, have been linked to limitations in physical functioning, frailty, depression, increased falls, and mortality.17-20 The older adult literature also has suggested that individuals with greater total life-space mobility may be more physically active, that life-space mobility commonly requires at least some walking (e.g., walking from the house to the car; walking in a store), and that delineating the walking component of life-space mobility may be important for understanding participation in meaningful activities.16,17,21
Figure 1.
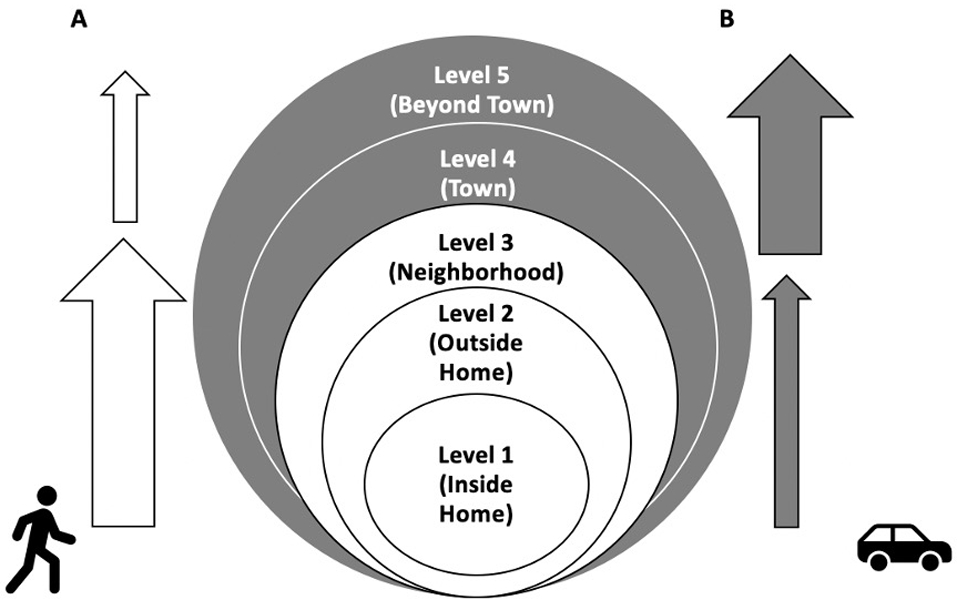
Model representing individual LSA levels within neighborhood limits (white) and beyond neighborhood limits (gray). The model portrays walking activity as more prevalent in LSA levels 1-3 (A) and passive mobility as more prevalent in LSA levels 4-5 (B).
Given its associations with older adult health, disability, and walking activity, life-space mobility provides a useful context in which physical therapists might better understand the daily walking of persons with PD. Unlike older adults in general, however, persons with PD appear to be particularly vulnerable to declines in walking activity.22,23 Does this vulnerability attenuate the mobility-activity relationship in persons with PD (i.e., are persons with PD who are mobile in the community necessarily more active)? Are there particular walking environments in which persons with PD tend to accumulate relatively greater amounts of walking activity, toward which walking promotion interventions for sedentary persons might be directed? Unfortunately, the relationship between life-space mobility and daily walking activity in PD has not been investigated. Prior studies investigating life-space in PD were limited to the reliability and validity of life-space mobility measures24-26 and on factors that may influence life-space mobility (e.g., motor impairments, perceived walking difficulty, depression, pain).27,28
The primary aims of this study were (1) to determine the extent to which walking activity might contribute to total life-space mobility as well as mobility occurring within and beyond neighborhood limits in persons with PD, and (2) to examine the relationship between walking activity and mobility at each life-space level. Based on the prevalence of reduced walking function in persons with PD,22,23 we hypothesized that the relationship between walking activity and life-space mobility would weaken in life-spaces relatively further from home where passive means of mobility (e.g., motorized transportation) could be used to compensate (Fig 1).16,17,21 Our secondary aim was to explore how life-space mobility might differ in sedentary persons with PD compared to their more active counterparts.29 Similar to findings in older adults,16,17 we hypothesized that sedentary persons with PD would be less mobile than active persons.
Methods
Study Design and Participants
This was a cross-sectional, secondary analysis of baseline life-space and walking activity data from a prospective, 12-month, single-blind, multi-site, randomized controlled trial examining the impact of mobile health technology on the daily walking behavior of individuals with PD.7 Participants in the parent study were adults with mild to moderate idiopathic PD30 who were able to safely participate in a progressive walking and strengthening exercise program. The parent study was approved by the Institutional Review Board at Boston University. Data used in the secondary analysis were collected between February 2019 and February 2020, prior to the coronavirus pandemic. The sample was comprised of those participants with complete baseline data for all pertinent variables.
Measures
Daily Walking Activity
The StepWatch 4 Activity Monitor (SAM; Orthocare Innovations, Mountlake Terrace, Washington) is an unobtrusive, microprocessor-linked device that was used to capture walking activity in participants’ real-world environments. The SAM is a self-contained, maintenance-free device that combines acceleration, position and timing information to count complete gait cycles (strides) of the user; it is the size of a pager, weighs 38g, and was attached with self-adhesive straps above the lateral malleolus of participants’ less impaired lower extremity. Participants were instructed to wear the SAM for seven consecutive days during all waking hours, except when showering/bathing or swimming. They were encouraged to engage in their usual daily activities and to record on a daily log sheet any periods during which the SAM was removed.
Using the manufacturer’s software, a SAM was calibrated to each participant’s gait pattern based on height, typical walking speed, and leg motion. Calibration accuracy was verified by research personnel who compared visual observation of participant steps taken over a short distance with the SAM-generated step count. Monitors were configured to store stride counts in one-minute intervals. A stride count of zero was recorded for minutes in which no steps were taken. Collected data were downloaded to a computerized tablet, with which manufacturer’s software was used to convert stride counts to step counts and calculate daily step count values. Mean daily steps were used to represent walking activity in subsequent analyses. The validity and reliability of the SAM for capturing stride counts has been demonstrated in persons with various neurological disorders including PD.31-37
Life-Space Mobility
The Life-Space Assessment (LSA) is a self-administered tool whereby participants report the frequency and independence of mobility excursions beyond their bedroom during the previous four weeks.8,9 The LSA identifies five life-spaces, represented by increasingly wide-ranging geographic regions (Level 1 = rooms inside the home beyond the bedroom, Level 2 = immediately outside the home (e.g., yard, driveway), Level 3 = neighborhood, Level 4 = town, Level 5 = beyond town). Excursions were scored separately at each life space level by multiplying the level number (1-5) by the frequency of excursions occurring therein (1 = < 1/week; 2 = 1-3 times/week; 3 = 4-6 times/week; 4 = daily) and by the amount of assistance required (1 = personal assistance; 1.5 = equipment only; 2 = independent).8,9 A total life-space score was calculated as the sum of individual level sub-scores. Total scores range from 0-120, with ‘0’ indicating total immobility (i.e., confined to bedroom) and ‘120’ indicating independent, daily mobility beyond town.8,9 The LSA total score has demonstrated construct validity and responsiveness in community-dwelling older adults.38 We also calculated a Level 1-3 summed score and a Level 4-5 summed score to distinguish between mobility occurring within and beyond neighborhood limits, (i.e., home and neighborhood vs town and beyond town) (Fig 1).
Statistical Analysis
Descriptive statistics were used to characterize the sample. For the primary aim, univariate linear regression analyses were conducted to determine the contribution of mean daily steps to LSA total score and the summed Level 1-3 (excursions within neighborhood limits) and Level 4-5 (excursions beyond neighborhood limits) scores. Spearman’s rank-order correlation analyses (ρ) were used to examine the relationship between mean daily steps and the mobility subscore at individual LSA levels (1-5). For the exploratory secondary aim, participants were classified into either sedentary (< 5,000 steps/day) or active (≥ 5,000 steps/day) groups.29 Because life-space subscores at each level were not normally distributed and within group variances per Levene’s test were unequal, we employed a series of Mann-Whitney U tests for between-group comparisons of LSA total score, summed Level 1-3 score, summed Level 4-5 score, and individual Level 1-5 subscores. Study data were stored in a Research Electronic Data Capture (REDCap) database.39-41 Statistical analyses were performed using SPSS statistical software program version 26.0 (IBM Corp, Armonk New York) with differences considered to be statistically significant at p<.05.
Results
The total sample (n= 69) included mostly older persons (58% male; mean age = 67.5 (8.7) years) with mild to moderate PD (H&Y 2 (n=27); H&Y 2.5 (n=30); H&Y 3 (n=12)) who were retired or not working (75.4%). In our sample, most participants (n=62, 90%) wore the SAM for 7 days; however, some participants completed fewer days (six days, n=5; five days, n=1; four days, n=1). The sample as a whole was somewhat active (mean daily walking activity = 7607.2 (3625.8) steps/day) and reported mobility excursions at home and in the community (median (IQR) total life-space score = 92 (42.25)).
Relationship Between Walking Activity and Life-Space Mobility
In the univariate linear regression analysis (Table 1), daily walking activity was a significant contributor to mobility within neighborhood limits (summed LSA Level 1-3 score, β=0.001, p=.004), but not beyond the neighborhood (summed LSA Level 4-5 score, β=0.001, p=.33) or to overall mobility (LSA total score (β=0.002, p=.07). Daily walking activity accounted for approximately 12% of the variability in the summed LSA Level 1-3 score, while only explaining approximately 1% of the variability in the summed LSA Level 4-5 score and 5% of the variability in LSA total score. Daily walking activity was significantly related to individual level LSA subscores representing mobility within neighborhood limits (Level 1 (inside home); Level 2 (outside home); Level 3 (neighborhood)), but not mobility beyond neighborhood limits (Level 4 (town); Level 5 (beyond town)) (Table 2).
Table 1.
Contribution of Daily Steps to Life-space Scores (n=69)
| Variable | Life-Space Total Score | Level 1-3 | Level 4-5 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | R2 | p | 95% CI | β | R2 | p | 95% CI | β | R2 | p | 95% CI | |
| Steps/day | .002 | .05 | .07 | (.000, .003) | .001 | .12 | .004* | (.000, .002) | .001 | .01 | .33 | (−.001, .002) |
Univariate regression of daily steps on Life-space Total Score; Level 1-3 summed score (excursions within neighborhood limits); and Level 4-5 summed score (excursions beyond neighborhood limits)
Score p<.01
Table 2.
Correlations of Life-Space Level Scores with Daily Steps (n=69)
| Variable | Correlation coefficient | p-value |
|---|---|---|
| Level 1 score | .336 | .005** |
| Level 2 score | .307 | .010* |
| Level 3 score | .314 | .009** |
| Level 4 score | .075 | .541 |
| Level 5 score | .193 | .113 |
Correlations are Spearman’s rho
p<.05
p<.01
Comparison of Life-Space Mobility Between Sedentary and Active Participants
Sedentary and active groups had similar total life-space mobility (LSA total scores; p=.129) and mobility beyond the neighborhood limits (LSA 4-5 summed score; p=.259; Table 3). Sedentary and active groups also were similarly mobile at individual life-space levels immediately outside the home (Level 2), in town (Level 4), and beyond the town (Level 5; Fig 2). In contrast, the sedentary group was significantly less mobile than the active group within the neighborhood limits (LSA Level 1-3 summed score; p=.030; Table 3), with the difference primarily accounted for by significantly lower mobility scores in the home (Level 1, p=.023) and in the neighborhood (Level 3, p=.023) (Fig 2). Indeed, less than half of participants in the sedentary group attained the maximum life-space level score for mobility excursions into the neighborhood (Level 3=31.3%) compared to over half of the participants in the active group (Level 3=58.5%; Fig 2).
Table 3.
Life-Space Scores Organized by Sedentary and Active Groups
| Variable | All (n=69) |
Sedentary (n=16) |
Active (n=53) |
p-value |
|---|---|---|---|---|
| LSA Summed 1-3 Scoreb (max = 48) | 48 (12) | 39 (27) | 48 (11) | .030* |
| LSA Summed 4-5 Scorec (max = 72) | 52 (32) | 44 (26) | 52 (36) | .259 |
| LSA Total Score (max = 120) | 92 (42.25) | 85 (59.38) | 100 (43) | .129 |
LSA Life-space Assessment
Calculated as the sum of LSA Level 1-3 scores
Calculated as the sum of LSA Level 4-5 scores
Note: Data are reported as median (IQR). Mann-Whitney U test used to determine differences between groups
p<.05
Figure 2.
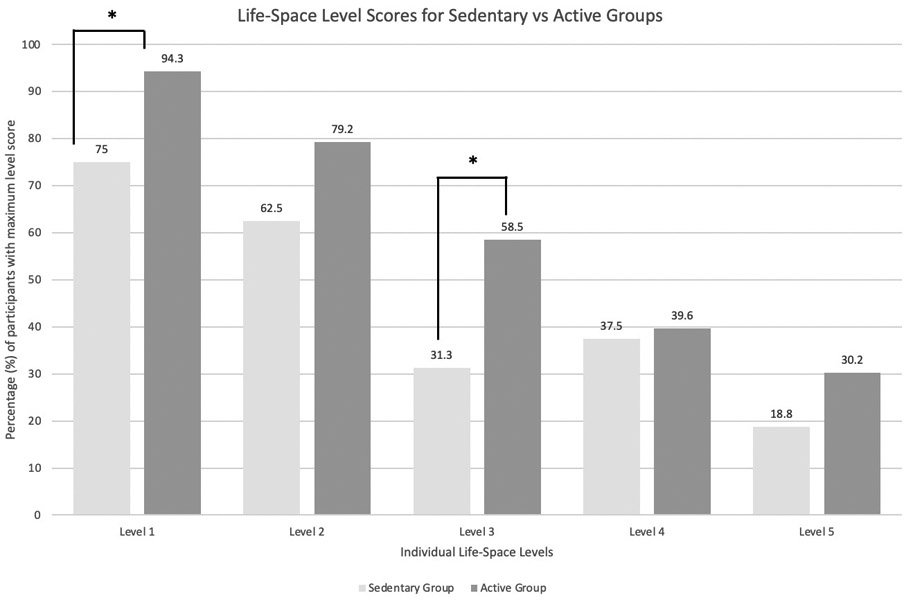
Between-group differences in individual level scores (LSA Levels 1-5) based on walking activity (sedentary vs active). The x-axis depicts the five individual life-space levels as follows: Level 1 = inside the home; Level 2 = immediately outside the home (e.g., yard, driveway); Level 3 = neighborhood; Level 4 = town; Level 5 = beyond town. The y-axis depicts the percentage of participants that scored the maximum score for each individual life-space level. *p<.05. The between-group difference in mobility is most pronounced in the neighborhood environment (Level 3).
Discussion
This cross-sectional study determined the extent to which a sample of persons with mild to moderate PD might rely on walking for mobility in home and community environments. Our results revealed that daily walking activity in persons with PD was not significantly associated with total life-space mobility (Table 1). Daily walking activity was also not associated with combined mobility beyond the neighborhood (Level 4-5 summed score; Table 1). However, as hypothesized (Fig 1), walking activity significantly contributed to combined mobility (Level 1-3 summed score) occurring within neighborhood limits (Table 1). Additionally, walking activity was significantly related to mobility at each of the three individual life-space levels (i.e., inside the home, immediately outside the home, and in the neighborhood) that comprised the Level 1-3 summed score (Table 2). Our findings suggested that unlike older adults in general, more mobile persons with PD are not necessarily more active (i.e., amount of daily walking activity may not necessarily indicate distance traveled from home). Furthermore, the walking activity of persons with PD may be most likely to occur in the home and neighborhood. These results also supported the idea that beyond the neighborhood limits, persons with PD might utilize passive means of mobility (e.g., motorized transportation) more often than older adults in general.16,17,21
Sedentary behavior may perpetuate functional decline in persons with PD.4-6 As hypothesized, sedentary participants generally were less mobile than their active counterparts (Table 3, Fig 2), but the between-group difference was significant only within neighborhood limits. At an even more granular level, the between-group difference was apparent primarily for mobility within the home (Level 1) and in the neighborhood (Level 3) (Fig 2). Otherwise, the groups were similarly mobile. These results were consistent with literature suggesting that older adults who are more sedentary may be less likely to walk outside of the home.16,17,21
Importantly, there appeared to be a disproportionately greater reduction in the neighborhood (Level 3) mobility scores of the sedentary group (Fig 2). Given that walking activity across the full sample contributed significantly to life-space mobility within the neighborhood limits, we speculated that the reduced neighborhood mobility of the sedentary group might have reflected lack of participation in a dedicated walking program (assuming that participants’ neighborhoods provided them with a safe walking environment). This proposition warrants further investigation. Nonetheless, physical therapists should consider the neighborhood environment as a potentially more likely target than more distant environments for walking activity interventions designed to delay gait-related disability and functional decline.
The study results also are important for physical therapists to consider when evaluating the walking activity of persons with PD in relation to their mobility. Based on our findings, persons with PD who report being mobile in the community, especially beyond the neighborhood limits, may not necessarily be physically active. Similarly, active persons with PD may not necessarily travel greater distances from home as compared to their sedentary counterparts. Therefore, the LSA Level 1-3 summed score, rather than the total score, may be a more useful participation-level measure to assess the impact of changes in walking activity in PD.
Our study is not without limitations. First, its relatively narrow scope and cross-sectional design did not allow for inferences of causality. We also acknowledge that although there was a stronger relationship between life-space mobility and walking activity within the neighborhood limits, walking activity explained only 12% of the variance in the summed Level 1-3 life-space score. Prior work in older adults has suggested that cognitive factors (e.g., mental status, memory), psychosocial factors (e.g., self-efficacy, fear of falling), physical factors (e.g., age-related impairments, walking speed), and environmental factors (e.g., social support, poor driving conditions) may influence life-space mobility.42,43 In PD, severity of motor and balance impairments, psychological factors (e.g., perceived walking difficulty), non-motor symptoms (e.g., depression, apathy) and pain27,28 also may have contributed. Longitudinal studies would help gain a deeper understanding of how the relationship between walking activity and life-space mobility might change over time or in response to an intervention. Second, the LSA was a self-report measure asking about excursions over the past four weeks, and therefore, may have been subject to recall bias. Furthermore, unlike GPS technology which precisely and continuously quantifies community location and distance traveled, the self-report LSA summarized mobility excursions on an ordinal scale of relative distance in any direction from a central (bedroom) location. As a result, the relatively coarse LSA instrument provided only an approximation of mobility excursions. Indeed, we could not account for variation in home location; rural and urban settings may have differently influenced the extent, frequency, and means of mobility excursions. Third, although the construct validity of the LSA had been established in community dwelling older adults,38 and the vast majority of study participants met that description, the LSA had not been validated specifically in persons with PD. Finally, our study sample was limited to individuals with mild to moderate disease severity (Modified H&Y 2-3) and included individuals who were fairly active (Mean daily walking activity =7607.2 steps/day); study findings may not be generalizable to those with greater disease severity or who are more sedentary.
Conclusions
Mobile persons with mild to moderate PD are not necessarily more active. The walking activity of individuals with PD may be relatively more important for mobility excursions occurring within neighborhood limits rather than more distant excursions. Life-space mobility scores for areas closer to home might be a useful participation-level measure for assessing the impact of changes in walking activity in PD. Interventions designed to increase walking activity may be more likely to enhance participation in home and neighborhood gait-related activities. Future research should consider how the relationship of walking activity and life-space mobility might change over time, either as a result of functional decline or as a positive response to intervention.
Supplementary Material
Zajac_SDC1.mov.mp4
Conflicts of Interest and Source of Funding:
The authors declare no conflict of interest. This study was funded by the National Institute of Health (NIH) and National Institute of Child Health and Human Development (NICHD), #1R01HD092444-01A1; K23 HD100569 (PI: Duncan). The clinical trials registry number is NCT03517371.
Footnotes
An abstract version of this work was published at APTA CSM Virtual Conference, February 1st-28th, 2021.
References
- 1.Skantz H, Rantanen T, Palmberg L, Rantalainen T, Aartolahti E, Portegijs E et al. Outdoor mobility and use of adaptive or maladaptive walking modifications among older people. The Gerontological Society of America 2020;75(4):806–812. [DOI] [PubMed] [Google Scholar]
- 2.Rantanen T Promoting mobility in older people. Journal of Preventative Medicine & Public Health 2013;46:S50–S54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ellis TD, Cavanaugh JT, Earhart GM, Ford MP, Foreman KB, Thackeray A, Thiese MS, Dibble LE. Identifying clinical measures that most accurately reflect the progression of disability in Parkinson disease. Parkinsonism Relat Disord 2016;25:65–71. [DOI] [PubMed] [Google Scholar]
- 4.Shulman LM, Gruber-Baldini AL, Anderson KE, Vaughan CG, Reich SG, Fishman PS et al. The evolution of disability in Parkinson disease. Movement Disorders. 2008;23(6):790–796. [DOI] [PubMed] [Google Scholar]
- 5.Shulman LM. Understanding disability in Parkinson’s disease. Movement Disorders. 2010;25(1):131–135. [DOI] [PubMed] [Google Scholar]
- 6.Lord S, Godfrey A, Galna B, Mhiripiri D, Burn D, Rochester L. Ambulatory activity in incident Parkinson’s: more than meets the eye? J Neurol. 2013;260:2964–2972. [DOI] [PubMed] [Google Scholar]
- 7.Rawson KS, Cavanaugh JT, Colon-Semenza C, DeAngelis T, Duncan R, Fulford D, LaValley M, Mazzoni P, Nordahl T, Quintiliani L, Marie Saint-Hilaire, Thomas CA, Earhart GM, Ellis TD. Design of the WHIP-PD study: a phase II, twelve-month, dual-site, randomized controlled trial evaluating the effects of a cognitive-behavioral approach for promoting enhanced walking activity using mobile health technology in people with Parkinson-disease. BMC Neurology April 2020;20:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. American Geriatrics Society. 2003;51:1610–1614. [DOI] [PubMed] [Google Scholar]
- 9.Peel C, Baker PS, Roth DL, Brown CJ, Bodner EV, Allman RM. Assessing mobility in older adults: The UAB study of aging life-space assessment. Physical Therapy. 2005;85(10):1008–1119. [PubMed] [Google Scholar]
- 10.Murata C, Kondo T, Tamakoshi K, Yatsuya H, Toyoshima H. Factors associated with life space among community-living rural elders in Japan. Public Health Nurs 2006;23:324–331. [DOI] [PubMed] [Google Scholar]
- 11.Barnes LL, Wilson RS, Bienias JL, de Leon CF, Kim HJ et al. Correlates of life space in a volunteer cohort of older adults. Exp Aging Res 2007;33(1):77–93. [DOI] [PubMed] [Google Scholar]
- 12.Sawyer P, Allman RM. Resilience in mobility in the context of chronic disease and aging: In: Fry PS, Keyes CLM, eds. New Frontiers in Resilient Aging: Life-Strengths and Well-Being in Late Life. Cambridge: Cambridge University Press;2010:310–339. [Google Scholar]
- 13.Satariano WA, Guralnik JM, Jackson RJ, Marottoli RA, Phelan EA, Prohaska TR. Mobility and aging: new directions for public health action. Am J Public Health 2012;102(8):1508–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosso AL, Taylor JA, Tabb LP, Michael YL. Mobility, disability, and social engagement in older adults. Journal of Aging and Health 2013;25(4):617–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rantakokko M, Mänty M, Rantanen T. Mobility decline in old age. Exerc Sport Sci Rev 2013;41:19–25. [DOI] [PubMed] [Google Scholar]
- 16.Tsai LT, Portegijs E, Rantakokko M, Viljanen A, Saajanaho M, Eronen J, et al. The association between objectively measured physical activity and life-space mobility among older people. Scand J Med Sci Sports. 2015;25:368–373. [DOI] [PubMed] [Google Scholar]
- 17.Tsai LT, Rantakokko M, Rantanen T, Viljanen A, Kauppinen M, Portegijs E. Objectively measured physical activity and changes in life-space mobility among older people. Journals of Gerontology: Medical Sciences. 2016;71(11):1466–1471. [DOI] [PubMed] [Google Scholar]
- 18.Rantakokko M, Portegijs E, Viljanen A, Iwarsson S, Kauppinen M, Rantanen T. Changes in life-space mobility and quality of life among community-dwelling older people: a 2-year follow-up study. Qual Life Res 2016;25:1189–97. [DOI] [PubMed] [Google Scholar]
- 19.Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, Allman RM. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. J Gerontol A Biol Sci Med Sci 2008;63(11):1241–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bentley JP, Brown CJ, McGwin G Jr, Sawyer P, Allman RM, Roth DL. Functional status, life-space mobility, and quality of life: a longitudinal mediation analysis. Qual Life Res 2013;22(7):1621–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Portegijs E, Tsai L-T, Rantanen T, Rantakokko M. Moving through Life-space areas and objectively measured physical activity of older people. Jepson R, ed. PLoS ONE. 2015;10(8):e0135308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cavanaugh JT, Ellis TD, Earhart GM, Ford MP, Foreman KB, Dibble LE. Capturing ambulatory activity decline in Parkinson’s disease. J Neurol Phys Ther 2012;36(2):51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cavanaugh JT, Ellis TD, Earhart GM, Ford MP, Foreman KB, Dibble LE. Toward understanding ambulatory decline in Parkinson disease. Phys Ther 2015;95(8):1142–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liddle J, Ireland D, McBride SJ, et al. Measuring the lifespace of people with Parkinson’s disease using smartphones: proof of principle. JMIR Mhealth Uhealth. 2014;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ireland D, McBride S, Liddle J, Chenery H. Towards quantifying the impact of Parkinson’s disease using GPS and lifespace assessment. In: UQ centre for clinical research. 2013 Presented at: 6th International Conference on Biomedical Engineering and Informatics (BMEI 2013); December 16-18, 2013; Hangzhou, China p. 564–569. [Google Scholar]
- 26.Zhu L, Duval C, Boissy P, Montero-Odasso M, Zou G, Jog M et al. Comparing GPS-based community mobility measures with self-report assessments in older adults with Parkinson’s disease. The Gerontological Society of America 2020; doi: 10.1093/Gerona/glaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lamont RM, Morris ME, Woollacott MH, Brauer SG. Community walking in people with Parkinson’s disease. Parkinson’s Disease. 2012:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rantakokko M, Iwarsson S, Slaug B, Nilsson MH. Life-space mobility in Parkinson’s disease: Associations with motor and non-motor symptoms. Journals of Gerontology: Medical Sciences. 2019;74(4):507–512. [DOI] [PubMed] [Google Scholar]
- 29.Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting “how many steps are enough?” Med Sci Sports Exerc 2008;40(7)(Suppl):S537–543. [DOI] [PubMed] [Google Scholar]
- 30.Gibbs WR, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 1988;51:745–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shepherd E, Toloza E, McClung C, Schmalzried T. Step activity monitor: increased accuracy in quantifying ambulatory activity. Journal of Orthopaedic Research 1999;17:703–8. [DOI] [PubMed] [Google Scholar]
- 32.Coleman K, Smith D, Boone C, Joseph A, Aguila M. Step activity monitor: long-term continuous recording of ambulatory function. Journal of Rehabilitation Research and Development 1999;36(1):8–18. [PubMed] [Google Scholar]
- 33.Macko R, Haeuber E, Shaughnessy M et al. Microprocessor-based ambulatory activity monitoring in stroke patients. Medicine and Science in Sports and Exercise 2002;34(3):394–99. [DOI] [PubMed] [Google Scholar]
- 34.Salarian A, Russmann H, Vingerhoets FJ et al. Gait assessment in Parkinson’s disease: toward an ambulatory system for long-term monitoring. IEEE Trans Biomed Eng 2004;51(8):1434–43. [DOI] [PubMed] [Google Scholar]
- 35.Gaines J, Coleman KL, Beck J, Shao YL. The effectiveness of the stepwatch activity monitor. The Gerontologist 2005;45(Special Issue II):524. [Google Scholar]
- 36.Manns PJ, Baldwin E. Ambulatory activity of stroke survivors: measurement options for dose, intensity, and variability of activity. Stroke 2009;40(3):864–67. [DOI] [PubMed] [Google Scholar]
- 37.Speelman AD, van Nimwegen M, Borm GF, Bloem BR, Munneke M. Monitoring of walking in Parkinson’s disease: a validation of an ambulatory activity monitor. Parkinsoniam Relat Disord 2011;17(5):402–04. [DOI] [PubMed] [Google Scholar]
- 38.McCrone A, Smith A, Hooper J, Parker RA, Peters A. The life-space assessment measure of functional mobility has utility in community-based physical therapist practice in the United Kingdom. Phys Ther 2019;99(12): 1719–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wright A Redcap: a tool for the electronic capture of research data. Journal of Electronic Resources in Medical Libraries. 2016;13:197–201. [Google Scholar]
- 41.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. The Gerontologist 2010;50(4):443–450. [DOI] [PubMed] [Google Scholar]
- 43.Kuspinar A, Verschoor CP, Beauchamp MK, Dushoff J, Ma J, Amster E. Modifiable factors related to life-space mobility in community-dwelling older adults: results from the Canadian longitudinal study on aging. BMC Geriatrics 2020;20(35): 10.1186/s12877-020-1431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Zajac_SDC1.mov.mp4


