Abstract
This viewpoint focuses on the ways in which digital medicine and measurement-based care can be utilized in tandem to promote better assessment, patient engagement, and an improved quality of psychiatric care. To date, there has been an underutilization of digital measurement in psychiatry, and there is little discussion of the feedback and patient engagement process in digital medicine. Measurement-based care is a recognized evidence-based strategy that engages patients in an understanding of their outcome data. When implemented as designed, providers review the scores and trends in outcome immediately and then provide feedback to their patients. However, the process is typically confined to office visits, which does not provide a complete picture of a patient's progress and functioning. The process is labor intensive, even with digital feedback systems, but the integration of passive metrics obtained through wearables and apps can supplement office-based observations. This enhanced measurement-based care process can provide a picture of real-world patient functioning through passive metrics (activity, sleep, etc.). This can potentially engage patients more in their health data and involve a critically needed therapeutic alliance component in digital medicine.
Keywords: Measurement-based care, Behavioral health, Digital medicine, Patient engagement, Outcomes
The Unrealized Potential of Digital Measurement in Behavioral Health
With the advent of digital health technologies, there have been increasing calls for behavioral health practitioners to enhance traditional self-report assessments through the inclusion of objective patient monitoring data [1, 2, 3]. Efforts to improve objective measurement are particularly important because psychiatry does not possess the observable and quantifiable vital signs that are available to other medical specialties. Ideally, the collection of this data should be continuous, precise, and reflect a patient's real-world functioning [4]. Easily interpretable, real-time, and actionable patient data would assist clinicians in adapting treatments to patient needs [4]. In order to scale appropriately, the ideal measurement process should be passive in order to minimize patient effort.
Digital medicine can potentially address this gap through a broad range of mobile health, health information, wearable, and personalized medicine technologies, many of which are focused on assessment and tracking of patient symptoms and behaviors. Wearable sensors now allow tracking of physiological functions such as movement patterns, sleep, heart rate, blood pressure, oxygen saturation, and skin conductance [5, 6, 7]. Digital biomarkers (aka digital phenotyping) have been defined as “consumer-generated physiological and behavioral measures collected through connected digital tools” [8]. These measurements may be extracted from smartphone scrolling patterns, keystrokes, and speech patterns, which may offer clues about processing speed, verbal memory, and executive function [3]. Together, such data can provide insights into domains that are linked to psychiatric disorders, such as stress, mood, sociability, motor patterns, and cognitive function [7]. Digital phenotyping has been applied to mood disorder identification, relapse prevention in bipolar disorder, opioid overdose prevention, and harmful drinking detection [5].
Unfortunately, digital measurement has primarily taken place in research studies and has been underutilized in clinical practice. Providers may be hesitant due to concerns about the validity and reliability of the tracking data, workflow and interoperability with record-keeping systems, limitations in reimbursement, and ethical concerns about responding to risk information arising from data monitoring as well as data privacy challenges [9]. Provider ambivalence may potentially detract from patients' and caregivers' use of these tools and lead to missed clinical opportunities. For example, wearable devices provide valid measures of sleep and activity, but less than 10% of these devices are still in use after 6 months [10]. Digital symptom monitoring can potentially affect the course of treatment, but such data are often not fed back to patients (or sometimes even clinicians) to guide treatment decisions [11]. Both provider and patient engagement are necessary to overcome the poor utilization that has been apparent in clinics, among the public, and even in more highly controlled digital health studies [12, 13].
Digital health tools may work better when paired with live support [14], but digital medicine tools (for example, mental health apps) duplicate existing face-to-face services without leveraging one of the primary ingredients in effective treatment − the therapeutic relationship [15]. An active feedback process in digital medicine seems critical. As stated by Torous and Hsin [12], … we propose that a failure to address the digital interaction between patients and clinicians − the digital therapeutic relationship − and resulting lack of support for this new relationship limits the true potential of digital care. The therapeutic relationship should not be considered complementary to the use of digital health tools; rather it should be seen as a necessary treatment component in the accurate quantification of outcomes. Although some studies recognize the importance of the therapeutic alliance in digital medicine, it is seldom measured or regarded as a primary outcome in its own right [16]. Behavioral engagement metrics in digital applications generally assess the quantity rather than the quality of engagement, for example, the clinically meaningful use of these tools [17].
Measurement-Based Care as a Model for Digital Measurement
Measurement-based care is considered a foundation of psychiatric care [17] and introduces clinician-patient engagement into the assessment process. Measurement-based care includes 4 components: (1) administration of validated self-report measures (e.g., Personal Health Questionnaire-9 or Personal Health Questionnaire-2 and Generalized Anxiety Disorder-7) to patients before treatment sessions; (2) clinician review of numerical and graphical scores over time; (3) feedback of this data back to patients; and (4) collaborative evaluation of the results to determine maintenance or change in treatment course [18]. Measurement-based care effects are robust across various treatment modalities, populations and settings [19]. Measurement-based care enhances outcomes with anxiety and/or depressive disorders [20], resulting in a doubling of overall effect sizes [21]. Measurement-based care is particularly useful with patients who are “not on track” for positive outcomes [22]. Measurement-based care appears to affect the course of treatment through the monitoring of symptom reduction and deterioration, enhancing clinical judgments and patient-provider communications, helping patients to improve their role functioning and quality of life [23]. Ultimately, measurement-based care can extend patient retention and engagement in treatment [21, 24].
To achieve these effects, measurement-based care works within a therapeutic relationship framework, enhancing communication and information sharing between providers and patients [19]. Assessment feedback is the foundation that supports active patient participation, patient self-management, a greater understanding of symptoms, and attention to the signs of relapse [18, 25]. The dynamics of patient-therapist communication may then be shifted so that patients can expand the objectives of treatment beyond simple symptom relief to quality of life issues [26].
Enhancing Measurement-Based Care through Digital Measurement Tools
There are inherent limitations with measurement-based care as currently practiced, as the process is focused heavily on self-report data based on symptom-focused questionnaires. These measures are designed to be quite brief in order to adapt to clinician workflows, so may only reflect a narrow band of patient functioning [3]. Self-report data is collected prior to clinical encounters and is followed by in-session patient feedback. Relying on synchronous interactions based on session attendance limits the impact of measurement-based care because self-report assessments are more likely to be administered on an irregular or intermittent basis [27]. The process is essentially a collection of snapshot assessments that do not extend data collection to real-world daily functioning or effects of therapeutic interventions. Relying on patients' subjective impressions in a context which is not necessarily representative of their functioning limits the potential for measurement-based care-generated data insights between sessions. These singular data points may call into question the reliability and validity of such data [28], especially when affected by recall bias or mood-state bias [2]. This workflow is labor intensive for clinicians and it may generate greater patient and clinician engagement if there were also opportunities for passive data collection.
Digital technologies can enhance measurement-based care by offering more representative and expansive real-world data-gathering and the introduction of passively gathered data. Experience sampling (also called ecological momentary assessment) is based on the idea patients will report on outcomes over time in real-world contexts [29]. Establishing a longitudinal pattern of assessments in home or other real-world environments can encourage additional clinical monitoring between sessions to better understand symptom fluctuations [30]. This allows the clinician to better understand the relationship between the patient's clinical changes, social interactions, and environmental factors. Even more importantly, expansion of real-world measurements should be patient-focused, otherwise there is a risk of simply applying burdensome and ineffective traditional measurements in a digital format [31]. Applying digital measures that matter to patients can help them define symptoms that affect activities, make sense of these symptoms in personal contexts, and gauge the degree of change that they need to make to experience meaningful change in their lives [31].
Assessment data obtained through self-reported and objective means may sometimes diverge, as symptom ratings may not correlate with quality of life or daily functioning [32]. This should not be viewed as a disadvantage but as a strength. The goal should not be to replace current measurement standards, but to comprehend ways in which new digital measures can augment traditional (self-report) measures to form a more wholistic, patient-centered clinical picture [33]. It is possible that combining data types may capture different elements of the disease experience and progression [2] and may point the way to more precise intervention targets [2]. At a population level, gathering objective data in combination with self-reports can enhance data mining to gain a greater contextual understanding of the course of psychiatric episodes, disorder phenotypes, and the effects of medications and therapies [34].
Are there additional technologies that can be leveraged? Traditionally, measurement-based care was implemented through paper-and-pencil but now is generally available through “digital measurement feedback systems” [35]. Computerized administration not only streamlines the assessment process (often only 5 min) but allows comparison of patient data to Expected Treatment Response curves (empirically derived displays of the one's predicted treatment progression based on available normative data) [36]. Additional components may include patient treatment engagement/satisfaction/alliance assessments and critical event alerts (for example, suicidal ideation).
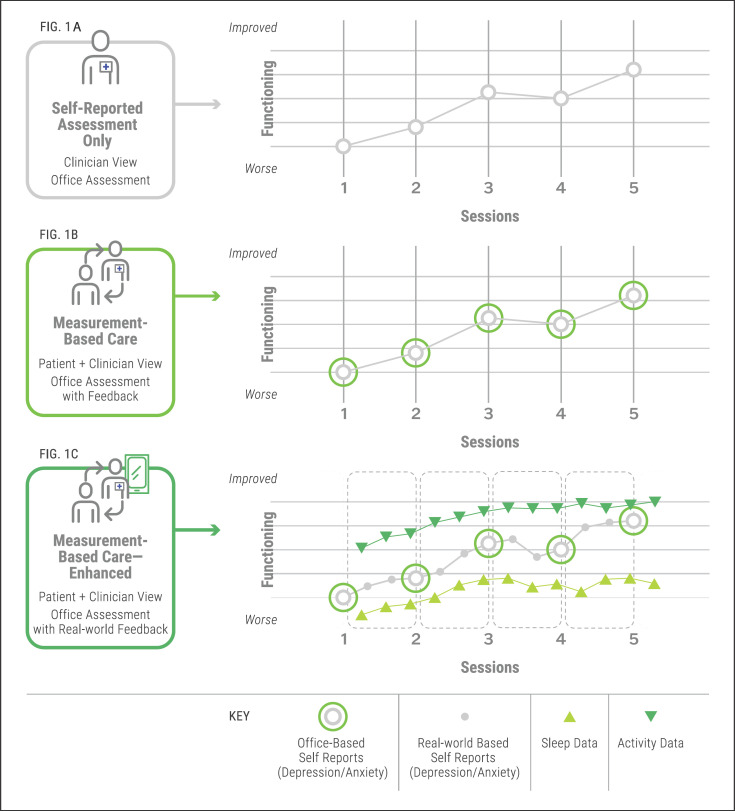
As seen in Figure 1A, the clinician is conducting assessments with a patient within the clinical encounter, offering no feedback. The process begins and ends with the clinical encounter, limiting observations and data points. The collection of data occurs in the treatment setting, which is not representative of the patient's daily routine. The assessment process is initiated and driven by the clinician. Figure 1B depicts traditional measurement-based care, which improves on this process by incorporating clinician feedback about assessment results. However, the nature of the assessment process is limited by its tethering to clinical sessions. In both 1A and 1B the patient is evidencing clinical improvement but this is based solely on self-reported assessments. Figure 1C expands self-reported assessments and incorporates the collection of passive data outside beyond the office. In this scenario, there are more opportunities for self-reported data collection between sessions with the addition of passive monitoring in the form of activity and sleep tracking. This can be accomplished through digital feedback systems or other technology-based platforms, for example, through an API, or application programming interface. In essence, this allows multiple forms of experience sampling that can provide a richer understanding of patient functioning in the real world. These data points may or may not converge. For example, the example above shows that Self-reported depression and activity levels appear to be improving, but progress on sleep is lagging behind. The relationships between these functional areas and symptoms can be processed and discussed by clinicians and patients in treatment sessions. With this enhanced measurement-based care model, there are new opportunities to move assessment beyond the office and construct a more accurate picture of patients' functioning in their natural settings. However, the use of measurement-based care-based feedback is the essential ingredient in enhancing the therapeutic relationship through digital data.
Fig. 1.
Enhanced measurement-based care with integrated digital metrics.
Telemental health offers an additional technology tool for moving patient measurement beyond the office. The COVID-19 pandemic has triggered dramatic changes in mental health service delivery, with many clinics and practices around the country shifting from virtually no telemental services to almost exclusive use of these services within the span of months [37]. Because many clinicians have overcome initial trepidation and technology aversion, the presence of these platforms in clinical offices provides an opportunity for the introduction of enhanced measurement-based care to traditional videoconferencing applications. On the patient side, the broad ownership of smartphones and desktop computers allows integration of digital measurement and measurement-based care-based feedback systems with at-home telemental health.
The assessment process does not seem to suffer from remote administration, as empirical studies have found an equivalence between face-to-face and videoconference-based assessments [30]. This addresses major measurement-based care implementation barriers − speeding delivery of assessments to patients, reducing strains on the clinical workflow, mitigating organizational and staffing challenges caused by on-site implementation of measurement-based care, and addressing systemic needs by expanding treatment access. Such integration reinforces assessment as part of the treatment experience, assures that data will be collected on a regular basis, and avoids the complications with setting up an office workflow to accommodate assessments.
The expansion of telemental health has revealed additional clinical benefits that may further enrich clinical measurement. Assessment that takes place in conjunction with in-person session attendance may be adversely affected by no-shows, cancellations, and other scheduling disruptions. Preliminary data indicate that telemental health reduces no-show rates [37], which broadens opportunities for data collection. Telemental health also enables greater access to and assessment with patients who are experiencing conditions that hinder in-person visits − severe anxiety, immobilizing depression, agoraphobia, and obsessive-compulsive behavior [37]. Administering assessments while a patient is in the waiting room may or may not be a representative indicator of a patient's clinical status. The conduct of sessions while patients are in their natural environments provides an opportunity for more direct engagement between their health data and surroundings. In addition, anecdotal reports by mental health providers have revealed that telemental health introduces additional assessment information through direct clinical observation of the stability and organization of patients' home environments [6, 37]. Leveraging measurement-based care-based videoconferencing is more than a convenience and good treatment will require agile models of technology-based assessment.
Implications of an Enhanced Measurement-Based Care Model
What would an enhanced model of measurement-based care mean for frontline clinical care? In these discussions, the issue of access always arises. Recent telemedicine data indicate that even with the pressure for greater mental health treatment access during the COVID-19 epidemic, there has not been a corresponding increase in digital health usage (telehealth, wearables, trackers, etc.) among underserved groups − rural, 55 and older, and underserved individuals [38]. Access issues persist, but there has been an assumption that these groups are disinterested in digital technology. Studies indicate that underserved groups are motivated to adopt technology and improve digital health literacy, but technology applications need to address the individualized needs of users [39]. The key in assuring clinical assessment value for patients (and clinicians) may be in the selection and relevance of real-world outcome metrics [31]. Shared decision-making, communication about data security, and attention to patient privacy are ultimately the critical factors in digital medicine success [40]. Utilizing the patient-centered approach described here along with a broader array of real-world metrics offers greater potential for patient engagement.
Ultimately, a more expansive model of measurement-based care is important in assessing and improving quality of care. The lack of patient outcomes monitoring engenders a variety of significant costs and financial inefficiencies. These may include under- or overtreatment of patients, poor therapist matching, and inadequate responses to clinical deterioration (thus leading to longer and more expensive services). Patients perceive these inefficiencies, as they may feel that treatment involves “spinning their wheels” through examination of past history and problem insight rather than accomplishing immediate goals [41]. Patients, clinicians, and payors all benefit from quantitative evidence that treatment is working, and if not, what appropriate corrective responses will be undertaken. Patients who have access to clinicians' outcome track record information agree that such information enhances the referral process and can improve mental health outcomes [42]. Accurate data may help clinicians, practices, and health systems serving challenging mental health patients from being unfairly penalized [19]. Using measurement-based care data to deploy clinicians based on their strengths rather than availability, preference, experience, or other non-outcome related factors may produce better outcomes is less time [43, 44]. Continuing education resources, often limited by tight budgets, can be better targeted to meet the needs of the organization and individual clinicians. Such feedback optimizes training and continuing education resources and does not hamper clinical outcomes or dropout rates of patients who are on track [22]. It is not unusual to have adverse events in mental health due to case mix, etc., but clinicians' responses and resulting treatment adjustments based on these outcomes [additional consultation or referring to higher levels of care] should be a focus [45]. As innovative digital assessment technologies improve, patients, clinicians, and payors can all benefit from greater measurement precision.
Statement of Ethics
This is a perspective piece and did not involve human subjects, so no ethics approval was required.
Conflict of Interest Statement
Emil Chiauzzi is an employee of Tridiuum, Inc. Paul Wicks is the founder and Independent Consultant with Wicks Digital Health, Ltd.
Funding Sources
There was no funding for this manuscript.
Author Contributions
Emil Chiauzzi developed the original concept for this viewpoint piece and was responsible for writing and editing the content. Paul Wicks contributed to the original concept and was involved in writing and editing the content.
References
- 1.Hsin H, Torous J. Creating boundaries to empower digital health technology. BJPsych Open. 2018;4((4)):235–7. doi: 10.1192/bjo.2018.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dogan E, Sander C, Wagner X, Hegerl U, Kohls E. Smartphone-based monitoring of objective and subjective data in affective disorders: where are we and where are we going? Systematic review. J Med Internet Res. 2017;19((7)):e262. doi: 10.2196/jmir.7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirschtritt ME, Insel TR. Digital technologies in psychiatry: present and future. Focus (Am Psychaitr Publ) 2018;16((3)):251–8. doi: 10.1176/appi.focus.20180001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chauvin JJ, Insel TR. Building the thermometer for mental health. Cerebrum. 2018:cer-14–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Huckvale K, Nicholas J, Torous JLM. Smartphone apps for the treatment of mental health conditions: status and considerations. Curr Opin Psychol. 2020;36:65–70. doi: 10.1016/j.copsyc.2020.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Munshi VN, Vahia I. Psychiatry is revealing the potential − and pitfalls − of telehealth. Harvard Business Rev. 2020 [Google Scholar]
- 7.Matcham F, Barattieri Di San Pietro C, Bulgari V, De Girolamo G, Dobson R, Eriksson H, et al. Remote assessment of disease and relapse in major depressive disorder (RADAR-MDD): a multi-centre prospective cohort study protocol. BMC Psychiatry. 2019;19((1)):1–11. doi: 10.1186/s12888-019-2049-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rock Health . The emerging influence of digital biomarkers on healthcare. San Francisco, CA: 2016. https://rockhealth.com/reports/the-emerging-influence-of-digital-biomarkers-on-healthcare/ [Google Scholar]
- 9.Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians' adoption of mobile health tools: systematic literature review. JMIR MHealth UHealth. 2020;8((2)):1–30. doi: 10.2196/15935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein DA, Caraway M, Johnston C, Ping A, Fogarty J, Munson SA. Beyond abandonment to next steps: understanding and designing for life after personal informatics tool use. Proc SIGCHI Conf Hum Factor Comput Syst. 2016;8((2)):1109–13. doi: 10.1145/2858036.2858045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsh S, Golden E, Priebe S. Systematic review of patients' participation in and experiences of technology-based monitoring of mental health symptoms in the community. BMJ Open. 2016;6((6)):1–9. doi: 10.1136/bmjopen-2015-008362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torous J, Hsin H. Empowering the digital therapeutic relationship: virtual clinics for digital health interventions. NPJ Digit Med. 2018;1((1)):16. doi: 10.1038/s41746-018-0028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pratap A, Steinhubl S, Neto EC, Wegerich SW, Peterson CT, Weiss L, et al. Changes in continuous, long-term heart rate variability and individualized physiological responses to wellness and vacation interventions using a wearable sensor. Front Cardiovasc Med. 2020;7:120. doi: 10.3389/fcvm.2020.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lyon AR, Lewis CC, Boyd MR, Hendrix E, Liu F. Capabilities and characteristics of digital measurement feedback systems: results from a comprehensive review. Adm Policy Ment Health. 2016 Feb;43((3)):441. doi: 10.1007/s10488-016-0719-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry. 2015;14((3)):270–7. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henson P, Wisniewski H, Hollis C, Keshavan M, Torous J. Digital mental health apps and the therapeutic alliance: initial review. BJPsych Open. 2019;5((1)):e15. doi: 10.1192/bjo.2018.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang R, Nicholas J, Knapp AA, Graham AK, Gray E, Kwasny MJ, et al. Clinically meaningful use of mental health apps and its effects on depression: mixed methods study. J Med Internet Res. 2019;21((12)):e15644. doi: 10.2196/15644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis CC, Boyd M, Puspitasari A, Navarro E, Howard J, Kassab H, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76((3)):324–35. doi: 10.1001/jamapsychiatry.2018.3329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fortney JC, Unützer J, Wrenn G, Pyne JM, Smith GR, Schoenbaum M, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68((2)):p. 179–88. doi: 10.1176/appi.ps.201500439. [DOI] [PubMed] [Google Scholar]
- 20.Peterson K, Anderson J, Bourne D. VA evidence synthesis program evidence briefs [Internet] Washington DC: Department of Veterans Affairs; 2018. Evidence brief: use of patient reported outcome measures for measurement based care in mental health shared decision-making. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30645065. [PubMed] [Google Scholar]
- 21.Miller SD, Duncan BLSR. Using formal client feedback to improve retention and outcome: making ongoing, real-time assessment feasible. J Brief Ther. 2006;5((1)):5–22. [Google Scholar]
- 22.Delgadillo J, de Jong K, Lucock M, Lutz W, Rubel J, Gilbody S, et al. Feedback-informed treatment versus usual psychological treatment for depression and anxiety: a multisite, open-label, cluster randomised controlled trial. Lancet Psychiatry. 2018;5((7)):564–72. doi: 10.1016/S2215-0366(18)30162-7. [DOI] [PubMed] [Google Scholar]
- 23.Aboraya A, Nasrallah HA, Elswick DE, Ahmed E, Estephan N, Aboraya D, et al. Measurement-based care in psychiatry-past, present, and future. Innov Clin Neurosci. 2018;15((11–12)):13–26. [PMC free article] [PubMed] [Google Scholar]
- 24.Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract. 2015;22((1)):49–59. doi: 10.1016/j.cbpra.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Valenstein M, Adler DA, Berlant J, et al. Implementing standardized assessments in clinical care: now's the time. Psychiatr Serv. 2009;60((10)):1372–5. doi: 10.1176/ps.2009.60.10.1372. [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman M, McGlinchey JB, Posternak MA, Friedman M, Attiullah N, Boerescu D. How should remission from depression be defined? The depressed patient's perspective. Am J Psychiatry. 2006;163((1)):148–50. doi: 10.1176/appi.ajp.163.1.148. [DOI] [PubMed] [Google Scholar]
- 27.Haberer JE, Trabin T, Klinkman M. Furthering the reliable and valid measurement of mental health screening, diagnoses, treatment and outcomes through health information technology. Gen Hosp Psychiatry. 2013 Jul-Aug;35((4)):349–53. doi: 10.1016/j.genhosppsych.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torous J. Measuring progress in measurement-based care with smartphone tools. Acta Psychiatr Scand. 2019;140((4)):293–4. doi: 10.1111/acps.13093. [DOI] [PubMed] [Google Scholar]
- 29.Myin-Germeys I, Kasanova Z, Vaessen T, Vachon H, Kirtley O, Viechtbauer W, et al. Experience sampling methodology in mental health research: new insights and technical developments. World Psychiatry. 2018;17:123–32. doi: 10.1002/wps.20513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luxton DD, Pruitt LD, Osenbach JE. Best practices for remote psychological assessment via telehealth technologies. Prof Psychol: Res Pract. 2014;45((1)):27–35. [Google Scholar]
- 31.Manta C. Digital measures that matter to patients: a framework to guide the selection and development of digital measures of health. Digit Biomark. 2020;02114:69–77. doi: 10.1159/000509725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faurholt-Jepsen M, Frost M, Christensen EM, Bardram JE, Vinberg M, Kessing LV. The association between mixed symptoms, irritability and functioning measured using smartphones in bipolar disorder. Acta Psychiatr Scand. 2019;139((5)):443. doi: 10.1111/acps.13021. [DOI] [PubMed] [Google Scholar]
- 33.Houts CR, Patrick-Lake B, Clay I, Wirth RJ. The path forward for digital measures: suppressing the desire to compare apples and pineapples. Digit Biomark. 2020;4((Suppl 1)):3–12. doi: 10.1159/000511586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monteith S, Glenn T, Geddes J, Whybrow PC, Bauer M. Big data for bipolar disorder. Int J Bipolar Disord. 2016;4((1)):10. doi: 10.1186/s40345-016-0051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lyon AR, Lewis CCC, Boyd MR, Hendrix E, Liu F. Capabilities and characteristics of digital measurement feedback systems: results from a comprehensive review. Adm Policy Ment Heal Ment Heal Serv Res. 2017;43((3)):441–66. doi: 10.1007/s10488-016-0719-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Langkaas TF, Wampold BE, Hoffart A. Five types of clinical difference to monitor in practice. Psychotherapy. 2018;55((3)):241–54. doi: 10.1037/pst0000194. [DOI] [PubMed] [Google Scholar]
- 37.Chen JA, Chung WJ, Young SK, Tuttle MC, Collins MB, Darghouth SL, et al. COVID-19 and telepsychiatry: early outpatient experiences and implications for the future. Gen Hosp Psychiatry. 2020 Sep-Oct;66:89–95. doi: 10.1016/j.genhosppsych.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rock Health . Digital health consumer adoption report 2020 [Internet] San Francisco, CA: 2020. Available from: https://rockhealth.com/reports/digital-health-consumer-adoption-report-2020/ [Google Scholar]
- 39.Huh J, Koola J, Contreras A, Castillo AK, Ruiz M, Tedone KG, et al. Consumer health informatics adoption among underserved populations: thinking beyond the digital divide. Yearb Med Inform. 2018;27((1)):146–55. doi: 10.1055/s-0038-1641217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rowland SP, Fitzgerald JE, Holme T, Powell J, McGregor A. What is the clinical value of mHealth for patients? NPJ Digit Med. 2020;3((1)):1–6. doi: 10.1038/s41746-019-0206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Werbart A, Annevall A, Hillblom J. Successful and less successful psychotherapies compared: three therapists and their six contrasting cases. Front Psychol. 2019;10:816. doi: 10.3389/fpsyg.2019.00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boswell JF, Constantino MJ, Oswald JM, Bugatti M, Coyne AE, Goodwin B, et al. A multimethod study of mental health care patients' attitudes toward clinician-level performance information. Psychiatr Serv. 2021;72((4)):452–6. doi: 10.1176/appi.ps.202000366. [DOI] [PubMed] [Google Scholar]
- 43.Brown GS, Lambert MJ, Jones ER, Minami T. Identifying highly effective psychotherapists in a managed care environment. Am J Manag Care. 2005;11((8)):513–20. [PubMed] [Google Scholar]
- 44.Laska K. 10 Ways to improve psychotherapy outcome [Internet] 2005. Available from: https://societyforpsychotherapy.org/10-ways-to-improve-psychotherapy-outcome/
- 45.Fortney J, Sladek R, Unützer J. Fixing behavioral health care in America: a national call for integrating and coordinating specialty behavioral health care with the medical system. The Kennedy Forum report. Part 1. 2005. Available from: https://chp-wp-uploads.s3.amazonaws.com/www.thekennedyforum.org/uploads/2017/06/KennedyForum-MeasurementBasedCare_2.pdf.