Abstract
Objectives
Ceramics can simulate the visual character of the tooth substance successfully and are biocompatible materials. However, a wide range of ceramic materials and systems on the market are available for use in dentistry. Therefore, it is the aim of this article to provide an overview of dental ceramics, their classifications, methods of construction, and clinically relevant aspects that enable the reader to select the most appropriate ceramic for a particular clinical situation.
Material and methods
The PubMed (MEDLINE) search engine was used to gather the most recent information on dental ceramics. The search was restricted to a ten-year period (January 1, 2010–December 31, 2019) and only English-language studies. A Boolean search of the PubMed data set was implemented to combine a range of keywords: (ceramics OR all-ceramics OR dental porcelain OR polycrystalline OR porcelain fused to metal OR ceramometal OR procera OR e max OR zirconia OR In-ceram OR Inlays OR Onlays OR Overlays OR Endocrown) AND (survival rate OR success rate OR clinical outcomes OR classification) AND (humans). Studies were also obtained by manual searches and from Google Scholar.
Results
By using this process, 2173 articles and studies were obtained. More studies were also obtained by manual searches and from Google Scholar. The most relevant published studies were chosen and used in the current review.
Conclusion
All-ceramic restoration use has increased in recent years. This increase has been attributed to patients’ demand for good aesthetics and an improvement in the materials’ mechanical and aesthetic properties as well as to required minimally invasive tooth preparation and the methods of fabrication. The success of ceramic restorations depends on several factors, such as selection of material, restoration design, occlusion, and cementation media.
Keywords: Porcelain fused to metal restorations, Ceramo-metal restorations, All-ceramic restorations, Dental ceramics, Zirconia
1. Introduction and background
Ceramics are biocompatible and inert materials and have a high degree of intra-oral stability. Therefore, they can be safely used in the oral cavity. However, ceramics are brittle materials that can be easily fractured (Jones, 1998, Sharkey, 2011). To combat this weakness, ceramics are usually reinforced with particles, supported by metal, or made purely of polycrystalline material.
When aesthetics are of utmost importance, dental ceramics are the material of choice because they can visually simulate the character of the tooth substance successfully (Contrepois et al., 2013). For instance, the use of all-ceramic restorations has increased in recent years (Zarone et al., 2011, Mitov et al., 2016, Zarone et al., 2019). Nevertheless, there is a wide range of ceramic materials and systems on the market that are available for use in dentistry (Kelly, 2004, Raigrodski, 2005, Sharkey, 2010).
All-ceramic restorations can be used as a bi-layered restoration in which a core or framework is veneered by more aesthetic ceramics. They can also be used as full-contour (monolithic) restorations, which can be stained when required.
In general, monolithic restorations have good mechanical properties but may not always provide the required aesthetic requirements. Monolithic restorations are more commonly used in the posterior region of the mouth because the aesthetic is less critical. On the other hand, bi-layered, all-ceramic restorations provide outstanding aesthetic results and may be used in the aesthetic areas (Hermann et al., 2006).
The predominantly glass-based ceramics such as feldspathic ceramics are used as veneers to cover the metal coping and framework. They are also used in the bi-layered, all-ceramic restoration method when the aesthetic is considered a dominant factor (Stappert et al., 2005). Although the predominantly glass-based ceramic restorations are the most aesthetic, they are also the weakest (Castelnuovo et al., 2000). The improved strength of highly filled glass-based ceramics such as leucite- and lithium disilicate–based types are considered for use as inlays and onlays, anterior and posterior crowns, and veneers. They can also be used as a short-span, three-unit, fixed partial denture (FPD). In addition, they can be used as monolithic or bi-layer restorations. Polycrystalline ceramics such as zirconia are more commonly used as monolithic restorations in posterior regions, but they can also be used as cores or frameworks for bi-layer restorations.
Generally, the success of ceramic restorations depends on several factors such as material selection, restoration design, and cementation media (Mizrahi, 2008, Sharkey, 2010, Rekow et al., 2011).
The aim of this article is to provide an overview of dental ceramics and their classifications and methods of construction. This knowledge will enable the reader to select the most appropriate ceramic for a particular clinical situation and aids communication between the clinical and laboratory personnel.
2. Materials and methods
The PubMed (MEDLINE) search engine was used to gather the most relevant and recent information on dental ceramics. The search was restricted to a ten-year period (January 1, 2010–December 31, 2019) and only English-language studies. A Boolean search of the PubMed data set was implemented to combine a range of keywords: (ceramics OR all-ceramics OR dental porcelain OR polycrystalline OR porcelain fused to metal OR ceramo-metal OR procera OR e max OR zirconia OR In-ceram OR Inlays OR Onlays OR Overlays OR Endocrown) AND (survival rate OR success rate OR clinical outcomes OR classification) AND (humans). By using this process, 2173 articles and studies were obtained. More studies were also obtained by manual searches and from Google Scholar. The most relevant published studies were chosen and used in the current review. The selected articles are included in the references list.
2.1. Porcelain fused to metal restorations
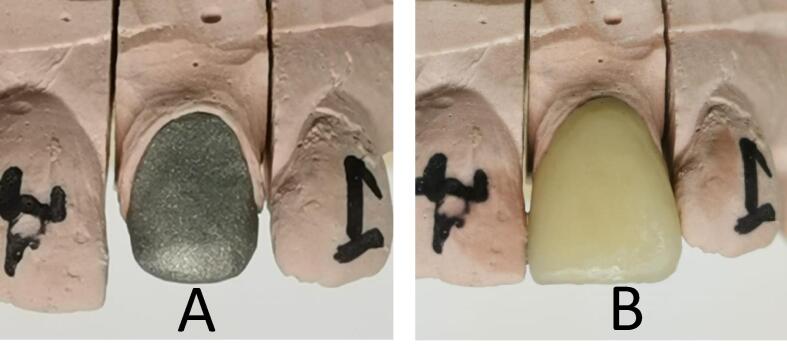
A porcelain fused to metal (PFM) restoration is composed of a metal coping that supports overlying ceramic (Fig. 1). PFM restorations have a long clinical track record (Denry and Holloway, 2010). However, failure rates of the PFM fixed partial denture was 4% after five years, 12% after 10 years, and 32% after 15 years (Valderhaug, 1991).
Fig. 1.
A PFM crown: a metal coping (A) that is veneered with ceramics (B).
Compatibility between the ceramic and the metal alloy is of paramount importance. Requirements for the metal alloys used in the construction of PFM restorations are presented in Table 1.
Table 1.
Requirements for the metal alloys used with PFM restorations.
|
PFM ceramic veneers consist of an opaque ceramic (e.g., a titanium oxide glass) that is required to mask the color of the underlying metal and provides the bond with the metal alloy (Terada et al., 1989). The opaque ceramic bonds to the metal alloy by an oxide layer that is created on the metal surface in a process known as degassing. The degassing process also removes the contaminants from the alloy surface. A dentine/body ceramic is applied over the opaque ceramic. The dentine ceramics simulate natural dentine. An incisal ceramic is then applied to the incisal third over the dentine/body ceramic. The restoration is also glazed either by the use of a low-fusing glazing ceramic or self-glazed, and it can be polished.
One of the main disadvantages of a PFM restoration is its inability to transmit light, thus having a negative effect on the aesthetic outcome of the restoration because it may appear dark in color (Sharkey, 2010, Sharkey, 2011). This drawback is more noticeable at the cervical area of the restoration where it is sometimes not possible to get enough room. To mitigate this effect, an adequate amount of the tooth structure should be removed to accommodate a ceramic material that can mask the underlying metal without over-contouring the restoration. In addition, the metal coping should stop 1 mm short of the buccal finish line, and a ceramic margin (shoulder ceramic) should be used (O’Boyle et al., 1997, Sharkey, 2011).
Another disadvantage of a PFM restoration is allergic reactions in some patients to metal elements such as nickel in the metal alloy.
Examples of ceramics used in PFM restorations include VM15® (Vita), and IPS InLine (Ivoclar Vivadent) represent powder ceramics, whereas PM9® (Vita) and IPS InLine POM® (Ivoclar Vivadent) represent pressed ceramics.
2.2. All-ceramic restorations
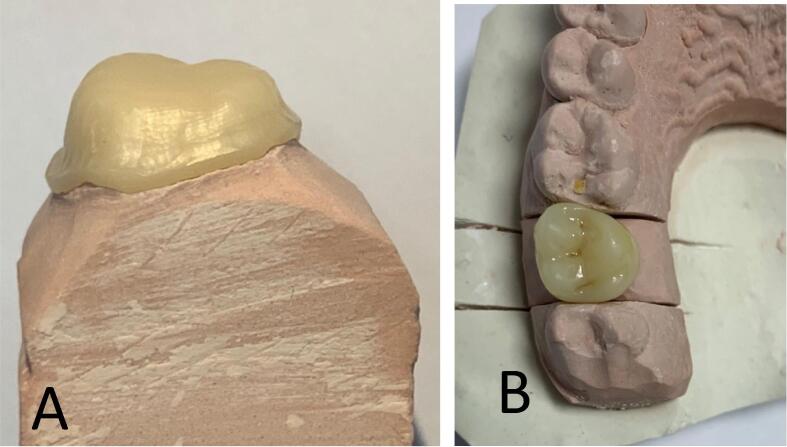
When a ceramic restoration is made completely of ceramic material, it is known as an all-ceramic restoration. In an all-ceramic restoration, the ceramic material may be monolithic (uni-layer) and consist of a single ceramic material, or it may consist of a ceramic core material that is covered with a ceramic veneer (Beuer et al., 2009, Sharkey, 2010) and is known as a bi-layered, all-ceramic restoration. In the bi-layered, all-ceramic restoration, the ceramic core supports the restoration and gives it strength, and the veneer provides the restoration with its final shape, shade, and aesthetic. However, the core may also play a part in the development of the final restoration’s shade. Nevertheless, the veneer-core bond strength is considered one of the weakest links of the bi-layered all-ceramic restorations (Holden et al., 2009), because they are prone to delamination and fracture (Rekow et al., 2011). The bi-layered, all-ceramic restoration is usually used when aesthetics is the prime motive for its use. The main drawbacks that are associated with this kind of restoration include delamination and fracture of the veneers. In addition, well-constructed occlusal contacts with opposing teeth are sometimes challenging to achieve. However, to achieve long-lasting restorations, the compatibility of the core and veneer materials is crucial. Fig. 2 shows a bi-layer, all-ceramic crown in which the zirconia core was veneered with a glass-based ceramic.
Fig. 2.
An all-ceramic core on a die stone (A). The same core veneered with a high glass–ceramic (B).
On the other hand, because the monolithic restoration is composed of only one ceramic material, it is more durable than the bi-layered type (Holden et al., 2009). Furthermore, a proper occlusal morphology and occlusal contacts can be achieved, especially when the pressable or computer-aided design and computer-aided manufacturing (CAD/CAM) method is used. However, the aesthetic outcome of such restoration may be inferior to that obtained by the bi-layering method (Hamza and Sherif, 2019). Hence, the monolithic ceramic may be recommended when aesthetics is not an issue. Therefore, it is more appropriate for restoring posterior teeth than for anterior teeth.
Unlike ceramics used with PFM restorations, ceramics used in fabricating all-ceramic restorations are made up of more crystalline particles. As such, the percentage of crystalline particles may range from 40% to 70%. Furthermore, the ceramic may be purely polycrystalline and can contain up to 99.9% particles (Deany, 1996, Aboushelib et al., 2005, Denry and Holloway, 2010).
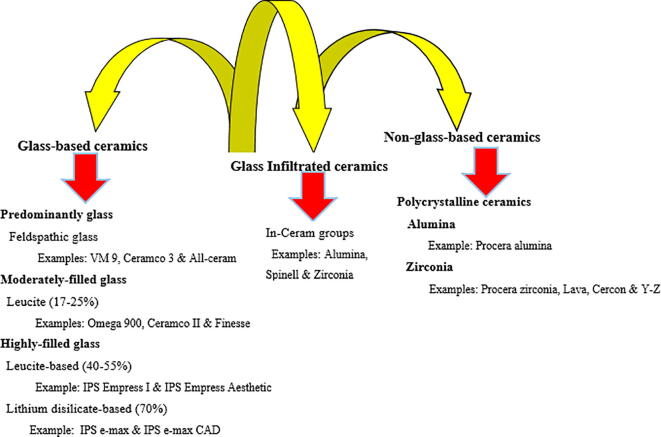
2.3. Classification of dental ceramics
Several classification methods are used in categorizing dental ceramics, one of which is based on their composition. The classification method, which is based for ceramics’ composition, is simple to understand and provides essential information that helps dental personnel select a suitable ceramic. Classifications of ceramics according to their composition are displayed in Fig. 3.
Fig. 3.
Classifications of ceramics according to their composition with examples of commercially available ceramic types.
Dental ceramics can also be classified based on their method of fabrication. This classification is also important because it sheds light on the techniques by which dental restorations are made.
2.3.1. Ceramic classification based on composition
This classification can be split into three categories: glass-based, glass-infiltrated, and non-glass-based (polycrystalline) ceramics.
2.3.1.1. Glass-based ceramics
According to the percentage of added particles, glass-based ceramics may also be divided into three subclasses: predominantly, moderately-filled, and highly-filled glass.
2.3.1.1.1. Predominantly glass (feldspathic glass)
Feldspathic class consists of ceramic materials that are principally glass with trace amounts of various kinds of particles. They are commonly known as feldspathic porcelain because they principally contain silica- and alumina-based feldspar. The percentage of added particles is less than 17%. Their flexure strengths are the weakest among ceramic materials, because they range from 70 to 90 MPa (Powers and Wataha, 2017). They are one of the most aesthetically pleasing ceramic types. They are usually used as veneers, inlays, and onlays as well as veneers for cores and frameworks for all-ceramic restorations (bi-layered).
This type of ceramic is brittle and needs support during fabrication and in service. They can be fabricated by using a platinum foil or a refractory die. They are also available as blocks that are used with the CAD/CAM systems. Examples of predominantly glass ceramics include VM 13® from Vita and AllCeram® from Degudent.
2.3.1.1.2. Moderately filled glass ceramics
This is also a glass-based ceramic and has a higher percentage of particles than that of predominantly glass ceramics. As such, it may contain 17–25% of particles such as leucite (Kelly and Benetti, 2011). The increased percentage of particles is associated with an improvement in the mechanical properties of this ceramic class. However, it may lead to ceramics that are less aesthetically pleasing than the predominantly glass–ceramic types.
The ceramics in this class can be used as veneers, inlays, onlays, and veneers for metal copings and framework (Rekow et al., 2011). Examples of this type of ceramic include VMK 95® (Vita) Ceramco II® (Dentsply) and IPS d.SIGN (Ivoclar Vivadent).
2.3.1.1.3. Highly filled glass ceramics
These are glass-based ceramics in which the percentage of particles ranges from 45 to 70 vol%. Crystalline particles such as leucite and lithium disilicate are the most commonly used particles in this category. The flexure strength of leucite-based glass ceramics ranges between 120 and 160 MPa, whereas lithium disilicate–based ceramics ranges between 300 and 500 MPa (Powers and Wataha, 2017).
They can be used as inlays, onlays, veneers, and crowns (anterior and posterior) (Fradeani and Redemagni, 2002). They can also be used as short-span, three-unit FPDs (Wolfart et al., 2009 or as core materials for crown and three-unit anterior FPDs (Guess et al., 2009).
Examples of a leucite-based highly filled glass include IPS Empress Aesthetic® (Ivoclar Vivadent), Optec OPC® (Jeneric Pentron), Authentic® (Jensen), and Finesse All-Ceramic (Dentsply). IPS Empress® CAD (Ivoclar Vivadent) is an example of CAD/CAM leucite-based ceramics.
Examples of lithium disilicate-based ceramics include IPS e.max® Press and IPS e.max® CAD (Ivoclar Vivadent) and 3G® (Jeneric Pentron).
2.3.1.2. Glass-infiltrated ceramics (In-Ceram group)
This type of ceramic is usually considered a glass-based ceramic. However, in this article, it is classified separately because it is based on particles such as alumina, magnesium, or zirconia that are then infiltrated with glass (Lekesiz, 2014). This ceramic type is known as In-Ceram ceramics and consists of a sintered mass that is infiltrated with a low-viscosity glass. They include In-Ceram® Alumina, In-Ceram® Spinell (magnesium aluminate spinel), and In-Ceram® Zirconia from Vita. In-Ceram Alumina® contains about 70 vol% alumina and about 30% glass matrix. Its fracture toughness and strength are close to that of 100% polycrystalline alumina (Aboushelib et al., 2005, Rekow et al., 2011). Therefore, In-Ceram Alumina is not a highly aesthetic material (Heffernan et al., 2002). In-Ceram Alumina has a flexural strength of about 600 MPa and, hence, can be used as single crowns and three-unit anterior bridges.
In-Ceram® Spinell is a modification of In-Ceram Alumina. It is mainly composed of magnesium spinel with trace amounts of alumina. It provides a more translucent but weaker ceramic restoration than In-Ceram Alumina and In-Ceram Zirconia because its flexure strength is approximately 350 MPa (Shenoy and Shenoy, 2010). Therefore, its use is limited to anterior crowns. Fig. 4 shows a schematic representation of a cross-section of an In-Ceram crown.
Fig. 4.
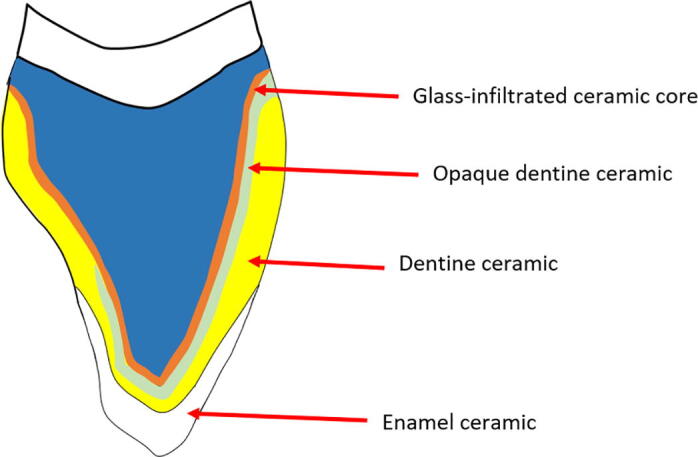
A schematic representation of a cross-section of an In-Ceram crown which consists of a glass-infiltrated core and a veneering ceramic.
In-Ceram® Zirconia is a mixture zirconia and alumina (~20 and ~ 50 vol%, respectively) (Rekow et al., 2011). However, it is opaque, which limits its use to posterior restorations.
In general, In-Ceram ceramic is usually used as a core for crowns and anterior three-unit FPDs (Guazzato et al., 2004).
2.3.1.3. Non-glass-based ceramics (polycrystalline ceramics)
Ceramics in this class do not contain glass. They may be alumina- or zirconia-based types. Both materials are characterized by their high mechanical properties. For example, alumina has flexure strength of about 650 MPa, whereas zirconia’s flexure strength ranges from 800 to 1500 MPa. Therefore, they are stronger and tougher than glass-based ceramics. However, this type of ceramics is less translucent and more opaque than glass-based ceramics (Rekow et al., 2011).
2.3.2. Ceramic classification based on its fabrications
Several methods are used to fabricate ceramic restorations. These methods range from a simple conventional technique in which a ceramic slurry is applied to platinum foil or a refractory die, to a relatively new method in which computer software (e.g., CAD/CAM) is used to design and make the restoration.
2.3.2.1. Conventional technique (stacking and sintering)
In the conventional method, ceramic powder is mixed with a liquid such as water or a water–glycerin mixture to form a malleable mass which is then applied to a platinum foil, a refractory die, or a metal coping to form a restoration (Puri, 2005, Sharkey, 2011). The excess liquid is drawn to the surface by a vibrating motion and then removed by absorbent tissue to form a “green state” that can be shaped and carved to the shape of the prospective core or restoration. The formed mass is then exposed to a high temperature, which allows the ceramic particles to attach at their borders and coalescence. Examples of ceramics made by this method include VM® 13 from Vita, and Ceramco 3® from Dentsply.
2.3.2.2. Heat-/hot-pressing technique (lost-wax technique)
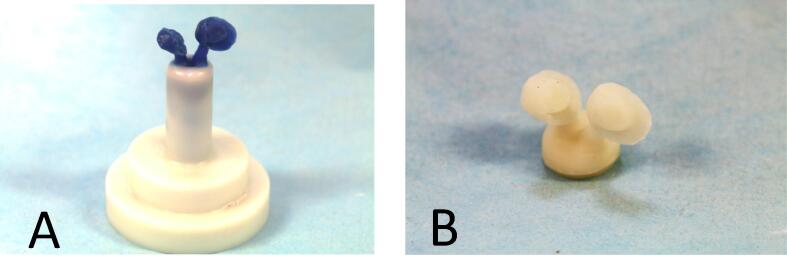
In principle, the restoration is made by the lost-wax technique by which cast metal restorations are fabricated. Hence, a wax pattern of the planned core or restoration is made and invested in refractory die materials (Puri, 2005, Sharkey, 2011). The wax is then eliminated, and a mold is produced. A ceramic ingot (block) is heated and pressed into the mold under high temperature. Restorations made by this method are also known as pressable ceramics. Because this method is based on the application of external pressure at high temperatures to produce the restoration, it is also known as the hot-pressing technique. One of the advantages of the hot-pressing method is that dental technicians are familiar with most of the fabrication steps such as investing, wax-elimination, and casting method. Two major, highly filled glass ceramic restorations are made using the heat-pressing method: leucite- and lithium disilicate–based ceramics (Ritzberger et al., 2010). An example of the commercially available products used with the press technique includes IPS Empress ceramics. The lost-wax technique is displayed in Fig. 5.
Fig. 5.
Two wax patterns attached to a sprue. Devested all-ceramic pattern replicating the two wax patterns.
2.3.2.3. Slip-casting and the glass-infiltration (infusion) method (In-Ceram® ceramic group)
This technique involves the application of ceramic slurry to a porous refractory die. The die absorbs water from the slurry by capillary action, which leads to compaction of the particles (Aboushelib et al., 2005). In-Ceram crowns can also be made by the CAD/CAM method, by which ceramic blocks are milled to the desired copings and then infiltrated with glass.
2.3.2.4. Dry-pressing method (Procera® ceramics)
This method represents one approach by which polycrystalline (alumina or zirconia) restorations are made. In this approach, a die stone is made from a conventional impression. The die is then scanned to obtain several thousands of measurements by which a computer-made enlarged (oversized) die is generated. A ceramic powder such as alumina is pressed on the enlarged die. The pressed powder is then heat treated and consequently shrinks to the required dimension. The die is oversized to compensate for shrinkage that occurs as a result of the sintering process. As the die is precisely enlarged (i.e., 12–20%), a core that is polycrystalline in nature would fit the prepared tooth with a reasonable degree of accuracy.
Examples of this method are Procera® Alumina and Procera® Zirconia from Vita (Andersson and Oden, 1993). The second method by which polycrystalline ceramics are fabricated is the CAD/CAM method.
2.3.2.5. CAD/CAMxx
CAD/CAM is an acronym for computer-aided design-computer-aided manufacturing (or computer-assisted machining) and is a technology used to produce different types of dental prostheses. CAD/CAM methods represent techniques in which the design and fabrication of ceramic restorations are carried out using computer software and have become an important part of dentistry (Mörmann, 2006).
The advantages of the CAD/CAM methods also include a decrease in clinical time as well as cross-infection between the clinic and the laboratory, particularly when intraoral scanning (digital impression) is used, and the degree of discomfort may be substantially reduced or eliminated. The digital impression can be sent immediately to the laboratory, and communication with the dental technician is improved. The CAD/CAM systems enable the clinician and/or the technician to examine the preparation from different sides for accuracy and verify interocclusal clearance before the milling procedure begins. Use of the CAD/CAM systems can prevent some human errors. Restorations made with CAD/CAM technology can be made chairside (in office) or in a dental or manufacturer’s laboratory (centralized) (Poticny and Klim, 2010).
Several drawbacks are associated with the use of CAD/CAM systems, including but not limited to the cost of the machines and the price of investment and maintenance (Baroudi and Ibraheem, 2015). Hence, the overall cost of the CAD/CAM systems is usually higher than other fabrication techniques.
2.3.2.5.1. Use of CAD/CAM techniques in fabrications of restorations
In general, the use of CAD/CAM systems involves three steps. First, an impression of the prepared tooth and the surrounding tissue is taken either digitally or by a conventional method. If the conventional method is used, a stone replica is usually obtained and then scanned to develop a digital impression. Second, the digital impression is then processed by a computer. Third, the processed information controls and guides a milling machine that is connected to a computer, thereby creating the planned restoration (Baroudi and Ibraheem, 2015).
The digital impression can also be used in some techniques to scan the prepared tooth or teeth and the occlusion of the opposing jaw, so an interocclusal record is not required.
Ceramic blocks from which the CAD/CAM restorations are made are either partially or fully sintered.
2.3.2.5.1.I Soft-machining (partially sintered state milling)
Because the blocks consist of partially sintered polycrystalline ceramics, the technique is called soft-machining to distinguish it from the hard-machining method. The produced core or restoration is oversized and is partially sintered. The blocks are milled to an enlarged core or restoration, which then shrinks during the subsequent sintering process. The enlarged core or restoration is produced to compensate for the shrinkage encountered during sintering (Kwon et al., 2013). Hence, further heat treatment is required to achieve a fully sintered state.
The main type of ceramic that is used in soft-machining is polycrystalline ceramics (i.e., zirconia and alumina). An example of zirconia ceramics is 3 yttrium-oxide, partially stabilized zirconia (3Y-PSZ).
An example of soft-machining ceramics is the Lava® CAD/CAM system and the IPS e.max ZirCAD® (Ivoclar Vivadent).
2.3.2.5.1.II Hard-machining (fully sintered state milling)
The blocks used in the hard-machining method are in a fully sintered state (Li et al., 2014) and do not require additional heat treatment. Restorations made by this method have a superior fit (Denry and Kelly, 2008).
The main disadvantages of this method include wearing down the cutting tool and a lengthy fabrication process (Aboushelib et al., 2005). Furthermore, the laboratory procedure is more complex than that of the soft-machining method.
3. Conclusion
All-ceramic restoration use has increased in recent years (Mitov et al., 2016, Zarone et al., 2019). The success of ceramic restorations depends on several factors such as material selection, restoration design, occlusion, and cementation media. The presented information is important because sound knowledge about different ceramic materials enables the dentist to select the most appropriate ceramic for a particular clinical situation and improves communication between the clinical and laboratory personnel.
Acknowledgement
The authors would like to thank Dr David McReynolds, Assistant Professor, Division of Restorative Dentistry and Periodontology, Dublin Dental University Hospital, for providing Fig. 5.
Footnotes
Peer review under responsibility of King Saud University.
References
- Aboushelib M.N., de Jagger N., Kleverlaan C.J., Feilzer A.J. Microtensile bond strength of different components of core veneered all-ceramic restorations. Dent Mater. 2005;21:984–991. doi: 10.1016/j.dental.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Andersson M., Oden A.A. new all-ceramic crown. A dense-sintered, high purity alumina coping with porcelain. Acta Odontol Scand. 1993;51:59–64. doi: 10.3109/00016359309041149. [DOI] [PubMed] [Google Scholar]
- Baroudi K., Ibraheem S.N. Assessment of Chair-side Computer-Aided Design and Computer-Aided Manufacturing Restorations: A Review of the Literature. J Int Oral Health. 2015;7:96–104. [PMC free article] [PubMed] [Google Scholar]
- Beuer F., Schweiger J., Eichberger M., Kappert H.F., Gernet W., Edelhoff D. High-strength CAD/CAM-fabricated veneering material sintered to zirconia copings–a new fabrication mode for all-ceramic restorations. Dent Mater. 2009;25:121–128. doi: 10.1016/j.dental.2008.04.019. [DOI] [PubMed] [Google Scholar]
- Castelnuovo J., Tjan A.H., Phillips K. Fracture load and mode of failure of ceramic veneers with different preparations. J Prosthet Dent. 2000;83:171–180. doi: 10.1016/s0022-3913(00)80009-8. [DOI] [PubMed] [Google Scholar]
- Contrepois M., Soenen A., Bartala M., Laviole O. Marginal adaptation of ceramic crowns: a systematic review. J Prosthet Dent. 2013;110:447–454. doi: 10.1016/j.prosdent.2013.08.003. [DOI] [PubMed] [Google Scholar]
- Deany I.L. Recent advances in ceramics for dentistry. Crit Rev Oral Biol Med. 1996;7:134–143. doi: 10.1177/10454411960070020201. [DOI] [PubMed] [Google Scholar]
- Denry I., Holloway J.A. Ceramics for Dental Applications: A Review. Materials. 2010;3:351–368. [Google Scholar]
- Denry I., Kelly J.R. State of the art of zirconia for dental applications. Dent Mater. 2008;24:299–307. doi: 10.1016/j.dental.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Fradeani M., Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quintessence Int. 2002;33:503–510. [PubMed] [Google Scholar]
- Guazzato M., Albakry M., Ringer S.P., Swain M.V. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part I. Pressable and alumina glass-infiltrated ceramics. Dent Mater. 2004;20:441–448. doi: 10.1016/j.dental.2003.05.003. [DOI] [PubMed] [Google Scholar]
- Guess P.C., Zhang Y., Thompson V.P. Effect of veneering techniques on damage and reliability of Y-TZP trilayers. Eur J Esthet Dent. 2009;4:262–276. [PubMed] [Google Scholar]
- Hamza T.A., Sherif R.M. Fracture Resistance of Monolithic Glass-Ceramics Versus Bilayered Zirconia-Based Restorations. J Prosthodont. 2019;28:e259–e264. doi: 10.1111/jopr.12684. [DOI] [PubMed] [Google Scholar]
- Heffernan M.J., Aquilino S.A., Diaz-Arnold A.M., Haselton D.R., Stanford C.M., Vargas M.A. Relative translucency of six all-ceramic systems. Part II: core and veneer materials. J Prosthet Dent. 2002;88:10–15. [PubMed] [Google Scholar]
- Hermann I., Bhowmick S., Zhang Y., Lawn B.R. Competing fracture modes in brittle materials subject to concentrated cyclic loading in liquid environments: Trilayer structures. J Mater Res. 2006;2:512–521. [Google Scholar]
- Holden J.E., Goldstein G.R., Hittelman E.L., Clark E.A. Comparison of the marginal fit of pressable ceramic to metal ceramic restorations. J Prosthodont. 2009;18:645–648. doi: 10.1111/j.1532-849X.2009.00497.x. [DOI] [PubMed] [Google Scholar]
- Jones D.W. A brief overview of dental ceramics. J Can Dent Assoc. 1998;64:648–650. [PubMed] [Google Scholar]
- Kelly J.R. Dental ceramics: current thinking and trends. Dent Clin North Am. 48. 2004;viii:513–530. doi: 10.1016/j.cden.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Kelly J.R., Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Aust Dent J. 56. Suppl. 2011;1:84–96. doi: 10.1111/j.1834-7819.2010.01299.x. [DOI] [PubMed] [Google Scholar]
- Kwon T.K., Pak H.S., Yang J.H., Han J.S., Lee J.B., Kim S.H., Yeo I.S. Comparative fracture strength analysis of Lava and Digident CAD/CAM zirconia ceramic crowns. J Adv Prosthodont. 2013;5:92–97. doi: 10.4047/jap.2013.5.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lekesiz H. Reliability Estimation for Single-unit Ceramic Crown Restorations. J Dent Res. 2014;93:923–928. doi: 10.1177/0022034514544215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R.W., Chow T.W., Matinlinna J.P. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res. 2014;58:208–216. doi: 10.1016/j.jpor.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Mitov G., Anastassova-Yoshida Y., Nothdurft F.P., von See C., Pospiech P. Influence of the preparation design and artificial aging on the fracture resistance of monolithic zirconia crowns. J Adv Prosthodont. 2016;8:30–36. doi: 10.4047/jap.2016.8.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizrahi B. The anterior all-ceramic crown: a rationale for the choice of ceramic and cement. Br Dent J. 2008;205:251–255. doi: 10.1038/sj.bdj.2008.735. [DOI] [PubMed] [Google Scholar]
- Mörmann W.H. The evolution of the CEREC system. J Am Dent Assoc. 2006;137(Suppl):7S–13S. doi: 10.14219/jada.archive.2006.0398. [DOI] [PubMed] [Google Scholar]
- O’Boyle K.H., Norling B.K., Cagna D.R., Phoenix R.D. An investigation of new metal framework design for metal-ceramic restorations. J Prosthet Dent. 1997;78:295–301. doi: 10.1016/s0022-3913(97)70029-5. [DOI] [PubMed] [Google Scholar]
- Poticny D.J., Klim J. CAD/CAM in-office technology: innovations after 25 years for predictable, esthetic outcomes. J Am Dent Assoc. 141. Suppl. 2010;2:5S–9S. doi: 10.14219/jada.archive.2010.0356. [DOI] [PubMed] [Google Scholar]
- Powers J., Wataha J. 11th Edition. Mosby; 2017. Dental Materials: Foundations and Applications. [Google Scholar]
- Puri S. Techniques used to fabricate all-ceramic restorations in the dental practice. Compend Contin Educ Dent. 2005;26:519–525. [PubMed] [Google Scholar]
- Raigrodski A.J. All-ceramic full-coverage restorations: concepts and guidelines for material selection. Pract Proced Aesthet Dent. 2005;17:249–256. [PubMed] [Google Scholar]
- Rekow E.D., Silva N.R., Coelho P.G., Zhang Y., Guess P., Thompson V.P. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011;90:937–952. doi: 10.1177/0022034510391795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritzberger C., Apel E., Höland W., Peschke A., Rheinberger V.M. Properties and Clinical Application of Three Types of Dental Glass-Ceramics and Ceramics for CAD-CAM Technologies Materials. 2010;3:3700–3713. [Google Scholar]
- Sharkey S. Metal ceramic versus all ceramic restorations: part I J Ir Dent Assoc. 2010;56:196–199. [PubMed] [Google Scholar]
- Sharkey S. Metal-ceramic versus all-ceramic restorations: part III. J Ir Dent Assoc. 2011;57:110–113. [PubMed] [Google Scholar]
- Shenoy A., Shenoy N. Dental ceramics: An update. J Conserv Dent. 2010;13:195–203. doi: 10.4103/0972-0707.73379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stappert C.F., Ozden U., Gerds T., Strub J.R. Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. J Prosthet Dent. 2005;94:132–139. doi: 10.1016/j.prosdent.2005.05.023. [DOI] [PubMed] [Google Scholar]
- Terada Y., Sakai T., Hirayasu R. The masking ability of an opaque porcelain: a spectrophotometric study. Int J Prosthodont. 1989;2:259–264. [PubMed] [Google Scholar]
- Valderhaug J.A. 15-year clinical evaluation of fixed prosthodontics. Acta Odontol Scand. 1991;49:35–40. doi: 10.3109/00016359109041138. [DOI] [PubMed] [Google Scholar]
- Zarone F., Di Mauro M.I., Ausiello P., Ruggiero G., Sorrentino R. Current status on lithium disilicate and zirconia: a narrative review. BMC Oral Health. 2019;19:134. doi: 10.1186/s12903-019-0838-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarone F., Russo S., Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent Mater. 2011;27:83–96. doi: 10.1016/j.dental.2010.10.024. [DOI] [PubMed] [Google Scholar]