Abstract
To study the prevalence of severe social anxiety (SSA) among a group of adolescents during the coronavirus disease of 2019 (COVID-19) pandemic. A total of 178 adolescents attending the private clinics of the authors were screened online for the presence of SSA, by using the self-reporting format of the Liebowitz Social Anxiety Scale for children and adolescents (LSAS-CA). SSA defined as LSAS-CA scores of 80 or more was checked for statistical association with the adolescents’ sociodemographic data and knowledge about the COVID-19 infection. The 18% of our participants had SSA, no correlation was found between having SSA and ä acknowledging or fearing the COVID-19 morbidity. Factors associated with SSA included texting, using social media, and playing video games during the lockdown. Mitigating factors include high family socioeconomic status, history of socialization with friends, and the use of WhatsApp as a source of information about COVID-19 infection.
Keywords: social anxiety, COVID-19 pandemic, adolescents, medical education, social media, patient education
Introduction
Adolescence is a dynamic period of development which sets physical, mental, and economic foundations for adulthood. It is a period of heightened stress that features complex neurological changes in social interactions, emotions, and risk processing influenced by peer and social pressures with unexpected outcomes.1–3 Up to 20% of adolescents experience mental health disorders during this period, 75% of which appear before the age of 18 years.4,5 Social interactions in the right environment and psychological assistance are crucial for the development of healthy physical, social, and mental skills during this sensitive period.1
The coronavirus disease of 2019 (COVID-19) pandemic, with its social restrictions such as staying at home, practicing social distancing, and engaging in distance learning, creates an environment that inhibits the adolescents’ social interactions and communications with teachers, peers, and other segments of the society. In addition, adolescents fear of infection and of the in appropriate implementation of COVID-19 protective measures with infected acquaintances may increase their worries about infecting family members and friends. These new experiences are associated with uncertainty and anxiety for the developing adolescent.6,7
While anxiety is a physiological behavioral response induced by a threat to wellbeing, social anxiety disorder is a pathological mental health problem characterized by the evasion of challenging social encounters and/or the development of incommensurate behavioral responses upon exposure to those encounters. It is often associated with functional impairment in social and occupational domains and in daily activities.8 It is estimated that 15% to 30% of youths are diagnosed with an anxiety disorder prior to adulthood, with social anxiety disorder accounting for a lifetime prevalence of 9.1% between the ages of 13 and 18 years.9 While some cases of social anxiety disorder may remit, if left untreated the patient may develop other anxiety disorders, depression, substance abuse problems, and suicide attempts.10
Actually, the current evidence of the association between the COVID-19 pandemic and the increase in the prevalence of mental health disorders among the general public and adolescents is limited. Previous epidemics like severe acute respiratory syndrome coronavirus-1 (SARS-CoV-1) revealed an increase in psychiatric symptoms like depression, anxiety, and posttraumatic stress disorder among the infected persons, healthcare workers, and noninfected persons during and after the epidemic.11 A literature review about the short-term mental consequences of the COVID-19 pandemic finds an increase in depression and anxiety symptoms among healthcare workers and infected patients, but not among the noninfected public.12 However, several reports from different parts of the world find an increased risk of anxiety, depression, feeling lonely, and a reduction in the quality of life among adolescents during the COVID-19 lockdown.13,14 A longitudinal survey assessing mental health problems among adolescents pre- and post-COVID-19 lockdown, reports adolescents to be more concerned about the restrictive measures than the viral infection itself. Additionally, they have increased symptoms of anxiety and depression and decreased life fulfillment compared to the prelockdown period.15 Another report about the impact of social isolation on mental health in the context of the COVID-19 pandemic finds adolescents to experience high rates of depression and anxiety during and after the end of the isolation period.16,17 Furthermore, the impact of the COVID-19 restrictions on mental health is more critical in children and adolescents with special needs, neurodevelopmental and psychiatric disorders who require close supportive services in schools that cannot be provided by distance learning.18
In light of these reports about the prevalence of mental health problems among adolescents during the COVID-19 lockdown, we conducted a study to evaluate the prevalence of severe social anxiety (SSA) disorder among a group of Lebanese adolescents during the COVID-19 pandemic.
Methods
The first case of SARS-CoV-2 infection was reported in Lebanon in February 2020. This was followed by a complete lockdown of all community facilities, schools, universities, and all ports of entry to the country. During that period, the country saw a few cases of SARS-CoV-2 weekly. Three months later all community facilities reopened with the exception of schools and universities, which made a transition to online distance teaching.
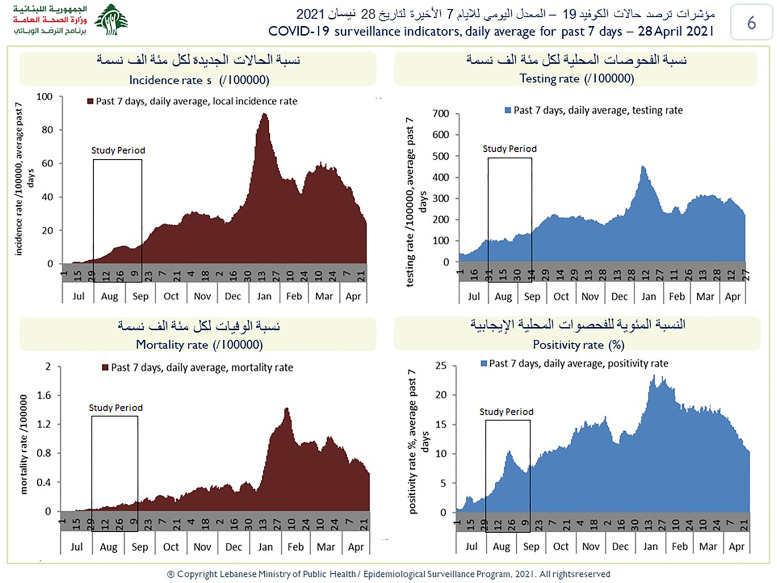
We conducted a cross-sectional online survey from August 1 through September 15, 2020, during the first wave of the COVID-19 epidemic in Lebanon (Figure 1).
Figure 1.
Coronavirus disease of 2019 (COVID-19) weekly surveillance in Lebanon (accessed on April 28, 2021).
The study was conducted to assess the prevalence of SSA in adolescents attending the private clinics of the participating authors, for which the medical files of eligible participants were reviewed, and their parents were contacted to get approval for their children's participation. The survey was created on Google Forms for the purpose of the study. Inclusion criteria consisted of healthy adolescents aged 15 to 19 years, with good English proficiency, as reflected in their school records. Exclusion criteria consisted of the presence of any chronic medical or physical disease, or mental health disorder including anxiety, depression, and attention deficit hyperactivity disorder in the participants’ medical files and the absence of a valid e-mail address. Since Lebanon is an Arabic-speaking country, with English commonly used and taught at schools, our English survey was first administered to a pilot group of 13 Lebanese adolescents between 15 and 19 years of age to assess the questionnaire clarity and to report the expected completion time for that age group. The group responded that the questions were direct, clear, and easy to answer and that they required 15 to 20 min to fill out.
Once oral approval was obtained from each participant's parents, a text message was sent to one of the parents’ cellphones outlining the purpose of the study, highlighting its anonymity, and ensuring the secure discarding of all collected data. The message also contained the Google Form link, for the adolescent to access and fill out the questionnaire. Upon clicking the link, the adolescents read a statement that further explained the objectives of the study, and asked them to sign the consent form to proceed.
The survey consisted of 2 parts. The first part inquired about some sociodemographic data including age, gender, and family conditions. Moreover, it inquired about activities during the COVID-19 lockdown including the daily amount of time spent studying and doing schoolwork, playing video games, texting with friends over social media, and practicing sports and hobbies. At the end of the survey, we included 6 questions related to the participant's knowledge about the COVID-19 disease, its cause, its route of infection and mode of transmission, the adolescent's source of information about the disease, the likelihood of being infected, and the likelihood of recovery after being infected.
The second part of the survey was the Liebowitz social anxiety scale for children and adolescents (LSAS-CA), (Supplemental file) which consisted of anxiety and avoidance subscales. Each subscale pertained to 24 different social situations, further classified into 12 social items and 12 performance items. The degree of anxiety was self-rated by the participant on a scale from 0 to 3 for each situation with a maximum total score of 144 for the 2 subscales. Participants put their ratings based on how those situations affected their behavior in the month prior to the survey. A total anxiety-avoidance cutoff score of 80 or more reflected severe/very severe anxiety and was referred to as the 30-day prevalence of SSA in our discussion.
The total LSAS-CA score was computed for each case in the survey. It was then mapped into a classification dependent variable where a total anxiety score of 80 or more reflected the presence of SSA in the participant. This dependent variable was tested for statistical association with the sociodemographic variables, and COVID-19 related questions on bivariate analysis, using Pearson's Chi-square tests in the cross-tabulation analyses. Results were presented as odds ratio (OR) with their 95% confidence interval (CI) using IBM SPSS Version 22. Statistical significance was considered at a P-value of .05 level.
Results
We invited 250 families to participate in the survey over the cellphone. A total of 202 adolescents responded by filling the online questionnaires. Twenty-four responses were discarded: 8 because the respondent was above 19 years of age, 7 because of double data entry with the same e-mail address, and 9 because of incomplete data entry.
A significant and positive correlation existed between the LSAS-CA anxiety and avoidance subscales’ scores with a Pearson correlation of 0.667 with a .01 significance level (2-tailed). Thirty two participants had LSAS-CA cutoff scores of ≥ 80 making an 18% prevalence of SSA among our participants.
Table 1 summarizes the results of sociodemographic variables and their association with SSA. High monthly family income and increased frequency of going out with friends per month had a negative association with SSA (OR = 0.321, 95% CI [0.135-0.761] and OR = 0.381, 95% CI [0.165-0.879] respectively). In contrast, time spent texting/chatting with friends and using social media, and time spent playing video games had a positive association with SSA (OR = 2.650, 95% CI [1.212-5.796] and OR = 2.866, 95% CI [1.166-7.045] respectively).
Table 1.
Sociodemographic Variables and Their Association With Severe Social Anxiety.
| Variable | Total number | None/mild/moderate/marked social anxiety number 146 | Severe social anxiety number 32 | Odd ratio (95% CI) | P-valuec |
|---|---|---|---|---|---|
| Age | |||||
| 15 to <16 years old | 47 | 38 (80.9%) | 9 (19.1%) | ||
| 16 to <17 years old | 122 | 103 (84.4%) | 19 (15.6%) | Not applicablea | .091 |
| ≥ 17 years old | 9 | 5 (55.6%) | 4 (44.4%) | ||
| Gender | |||||
| Male | 73 | 63 (86.3%) | 10 (13.7%) | 1.670 | .215 |
| Female | 105 | 83 (79.0%) | 22 (21.0%) | (0.738-3.777) | |
| Grade level | |||||
| Grade 9 or 10 | 69 | 55 (79.9%) | 14 (20.3%) | 0.777 | .523 |
| Grade 11 or 12 | 109 | 91 (83.5%) | 18 (16.5%) | (0.358-1.686) | |
| Monthly family income/month | |||||
| ≤ 1,500,000 LL | 95 | 21 (65.6%) | 11 (34.4%) | 0.321 | .008 |
| > 1,500,00 LL | 83 | 125 (85.6%) | 21 (14.4%) | (0.135-0.761) | |
| Current living conditions | |||||
| Living with parents | 143 | 120 (83.9%) | 23 (16.1%) | 1.806 | .184 |
| Living with 1 parent/othersb | 35 | 26 (74.3%) | 9 (25.7%) | (0.749-4.352) | |
| Family members living in the same house | |||||
| ≤ 4 members | 67 | 58 (86.6%) | 9 (13.4%) | 1.684 | .220 |
| > 4 members | 111 | 88 (79.3%) | 23 (20.7%) | (0.728-3.897) | |
| Time spent practicing sports and hobbies | |||||
| ≤ 2 h | 155 | 126 (81.3%) | 29 (18.7%) | 0.652 | .509 |
| > 2 h | 23 | 20 (87.0%) | 3 (13.0%) | (0.181-2.341) | |
| Time spent going out with friends/month | |||||
| <2 times/month | 95 | 72 (75.8%) | 23 (24.2%) | 0.381 | .021 |
| ≥3 times/month | 83 | 74 (89.2%) | 9 (10.8%) | (0.165-0.879) | |
| Time spent in study and schoolwork | |||||
| ≤ 4 h/day | 159 | 129 (81.1%) | 30 (18.9%) | 0.506 | .371 |
| > 4 h/day | 19 | 17 (89.5%) | 2 (10.5%) | (0.111-2.309) | |
| Time spent texting, chatting, and watching social media | |||||
| ≤ 4 h/day | 122 | 106 (86.9%) | 16 (13.1%) | 2.650 | .013 |
| > 4 h/day | 56 | 40 (71.4%) | 16 (28.6%) | (1.212-5.796) | |
| Time spent playing video games | |||||
| ≤6 h/day | 72 | 65 (90.3%) | 7 (9.7%) | 2.866 | .018 |
| > 6 h/day | 106 | 81 (76.4%) | 25 (23.6%) | (1.166-7.045) | |
| History of smoking | |||||
| No | 150 | 126 (84.0%) | 24 (16.0%) | 2.100 | .112 |
| Yes | 28 | 20 (71.4%) | 8 (28.6%) | (0.829-5.316) |
Odds ratio and 95% confidence interval could not be calculated because of the presence of 3 categories for age.
This category involves adolescents living with separated/divorced parents, single parents, grandparents, or other guardians.
Significant at the .05 level.
Table 2 summarizes the results of the source of information about COVID-19 and its impact on SSA. All participants used more than one source of information about COVID-19, with some sources more commonly used than others. The majority of our participants get their information from television, followed by social media platforms, such as WhatsApp and Instagram. Out of the 9 suggested sources of information, WhatsApp was the only variable that had a negative statistical association with SSA (OR = 0.474, 95% CI [0.219-1.026]).
Table 2.
Source of Information About COVID-19 and its Impact on Severe Social Anxiety.
| Variable | Total number | None/mild/moderate/marked social anxiety number 146 | Severe anxiety number 32 | Odd ratio (95% CI) | P-valuea |
|---|---|---|---|---|---|
| Television | |||||
| No | 45 | 35 (77.8%) | 10 (22.2%) | 0.694 | .391 |
| Yes | 133 | 111 (83.5%) | 22 (16.5%) | (0.300-1.604) | |
| No | 68 | 51 (75.0%) | 17 (25.0%) | 0.474 | .055 |
| Yes | 110 | 95 (86.4%) | 15 (13.6%) | (0.219-1.026) | |
| No | 78 | 64 (82.1%) | 14 (17.9%) | 1.003 | .993 |
| Yes | 100 | 82 (82.0%) | 18 (18.0%) | (0.464-2.170) | |
| Parents | |||||
| No | 79 | 62 (78.5%) | 17 (21.5%) | 0.651 | .272 |
| Yes | 99 | 84 (84.8%) | 15 (15.2%) | (0.302-1.404) | |
| Peers | |||||
| No | 116 | 91 (78.4%) | 25 (21.6%) | 0.463 | .089 |
| Yes | 62 | 55 (88.7%) | 7 (11.3%) | (0.188-1.142) | |
| No | 149 | 123 (82.6%) | 26 (17.4%) | 1.234 | .678 |
| Yes | 29 | 23 (79.3%) | 6 (20.7%) | (0.457-3.332) | |
| No | 153 | 124 (81.0%) | 29 (19.0%) | 0.583 | .401 |
| Yes | 25 | 22 (88.0%) | 3 (12.0%) | (0.163-2.081) | |
| Other sources | |||||
| No | 109 | 94 (86.2%) | 15 (13.8%) | 2.049 | .066 |
| Yes | 69 | 52 (75.4%) | 17 (24.6%) | (0.946-4.436) |
Significant at the .05 level.
Table 3 summarizes the adolescents’ knowledge about COVID-19 disease and its association with SSA. One hundred seventy-eight participants responded to the first 3 questions related to knowledge about COVID-19. There was no statistical association between the participants’ knowledge about COVID-19 and SSA (Table 3). Only 69 adolescents responded to the questions related to the likelihood of infection and recovery from COVID-19. Fifty-one percent of the participants believed that they were likely to acquire infection. There was no statistical association between their fear of infection and the prevalence of SSA (OR = 2.222, 95% CI [0.601-8.220]). Most participants (95.6%) believed they were likely to recover from an infection (OR = 0.400, 95% CI [0.033-4.806]).
Table 3.
Adolescents’ Knowledge About Coronavirus Disease of 2019 (COVID-19) and its Association With Severe Social Anxiety.
| Variable | Total number | None/mild/moderate/marked social anxiety number | Severe/very severe social anxiety number | Odd ratio (95% CI) | P-valuea |
|---|---|---|---|---|---|
| Cause of COVID-19 | 178 | ||||
| Viral | 174 | 143 (82.2%) | 31 (17.8%) | 0.650 | .711 |
| Other than viral | 4 | 3 (75.0%) | 1 (25.0%) | (0.065-6.462) | |
| Route of infection with COVID-19 | 178 | ||||
| Scratching eyes or noses with fingers | 155 | 130 (83.9%) | 25 (16.1%) | 0.440 | .095 |
| Others | 23 | 16 (96.6%) | 7 (30.4%) | (0.164-1.178) | |
| Mode of transmission of COVID-19 | 178 | ||||
| Droplets from nasal secretions of infected person | 145 | 121 (83.4%) | 24 (16.6%) | 0.620 | .299 |
| Others | 33 | 25 (75.8%) | 8 (24.2%) | (0.250-1.538) | |
| During COVID-19 outbreak, how much likely do you think you are exposed to become infected? | 69 | ||||
| Absolutely Not or Unlikely | 34 | 30 (88.2%) | 4 (11.8%) | 2.222 | .224 |
| Possibly or Likely | 35 | 27 (77.1%) | 8 (22.9%) | (0.601-8.220) | |
| If you are infected with COVID-19 do you think you can recover? | 69 | ||||
| Absolutely not or unlikely | 3 | 2 (66.7%) | 1 (33.3%) | 0.400 | .456 |
| Possibly or likely | 66 | 55 (83.8%) | 11 (16.7%) | (0.033-4.806) |
Significant at the .05 level.
Discussion
Social anxiety is one of the most prevalent psychiatric disorders in children and adolescents. Its prevalence is underestimated because it is ignored and misinterpreted as a transient mood problem and because adolescents use tactics to avoid social and performance situations that evoke their fears.19
The prevalence of social anxiety disorder varies not only according to ethnic, cultural, and psychosocial backgrounds of the community, but also according to the diagnostic tool used for its assessment. A formal assessment of social anxiety disorder depends on diagnostic interviews, self-report questionnaires, and behavioral assessments, all of which are based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) or Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) criteria. Self-rating scales, like the LSAS-CA, are very helpful screening tools in identifying asymptomatic individuals with anxiety in clinical and research settings. They are not diagnostic by themselves and require further confirmation by structured diagnostic interviews.20 The LSAS-CA is often used to screen for social phobias in children and adolescents. In addition to its ability to identify between healthy individuals and those with anxiety disorder, it identifies the severity of the avoidance and the phobic behavior of the individual during both performance and social interaction situations. It has excellent transcultural psychometric properties. Its cutoff scores may be used to provide the best balance between specificity and sensitivity for the diagnosis of social anxiety disorder with higher total scores reflecting more severe disorder. A total anxiety-avoidance cutoff score of 30 and above has a sensitivity of 90.7% and a specificity of 65.2% for the differentiation between individuals with social phobia and other anxiety disorders. A total cutoff score of 60 and above differentiates between social anxiety and generalized social anxiety disorder.21 In our study, 82% of our participants had a total cutoff score of ≥ 30, and 45% had a total cutoff score of ≥ 60, while 18% had a total cutoff score of ≥ 80. The major limitation of LSAS-CA is that it does not capture the impact of the anxiety disorder on the cognitive function and daily activities of the individual.22,23
In general, the reported cumulative prevalence of any anxiety disorder in children and adolescents in Western countries ranges between 15% and 20%,24 and data from the US National Comorbidity Survey Adolescent Supplement, reveals a lifetime prevalence of any anxiety disorder of 31.9%, a 1-month prevalence of 14.9% and severe impairment of 8.3% among US adolescents aged 13 to 18 years, diagnosed by a structured diagnostic interview.25 As for low and middle-income countries, reports are scarce, but reveal prevalence rates of around 28%.26 On the other hand, Zhou et al,27 reported a 37.4% prevalence of generalized anxiety disorder among Chinese adolescents during COVID-19 lockdown by using the Generalized Anxiety Disorder scale as a screening tool.
Fegert et al28 divide the impacts of infectious epidemics, like COVID-19, on the community into 3 phases. The first phase is the preparation phase during which governments enforce restrictive measures to mitigate the spread of infection. The second is a punctum maximum phase during which the number of reported cases and mortality rate reaches a peak. Finally, a third phase is associated with the return to normality and a recovery from the epidemic. Each phase has its different psychosocial impacts on the community. Accordingly, our study was performed during the preparatory phase of the COVID-19 pandemic in Lebanon (Figure 1). Thus, performing the study at later phases of the epidemic may reveal different prevalence rates.
There are no national statistical data about the prevalence of social anxiety in Lebanon among adolescents. Available data from the World Mental Health Survey Initiative study in 2017, reveals that the 30-day and lifetime prevalence of social anxiety disorder among individuals above 18 years of age in Lebanon are 0.8% and 1.9%, respectively.29 Comparatively, 18% of our participants are found to have 30-day SSA (Table 1). This high rate of SSA in our study can be partly explained by our use of a different study methodology for diagnosis and because some adolescents with social anxiety disorder remit or develop other psychiatric or behavioral problems in adulthood.10 Additionally, the country witnessed 2 major national crises at the time of our study. The first crisis was the Beirut port explosion on August 4, 2020, with tragic implications on the economic, social, and environmental levels. The second crisis is the ongoing largest and severest economic depression in the country since October 2019, which left more than half of the population below the poverty line with major challenges in accessing food, healthcare, and basic services with a rise in the unemployment rate.30 Together, these events could have played a part in the high prevalence of SSA among our participants during the COVID-19 lockdown.
Several studies demonstrate that social anxiety disorders aggregate in families secondary to genetic and environmental factors. Genetic factors include familial temperamental fearfulness and withdrawal in response to novel stimuli.31 While environmental factors include parenting practices, such as over-involvement or overprotection from parents and/or harsh familial interactions and family socioeconomic conditions.32,33 Both factors may cause substantial impairment in family relationships, academic achievements, and vice versa.34 The prevalence of anxiety disorders remains stable during the first 6 years of life and increases in adolescence, which reflects an increasing impact of other environmental factors and peer pressure with age.35,36 In our study, 76.5% of the participants live with biological parents, and 23.5% live with 1 parent. Neither living with a single parent, overcrowding, nor place of residence are associated with SSA in our study. The effects of parenting practices with SSA are not investigated in our study. The only family variable associated with SSA in our study is family income. Families with high monthly incomes suffer less SSA compared to low-income families. Our finding is consistent with studies about the influence of family income on the socioemotional, mental, physical, and environmental health of family members.37 With increased family income parents are less stressed and can provide better nutrition and health care for their family and they are able to invest more in educational resources for their children. A low family income is associated with parental mental health problems, financial difficulties, divorce and lack of intimacy with children, trouble with the law, school problems, and different treatment of siblings.38 In contrast high family income allows children to go out with their friends more frequently and hence enables more socialization. Our study shows that adolescents who go out with their friends more than 3 times per month have less SSA than the rest of their peers.
Females are reported to have a higher prevalence of anxiety disorder in several studies,25,27,39 yet, other studies show no gender differences.40 A study by Ranta et al,41 finds girls to have higher levels of anxiety symptoms on most items of the Social Phobia Inventory questionnaire, yet both genders scored equally on items related to reluctance to public speaking and being the center of attention. Importantly, most of the studies on anxiety trajectories were on participants in early adolescence, and studies conducted on participants in middle-to-late adolescence might show different results. In our study, no significant association between gender and SSA is found (OR = 1.670, 95% CI [0.738-3.777]). Overall, further research is required to address whether SSA is more prevalent in a specific gender in the different developmental stages.
Physical activity positively affects a number of biological and psychological mechanisms including anxiety disorders.42 No single mechanism sufficiently accounts for the anxiolytic effect of exercise. The Global School-Based Student Health Survey in Lebanon in 2017,43 defines physical activity as any activity that increases heart rate and breathing efforts like practicing sports, playing with friends, or walking to school for a total time of at least 60 min per day. The 13% of the adolescents included in that survey were physically active. In our study, 87% of our participants claimed to practice sports and hobbies for more than 2 h per day. This high percentage is probably because we grouped the practice of sports and hobbies together in 1 question. That approach was not associated with the reduction of SSA in our population (Table 1). To explore the clinical role of exercise or hobbies in the prevalence of SSA, we need further studies addressing each activity separately.
Adolescents are active users of online social media with 71% of them using more than 1 platform.44,45 Social media platforms can have educational benefits by delivering useful information and support. However, some websites are harmful because they require an exchange of personal information, deliver false information and expose children and adolescents to inappropriate content like sexting and cyberbullying and are associated with Facebook depression.46 Another problem with social media is advertising and digital marketing which may reinforce harmful behaviors like high/low-calorie diet, use of tobacco products, use of alcohol, and marijuana.47,48 During the lockdown, around 31.5% of our participants spent more than 4 h per day using social media and texting with friends, a behavior that was associated with SSA. In addition, 59.5% spent more than 6 h per day playing video games, which was also associated with SSA. Our findings are consistent with the study of Sampasa-Kanyinga et al,49,50 which found that spending more than 2 h per day on social networking sites was associated with poorer self-rated mental health, psychological distress, suicidal ideation, and unmet needs for mental health support. Our study shows that adolescents who spend longer time on social media during the COVID-19 lockdown have more SSA than the rest of their peers.
In February 2020, the WHO warned about fake COVID-19 information on social media.51 One of the challenges in using social media is to be able to identify fabricated from truthful information. To get evidence-based information about COVID-19, WHO recommends its social media channels and its official websites. Our participants use more than one social media platform as a source of information about COVID-19 disease (Table 2). The majority get their information from television followed by WhatsApp, Instagram, and their parents. Participants who used WhatsApp as a source of information had less SSA in comparison to the users of other sources. This may be because frequent WhatsApp users are more sociable than their peers or it may be a coincidental finding. More detailed information about the social characteristics of the WhatsApp users and the purpose of its utilization is required to validate our findings.
The association of smoking with mental illness is a major health problem. The co-occurrence varies with evidence that smoking is associated with subsequent depression and anxiety and vice versa.52,53 Furthermore, smoking in adolescents is associated with both having close friends who smoke and lower socioeconomic status.54 The Global School-Based Student Health Survey in Lebanon in 2017,43 revealed that 12.7% of adolescents have smoked in the past 30 days and 32.7% have used some tobacco product other than cigarettes. In our survey, 15.7% of our participants have ever smoked (Table 1), 30% of them used regular cigarettes, 26.5% used both regular and e-cigarettes, 20% smoked e-cigarettes, and 23.5% used some other tobacco products. It is worth noting that in spite of the toxic effects of e-cigarettes on the lungs, particularly during the COVID-19 pandemic, their use is gaining a reputation among adolescents.55,56 Our study shows no association between smoking and SSA in our participants (OR = 2.100, 95% CI [0.829-5.316]). The absence of association is probably due to the small number of frequent smokers in our participants.
The available data from the COVID-19 outbreak in China show exacerbation of common mental disorders like major sleep disturbances, depression, and anxiety in infected persons.57 Our study was performed during the preparatory phase of the COVID-19 pandemic in Lebanon, few months after the resumption of social activities with adherence to social distancing, facemasks, hand washing, and distance learning. Over that period, the number of daily COVID-19 cases increased to more than 1200 cases/day, with daily mortalities growing to reach 20 cases per day.58 The increase in the number of cases was due to poor public compliance with the recommended preventive measures.
Given that context, 178 participants answered the questions related to the COVID-19 causative agent, route of infection, and method of spread of the virus (Table 3). There was no statistical correlation between knowledge about any of the above questions and the prevalence of SSA. This finding is consistent with a previous study which showed that knowledge about the virus does not increase anxiety level among the public15 and is in contradiction with a previous Chinese study which showed that adolescents’ awareness about SARS-CoV-2 infection was negatively associated with generalized anxiety.27
Only 69 participants answered the questions related to the likelihood of infection and recovery. Internationally, SARS-CoV-2 infection has a lower prevalence and a benign course in children.59 Yet recent CDC reports show that adolescents may have a higher risk for infection compared to other children.60 In addition, newer data from the United States reveal an increase in the number of infected children reaching up to 12.6% of all the reported COVID-19 cases, 0.8% of them require hospitalization with a mortality rate of 0.01%.61 Although less than 40% of our participants responded to the questions related to the chances for infection and recovery. Their responses show that they had little awareness about their likelihood of infection, as 49% of them wrongly believed they were unlikely to get infected, and 95.6% of them truly believed they would recover from an infection. In view of the increasing number of children and adolescents acquiring the disease, the appearance of new virulent strains of the virus, and until an effective vaccine coverage is attained among children and adolescents, more efforts are required to increase awareness among adolescents about COVID-19 disease and the compliance with its preventive measures.
Our study has the following limitations: It is performed at the preparatory phase of the COVID-19 pandemic in Lebanon and during the presence of 2 major socioeconomic crises, our participants are healthy adolescents recruited from the greater Beirut area, attending private schools with good English proficiency, and it lacks the inquiry about the impact of COVID-19 restrictive measures on the prevalence of SSA in our participants. Finally, our findings are preliminary and a more comprehensive longitudinal survey on a larger and more representative sample is required to identify the true burden of the disorder in Lebanese adolescents. In spite of these limitations, our study provides baseline data about the prevalence of SSA in Lebanon during the COVID-19 pandemic.
Conclusion
Social anxiety is a common disorder among adolescents with serious future mental health impacts if not attended to early. SSA was prevalent in 18% of the adolescents in our study during the preparatory phase of the COVID-19 lockdown. Furthermore, our study showed decreased awareness about the COVID-19 disease among adolescents whose SSA at the time of the study was associated with the use of social media for chatting and texting, and with playing video games during the lockdown. Mitigating factors included high family socioeconomic status, socializing with friends, and using WhatsApp as a source of information about COVID-19. National mental health policymakers are prompted to implement early intervention strategies to prevent and counteract the consequences of social anxiety disorder on the health of the future generation, particularly those associated with the COVID-19 pandemic and other socioeconomic crises.
Supplemental Material
Supplemental material, sj-docx-1-jpx-10.1177_23743735211038386 for Severe Social Anxiety Among Adolescents During COVID-19 Lockdown by Mohamad H. Itani, Ekram Eltannir, Hayat Tinawi, Dima Daher, Akram Eltannir and Adib A. Moukarzel in Journal of Patient Experience
Supplemental material, sj-JPG-2-jpx-10.1177_23743735211038386 for Severe Social Anxiety Among Adolescents During COVID-19 Lockdown by Mohamad H. Itani, Ekram Eltannir, Hayat Tinawi, Dima Daher, Akram Eltannir and Adib A. Moukarzel in Journal of Patient Experience
Acknowledgments
The authors thank Mr Hadi Itani and Miss Sanaa Itani for reviewing the manuscript.
Author Biographies
Mohamad H. Itani is a pediatrician with a Master's Degree in Family medicine. He is currently the chief of the medical staff at Mohamad Khaled Rehabilitation Hospital, Beirut, Lebanon. His fields of interest include general and behavioral pediatrics and rehabilitation and improvement of quality of life delivered for children with disabilities and elders.
Ekram Eltannir is a pediatrician, the head of the pediatric division in Najjar Hospital, Beirut, Lebanon. Her areas of interest include improving the quality of care delivered for children and education of parents to improve patients' care outcomes.
Hayat Tinawi is a pediatrician in Najjar Hospital, Beirut, Lebanon. She runs her private clinic in Beirut. Her areas of interest include improving timely vaccination coverage and applying adequate nutrition practices for infants and children.
Dima Daher is a clinical neuropsychology (Psy.D.) student at the Université de Montréal, Canada. She completed her undergraduate study in psychology at King's College London. Her areas of interest include the gut-brain axis in autism and neurofeedback training following concussions.
Akram Eltannir is an associate professor of Industrial Engineering at Beirut Arab University, Beirut, Lebanon. His area of specialty includes advanced statistical analysis and risk modeling for supply chains and project management.
Adib A. Moukarzel is a pediatric gastroenterologist and the chairman of the Department of Pediatrics at Hotel Dieu de France Saint Joseph University Hospital, Beirut, Lebanon. His areas of interest are Parenteral Nutrition and trace minerals, Gastro-intestinal manometry, Diarrhea in children, and Improvement of quality of life in children.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mohamad H. Itani, MSc, MRCGP [INT] https://orcid.org/0000-0002-3318-9001
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Blakemore SJ, Mills KL. Is adolescence a sensitive period for sociocultural processing? Annu Rev Psychol. 2014;65(1):187-207. [DOI] [PubMed] [Google Scholar]
- 2.Stirrups R. The storm and stress in the adolescent brain. Lancet Neurol. 2018;17(5):404. [DOI] [PubMed] [Google Scholar]
- 3.Knoll LJ, Magis-Weinberg L, Speekenbrink M, Blakemore S-J. Social influence on risk perception during adolescence. Psychol Sci. 2015;26(5):583-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. 2020;20(1):293. Published 2020 Jun 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michaud P, Fombonne E. The ABC of adolescence: common mental health problems. Br Med J. 2005;330(7495):835-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooks S.K, Webster R.K, Smith L.E, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet (London, England) 2020;395(10227):912-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293(113429):113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and statistical manual for mental disorders. Vol. 5. Washington, DC: American Psychiatric Press; 2013. [Google Scholar]
- 9.Freidl EK, Stroeh OM, Elkins RM, Steinberg E, Albano AM, Rynn M. Assessment and treatment of anxiety among children and adolescents. Focus (Am Psychiatr Publ). 2017;15(2):144-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, et al. Clinical characteristics of anxiety disordered youth. J Anxiety Disord. 2010;24(3):360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ko C-H, Yen C-F, Yen J-Y, Yang M-J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006;60(4):397-403 [DOI] [PubMed] [Google Scholar]
- 12.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ravens-Sieberer U, Kaman A, Otto C, Adedeji A, Devine J, Erhart M, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int 2020; 117(48):828-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50(1):44-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-39.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajabi M. Mental health problems amongst school-age children and adolescents during the COVID-19 pandemic in the UK, Ireland and Iran: a call to action and research. Health Promot Perspect. 2020;10(4):293-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ollendick TH, Hirshfeld-Becker DR. The developmental psychopathology of social anxiety disorder. Biol Psychiatry. 2002;51(1):44-58. [DOI] [PubMed] [Google Scholar]
- 20.Letamendi AM, Chavira DA, Stein MB. Issues in the assessment of social phobia: a review. Isr J Psychiatry Relat Sci. 2009;46(1):13-24. [PMC free article] [PubMed] [Google Scholar]
- 21.Mennin DS, Fresco DM, Heimberg RG, Schneier FR, Davies SO, Liebowitz MR. Screening for social anxiety disorder in the clinical setting: using the Liebowitz social anxiety scale. J Anxiety Disord. 2000;16(6):661-73. [DOI] [PubMed] [Google Scholar]
- 22.Masia-Warner C, Storch EA, Pincus DB, Klein RG, Heimberg RG, Liebowitz MR. The Liebowitz social anxiety scale for children and adolescents: an initial psychometric investigation. J Am Acad Child Adolesc Psychiatry. 2003;42(9):1076-84. [DOI] [PubMed] [Google Scholar]
- 23.Tulbure BT, Szentagotai A, Dobrean A, David D. Evidence based clinical assessment of child and adolescent social phobia: a critical review of rating scales. Child Psychiatry Hum Dev. 2012;43(5):795-820. [DOI] [PubMed] [Google Scholar]
- 24.Beesdo-Baum K, Knappe S. Developmental epidemiology of anxiety disorders. Child Adolesc Psychiatr Clin N Am. 2012;21(3):457-78. [DOI] [PubMed] [Google Scholar]
- 25.Merikangas K.R., He J.-P., Burstein M., Swanson S.A, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U. S. Adolescents: results from the national comorbidity survey replication- adolescent supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yatham S, Sivathasan S, Yoon R, da Silva TL, Ravindran AV. Depression, anxiety, and post-traumatic stress disorder among youth in low and middle income countries: a review of prevalence and treatment interventions. Asian J Psychiatr. 2018;38:78-91. [DOI] [PubMed] [Google Scholar]
- 27.Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29(6):749-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stein DJ, Collaborators WHOWMHS, Lim CCW, Roest AM, Jonge P, Aguilar-Gaxiola S, et al. The cross-national epidemiology of social anxiety disorder: data from the world mental health survey initiative. BMC Med. 2017;15(1):1186.12916-017-0889-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Worldbank.org. [cited 2021 May 25]. Available from: Lebanon Overview (worldbank.org)
- 31.Ginsburg GS, Schleider J, Tein JY, Drake KL. Family and parent predictors of anxiety disorder onset in offspring of anxious parents. Child Youth Care Forum. 2018;47(3):363-76. [PMC free article] [PubMed] [Google Scholar]
- 32.Drake KL, Ginsburg GS. Parenting practices of anxious and non-anxious mothers: a multi-method multi-informant approach. Child Fam Behav Ther. 2011;33(4):299-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghazwani JY, Khalil SN, Ahmed RA. Social anxiety disorder in Saudi adolescent boys: prevalence, subtypes, and parenting style as a risk factor. J Family Community Med. 2016;23(1):25-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: linking biology and behavior within a developmental framework. Annu Rev Psychol. 2005;56(1):235-62. [DOI] [PubMed] [Google Scholar]
- 35.Bufferd SJ, Dougherty LR, Carlson GA. Psychiatric disorders in preschoolers: continuity from ages 3 to 6. Am J Psychiatr. 2012;169(11):1157-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McLaughlin KA, King K. Developmental trajectories of anxiety and depression in early adolescence. J Abnorm Child Psychol. 2015;43(2):311-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gennetian LA, Castells N, Morris P. Meeting the basic needs of children: does income matter? Child Youth Serv Rev. 2010;32(9):1138-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reiss F, Meyrose A-K, Otto C, Lampert T, Klasen F, Ravens-Sieberer U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: results of the German BELLA cohort-study. PLoS One. 2019;14(3):e0213700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leadbeater B, Thompson K, Gruppuso V. Co-occurring trajectories of symptoms of anxiety, depression, and oppositional defiance from adolescence to young adulthood. J Clin Child Adolesc Psychol. 2012;41(6):719-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ohannessian CM, Milan S, Vannucci A. Gender differences in anxiety trajectories from middle to late adolescence. J Youth Adolesc. 2017;46(4):826-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ranta K, Kaltiala-Heino R, Koivisto A-M, Tuomisto MT, Pelkonen M, Marttunen M. Age and gender differences in social anxiety symptoms during adolescence: the social phobia inventory (SPIN) as a measure. Psychiatry Res. 2007;153(3):261-70. [DOI] [PubMed] [Google Scholar]
- 42.Meyer T, Broocks A, Bandelow B, Hillmer-Vogel U, Rüther E. Endurance training in panic patients: spiroergometric and clinical effects. Int J Sports Med. 1998;19(7):496-502. [DOI] [PubMed] [Google Scholar]
- 43.Lebanon—global school-based student health survey 2017 [Internet]. Who.int. [cited 2021 Feb 5]. Available from: https://extranet.who.int/ncdsmicrodata/index.php/catalog/645/datafile/F1
- 44.Antheunis ML, Schouten AP, Krahmer E. The role of social networking sites in early adolescents’ social lives. J Early Adolesc. 2016;36(3):348-71. [Google Scholar]
- 45.Lenhart A. Teens, social media & technology overview 2015 [Internet]. Pewresearch.org. 2015 [cited 2021 Feb 5]. Available from: https://www.pewresearch.org/internet/2015/04/09/teens-social-media-technology-2015/. 2015
- 46.Chretien KC, Kind T. Social media and clinical care: ethical, professional, and social implications. Circulation. 2013;127(13):1413-21. [DOI] [PubMed] [Google Scholar]
- 47.Denecke K, Bamidis P, Bond C, Gabarron E, Househ M, Lau AYS, et al. Ethical issues of social media usage in healthcare. Yearb Med Inform. 2015;10(1):137-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Radesky J, Chassiakos YLR, Ameenuddin N, Navsaria D, Council on communication and media. Digital advertising to children. Pediatrics. 2020;146(1):e20201681. [DOI] [PubMed] [Google Scholar]
- 49.Sampasa-Kanyinga H, Lewis RF. Frequent use of social networking sites is associated with poor psychological functioning among children and adolescents. Cyberpsychol Behav Soc Netw. 2015;18(7):380-5. [DOI] [PubMed] [Google Scholar]
- 50.Sampasa-Kanyinga H, Hamilton HA. Social networking sites and mental health problems in adolescents: the mediating role of cyberbullying victimization. Eur Psychiatry. 2015;30(8):1021-7. [DOI] [PubMed] [Google Scholar]
- 51.Munich security conference [Internet]. Who.int. [cited 2021 Feb 5]. Available from: https://www.who.int/director-general/speeches/detail/munich-security-conference
- 52.Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19(1):3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smoking and mental health [Internet]. Rcplondon.ac.uk. 2013[cited 2021 Feb 5]. Available from: https://www.rcplondon.ac.uk/projects/outputs/smoking-and-mental-health
- 54.Jenssen BP, Walley SC, Section on tobacco control. E-cigarettes and similar devices. Pediatrics. 2019;143(2):e20183652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lorant V, Rojas VS, Robert P-O, Kinnunen JM, Kuipers MAG, Moor I, et al. Social network and inequalities in smoking amongst school-aged adolescents in six European countries. Int J Public Health. 2017;62(1):53-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health. 2020;67(4):519-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huang X, Li H, Meyers K, Xia W, Meng Z, Li C, et al. Burden of sleep disturbances and associated risk factors: a cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci Rep. 2017;7(1):3657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lebanese Ministry of Public Health. Monitoring of COVID-19 Infection in Lebanon [cited 2020 October 21]. Available from: https://www.moph.gov.lb/en/Media/view/41403/1/monitoring-of-covid-19-infection-in-lebanon
- 59.Ortiz-Prado E, Simbaña-Rivera K, Gómez-Barreno L, Rubio-Neira M, Guaman LP, Kyriakidis NC, et al. Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the coronavirus disease 2019 (COVID-19), a comprehensive literature review. Diagn Microbiol Infect Dis. 2020;98(1):115094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leeb RT, Price S, Sliwa S, Kimball A, Szucs L, Caruso E, et al. COVID-19 trends among school-aged children—United States, March 1–September 19, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(39):1410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jenco M. Pediatric COVID-19 cases surpass record for a single week. AAP News [Internet]. 2021. [cited 2021 May 27]; Available from: https://www.aappublications.org/news/2021/01/19/pediatric-covid-cases-weekly-record-011921?utm_source=TrendMD&utm_medium=TrendMD&utm_campaign=AAPNews_TrendMD_0 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpx-10.1177_23743735211038386 for Severe Social Anxiety Among Adolescents During COVID-19 Lockdown by Mohamad H. Itani, Ekram Eltannir, Hayat Tinawi, Dima Daher, Akram Eltannir and Adib A. Moukarzel in Journal of Patient Experience
Supplemental material, sj-JPG-2-jpx-10.1177_23743735211038386 for Severe Social Anxiety Among Adolescents During COVID-19 Lockdown by Mohamad H. Itani, Ekram Eltannir, Hayat Tinawi, Dima Daher, Akram Eltannir and Adib A. Moukarzel in Journal of Patient Experience