Abstract
Background:
Clostridioides difficile infection (CDI) and inflammatory bowel disease (IBD) are global gastroenterological diseases that cause considerable burden on human health, healthcare systems, and society. Faecal microbiota transplantation (FMT) is an effective treatment for recurrent Clostridioides Difficile Infection (rCDI) and a promising therapy for IBD. However, indication for FMT in IBD is still unofficial. Consequently, the National Institute for Health and Care Excellence (NICE) is seeking healthcare providers’ advice on whether to update FMT guidelines.
Methods:
A systematic review methodology was adopted for this study. Five databases (CINAHL, MEDLINE, Cochrane Library, Scopus, Web of Science) and grey literature were systematically searched for English language literature to 14 May 2021. The quality of the included studies was then appraised using the Institute for Public Health Sciences cross-sectional studies tool, after which the findings of the studies were narratively synthesised.
Results:
Thirteen cross-sectional studies with 4110 validated questionnaire responses were included. Narrative synthesis found that 39.43% of respondents were familiar with FMT (N = 3746, 95%CI = 37.87%–41%), 58.81% of respondents would recommend FMT to their patients (N = 1141, 95%CI = 55.95%–61.67%), 66.67% of respondents considered lack of clinical evidence was the greatest concern regarding FMT (N = 1941, 95%CI = 64.57%–68.77%), and 40.43% respondents would not implement FMT due to concerns about infection transmission (N = 1128, 95%CI = 37.57%–43.29%).
Conclusion:
Healthcare providers’ knowledge of FMT is relatively low and education is an effective strategy to improve it. As knowledge of FMT increases, willingness to recommend it also increases. Strengthening FMT clinical efficacy and reducing infection can enhance its public acceptance, application and popularity. However, further research is required to explore the donor screening procedure.
Keywords: Clostridioides difficile infection, faecal microbiota transplantation, healthcare providers, inflammatory bowel disease, perception, quantitative systematic review
Introduction
Clostridioides difficile infection (CDI) is the most common healthcare-associated infection and is predicted to become a global health threat.1 In 2017, an estimated 223,900 cases of hospitalised infections related to CDI occurred in the United States (US),2 while Public Health England reports that there were 3380 cases in the United Kingdom (UK) the same year.3 In China, however, the incidence of CDI was 3.4 per 10,000 admissions from 2009 to 2016.4
Similarly, inflammatory bowel disease (IBD) has developed into a worldwide gastroenterological disease in the 21st century due to the changing diets that accompany industrialising societies.5 The pathogenesis and clinical course of IBD are directly influenced by diet and the higher animal-sourced and higher calorie intake characteristics of Western diets may have negative effects on gut microbiota.6 IBD includes two chronic inflammation diseases into the gut: ulcerative colitis (UC) and Crohn’s disease.7 Currently, there are up to 300,000 patients suffering from IBD in the United Kingdom, an estimated 3.1 million in the United Studies, and about 350,000 from 2005 to 2014 in China.8–10
CDI is more common in patients with IBD, which can lead to higher recurrence, worse disease course, longer hospitalisation, diarrhoea, and higher rates of colectomy and mortality.11,12 A review reported that the CDI directly caused mortality rate is estimated at 5%, while deaths associated with its complications stands at 15% to 25%.13
Faecal Microbiota Transformation (FMT) has been attracting increasing interest as a treatment for CDI and IBD in recent years. FMT involves taking faeces from healthy donors to rebuild the gut microbiota of a diseased individual,14–16 and has shown to be an efficient alternative therapy for recurrent CDI (rCDI)17 and a potential treatment for IBD.18,19 Even though FMT has wide-ranging therapeutic potential, how precisely it works is still poorly understood.20 As such, the use of FMT is lower than the interest in it. A survey undertaken in the UK revealed that only 22% of physicians reported FMT utilisation in their institution in the last 10 years, while only 6% reported performing over ten FMTs.21 The perception of FMT as a treatment is also a key factor in its utilisation. From a patient perspective, a survey revealed that approximately 46% of patients with UC were prone to accept FMT as a treatment, and up to 94% of patients with rCDI were willing to accept FMT if it was recommended by physicians.22 Likewise, another survey showed that although patients found FMT unappealing, > 81% were open to it and this number increased to 94% when advised by their physicians.23 Consequently, healthcare providers and their perception towards FMT are very important and directly influence patients’ acceptance of FMT. Therefore, the purpose of this systematic review is to analyse and synthesise contemporary evidence about the healthcare providers’ perception of FMT for CDI and IBD.
Aim and objective
This systematic review aims to explore healthcare providers’ perception of FMT for CDI and IBD. This will be achieved through identifying, critically appraising and synthesising all available research that answers the following question:
What are the knowledge and attitudes of healthcare providers regarding FMT for CDI and IBD?
Methods
Search strategy
To identify primary studies, CINAHL, MEDLINE, Cochrane Library, Scopus, Web of Science, Google Scholar and grey literature were searched. The search strategy was conducted by two authors independently (YL, KA). The following search terms were utilised: [“healthcare professional” OR “healthcare giver” OR “healthcare provider” OR “healthcare worker” OR “physician” OR “medical staff” OR “doctor” OR “nurse” OR “medical student” OR “healthcare personnel”] AND [“perception of FMT” OR “attitudes of FMT” OR “recognition of FMT” OR “awareness of FMT”]. Due to FMT being a novel treatment in recent years and a limited number of studies focusing on this topic, no date limitation was applied to the search, with all studies published up until the latest search date (14 May 2021) being considered.
Study participants
Physicians, nurses, medical students, or associated health professions in any kind of healthcare settings globally were included in this systematic review.
Inclusion and exclusion criteria
Different types of studies were included if they were primary research and focused on healthcare providers’ perception of FMT for CDI, rCDI, IBD, UC, Crohn’s disease or CDI and IBD. However, other related gut microbial dysbiosis disease using FMT were excluded. Any reviews, editorials, letters, perspectives, commentaries, reports, and studies with insufficient related data were excluded as well.
Data extraction
Two researchers (YL and KA) independently extracted data into a data extraction template which was pilot tested with two included papers. The authors extracted data after quality assessment to save time and reduce potential selection bias.24 Any disagreements were discussed by the two researchers to reach a consensus and the other two authors were consulted if necessary. The researchers extracted data from each included study as follows: title, the first author, publication year, type of study design, setting, country, the approaches of data collection and analysis, targeted population, the number of participants included in the survey or questionnaires, healthcare providers’ knowledge and attitudes towards FMT.
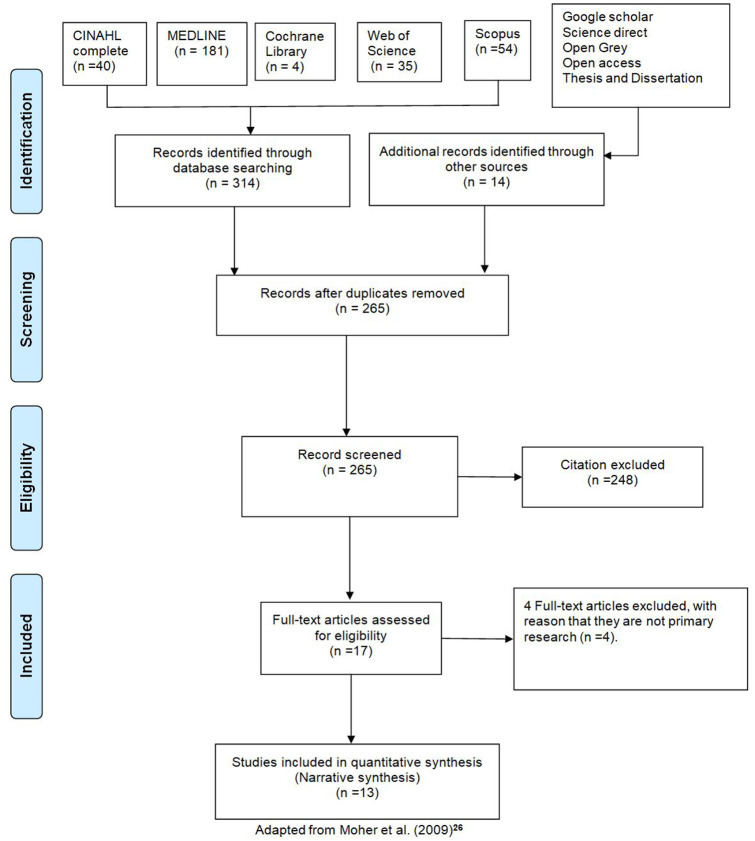
Study screening and selection
The selection process was guided by the PRISMA flow diagram shown in Figure 1. All included studies were selected by following the three-stage screening process; the authors browsed and appraised the titles after removing duplicated studies from different databases; abstracts were assessed to double-check the qualification of those included by title and finally a full-text assessment was implemented to guarantee all inclusion criteria were completely satisfied. The whole process was undertaken with the assistance of Endnote software, which is recommended by Bramer and colleagues.25 The authors YL and YY implemented and recorded the above process, and shared the record with the other authors for confirmation. Disagreements were discussed and solved by consensus.
Figure 1.
PRISMA flow diagram.
Adapted from Moher and colleagues.26
Assessment of quality
Although an interest in perceptions may generally fall within the realm of qualitative research, the literature on FMT for CDI and IBD has exclusively explored this question through quantitative approaches so far, specifically through cross-sectional studies. Quality assessment of these studies was independently carried out by the authors YL and KA who used the quality assessment tool from the Institute for Public Health Sciences.27 This is widely used for appraising descriptive/cross-sectional studies and is suitable for the questionnaire methods employed in the included studies. The other authors were consulted to resolve any discrepancies or disagreements in this process.
Data synthesis and analysis
A narrative synthesis was conducted in this review due to the diversity in the participants’ recruitment, different methodologies and statistical heterogeneity. To conduct the narrative synthesis the present researchers followed four main steps.28 First, the authors organised results in a data extraction table (see Supplemental Appendix 1). Following that, the authors created a theming table to illustrate how themes were generated. The next step was to list results and chunk results into distinct sections. Finally, the authors labelled each section as a category and used categories to discuss results in the review. Through this approach, the present researchers integrated different studies to generate new understandings around healthcare providers’ perceptions of FMT for CDI and IBD rather than simply summarising pre-existing research. This contributed to the high-quality of this research while any discrepancies were discussed to reach consensus among the authors.
Results
Thirteen quantitative studies were included in this review for analysis, which are detailed in Table 1 alongside their bibliographic details and narrative outcomes.
Table 1.
Characteristics of included studies.
| Study ID | Country | Study design | Sample size (SS) and the response rate (RR) | Conclusions |
|---|---|---|---|---|
| Al-Bakri and colleagues29 | Jordan | Cross-sectional study | SS: Healthcare providers n = 300 RR: Not report |
4.3% respondents were familiar with FMT (95%CI = 2%–6.59%). 5% respondents would refer a patient for FMT (95%CI = 2.53%–7.47%). 40% respondents would not perform FMT due to concerns about medical litigation (95%CI = 34.46%–45.54%). Regarding FMT bank, 47.7% were worried about the consent methods (95%CI = 42.05%–53.35%). 38% respondents would not implement FMT due to fear of infection (95%CI = 32.51%–43.49%). |
| Dennis and colleagues30 | Canada | Cross-sectional study | SS: Physicians n = 253 RR: 15% |
More than 60% of respondents described themselves as being ‘not at all’ or ‘somewhat’ familiar with faecal transplantation (FT) (95%CI = 44.62%–75.38%). 76% respondents who had never referred a patient for FT (95%CI = 62.60%–89.40%). 50% respondents would not refer FT due to not knowing where to access FT (95%CI = 34.31%- 65.69%). |
| Jiang and colleagues31 | US | Cross-sectional study | SS: Physicians n = 264 RR = 34% |
86.21% of respondents would refer patients to a FT centres (95%CI = 78.96%–93.46%). |
| Ma and colleagues32 | China | Cross-sectional study | SS: Clinicians n = 150 RR: 66.67% |
36% respondents are highly familiar with and had performed FMT (95%CI = 26.59%–45.41%). 88% (n = 96) respondents would recommend FMT (95%CI = 81.50%–94.50%). 33% (n = 16) respondents would not recommend FMT due to high expectations from patients and pressure on clinical efficacy (95%CI = 9.96–56.04%). Regarding the ethical aspects of FMT banks, 64% clinicians agreed informed consent of donors and 63% privacy protection of personal information (95%CI = 54.06%–72.94%, average level). 19% (n = 16) respondents would not recommend FMT due to infection (95%CI = 0–38.22%). |
| Madar and colleagues33 | Romania | Cross-sectional study | SS: Medical students n = 80 RR: 65% |
34% respondents had at least a medium level of familiarity with FMT (95%CI = 21.12%–46.88%). 98.1% respondents are likely to recommend FMT (95%CI = 94.39%–101.81%) 31% respondents considered donor screening as a complex and expensive process (95%CI = 18.43%–43.57%); 75% respondents thought the transmission of disease undetected by screening procedures was the most worrying adverse effect (95%CI = 63.23%–86.77%). 69% respondents assumed FMT could result in the recipient acquiring an infection from the donor (95%CI = 56.43%–81.57%). |
| Mcilroy and colleagues34 | UK | Cross-sectional study | SS: Gastroenterologists n = 61 RR: Not report |
50% respondents would not consider using FMT due to a lack of strong evidence to support its safety (95%CI = 37.45%–62.55%). |
| Moossavi and colleagues35 | Iran | Cross-sectional study | SS: Physicians n = 217 RR: 98.16% |
68.5% respondents were familiar with FMT (95%CI = 62.26%–74.74%). 88.46% (n = 130) respondents refer their patients for FMT if indicated (95%CI = 82.97%–93.95%). 94.18% (n = 140) respondents were willing to accept FMT if scientifically and ethically approved (95%CI = 90.30%–98.06%). 30.7% (n = 137) respondents had recognised stool preparation as the most unappealing aspect of FMT (95%CI = 22.98%–38.43%). |
| Paramsothy and colleagues36 | Australia | Cross-sectional study | SS: Gastroenterologists n = 52 RR: Not report |
90% respondents would refer FMT for CDI, 37% for UC, 13% for Crohn’s disease and 6% for IBS (95%CI = 33.23%–60.35%, average level) 42% respondents reported a lack of evidence was the most commonly cited concern (95%CI = 28.58%–55.42%). 25% respondents agreed that there was a significant infection risk from donor stool despite screening (95%CI = 13.23%–36.77%). 12% respondents considered infection risk as their greatest concern towards FMT (95%CI = 0–20.83%). |
| Porter and Fogg21 | UK | Cross-sectional study | SS: Physicians n = 162 RR: Not report |
96% believe that the evidence base supports the use of FMT (95%CI = 92.98%–99.02%), and 94% reported consulting on at least one patient a year for whom they would recommend FMT (95%CI = 90.34%–97.66%). 33.6% respondents think a lack of availability of screened faecal solution (95%CI = 25.78%–41.42%) and 9.3% respondents think donor selection inhibits the uptake of FMT (95%CI = 4.49%–14.11%). |
| Ren and colleagues37 | China | Cross-sectional study | SS: Physicians n = 980 RR: 86.1% |
45.6% respondents had an awareness or understanding of FMT (95%CI = 42.24%–48.96%). 79.2% respondents’ greatest concerns regarding FMT were patients’ acceptability (95%CI = 76.46%–81.94%). Most respondents preferred donors who had a similar microbiota environment to the recipient, including blood relatives (50.6%, 95%CI = 47.23%–53.97%), non blood relatives (30.1%, 95%CI = 27.01%–33.19%) and intimate friends (11.9%, 95% CI = 9.71%–14.08%). |
| Stevenson38 | US | Cross-sectional study | SS: Registered nurses n = 4400 RR: 5.36% |
More than half of respondents strongly agreed (n = 24, 10.2%) or agreed (n = 110, 46.6%) in response to “I am familiar with FMT” (95%CI = 31.32%–47.88%). In the education group, 46.5% nurses agreed that FMT could cause transmission of infection (95%CI = 40.14%–52.86); 42.3% nurses in the all other practice setting agreed with this opinion (95%CI = 36%–48.60%) and 36.8% in the Acute Care group (95%CI = 30.65%–42.95%). |
| Wu and colleagues39 | China | Cross-sectional study | SS: Medical students n = 2113 RR: 86.51% |
38.2% respondents had high-level recognition of FMT (95%CI = 35.97%–40.43%). The main justifications for respondents not supporting FMT were limited reported clinical evidence (67.94%, 95%CI = 65.80%–70.80%). 73.69% participants were willing to donate their faces (95%CI = 71.67%–75.71%), while only 26.31% were unwilling or uncertain about it (95%CI = 24.91%–28.33%). |
| Zipursky and colleagues40 | USA | Cross-sectional study | SS: Physicians n = 139 RR: 97% |
95% participants were generally aware of FMT as a treatment modality (95%CI = 91.32%–98.68%) and 24% indicated they were very informed about FMT (95%CI = 16.80%–31.20%). 65% participants had neither offered nor referred a patient for FMT (95%CI = 56.95%–73.05%). 33% participants not offering or referring a patient for FMT was mainly due to not having an appropriate clinical situation (95%CI = 25.07%–40.93%). |
CDI, Clostridioides difficile infection; CI, confidence interval; FMT, Faecal Microbiota Transplantation; FT, faecal transplantation; IBS, irritable bowel syndrome; RR, Response rate; SS, Sample size; UC, Ulcerative Colitis; UK, United Kingdom; US, United States.
General characteristics
Languages, publication dates and countries
All included studies were in English and published between 2013 and 2020. Three studies were carried out in China and another 10 studies were conducted in other countries spanning Europe, North America, Jordan, Australia and Asia as shown in Table 1.
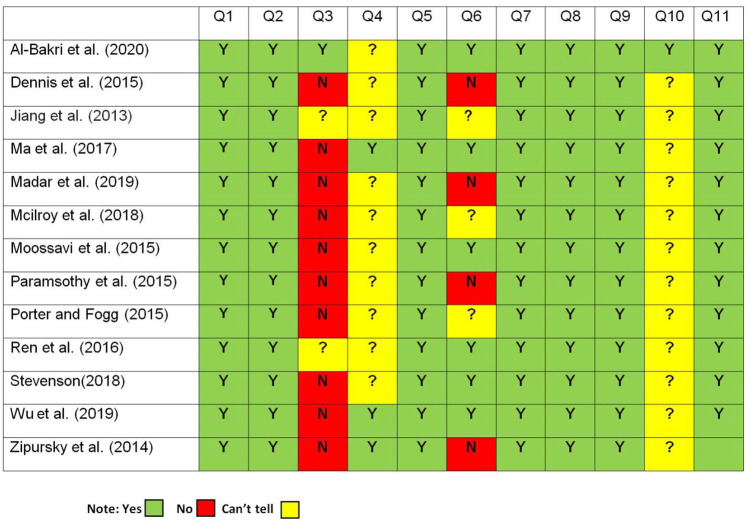
Study design, participants, questionnaires’ design and quality of included studies
All thirteen included studies were cross-sectional studies; four studies were conducted via field survey, while another nine studies were carried out via the Internet or e-mail. As shown in Table 1, the targeted population was varied among the included studies, six studies focused on physicians, two studies focused on gastroenterologists, one study focused on healthcare providers, one study focused on clinicians (clinicians are all healthcare providers who directly treat patients, while physicians are clinicians who focus in a particular specialty involving non-surgical treatment), one study focused on registered nurses, two studies focused on medical students. All these participants could be classified as healthcare providers. A total of 9171 baseline questionnaires were distributed, while 4110 valid questionnaires were returned with an overall return rate of 44.82% and the range for the return rate of questionnaires was from 5.36% to 98.16%.
Due to there being no validated survey instruments assessing healthcare providers’ perception regarding FMT available, seven studies used self-designed questionnaires. Another two studies’ questionnaires were adapted from Ma and colleagues because they had similar research objectives, but there was no information about the questionnaire design in another four studies. However, among thirteen included studies, only three studies pilot tested their questionnaires before distribution, while another ten studies did not describe whether they tested their questionnaires before distribution. The present authors used the 11 questions included in the Institute for Public Health Sciences tool to appraise the quality of included studies; the detailed questions are presented in Table 2 and the quality assessment of each included study is shown in Figure 2.
Table 2.
11 questions to help you make sense of descriptive cross-sectional studies.
| Screening Questions | |
| 1. Did the study address a clearly focused issue? | Yes Can’t tell No |
| 2. Did the authors use an appropriate method to answer their question? | Yes Can’t tell No |
| Detailed Questions | |
| 3. Were the subjects recruited in an acceptable way? | Yes Can’t tell No |
| 4. Were the measures accurately measured to reduce bias? | Yes Can’t tell No |
| 5. Were the data collected in a way that addressed the research issue? | Yes Can’t tell No |
| 6. Did the study have enough participants to minimise the play of chance? | Yes Can’t tell No |
| 7. How are the results presented and what is the main result? | Yes Can’t tell No |
| 8. Was the data analysis sufficiently rigorous? | Yes Can’t tell No |
| 9. Is there a clear statement of findings? | Yes Can’t tell No |
| 10. Can the results be applied to the local population? | Yes Can’t tell No |
| 11. How valuable is the research? | Yes Can’t tell No |
Adapted from Institute for Public Health Sciences.27
Figure 2.
Quality criteria assessment for references 21 and 29-40.
The answer to Q1 and Q2 among all the included studies were Yes (see Figure 2), thus, according to Institute for Public Health Sciences, it was worth proceeding with the remaining questions. Q3 assessed the selection bias of each study, which could be evaluated by assessing the sample. Q4 checked the measurement bias and it could be assessed by whether the researchers used subjective or validated measurements in the studies. Q5 assessed whether the researchers collected data in a correct and justified way. Q6 aimed to explore whether the result of each included study was precise. Q7 regarded how results were presented in each study, which will be assessed in the results section. Q8 was about the studies’ analysis process and whether in-depth description was provided or whether there was insufficient data to support the findings. Q9 focused on whether the researchers offered adequate discussion of the evidence and the reliability of their findings. Q10 aimed to explore the applicability of the research, which was considered through examining the similarities between research subjects and contexts to other settings. The last question was about the contribution of the studies. As Figure 2 shows, the overall quality of the included studies was assessed as ‘good’. The main issues among the included studies were selection and measurement bias. Future studies would not only benefit from larger sample sizes and the validation of questionnaires to enhance reliability and generalisation, but also employing qualitative research approaches to understand perceptions in more depth.
Results and synthesis
Familiarity with FMT
Nine studies mentioned this topic, and the detailed description is presented in Table 1. In total 3746 participants responded and the overall level of their familiarity with FMT was 39.43%. Among these nine studies, the highest percentage of them was Iranian physicians who reported a 68.5% familiarity rate, while the lowest was Jordanian healthcare providers who reported a 4.3% familiarity rate. The average familiarity with FMT of Chinese respondents was 40.37% which exceeds the average level. There appeared to be difference in familiarity between different healthcare workers, with nurses reporting a familiarity rate of 56.77%, doctors 46.21% and medical students 38.09%. From the included studies, it seems that age, gender, educational level, professional title, practice setting, working experience, specialty, health status, university, ethics and culture may influence healthcare providers’ familiarity with FMT, while the reason behind this phenomenon will be explored in the discussion section.
Readiness to recommend FMT to patients
Nine included studies’ outcomes referred to the readiness to recommend FMT to patients. As Table 1 outlines, a total of 1141 participants responded with the readiness to recommend FMT to patients and the global average level was 58.81%. Compared with the global average level of familiarity with FMT, healthcare providers’ readiness to recommend FMT to patients was higher (39.43% vs 58.81%). In all, 98.1% of Romanian third-year medical students were likely to recommend FMT, but only 9.6% would utilise it as the first line treatment. However, only 5% of Jordanian physicians would refer their patients for FMT. Compared with other countries included in this review, Jordanian physicians have the lowest level of knowledge of FMT and readiness to recommend it to patients. Differences in theoretical and practical focus between medical students and physicians may be causing the differences in their readiness to recommend FMT, however more certain reasons would need to be explored in future studies.
Greatest concerns regarding FMT
Nine included studies assessed the greatest concerns regarding FMT from healthcare providers’ perspectives. Each included study used percentages to narrow down the greatest concerns and apply descriptive statistics to analyse data. Three out of nine included studies reported that the greatest concern regarding FMT was lacking clinical evidence to support its safety. However, Dennis and colleagues reported that they would not refer FT due to not knowing where to access FT, whose conclusion was similar to Zipursky and colleagues’s study. It is likely that access and knowledge of accessing FT have improved since these early studies as interest in FMT has grown. Compared with the previous five studies, Ma and colleagues pointed out that high expectations from patients and pressure on clinical efficacy were the greatest concerns towards FMT from Chinese clinicians. Ren and colleagues stated that acceptability to patients (79.2%) was the major concern of FMT from Chinese physicians’ perspective. Similarly, another study carried out by Wu and colleagues also reported that 36.71% of Chinese medical students did not support FMT due to lack of analysis of patients’ willingness or cost-effectiveness. The findings from these studies suggest that patients’ perceptions and expectations regarding FMT are significantly important for its application and popularity in China, while the clinical efficacy and appropriate clinical situation of FMT is relatively more important in other countries. However, further research needs to be conducted to confirm this suggestion.
Donor screening procedures
In total six included studies and 3176 participants responded to the donor screening procedure; however, their perspectives were different. Two studies referred to FMT banks and emphasised the consent of donors, and two studies showed their concerns regarding the infection risk from donor stool. Compared with the above perspectives, 30.7% of Iranian physicians assumed that stool preparation was the most unappealing aspect of FMT. Chinese physicians preferred donors who had a similar microbiota environment to the recipient, and 73.69% Chinese postgraduate medical students were willing to donate their faeces.
Causing the transmission of infection
From the data in Table 1, it is apparent that the overall level of 40.43% of respondents would not implement FMT due to infection concerns. This varied between professions, however: 33.42% of doctors, 41.96% of nurses and 69% of medical students would not implement FMT due to these concerns.
Discussion
Summary of the main results
The purpose of the current review is to evaluate healthcare providers’ perception of FMT with IBD and CDI. The thirteen included studies include perspectives from healthcare providers in eight different countries. Among them, six studies were conducted in developing countries, while seven studies were undertaken in developed countries. All major outcomes are illustrated in the summary of the findings table which is presented in Table 3. The overall rate given in Table 3 was calculated by dividing the overall number of people responding the topic by the total number of valid respondents.
Table 3.
Summary of the findings.
| Outcomes | Conclusion | 95%CI | Number of studies |
|---|---|---|---|
| Familiarity with FMT | 39.43% (the overall level, N = 3746) healthcare providers were familiar with FMT. | 37.87%–41% | Nine observational studies |
| Readiness to recommend FMT to patients | 58.81% (the overall level, N = 1141) healthcare providers were willing to recommend FMT to their patients. | 55.95%–61.67% | Nine observational studies |
| Greatest concerns regarding FMT | 66.67% (the overall level, N = 1941) healthcare providers considered that lacking clinical evidence was the greatest concerns regarding FMT. | 64.57%–68.77% | Nine observational studies |
| Donor screening procedures | Healthcare providers’ perspectives regarding donor screening procedures were different, thus it was difficult to calculate the overall level. | Unclear | Seven observational studies |
| Causing the transmission of infection | 40.43% (the overall level, N = 1128) healthcare providers would not implement FMT due to infection. | 37.57%–43.29% | 5 observational studies |
CI, confidence interval; FMT, faecal microbiota transplantation.
Contributions to the literature
Familiarity with FMT
Despite the 7-year time-range of included studies, the results of the present review’s consistently suggests that the overall level of familiarity with FMT among healthcare providers is low. One possible implication of this is that healthcare providers’ familiarity with FMT has not changed much despite the various advances that have been made in FMT. Ren and colleagues found that geographical region was an essential factor impacting their knowledge of FMT and this was also evident in this review. This phenomenon may be caused by the dissimilarity of the economy, the frequency of information exchange and the unequal allocation of medical resources, which can impact public acceptance and the speed of spreading new knowledge and technology.37 Meanwhile, this review also found that ethics and culture are important elements of the geography of healthcare providers’ FMT knowledge as discussed later.
Furthermore, healthcare providers’ familiarity with FMT may positively influence their willingness to perform it. As found in other studies, Sofi and colleagues41 reported that the lack of knowledge of FMT was the principal reason for their respondents not considering FMT. However, the familiarity with FMT does not guarantee healthcare providers are willing to experience it. Zipursky and colleagues argued that 100% of respondents in their survey treated rCDI, but only 20% chose FMT. This is similar to another study who reported that 40% of physicians had heard of FMT but were reluctant to try it.42 More surprisingly, a survey conducted by Stevenson revealed that registered nurses’ knowledge and perception of FMT were irrelevant to their age, education, years of experience and practice setting.
However, compared with Stevenson’s finding, Ren and colleagues found that age, educational level, professional title, practice setting and working experience could influence physicians’ knowledge. Similarly, Wu and colleagues reported that gender, speciality, university and health status can also affect postgraduate medical students’ recognition level of FMT. However, other included studies did not analyse whether these confounding factors influenced the targeted population’s knowledge. Consequently, it is difficult to draw a conclusion from current evidence of whether there is a relationship between healthcare providers’ knowledge and these variants. Overall, healthcare providers have poor health literacy towards FMT, thus, it is urgent to improve their knowledge in the future.
Readiness to recommend FMT to patients
This review suggests that healthcare providers’ knowledge directly influences their attitudes towards FMT. Compared with other countries, Iranian physicians have the highest-level knowledge of FMT and their readiness to recommend it to patients is relatively higher. The most likely cause of this phenomenon was educational monthly seminars which were held by the Iranian Association of Gastroenterologists and Hepatologists.35 Similarly, Wu and colleagues reported that Nanjing Medical University students have the highest rate of familiarity with FMT in this review, possibly due to the leading FMT centre and the Chinese FMT Bank being supported by this university. Thus, compared with other medical students, they may have more chance and medical resources to understand FMT. This also can explain why students in this university are more willing to donate faeces. Interestingly, Madar and colleagues indicated that low familiarity with FMT of Romania medical students owed to inadequate exposure through lack of lectures focusing on FMT. Consequently, education would appear to be an effective strategy to improve healthcare providers’ knowledge and attitudes towards FMT.
By contrast, Jordanian healthcare providers have the lowest familiarity with FMT and the most negative attitudes towards it. Two possible reasons for this consequence are ethics and cultural aspect. With regard to ethical issues, Al-Bakri and colleagues reported that most respondents were doubtful and not supportive of performing FMT method. Similarly, Ma and colleagues revealed that 43% of clinicians believed patients who undertook FMT may feel shame or degradation of dignity. When it comes to cultural factors, 52% of respondents pointed out religion as the possible cause of it impacting their choice of using FMT.29 Most people in Jordan are Muslim; it is significantly important to obey the religious commitment to halal non-alcoholic foods and beverages.29 Likewise, Ontario physicians shared similar attitudes towards FMT and 76% respondents would not recommend it to patients, the most common reason being insufficient awareness of where to access the treatment.30 Similarly, Zipursky and colleagues found that 65% respondents had not recommended FMT due to lacking the right clinical situation to perform FMT, which is in accordance with Dennis and colleagues. These results would seem to suggest that healthcare providers’ readiness to recommend FMT to patients may improve with their knowledge of FMT increasing and FMT’s wider application.
Meanwhile, the unpleasant nature of FMT is another barrier for healthcare providers in recommending it to their patients.30,40,41 However, according to Brandt, physicians’ reluctance to recommend FMT to patients is due to the inadequate number of randomised controlled trials to demonstrate its efficacy and safety.43 This is congruent with Xu and colleagues who reported that clinical effectiveness is a significantly important factor to determine patients’ positive attitudes regarding FMT and physicians’ readiness to recommend it.44 However, a growing body of evidence has reported the safety and effectiveness of FMT. A study by Hota and Poutanen45 showed that FMT was an effective treatment to rCDI, and multiple FMT could achieve better patient outcomes than single FMT. Similarly, a prospective real-world study by Kelly and colleagues also suggested that FMT was highly effective and secure for CDI,46 which was consistent with the conclusion from a systematic review by Moayyedi and colleagues.47
Furthermore, a cohort study reported that the overall cure rate of CDI was high and most IBD patients acquired clinical improvement after FMT, and they found no severe adverse events directly contributed to FMT.48 Meanwhile, a case report suggested that FMT could effectively improve Crohn’s colitis patients’ clinical, endoscopic, and histological symptom,49 while FMT could also be significantly effective for active UC patients.50 Similarly, Paramsothy and colleagues indicated that 90% of Australian gastroenterologists would recommend FMT to CDI patients, while 37% for UC and 13% for CD patients. Furthermore, a national survey conducted by Mcilroy and colleagues reported that 38% respondents had implemented FMT on CDI patients, while 34% would consider utilising FMT on IBD patients. It could be concluded that healthcare providers’ perception towards FMT may change with increased evidence to support its safety and efficacy in CDI and IBD. However, not all of this evidence was available when the studies included in this review surveyed their participants, and therefore, may not have impacted on the perceptions reported here.
In conclusion, it seems that the limited knowledge, insufficient practising experience, unappealing nature of FMT and clinical efficacy may directly impact healthcare providers’ readiness to recommend it. It also appears that healthcare providers’ readiness to recommend would improve with their knowledge increasing and FMT’s wider implication. Meanwhile, this review also suggests that ethical and cultural factors also need to be considered and the most effective educational style for enhancing FMT knowledge needs to be explored in the future.
Greatest concerns regarding FMT
Clinical efficacy and safety of FMT are the leading concerns among healthcare providers in this review, whose conclusion was consistent with the statement in the NICE’s 2021 guideline.51 Several factors play a role in determining this phenomenon. First, FMT is a novel therapy that is short of substantial clinical evidence to demonstrate its safety and effectiveness with the related disease, and only rCDI was written into the NICE’s 2014 guideline.39 Second, no worldwide and standardised FMT procedure is available, including donor selection, laboratory preparation and delivery approaches.33,39 However, a prospective survey-based study revealed that FMT was safe for long-term rCDI.52 With efficacy varying with indication, healthcare providers’ perception may also vary based on indications. Consequently, future research should focus more on exploring FMT’s safety and effectiveness, and standard treatment protocols also need to be developed.
However, apart from the clinical effectiveness and safety of FMT, patients’ acceptability is another most common consideration for the therapeutic application of FMT. The possible reasons are the ‘yuck factor’ or the cleanliness/hygiene of the faecal matter.22,30,32 Consequently, to enhance patients’ acceptance, the FMT delivery route is essential. Compared with the upper GI tract, the lower GI tract is more acceptable by most patients.22,32 The upper GI route consists of gastroduodenoscopy, nasointestinal tube and oral capsule, while the lower GI route includes colonoscopy and retention enema.37 To date, the optimal method is still unclear, but a systematic review reported that rCDI had a higher cure rate by FMT via colonoscopy than other routes.53 Brandt and Aroniadis found that approximately 75% of FMT for patients with rCDI are conducted through the lower GI tract, while 25% through the upper GI tract.54 Similarly, previous studies by Madar and colleagues and Paramsothy and colleagues revealed that colonoscopy was the most preferred routes for healthcare providers performing FMT. However, according to Chuong and colleagues, social stigma or concerns regarding facing stigma towards FMT is another factor which can impact its acceptance.55 In such circumstance, social media should not exaggerate or underestimate the efficacy of FMT.32 The conclusion can be drawn from these findings that enhancing social acceptance is crucial for FMT’s future application.
Donor screening procedures
Due to there being no international regulatory or common legal framework regarding the donation of human faecal available,56 different studies and guidelines hold different opinions towards FMT donor screening procedure. According to Ma and colleagues, FMT is more like blood donation rather than organ donation. Thus, different stool banks agreed that the pathogens included in the blood-screening programme should be consistent with the screening procedure for blood donors.57,58
However, a recent consensus guideline released by Australian experts suggested that stool donors should be screened with a careful history together with blood and stool testing, and should test Multi Drug Resistant Organisms (MDROs) as well.59 Cammarota and colleagues hold a similar view in the European consensus conference; they stated that healthcare workers should be paid more attention as potential donors because they possibly have greater chance to transmit MDROs.57 Experts have seemingly reached the consensus of testing MDROs in donor screening, which can provide valuable clues for updating the NICE guideline to some extent. However, with the outbreak of coronavirus disease 2019 (COVID-19), an international expert panel published an urgent suggestion for screening FMT donors.60 In this statement, Ianiro and colleagues suggested that FMT donors should be also screened for the presence of typical COVID-19 symptoms (e.g. fever, fatigue, dry cough, myalgia, dyspnoea, and headache), travel and close contact history within the previous 30 days. In conclusion, further research is needed on stool donor screening procedure, especially test donors’ MDROs and COVID-19.
In addition, healthcare providers should also consider religion, culture and diets in donor screening processes. This argument is supported by Al-Bakri and colleagues and Bokek-Cohen and Ravitsky.61 Islam is the predominant religion in Jordan,29 and Muslim patients might have a strong prohibition to receive a faecal transplant from non-Muslim donors.32 Similarly, kosher requirements for some Jews and vegetarian requirements for some Buddhists or Hindus may need consideration.61 This phenomenon may result from recipients considering FMT as the ingestion of a derivative of food which they consider as forbidden, thus they may have a strong emotional rejection to receive a sample from these donors.61 Although consent is a standard of care for FMT in most centres, healthcare providers should consider such religious or cultural factors when obtaining consent from recipients before performing FMT, especially the samples from unknown donors.
A recent international consensus conference reported that stool banks may offer trustworthy, timely and equal access to FMT for patients and a traceable procedure which can guarantee its safety and quality.62 However, ethical issues regarding stool donors should also be given further consideration, including informed consent guidelines for stool banks and the privacy of stool donors.63 To recruit and retain more donors, the organisers should motivate and express gratitude to them, and highlight their positive influence on FMT research.63 Therefore, healthcare providers should consider the challenges and concerns with stool banks when conducting FMT.
Nonetheless, in terms of the donor screening criteria, it should comply with the national regulatory guidelines or follow the most updated international expert consensus.56 To select a healthy, stable and diverse faecal microbiota donor, age, weight criteria, healthy lifestyle and no antibiotic use within a certain period before donation should be considered as well.56 Cammarota and colleagues hold a similar viewpoint which was presented in the European consensus conference, in which they summarised the donor selection procedure. In the preliminary stage, donors’ medical history, lifestyle habits, age and medication history should be considered, while on the day of donation, donors’ recent history, risk factors of selected and their laboratory outcomes also need to be checked.57
In summary, the current evidence suggests that age, medical history, religion and cultural background, lifestyle habits, medication history, informed consent, and clinical testing (e.g. MDROs) should be taken into consideration when developing the donor screening procedure.
Causing the transmission of infection
As presented in this review, infection is one of the most common concerns regarding side effects of FMT, yet, the perceived risk may outstrip actual risk here; FMT seemed safe and the rate of infection transmission was low.52,64 However, there are other side effects as well, including physical detrimental events (e.g. fever and abdominal disorder)64 and mental illness (anxiety and depression).65,66 Therefore, strict donor screening is an effective strategy to reduce this potential risk. However, Dennis and colleagues found that no physicians agreed that FMT could cause transmission of infection. This phenomenon may have been attributed to many hospitals in Canada having not performed FMT and this study having been carried out before publication of a randomised controlled trial (RCT) on FMT, thus Ontario physicians could not predict the side effects of FMT. It seems possible that over time, healthcare providers have become more concerned about the transmission of infection with FMT.
Apart from stricter donor screening, exploring a standardised procedure of collection, preparation and storage of faecal samples is also significantly important to reduce infection. In terms of the faecal sample, faeces should preferably be collected in a specific single-use container in the stool bank.62 Meanwhile, to guarantee the quality, faecal samples should be manipulated and stored within 6 hours after defaecation in the stool bank.62 Furthermore, every faecal sample is marked with a unique bar code to provide efficient donor-recipient trace back.67 Finally, to assess potential infection after FMT, Gliklich and colleagues indicated that prospective registries recruiting large cohorts of recipients with long-term follow-up are the only practical approach to achieve this purpose.68 In summary, effectively controlling possible infection is essential to ensure FMT safety and enhance patients’ satisfaction in clinical practice.
In conclusion, this section has discussed that healthcare providers’ knowledge and attitudes can be improved through education, while stricter donor screening procedures can effectively prevent infection and enhance clinical safety. Most patients experienced diarrhoea and constipation in the short-term follow-up after FMT, while 13% had gastrointestinal discomfort, 10% weight gain, and 11.8% new infections (all considered irrelevant to FMT) in the long-term follow-up.52 Therefore, as a novel and promising therapy, more research is required to examine the long-term efficacy and safety of FMT.
Limitations
Several limitations exist in the present review. First, due to time and language limitations, the authors only extracted data from studies published in English which may lead to language bias. Second, although the authors attempted to search as many as papers through several different databases, grey literature and manual searching, there was no qualitative evidence that focused on this review topic and the existing evidence was limited. Third, the small number of studies is also limits our evaluation of factors which may affect healthcare providers’ perceptions. The main reason for this phenomenon may contribute to FMT being underused present and most studies only focusing on exploring its long-term efficacy and safety. Thus, few studies pay attention to the topic of this review. Finally, the questionnaires used in the included studies were varied, thus outcomes were heterogeneous and conducting meta-analysis was not suitable. All these weaknesses may impact the robustness of the review outcomes. Consequently, in the future, it is necessary to conduct qualitative research to explore this topic in greater depth, which could be useful in understanding these issues more deeply, and also create an internationally recognised and validated questionnaire on this topic.
Conclusion
This report was the first systematic review that focused on healthcare providers’ perception and attitudes towards FMT with CDI and IBD, whose outcomes were valuable for FMT application and popularity, and have highlighted various avenues for future FMT research more widely. Through a comprehensive literature search, the critical appraisal of included studies, data extraction and narrative synthesis, five major outcomes were synthesised from thirteen cross-sectional studies to achieve the objective of this review. The familiarity with FMT and healthcare providers’ readiness to recommend it could provide insight into their knowledge and attitudes of FMT with CDI and IBD, while donor screening procedures, greatest concerns regarding FMT and its potential transmission of infection could provide useful information towards the further improvements for FMT in the future.
We found that the overall level of healthcare providers’ knowledge towards FMT is still low, while education may be an effective strategy to improve it. To enhance their recognition of FMT, strengthening the professional training of FMT together with positive portrayal within mainstream media may have a positive effect. In terms of educating medical students, medical lectures, classroom teaching and social media are effective ways. However, the mass media and mainstream media should neither exaggerate nor underestimate the function of FMT, which may mislead the public.
Over time, readiness to recommend FMT seems to have increased, which may be a result of increasing interest, evidence and guidelines surrounding its use. However, to enhance healthcare providers’ willingness to recommend FMT, apart from increasing their knowledge and practising experience, optimising stool preparation and reinforcing FMT clinical efficacy, ethics and cultural components also need to be considered. Furthermore, knowledge had a positive influence on healthcare providers’ attitudes towards FMT. The evidence from this review implies that education is the best strategy to improve healthcare providers’ knowledge and willingness to recommend FMT, thus future practice should be taken into consideration to explore the most effective education time and methods.
This review demonstrates that clinical efficacy and safety are still the most significant concerns for healthcare providers. Therefore, future practice should focus on seeking a larger sample size RCT to demonstrate FMT’s long-term efficacy and safety. This review has found concerns about infection transmission, while strict donor screening procedures are crucial to reducing this risk. Despite different healthcare providers holding different perspectives towards donor screening procedures, an increasing number of experts have reached the consensus of testing MDROs in donor screening which can provide some valuable information for future research. However, healthcare providers should also consider donors’ age, medical history, religion and cultural background, lifestyle habits, medication history, informed consent, and clinical testing. In summary, future practice should emphasise investigating an international standard donor screening procedure.
In conclusion, as a novel treatment, FMT has a long way to proceed to achieve wide application and popularity. The most urgent strategies include improving healthcare providers’ knowledge, demonstrating its long-term efficacy and safety, and designing an international standard donor screening procedure.
Supplemental Material
Supplemental material, sj-xlsx-1-tag-10.1177_17562848211042679 for Healthcare providers’ perception of faecal microbiota transplantation with clostridium difficile infection and inflammatory bowel disease: a quantitative systematic review by Yanghua Liu, Kal Alnababtah, Simon Cook and Ying Yu in Therapeutic Advances in Gastroenterology
Footnotes
Author contributions: Kal Alnababtah and Yanghua Liu designed the study. Yanghua Liu drafted the manuscript; Ying Yu, Kal Alnababtah and Simon Cook were involved in the revision of the manuscript. Yongjian Zhou and Yong Lin provided professional consultation; Alice May offered language support. Yanghua Liu and Helen Ryba were responsible for literature retrieval. Kal Alnababtah supervised data collection and analysis. All of the authors have read and approved the final version of this manuscript.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author(s) received financial support for the research, authorship, and/or publication of this article from Guangzhou First People’s Hospital, School of Medicine, South China University of Technology, China.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Yanghua Liu  https://orcid.org/0000-0002-9618-8196
https://orcid.org/0000-0002-9618-8196
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Yanghua Liu, Department of Nursing, Guangzhou First People’s Hospital, School of Medicine, South China University of Technology, Guangzhou, China; Faculty of Health, Education and Life Sciences, Birmingham City University, Birmingham, UK.
Kal Alnababtah, Faculty of Health, Education and Life Sciences, Birmingham City University, Birmingham, UK.
Simon Cook, Faculty of Health, Education and Life Sciences, Birmingham City University, Birmingham, UK.
Ying Yu, Department of Nursing, Guangzhou First People’s Hospital, School of Medicine, South China; University of Technology, Guangzhou 510180, Guangdong Province, China.
References
- 1.Balsells E, Shi T, Leese C, et al. Global burden of Clostridium difficile infections: a systematic review and meta-analysis. J Glob Health 2019; 9: 010407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Clostridioides difficile. Atlanta, GA: Department of Health and Human Services, https://www.cdc.gov/drugresistance/pdf/threats-report/clostridioides-difficile-508.pdf (2019, accessed 7 August 2020). [Google Scholar]
- 3.Public Health England. Quarterly epidemiological commentary, mandatory MRSA, MSSA, Gram-negative bacteraemia and C. difficile infections data (up to October to December 2019). London: PHE Publications, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/871239/Quarterley_Epi_Commentary_March_2020.pdf (2020, accessed 7 August 2020). [Google Scholar]
- 4.Xu Q, Chen Y, Gu S, et al. Hospital-acquired Clostridium difficile infection in Mainland China: a seven-year (2009–2016) retrospective study in a large university hospital. Sci Rep 2017; 7: 9645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2017; 390: 2769–2778. [DOI] [PubMed] [Google Scholar]
- 6.Rizzello F, Spisni E, Giovanardi E, et al. Implications of the westernized diet in the onset and progression of IBD. Nutrients 2019; 11: 1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NHS. Inflammatory bowel disease, https://www.nhs.uk/conditions/inflammatory-bowel-disease/ (2020, accessed 7 August 2020).
- 8.Bowel Disease Research Foundation. Inflammatory bowel disease (IBD), https://bdrf.org.uk/bowel-disease/ibd/ (2019, accessed 7 August 2020).
- 9.Dahlhamer JM, Zammitti EP, Ward BW, et al. Prevalence of inflammatory bowel disease among adults aged⩾ 18 years – United States, 2015. Morb Mortal Wkly Rep 2016; 65: 1166–1169. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan GG.The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol 2015; 12: 720–727. [DOI] [PubMed] [Google Scholar]
- 11.Kelsen JR, Kim J, Latta D, et al. Recurrence rate of Clostridium difficile infection in hospitalized pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis 2011; 17: 50–55. [DOI] [PubMed] [Google Scholar]
- 12.Razik R, Rumman A, Bahreini Z, et al. Recurrence of Clostridium difficile infection in patients with inflammatory bowel disease: the RECIDIVISM study. Am J Gastroenterol 2016; 111: 1141–1146. [DOI] [PubMed] [Google Scholar]
- 13.Czepiel J, Dróżdż M, Pituch H, et al. Clostridium difficile infection: review. Eur J Clin Microbiol Infect Dis 2019; 38: 1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borody TJ, Khoruts A.Fecal microbiota transplantation and emerging applications. Nat Rev Gastroenterol Hepatol 2012; 9: 88–96. [DOI] [PubMed] [Google Scholar]
- 15.Gough E, Shaikh H, Manges AR.Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis 2011; 53: 994–1002. [DOI] [PubMed] [Google Scholar]
- 16.Landy J, Al-Hassi HO, McLaughlin SD, et al. Review article: faecal transplantation therapy for gastrointestinal disease. Aliment Pharmacol Ther 2011; 34: 409–415. [DOI] [PubMed] [Google Scholar]
- 17.McDonald LC, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 2018; 66: e1–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson JL, Edney RJ, Whelan K.Systematic review: faecal microbiota transplantation in the management of inflammatory bowel disease. Aliment Pharmacol Ther 2012; 36: 503–516. [DOI] [PubMed] [Google Scholar]
- 19.Palmer R.Fecal matters. Nat Med 2011; 17: 150–152. [DOI] [PubMed] [Google Scholar]
- 20.Holmes E, Li JV, Marchesi JR, et al. Gut microbiota composition and activity in relation to host metabolic phenotype and disease risk. Cell Metab 2012; 16: 559–564. [DOI] [PubMed] [Google Scholar]
- 21.Porter RJ, Fogg C.Faecal microbiota transplantation for Clostridium difficile infection in the United Kingdom. Clin Microbiol Infect 2015; 21: 578–582. [DOI] [PubMed] [Google Scholar]
- 22.Kahn SA, Vachon A, Rodriquez D, et al. Patient perceptions of fecal microbiota transplantation for ulcerative colitis. Inflamm Bowel Dis 2013; 19: 1506–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zipursky JS, Sidorsky TI, Freedman CA, et al. Patient attitudes toward the use of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection. Clin Infect Dis 2012; 55: 1652–1658. [DOI] [PubMed] [Google Scholar]
- 24.Boland A, Cherry MG, Dickson R.Doing a systematic review: a student’s guide. 2nd ed. Los Angeles, CA: SAGE, 2017. [Google Scholar]
- 25.Bramer WM, Rethlefsen ML, Kleijnen J, et al. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev 2017; 6: 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264–269. [DOI] [PubMed] [Google Scholar]
- 27.Institute for Public Health Sciences. 11 questions to help you make sense of descriptive/cross-sectional studies. New York: Yeshiva University, http://reache.files.wordpress.com/2010/03/cross-sectional-appraisal-tool.pdf (2002, accessed 9 August 2020). [Google Scholar]
- 28.Popay J, Roberts H, Sowden A, et al. Developing methods for the narrative synthesis of quantitative and qualitative data in systematic reviews of effects. York: Centre for Reviews and Dissemination, 2006. [Google Scholar]
- 29.Al-Bakri AG, Akour A, Al-Delaimy WK.Knowledge, attitudes, ethical and social perspectives towards fecal microbiota transplantation (FMT) among Jordanian healthcare providers. BMC Med Ethics 2021; 22: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dennis M, Salpeter MJ, Hota S.Low awareness but positive attitudes toward fecal transplantation in Ontario physicians. Can J Infect Dis Med Microbiol 2015; 26: 30–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiang ZD, Hoang LN, Lasco TM, et al. Physician attitudes toward the use of fecal transplantation for recurrent Clostridium difficile infection in a metropolitan area. Clin Infect Dis 2013; 56: 1059–1060. [DOI] [PubMed] [Google Scholar]
- 32.Ma Y, Yang J, Cui B, et al. How Chinese clinicians face ethical and social challenges in fecal microbiota transplantation: a questionnaire study. BMC Med Ethics 2017; 18: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Madar PC, Petre O, Baban A, et al. Medical students’ perception on fecal microbiota transplantation. BMC Med Educ 2019; 19: 368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mcilroy JR, Nalagatla N, Hansen R, et al. Faecal microbiota transplantation as a treatment for inflammatory bowel disease: a national survey of adult and paediatric gastroenterologists in the UK. Frontline Gastroenterol 2018; 9: 250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moossavi S, Salimzadeh H, Katoonizadeh A, et al. Physicians’ knowledge and attitude towards fecal microbiota transplant in Iran. Middle East J Dig Dis 2015; 7: 155–160. [PMC free article] [PubMed] [Google Scholar]
- 36.Paramsothy S, Walsh AJ, Borody T, et al. Gastroenterologist perceptions of faecal microbiota transplantation. World J Gastroenterol 2015; 21: 10907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ren RR, Sun G, Yang YS, et al. Chinese physicians’ perceptions of fecal microbiota transplantation. World J Gastroenterol 2016; 22: 4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stevenson E.Registered nurses’ knowledge and perception of fecal microbiota transplantation. PhD Dissertation, Kean University, Union, NJ, https://search.proquest.com/openview/6e3f429fff761553ccd3b406da7a231e/1?pq-origsite=gscholar&cbl=18750&diss=y (2018, accessed 9 August 2020). [Google Scholar]
- 39.Wu X, Dai M, Buch H, et al. The recognition and attitudes of postgraduate medical students toward fecal microbiota transplantation: a questionnaire study. Therap Adv Gastroenterol 2019; 12: 1756284819869144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zipursky JS, Sidorsky TI, Freedman CA, et al. Physician attitudes toward the use of fecal microbiota transplantation for the treatment of recurrent Clostridium difficile infection. Can J Gastroenterol Hepatol 2014; 28: 319–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sofi AA, Georgescu C, Sodeman T, et al. Physician outlook toward fecal microbiota transplantation in the treatment of Clostridium difficile infection. Am J Gastroenterol 2013; 108: 1661–1662. [DOI] [PubMed] [Google Scholar]
- 42.Kelly C, de Leon L, Kerstetter D, et al. Barriers to greater utilization of fecal bacteriotherapy for chronic Clostridium difficile infection. Am J Gastroenterol 2010; 105: S135–S136. [Google Scholar]
- 43.Brandt LJ.Editorial commentary: fecal microbiota transplantation: patient and physician attitudes. Clin Infect Dis 2012; 55: 1659–1660. [DOI] [PubMed] [Google Scholar]
- 44.Xu L, Zhang T, Cui B, et al. Clinical efficacy maintains patients’ positive attitudes toward fecal microbiota transplantation. Medicine 2016; 95: e4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hota SS, Poutanen SM.Is a single fecal microbiota transplant a promising treatment for recurrent Clostridium difficile infection? Open Forum Infect Dis 2018; 5: ofy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kelly CR, Yen EF, Grinspan AM, et al. Fecal microbiota transplantation is highly effective in real-world practice: initial results from the FMT National Registry. Gastroenterology 2021; 160: 183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moayyedi P, Yuan Y, Baharith H, et al. Faecal microbiota transplantation for Clostridium difficile-associated diarrhoea: a systematic review of randomised controlled trials. Med J Aust 2017; 207: 166–172. [DOI] [PubMed] [Google Scholar]
- 48.Fischer M, Kao D, Kelly C, et al. Fecal microbiota transplantation is safe and efficacious for recurrent or refractory Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis 2016; 22: 2402–2409. [DOI] [PubMed] [Google Scholar]
- 49.Kao D, Hotte N, Gillevet P, et al. Fecal microbiota transplantation inducing remission in Crohn’s colitis and the associated changes in fecal microbial profile. J Clin Gastroenterol 2014; 48: 625–628. [DOI] [PubMed] [Google Scholar]
- 50.Moayyedi P, Surette MG, Kim PT, et al. Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology 2015; 149: 102–109.e6. [DOI] [PubMed] [Google Scholar]
- 51.NICE. Faecal microbiota transplant for recurrent or refractory Clostridioides difficile infection, https://www.nice.org.uk/advice/mib247 (2021, accessed 31 May 2021).
- 52.Saha S, Mara K, Pardi DS, et al. Long-term safety of fecal microbiota transplantation for recurrent Clostridioides difficile infection. Gastroenterology 2021; 160: 1961–1969. [DOI] [PubMed] [Google Scholar]
- 53.Van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 2013; 368: 407–415. [DOI] [PubMed] [Google Scholar]
- 54.Brandt LJ, Aroniadis OC.An overview of fecal microbiota transplantation: techniques, indications, and outcomes. Gastrointest Endosc 2013; 78: 240–249. [DOI] [PubMed] [Google Scholar]
- 55.Chuong KH, O’Doherty KC, Secko DM.Media discourse on the social acceptability of fecal transplants. Qual Health Res 2015; 25: 1359–1371. [DOI] [PubMed] [Google Scholar]
- 56.Kragsnaes MS, Nilsson AC, Kjeldsen J, et al. How do I establish a stool bank for fecal microbiota transplantation within the blood-and tissue transplant service? Transfusion 2020; 60: 1135–1141. [DOI] [PubMed] [Google Scholar]
- 57.Cammarota G, Ianiro G, Tilg H, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut2017; 66: 569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Woodworth MH, Carpentieri C, Sitchenko KL, et al. Challenges in fecal donor selection and screening for fecal microbiota transplantation: a review. Gut Microbes 2017; 8: 225–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haifer C, Kelly CR, Paramsothy S, et al. Australian consensus statements for the regulation, production and use of faecal microbiota transplantation in clinical practice. Gut 2020; 69: 801–810. [DOI] [PubMed] [Google Scholar]
- 60.Ianiro G, Mullish BH, Kelly CR, et al. Screening of faecal microbiota transplant donors during the COVID-19 outbreak: suggestions for urgent updates from an international expert panel. Lancet Gastroenterol Hepatol 2020; 5: 430–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bokek-Cohen YA, Ravitsky V.Cultural and personal considerations in informed consent for fecal microbiota transplantation. Am J Bioeth 2017; 17: 55–57. [DOI] [PubMed] [Google Scholar]
- 62.Cammarota G, Ianiro G, Kelly CR, et al. International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut2019; 68: 2111–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mikail M, O’Doherty KC, Poutanen SM, et al. Ethical implications of recruiting universal stool donors for faecal microbiota transplantation. Lancet Infect Dis 2020; 20: e44–e49. [DOI] [PubMed] [Google Scholar]
- 64.Kelly CR, Laine LA, Wu GD.Monitoring fecal microbiota transplantation practice in a rapidly evolving health and regulatory environment. Gastroenterology 2020; 159: 2004–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Friedrich MJ.Unraveling the influence of gut microbes on the mind. JAMA 2015; 313: 1699–1701. [DOI] [PubMed] [Google Scholar]
- 66.Sha S, Liang J, Chen M, et al. Systematic review: faecal microbiota transplantation therapy for digestive and nondigestive disorders in adults and children. Aliment Pharmacol Ther 2014; 39: 1003–1032. [DOI] [PubMed] [Google Scholar]
- 67.Openbiome. https://www.openbiome.org/ (2019, accessed 18 August 2020).
- 68.Gliklich RE, Dreyer NA, Leavy MB. (eds). Registries for evaluating patient outcomes: a user’s guide (no. 13). Washington, DC: Government Printing Office, 2014. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-tag-10.1177_17562848211042679 for Healthcare providers’ perception of faecal microbiota transplantation with clostridium difficile infection and inflammatory bowel disease: a quantitative systematic review by Yanghua Liu, Kal Alnababtah, Simon Cook and Ying Yu in Therapeutic Advances in Gastroenterology