Abstract
Background
To date, no attempt has been made to collate literature on the relationship between the social environmental impact of COVID-19 and erectile dysfunction. The aim of this explorative review was to assess and compare the prevalence of erectile dysfunction (ED) in male healthcare workers and males during the COVID-19 pandemic.
Methods
A systematic review of major databases from inception to February 2021 was conducted. Prevalence data were extracted, and a random-effects meta-analysis was undertaken.
Outcomes
The pooled prevalence of ED amongst healthcare workers working in COVID-19 specific environments, and non-healthcare during the COVID-19 pandemic.
Results
Of 52 initial studies, six were included for the final analysis. The pooled prevalence of ED in healthcare workers working in a COVID-19 environment was 63.6% (95% CI 20.3–92.3%), and in non-healthcare workers during the COVID-19 pandemic was 31.9% (95% CI 19.5–47.6%).
Conclusion
The prevalence of ED in healthcare workers working in COVID-19 environments was higher than representative samples and is of concern. Sexual health (and by extension, overall health), should be a priority when considering ways to care for this population. Considering the social environmental impact of COVID-19 on sexual health and in particular on ED, it is important to provide adequate psychological support systems and to promote quality of life with particular attention to sexual health.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40618-021-01679-1.
Keywords: Erectile dysfunction, Sexual health, COVID-19, Prevalence
Introduction
In 2020, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread worldwide at an unprecedented pace. Restrictions implemented to control and reduce the spread of the virus restricted social interaction and changed lifestyle behaviours and routines [1]. In particular, the socio-economic impact and the measures to reduce viral transmission, such as self-isolation, home-working, and reduced ability to socialise, reportedly resulted in increases in loneliness, anxiety, depression and impaired psychological wellbeing [2]. Indeed, perhaps the greatest exposure to the virus and its impact on health were experienced by health care workers particularly those having direct contact with COVID-19 patients.
It is plausible that the above-mentioned measures also impacted on sexual wellbeing. Indeed, a frequent and trouble-free sex life could act as an antidote mitigating self-isolation and its consequences, with a fulfilling sex life being found to be associated with multiple mental and physical health benefits [3, 4]. Interestingly, literature has suggested that during COVID-19 restrictions, levels of sexual activity have been low [5]. It could be speculated that low levels of sexual activity during the pandemic may be partly caused by an increase in population levels of sexual dysfunction. Erectile dysfunction (ED) is the most common sexual health issue in men, and it can be caused by organic, hormonal, and/or psychological factors [6]. In turn, ED is associated with a substantial range of mental, physical and psychologically adverse outcomes, including anxiety, low mood and quality of life [6]. To date, limited literature is available on the impact of COVID-19 on ED although studies are starting to emerge on this topic. The aim of this explorative review was to assess the prevalence of ED in male healthcare workers working in direct contact with COVID-19 patients and males during the COVID-19 pandemic.
Methods
This systematic review adhered to the PRISMA [7] and MOOSE [8] statements and followed a structured protocol available under reasonable request from the corresponding author.
Search strategy
Two investigators (NV and DP) independently conducted a literature search using MEDLINE/PubMed, Scopus, CINAHL, Embase, PsycINFO and Cochrane Library databases from inception to the 7th of February 2021. The following search strategy was used: “COVID-19” OR "Novel Coronavirus–Infected Pneumonia" OR "2019 novel coronavirus" OR "2019-nCoV" OR “SARS-CoV-2” AND “erectile dysfunction" OR "erectile function" OR "sexual dysfunction" OR "sexual function" OR “impotence”. The references of retrieved articles together with the proceedings of relevant conferences were hand-searched to identify other potentially eligible studies for inclusion in the analysis missed by the initial search or any unpublished data. The literature search, assessment of inclusion and exclusion criteria, quality of studies and extraction of data were independently undertaken and verified by two investigators (MT, DP). The results were then compared, and in case of discrepancies, a consensus was reached with the involvement of a third senior investigator (LS). There was no language restriction applied.
Type of studies, inclusion and exclusion criteria
Following the PICOS (participants, intervention, controls, outcomes, study design) criteria, we included studies assessing:
P: Healthcare workers working with COVID-19 patients.
I: None.
C: Non-healthcare workers during the COVID-19 pandemic.
O: Number/prevalence of ED.
S: Observational (case–control, cross-sectional).
All retrospective, cross-sectional or prospective studies reporting the prevalence of ED in healthcare workers working with COVID-19 patients and non-healthcare workers during the COVID-19 pandemic were included. Studies were excluded if they had no data on prevalence of ED or if ED was related to other diseases.
Data extraction and statistical analyses
For each eligible study, two independent investigators (NV, DP) extracted: name of the first author and year of publication, setting, sample size, being a healthcare working or not, mean age of the population, % ED.
Outcomes
The primary outcome was the prevalence of ED in healthcare workers working directly with COVID-19 patients and non-health care workers during the COVID-19 pandemic.
Analysis
Due to the anticipated heterogeneity, a random-effects model was conducted, using the method proposed by DerSimonian and Laird [9]—weighting cases using the inverse of the variance, calculating prevalence rates with 95% confidence intervals (CIs). Using Comprehensive Meta-Analysis Version 3 [10], we calculated the prevalence rates of ED in healthcare professionals working with COVID-19 patients and non-healthcare professionals living with COVID-19 restrictions.
The meta-analysis was conducted in the following steps. (1) Prevalence rates of ED were calculated with 95% CIs using total ns and event ns, or means with 95% CIs. (2) Heterogeneity was assessed with the I2 statistic for all analyses, with 0–50% being classified as low, 50–75% moderate, and > 75% high heterogeneity [11]. (3) As recommended by Sterne and colleagues [12], if the meta-analysis exceeded 10 studies, publication bias was assessed with the Begg-Mazumdar Kendall’s tau [13] and Egger bias test [14]. If publication bias was found, then we used the trim-and-fill adjusted analysis to remove the most extreme small studies from the positive side of the funnel plot and effect sizes re-calculated, until the funnel plot was symmetrical with the new effect size [15].
Assessment of study quality
Two independent authors (DP, MT) assessed the quality of studies using the Newcastle–Ottawa Scale (NOS) [16]. The NOS assigns a maximum of 9 points based on three quality parameters: selection, comparability, and outcome. As per the NOS grading in past reviews, we graded studies as having a high (< 5 stars), moderate (5–7 stars) or low risk of bias (≥ 8 stars) [17].
Assessment of the certainty of evidence
To ascertain the certainty of the evidence, the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework was used [18].
Results
Literature search
As shown in Supplementary Fig. 1, we initially found 52 possibly eligible articles. After removing 44 papers through the title/abstract screening, 8 were retrieved as full text. Of the 8 full text, two studies were excluded because of a lack of data on ED prevalence, leaving six studies to be included in the systematic review and meta-analysis [19–23].
Descriptive data
The six studies included a total of 1908 males, 1653 non-healthcare workers during the COVID-19 pandemic and 255 healthcare workers located in COVID-19 departments. The descriptive characteristics of the included studies are reported in Table 1.
Table 1.
Descriptive characteristics of the included studies
| Author (year) | Country | Area | Setting | Sample size | Mean age (SD) or range | ED prevalence | NOS |
|---|---|---|---|---|---|---|---|
| Bulut (2021) [19] | Turkey | Middle East | COVID healthcare worker | 159 | 19–55 | 131/159 | 6 |
| Culha (2020) [20] | Turkey | Middle East | COVID healthcare worker | 96 | 30.6 (5.9) | 38/96 | 7 |
| Fang (2021) [21] | China | Asia | Non COVID-19 healthcare worker | 251 | NR | 80/251 | 7 |
| Mollaioli (2021) [22] | Italy | Europe | Non COVID-19 healthcare worker | 985 | 35.9 (11) | 182/985 | 7 |
| Omar (2021) [23] | Egypt | Africa | Non COVID-19 healthcare worker | 217 | NR | 69/217 | 7 |
| Bulut (2021) [19] | Turkey | Middle East | Non COVID-19 healthcare worker | 200 | 18–55 | 101/200 | 6 |
ED erectile dysfunction, NOS Newcastle–Ottawa Scale
Prevalence of ED
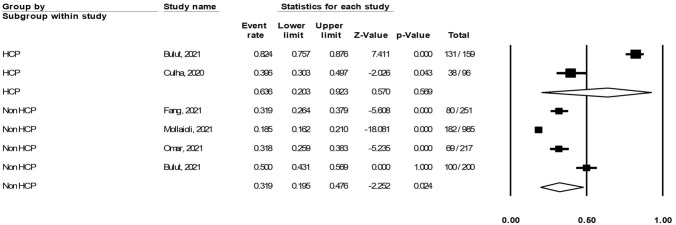
The pooled prevalence of ED in healthcare professionals working with COVID-19 patients was 63.6% (95% CI 20.3–92.3%; I2 = 97.75%), while the pooled prevalence of ED in males living during the COVID-19 pandemic was 31.9% (95% CI 19.5–47.6%; I2 = 96.69%). Figure 1 shows this information graphically.
Fig. 1.
Prevalence of erectile dysfunction in healthcare workers working with COVID-19 patients and males living in an area with COVID restrictions
Publication bias
As no single analysis exceeded ten studies, no publication bias test was performed.
Risk of bias
The risk of bias, evaluated through the NOS, is fully reported in Table 1 as a total score. The median quality of the studies was 6.7 (range: 5–9), indicating an overall more than satisfactory quality of the included studies.
Certainty of evidence
Because of the limited number of studies, and high heterogeneity, the certainly of this evidence has been rated as moderate.
Discussion
The present study is the first explorative systematic review to investigate the impact of COVID-19 on ED. The prevalence of ED in healthcare professionals working with COVID-19 patients was double when compared to non-healthcare working men who were living under COVID-19 restrictions. The high rate of ED in healthcare workers is likely a consequence of the heavy workload and stressful environment experienced during the COVID-19 pandemic. For example, data suggest that during periods where the number of COVID-19 infections were at their highest, hospitals were running at maximum or over-capacity [24]. Indeed, there is increasing evidence showing the negative impact of acute and chronic stressors on erectile function [25]. Moreover, stress and anxiety may trigger a vicious cycle with ED as they can be the cause of ED and, in turn, ED may increase these symptoms [19]. Interestingly, in a study during the H7N9 epidemic, authors showed that anxiety levels were highest in healthcare workers [26]. Similarly, during the SARS epidemic, social and mental health of healthcare workers were observed to decline [27].
An additional factor impacting on general sexual health and, thus, on ED could be fear of COVID-19 infection, specifically transmission during sexual intercourse. To date, there still is a lot to understand in relation to COVID-19 epidemiology, life course, infectiveness and this, added to frequent fake news circulating, leads to the insecurity regarding the safe behaviour to adopt. Other important aspects related to ED are sexual desire, foreplay, sexual frequency and satisfaction that have been observed to decline during the COVID-19 pandemic [20–22]. In particular, sexual frequency has been reported as significantly related to ED; men who have less frequent sexual intercourse have less partner time, less intimacy and higher ED prevalence [21]. Interestingly, during the COVID-19 pandemic, people with a stable relationship had an advantage over those with occasional relationships [21] and men who could maintain sexual activity during the pandemic had lower psychological distress [22].
The results of this preliminary systematic review should be considered in light of its limitations. First, the limited number of studies prevents conclusive indication. Moreover, none of the studies reported on the hormonal profile, smoking, metabolic profile and drugs abuse that could be useful to have a more complete picture of the ED pathophysiological mechanism. Finally, a limited number of studies took into consideration other aspects related to ED, such as sexual desire and orgasmic function.
Findings from the present study suggest that it is mandatory to facilitate sexual health both among healthcare workers working with COVID-19 patients and men during the COVID-19 pandemic. To reduce workload and workplace stress among healthcare professionals, possible options such as telemedicine should be utilised. Moreover, the New York City Health Department has developed guidelines for safe sex practices during the COVID-19 outbreak, namely suggesting to (a) reduce the number of partners; (b) reduce or not to have foreplay; (c) to provide hand hygiene before and after sexual intercourse and; (d) to use male condoms as a method of protection for a safe sexual intercourse [28].
In conclusion, considering the impact of COVID-19 on sexual health and in particular on ED, it is important to provide adequate psychological support systems and to promote quality of life with particular attention to sexual life.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Conceptualisation and design: DP, NV, IG and LS. Acquisition of Data: SI, PS, MT, LB and AK. Analysis and interpretation of data: MAT, LM, MT, JMM and P-CI. Drafting the article:YB, LM, DTMD, JIS, AMC, JMOL and RAG. Revising article for intellectual content: All authors. Final approval of the completed article: All authors.
Funding
None to declare.
Declarations
Conflict of Interest
All authors declare no conflict of interest.
Research involving human participants and/or animals
Not applicable.
Informed consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Di Gennaro F, Pizzol D, Marotta C, Antunes M, Racalbuto V, Veronese N, Smith L. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int J Environ Res Public Health. 2020;17(8):2690. doi: 10.3390/ijerph17082690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen SF, Stevenson J, Lazuras L, Akram U. The role of the COVID-19 pandemic in altered psychological well-being, mental health and sleep: an online cross-sectional study. Psychol Health Med. 2021;20:1–9. doi: 10.1080/13548506.2021.1916963. [DOI] [PubMed] [Google Scholar]
- 3.Smith L, Yang L, Veronese N, Soysal P, Stubbs B, Jackson SE. Sexual activity is associated with greater enjoyment of life in older adults. Sex Med. 2019;7(1):11–18. doi: 10.1016/j.esxm.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson SE, Yang L, Koyanagi A, Stubbs B, Veronese N, Smith L. Declines in sexual activity and function predict incident health problems in older adults: prospective findings from the English longitudinal study of ageing. Arch Sex Behav. 2020;49(3):929–940. doi: 10.1007/s10508-019-1443-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacob L, Smith L, Butler L, Barnett Y, Grabovac I, McDermott D, Armstrong N, Yakkundi A, Tully MA. Challenges in the practice of sexual medicine in the time of COVID-19 in the United Kingdom. J Sex Med. 2020;17(7):1229–1236. doi: 10.1016/j.jsxm.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pizzol D, Demurtas J, Stubbs B, Soysal P, Mason C, Isik AT, Solmi M, Smith L, Veronese N. Relationship between cannabis use and erectile dysfunction: a systematic review and meta-analysis. Am J Mens Health. 2019;13(6):1557988319892464. doi: 10.1177/1557988319892464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100–e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 9.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 10.Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta analysis. Englewood: Biostat; 2013. [Google Scholar]
- 11.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 12.Sterne JA, Egger M, Moher D (2008) Addressing Reporting Biases. In: Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. John Wiley & Sons, Inc, pp 297–333. 10.1002/9780470712184.ch10
- 13.Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–101 [PubMed]
- 14.Egger M, Smith GD, Schneider M, Minder C. Bias in meta analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 16.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2015) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses
- 17.Luchini C, Stubbs B, Solmi M, Veronese N. Assessing the quality of studies in meta-analysis: advantages and limitations of the Newcastle Ottawa Scale. World J Meta-Anal. 2017;5:1–48. [Google Scholar]
- 18.Reed Siemieniuk and Gordon Guyatt. What is GRADE? BMJ Best practice. https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/. Accessed April 2021
- 19.Bulut EC, Ertaş K, Bulut D, Koparal MY, Çetin S. The effect of COVID-19 epidemic on the sexual function of healthcare professionals. Andrologia. 2021;53(3):e13971. doi: 10.1111/and.13971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Culha MG, Demir O, Sahin O, Altunrende F. Sexual attitudes of healthcare professionals during the COVID-19 outbreak. Int J Impot Res. 2021;33(1):102–109. doi: 10.1038/s41443-020-00381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fang D, Peng J, Liao S, Tang Y, Cui W, Yuan Y, Wu D, Hu B, Wang R, Song W, Gao B, Jin L, Zhang Z. An Online Questionnaire Survey on the Sexual Life and Sexual Function of Chinese Adult Men During the Coronavirus Disease 2019 Epidemic. Sex Med. 2021;9(1):100293. doi: 10.1016/j.esxm.2020.100293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mollaioli D, Sansone A, Ciocca G, Limoncin E, Colonnello E, Di Lorenzo G, Jannini EA. Benefits of sexual activity on psychological, relational, and sexual health during the COVID-19 breakout. J Sex Med. 2021;18(1):35–49. doi: 10.1016/j.jsxm.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Omar SS, Dawood W, Eid N, Eldeeb D, Munir A, Arafat W. Psychological and sexual health during the COVID-19 pandemic in Egypt: are women suffering more? Sex Med. 2021;9(1):100295. doi: 10.1016/j.esxm.2020.100295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rocks S and Idriss O. Did hospital capacity affect mortality during the pandemic’s first wave? https://www.health.org.uk/news-andcomment/charts-and-infographics/did-hospital-capacity-affect-mortality-during-the-pandemic. Accessed May 2021
- 25.Brotto L, Atallah S, Johnson-Agbakwu C, Rosenbaum T, Abdo C, Byers ES, Graham C, Nobre P, Wylie K. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sex Med. 2016;13(4):538–571. doi: 10.1016/j.jsxm.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 26.Tang L, Pan L, Yuan L, Zha L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int J Nurs Sci. 2016;4(1):63–67. doi: 10.1016/j.ijnss.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen NH, Wang PC, Hsieh MJ, Huang CC, Kao KC, Chen YH, Tsai YH. Impact of severe acute respiratory syndrome care on the general health status of healthcare workers in taiwan. Infect Control Hosp Epidemiol. 2007;28(1):75–79. doi: 10.1086/508824. [DOI] [PubMed] [Google Scholar]
- 28.Sex and COVID-19 Fact Sheet The NYC Health Department 2020. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-sexguidance.pdf. Accessed May 2021
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.