Abstract
Background: The aim of this study was to assess factors associated with long-term patient-reported functional, pain, and satisfaction scores in patients who underwent (Bowers) hemiresection interposition technique (HIT) arthroplasty of the distal radioulnar joint (DRUJ). The secondary aims were to determine the complication and reoperation rates. Methods: A retrospective study with long-term follow-up of patients undergoing HIT arthroplasty was performed. Demographic, disease, and treatment characteristics were collected for the 66 included patients. Thirty-one patients completed all surveys, which were the Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH), our custom-made HIT arthroplasty questionnaire, Numeric Rating Scale (NRS) for pain, and NRS for satisfaction. The mean interval between surgery and follow-up by means of questionnaires was 8.6 ± 3.4 years. Results: The mean QuickDASH score was 31.0 ± 20.2. The mean score of the HIT arthroplasty questionnaire was 2 ± 2. The median NRS for pain was 1 (interquartile range [IQR], 0-3), and the median NRS for satisfaction was 9 (IQR, 8-10). The complication rate and reoperation rate were 14% and 8%, respectively. Conclusion: Overall, patients expressed satisfaction with HIT arthroplasty, despite a mean QuickDASH score of 31.0. In our cohort, patients with inflammatory arthritis had higher satisfaction and lower pain scores. Patients who had prior trauma, prior surgery, or DRUJ subluxation are generally less satisfied. Men, older patients, and posttraumatic patients had higher long-term pain scores; however, posterior interosseous nerve neurectomy is associated with improved pain scores. Our findings support the use of HIT arthroplasty in patients with inflammatory arthritis.
Keywords: ulnar resection, arthritis, hemiresection interposition arthroplasty, Bowers arthroplasty, DASH, pain, satisfaction
Introduction
Arthritis of the distal radioulnar joint (DRUJ) is one of the causes of ulnar-sided wrist pain.1-3 Etiologies include inflammatory arthritis, posttraumatic arthritis, and primary osteoarthritis2,4 Options for the treatment of DRUJ arthritis include resection of the entire ulnar head (Darrach resection), fusion of the DRUJ combined with a segmental resection of the ulna just proximal to the DRUJ (Sauvé-Kapandji resection), partial resection of the ulnar joint surface with interposition of soft tissue using tendons or joint capsule (hemiresection interposition technique [HIT] arthroplasty), or DRUJ replacement (eg, Aptis-Scheker replacement).2,5-8
The theoretical advantage of HIT arthroplasty compared with procedures such as the Darrach and Sauvé-Kapandji is the preservation of the attachment of the triangular fibrocartilage complex (TFCC) to the ulnar styloid process. Using an oblique distal ulnar resection, the DRUJ remains stable, while the arthritic portion of the DRUJ is removed.6,9,10 However, some warn that this technique should be used with caution in patients with inflammatory or posttraumatic arthritis because the TFCC may be structurally incompetent. In cases where the TFCC is compromised, stylocarpal impingement is a potential complication.4,11
There is a paucity of studies evaluating the overall long-term outcomes of HIT arthroplasty.3,6,7,11 Therefore, the aim of this study was to assess factors associated with long-term patient-reported functional, pain, and satisfaction scores in patients who underwent an HIT arthroplasty of the DRUJ. The secondary aims were to describe our complication and reoperation rates.
Methods
A priori, the institutional review board (IRB) granted permission for retrospective data collection (IRB #1999P008705). We performed a retrospective multicenter study with long-term follow-up of all patients undergoing HIT arthroplasty for DRUJ arthritis at 1 of 3 large urban area hospitals (2 large academic hospitals and 1 community hospital tied to an academic hospital) from January 2001 until January 2016. We identified patients from the Institutions’ Research Patient Data Registry using multiple Current Procedural Terminology (CPT) codes (25105, 25107, 25119, 25240, 25332, 25337, 25360, 25676, 25830). Patients eligible for inclusion underwent HIT arthroplasty that was confirmed either by operative note or by radiographs. The surgeries were performed according to the HIT first described by Bowers.4,6
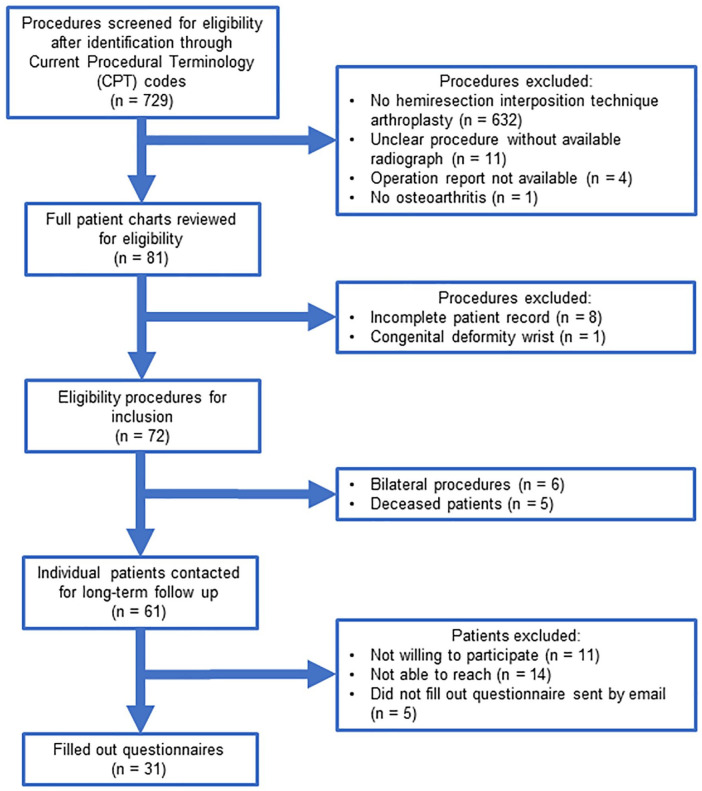
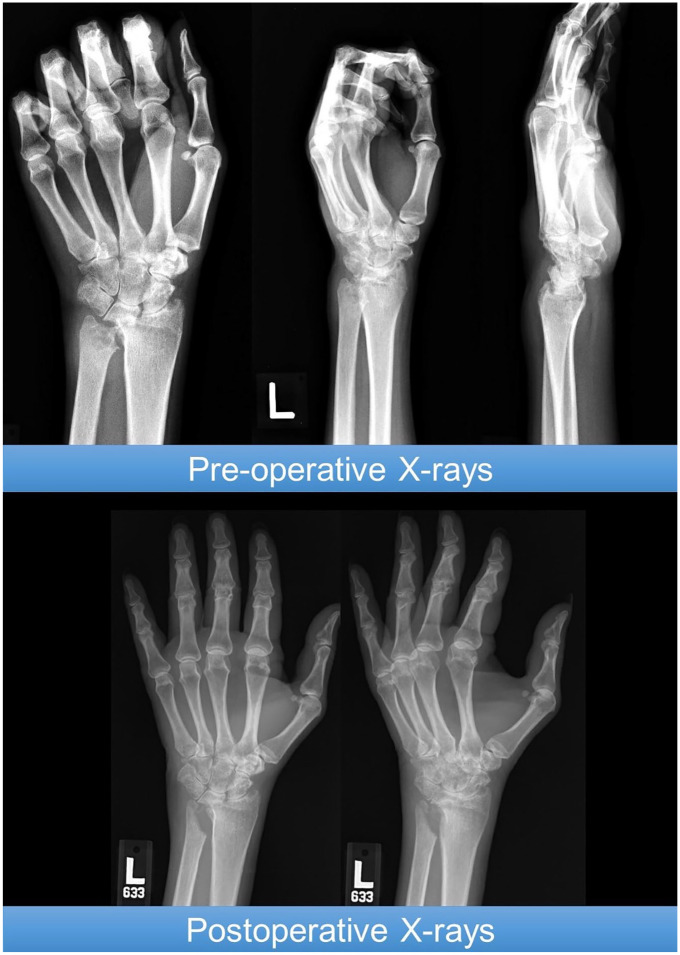
After exclusion of patients younger than 18 years at the time of surgery or patients with DRUJ dysfunction resulting from congenital causes, the cohort consisted of 66 patients (Figure 1). The mean age of the population at the time of surgery was 58 ± 15 years. The majority were women (n = 57, 86%) (Table 1). The most common indication for surgery was inflammatory arthritis (n = 55, 83%), followed by posttraumatic arthritis (n = 9, 14%) (Supplement 1). On radiographic evaluation, arthritic change was visible in 42 of 50 patients (84%), and 24 of 47 patients with radiographs suitable for assessing subluxation (51%) had subluxation prior to surgery (Table 2). There were 8 patients (16%) for whom arthritic changes were not evident on the radiograph; these patients were diagnosed based on their symptoms and physical examination. Fourteen patients (22%) had prior surgery on the affected wrist, and 9 patients (14%) had a prior fracture of the affected wrist. Supplemental procedures in addition to HIT arthroplasty included posterior interosseous nerve (PIN) neurectomy (n = 48, 72%), tenosynovectomy (21, 32%), tendon transfer (n = 21, 32%), and DRUJ ligament reconstruction (n = 4, 6%) (Table 2). After HIT arthroplasty, patients had a median in-clinic follow-up of 8 months (interquartile range [IQR], 4-18). See Figures 2 and 3 for examples of radiographs before and after the surgery for this procedure.
Figure 1.
Flowchart of inclusion and exclusion of patients with hemiresection interposition arthroplasty.
Table 1.
Patient Demographics of Hemiresection Interposition Arthroplasty.
| Patient Characteristics | Total n = 66 (100%) |
Responder n = 31 (51%) |
DASH score P value | HIT arthroplasty Questionnaire P value | NRS pain P value | NRS satisfaction P value |
|---|---|---|---|---|---|---|
| Age, mean ± SD | 58 ± 15 | 58 ± 13 | .362a | .802a | .024 b | .655b |
| Sex, No. (%) | .250c | .010 c | .005 d | .641d | ||
| Male | 9 (14) | 3 (10) | ||||
| Female | 57 (86) | 28 (90) | ||||
| Body mass index, kg/m2,* median (IQR) | 26 (23-30) | 26 (22-30) | .123b | .320b | .245b | .733b |
| Comorbidities, No. (%) | ||||||
| Diabetes mellitus† | 8 (12) | 3 (10) | .731c | .183c | .272d | .883d |
| Osteoporosis† | 18 (28) | 6 (20) | .352c | .840c | .010 d | .438d |
| Tobacco use reported in chart,‡ No. (%) | 5 (8) | 3 (10) | .159c | .619c | .732d | .133d |
| Alcohol dependency reported in chart,§ No. (%) | 2 (3) | 0 (0) | NA | NA | NA | NA |
| Heavy manual labor as occupation,** No. (%) | 5 (9) | 2 (8) | .322c | .243c | .624d | .149d |
Note. DASH = Disabilities of the Arm, Shoulder and Hand; HIT = hemiresection interposition technique; IQR = interquartile range; NRS = Numeric Rating Scale.
Missing cases: *11 missing; †1 missing; ‡3 missing; §5 missing; **10 missing.
Statistical test used: aPearson correlation coefficient, bSpearman rank correlation coefficient, cIndependent t test, and dMann-Whitney U test. Bold font denotes significant P value.
Table 2.
Preoperative and Procedural Characteristics of Hemiresection Interposition Arthroplasty.
| Preoperative and Procedural Characteristics | Total n = 66 (100%) |
Responder n = 31 (51%) |
DASH score P value | HIT arthroplasty questionnaire P value | NRS pain P value | NRS satisfaction P value |
|---|---|---|---|---|---|---|
| Dominant hand affected,* No. (%) | 35 (61) | 13 (48) | .671a | .392a | .075b | .397b |
| Prior surgery on ipsilateral wrist,† No. (%) | 14 (22) | 7 (23) | .918a | .616a | .052b | .030 b |
| Prior ipsilateral wrist fracture, No. (%) | 9 (14) | 4 (13) | .428a | .361a | .010 b | .043 b |
| Distal radius fracture | 5 (56) | 3 (75) | ||||
| Distal radius fracture with DRUJ dislocation | 1 (11) | 0 (0) | ||||
| Ulna fracture | 2 (22) | 1 (25) | ||||
| Unknown | 1 (11) | 0 (0) | ||||
| Radiology, No. (%) | ||||||
| Visible arthritic changes‡ | 42 (84) | 20 (80) | .877a | .657a | .175b | .417b |
| Subluxation§ | 24 (51) | 9 (38) | .020 a | .931a | .875b | .010 b |
| Indication for surgery, No. (%) | .196c | .283c | .004 d | .305d | ||
| Inflammatory arthritis | 55 (83) | 25 (81) | ||||
| Posttraumatic arthritis | 9 (14) | 5 (16) | ||||
| Other | 2 (3) | 1 (3) | ||||
| Concomitant wrist diagnosis at time of surgery,† No. (%) | 43 (66) | 20 (65) | .875a | .469a | .878b | .111b |
| Tendon rupture | 23 (35) | 10 (32) | .715a | .564a | .280b | .049 b |
| Dorsal (teno)synovitis | 19 (29) | 8 (26) | .818a | .041 a | .211b | .594b |
| Nonunion/Malunion | 2 (3) | 2 (6) | .646a | .857a | .029 b | .167b |
| Caput ulnae syndrome | 2(3) | 1 (3) | NA | NA | NA | NA |
| DRUJ dislocation | 2 (3) | 1 (3) | NA | NA | NA | NA |
| Other** | 10 (15) | 6 (19) | .928a | .557a | .352b | .391b |
| Concomitant procedures performed, No. (%) | 65 (98) | 31 (100) | ||||
| Total wrist replacement | 6 (9) | 2 (6) | .233a | .827a | .171b | .897b |
| Wrist arthrodesis | 20 (30) | 12 (39) | .322a | .281a | .517b | .572b |
| Radiolunate arthrodesis | 4 (6) | 1 (3) | NA | NA | NA | NA |
| Carpectomy | 6 (9) | 4 (13) | .973a | .361a | .380b | .569b |
| DRUJ reconstruction | 4 (6) | 1 (3) | NA | NA | NA | NA |
| Tendon transfer | 21 (32) | 10 (32) | .715a | .564a | .280b | .049 b |
| Posterior interosseous neurectomy | 48 (72) | 24 (77) | .243a | .419a | .007 b | .224b |
| (Teno)synovectomy | 46 (70) | 20 (65) | .833a | .605a | .210b | .019 b |
| Other†† | 15 (25) | 3 (10) | .597a | .577a | .213 | .085b |
Note. DASH = Disabilities of the Arm, Shoulder and Hand; DRUJ = distal radioulnar joint; HIT = hemiresection interposition technique; NRS = Numeric Rating Scale.
Missing cases: *9 missing; †1 missing; ‡16 missing; §19 missing.
Bone spicules, carpal tunnel release, dislocation of hand joints other than DRUJ, joint destruction other than DRUJ; ††Thumb arthroplasty, bursectomy, carpal tunnel release, capsulodesis, intercarpal fusion, open reduction and internal fixation, distal radius osteotomy, plate removal, tendon release, ulnar shortening osteotomy.
Statistical tests used: aIndependent t test, bMann-Whitney U test, cAnalysis of variance, dKruskal-Wallis test. Bold font denotes significant P value.
Figure 2.
Preoperative and postoperative radiographs of a patient undergoing hemiresection interposition arthroplasty for inflammatory arthritis of the distal radioulnar joint. This patient had no complications and did not undergo reoperation.
Figure 3.
Preoperative and postoperative radiographs of a patient undergoing hemiresection interposition arthroplasty combined with open reduction and internal fixation for posttraumatic arthritis of the distal radioulnar joint. This patient had a fracture a year prior to the surgery for which the patient was treated conservatively. This patient had no complications and did not undergo reoperation.
Explanatory Variables and Outcome Measures
For all identified patients, demographic characteristics (age, sex, dominant hand, body mass index [BMI], diabetes mellitus, smoking status, alcohol dependency, heavy manual labor as occupation), disease characteristics (affected wrist side, type of arthritis, prior ipsilateral wrist surgery or fracture), and treatment characteristics (concomitant wrist diagnosis at the time of surgery, concomitant procedures performed during surgery, follow-up time, complications and unplanned reoperations affecting the ulna) were extracted from the hospital’s electronic medical charts. In the case of bilateral HIT arthroplasties, only data from the first procedure were analyzed to avoid violating the statistical assumption of independence. Furthermore, 2 researchers (F.N., S.H.W.L.V.) extracted all radiographs and independently assessed each radiograph for the presence of arthritis and ulnar subluxation. When no consensus could be reached, the senior author was consulted until consensus was reached.
Five patients passed away during the follow-up period, which resulted in 61 potential subjects available for contact. Patients who responded that they were willing to participate or did not respond within 2 weeks were contacted by telephone to administer the questionnaires. Multiple attempts were made to obtain the highest possible response rate for each patient and reduce selection bias caused by nonresponse. If preferred, the questionnaires were sent by mail through a secured survey system. Thirty-one patients participated in the study, reflecting a response rate of 51% (Figure 1). The mean interval between the surgery and the survey was 8.6 ± 3.4 years (range, 2.8-13.9 years).
Our primary outcome measure was the Quick Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire score and our custom-made HIT arthroplasty questionnaire. Our secondary outcome measures were Numeric Rating Scale (NRS) for pain and NRS for patient’s satisfaction. The QuickDASH consists of 11 questions about daily activities and symptoms, each scored on a scale of 1 (no disability) to 5 (severe disability). These scores are transformed to a scale of 0 to 100, reflecting patients’ perception of physical arm function and symptoms. A higher score indicates more arm-related disabilities experienced by the patient.12 The HIT arthroplasty questionnaire was developed by our department to assess the common symptoms and complaints related to the DRUJ.1-3 The full questionnaire is available in Table 3. The score ranges between 0 and 6, with a high score indicating that there are more DRUJ symptoms still present after surgery. The NRS for pain measures the average amount of pain a patient experiences during a regular day on a scale of 0 (no pain) to 10 (worst pain imaginable).13 The NRS for patient’s satisfaction measures satisfaction with the given treatment on a scale of 0 (completely unsatisfied) to 10 (very satisfied).
Table 3.
Results of Hemiresection Interposition Arthroplasty Questionnaire.
| Questions | n = 31 |
|---|---|
| Do you experience more swelling at the ulnar side of your wrist and/or forearm which was operated on compared with your other wrist and/or forearm? | 6 (19%) |
| Do you experience weakness of the wrist and/or forearm which was operated on (eg, dropping objects, unable to carry heavy groceries with operated hand)? | 18 (58%) |
| Do you feel an increase in pain located at the ulnar side of your wrist and/or forearm which was operated on during rotation of your forearm (eg, changing a light bulb, turning a key)? | 11 (35%) |
| Do you feel or hear a “click” over the ulnar side of your wrist or/and forearm which was operated on during rotation of your forearm (eg, changing a light bulb, turning a key)? | 8 (26%) |
| Do you experience the sensation of instability of the wrist and/or forearm that was operated? | 7 (23%) |
| Does the wrist and/or forearm you were operated on cause you any limitations in your daily activity (compared with before the surgery or before the onset of your wrist complaints)? | 19 (61%) |
| Total score of hemiresection interposition arthroplasty questionnaire, mean ± SD | 2 ± 2 |
Statistical Analysis
Continuous variables were presented as mean ± standard deviation if normally distributed or as median with IQR if nonnormally distributed. Categorical variables were presented as frequencies and percentages. Missing data were handled using pairwise deletion to reduce information bias. Bivariate analyses were performed to identify associations between our explanatory variables and outcome variables (QuickDASH score, HIT arthroplasty questionnaire, NRS for pain score, NRS for patient’s satisfaction score). For bivariate analyses, independent t test was used for dichotomous explanatory variables, one-way analysis of variance for categorical explanatory variables, and Pearson correlation coefficient for continuous explanatory variables. Based on normality, the nonparametric equivalent of these tests was used (Mann-Whitney test, Kruskal-Wallis test, Spearman rank correlation coefficient, respectively). A multivariable linear regression was attempted to identify factors independently associated with a higher QuickDASH score; therefore, the most clinically relevant variables with a value of P < .2 were imputed in the model. This was not attempted for the other questionnaires due to the limited and, therefore, not clinically relevant spread of outcomes on the continuous scales. A value of P < .05 was considered statistically significant. All analyses were performed with STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, Texas: StataCorp LP).
Results
Clinical Outcomes
The complication rate was 14% (n = 9). Complications included stylocarpal impingement (n = 2), wound complications (n = 2), ulnar exostoses (n = 1), ulnar subluxation (n = 1), carpus subluxation (n = 1), tendon rupture (n = 1), and necrotizing fasciitis (n = 1). The reoperation rate was 8% (n = 5). Reoperations included a Darrach resection to treat stylocarpal impingement (n = 2), a Darrach resection and tendon repair to treat persistent complaints and an extensor tendon rupture (n = 1), hemiarthroplasty revision to treat a distal ulnar exostosis (n = 1), and surgical exploration with irrigation and debridement for necrotizing fasciitis (n = 1).
Patient-Reported Outcomes
The mean QuickDASH score was 31.0 ± 20.2 (range, 0-65.9). Distal radioulnar joint subluxation visible on radiographs prior to surgery was associated with a higher QuickDASH score (41.9 ± 20.0 vs 24.1 ± 14.6; P = .020). Imputation of BMI, smoking, posttraumatic arthritis as surgery indication, and subluxation on radiographic evaluation in a multivariable linear regression model did not identify a variable independently associated with the QuickDASH score (Supplement 2).
The mean HIT arthroplasty questionnaire score was 2 ± 2 (range, 0-5). Male sex (2 ± 2 vs 5 ± 1; P = .010) and dorsal tenosynovectomy (1 ± 1 vs 3 ± 2; P = .041) were associated with inferior scores. The most common persistent wrist symptom was the experience of weakness of the wrist after surgery (n = 18, 58%) (Table 3).
The median NRS for pain was 1 (IQR, 0-3; range, 0-10). Higher pain scores were associated with older age (P = .024), male sex (8 [IQR, 4-10] vs 0 [IQR, 0-2]; P = .005), presence of osteoporosis (1 [IQR, 0-4] vs 0 [IQR, 0-0]; P = .010), prior ipsilateral wrist fracture (6 [IQR, 3-9] vs 0 [IQR, 0-2]; P = .010), posttraumatic arthritis as indication for surgery (5 [IQR, 4-8] vs 0 [0-2]; P = .004), or nonunion or malunion as concomitant diagnosis at the time of surgery (7 [IQR, 4-10] vs 0 [IQR, 0-2]; P = .029). Patients in whom PIN resection was performed had lower pain scores (0 [IQR, 0-2] vs 4 [IQR, 1-8]; P = .007).
The median NRS for satisfaction was 9 (IQR, 8-10; range, 0-10). Twenty-nine patients (94%) had a satisfaction score greater than 7. In bivariate analysis, patients who had prior surgery on the ipsilateral wrist (9 [IQR, 8-10] vs 10 [IQR, 10-10]; P = .030), prior fracture of the ipsilateral wrist (9 [IQR, 8-10] vs 10 [IQR, 10-10]; P = .043), subluxation visible on radiographic evaluation (9 [IQR, 7-9] vs 10 [IQR, 9-10]; P = .010), tendon rupture at the time of surgery (9 [IQR, 7-10] vs 10 [IQR, 9-10]; P = .049), tendon repair as concomitant procedure (9 [IQR, 7-10] vs 10 [IQR, 9-10]; P = .049), and who did not undergo tenosynovectomy as concomitant procedure (9 [IQR, 8-10] vs 10 [IQR, 10-10]; P = .019) were less satisfied (Tables 1 and 2).
The occurrence of complications or reoperations did not appear to influence the patient-reported outcomes.
Discussion
This study investigated the factors associated with long-term patient-reported functional, pain, and satisfaction scores and to determine the rate of complications and reoperations of patients who underwent an HIT arthroplasty. We found a mean QuickDASH of 31.0, an NRS for pain of 1, and an NRS for satisfaction of 9. The complication rate and reoperation rate during the 8.6 years of follow-up were, respectively, 14% and 8%.
This study is limited by its retrospective nature: First, the complication rate and reoperation rate might be underreported due to patients seeking care for new or persistent wrist complaints at a hospital outside our records. Based on our experience with referral patterns within our institutions, this is uncommon. We found that 2 of our included patients switched care from one institution to another institution within our system. Second, CPT codes were used to identify patients; however, no specific CPT codes are available for HIT arthroplasty. We used 9 different CPT codes and manual chart review to try to capture as many cases as possible. Third, our results are likely influenced by selection bias because it is possible that those who chose not to respond had a different outcome than those who chose to participate. However, when evaluating the demographic, preoperative, and procedure characteristics, the responder cohort appears similar to the initial cohort. Finally, the DASH scores reflect not only HIT arthroplasty but also the global problems of the wrist, including inflammatory arthritis and posttraumatic sequelae of the radiocarpal joint.
The study also has some strengths: It is a relatively large cohort of patients who underwent HIT arthroplasty with a considerably long follow-up of 8.6 years. There were 9 surgeons performing this procedure, all of whom were attending-level surgeons. We used a specific HIT arthroplasty questionnaire to assess symptoms postoperatively. Although this is not validated, we asked reasonable questions that can be applied in practical manner to interpret symptoms that are not captured by other outcome measures.
Van Schoonhoven et al14 found an average DASH score of 35 with an average follow-up of 34 months, which is a similar finding compared with this study. In our study, we found that preoperative subluxation on radiograph was a predictive factor for worse QuickDASH scores because patients with subluxation had a score of 41.9 compared with 14.6 in patients without preoperative subluxation. Preoperative subluxation likely indicates preoperative joint instability and TFCC incompetence.15 Compared with the Darrach or Sauvé Kapandji procedure, DASH scores in patients with posttraumatic or degenerative arthritis vary between 17-26 and 23-28, respectively.16-19
The survey specifically made for patients with DRUJ symptoms showed that 58% of the patients still experienced weakness of the wrist. Previous studies showed slight increases in grip strength postoperatively, but this eventually never matches the strength of the contralateral side, possibly explaining why patients still report on experiencing weakness of the wrist.9,20,21 In our study, 23% of the patients reported instability of the wrist, which is in line with previous described rates for HIT arthroplasty.20
We found that the mean NRS for pain was 1 (IQR, 0-3). This is a very low score compared with the mean DASH score of 31; however, most patients we spoke to were satisfied with the procedure because it reduced pain. Previous studies report that 54% to 94% of patients described no remaining pain at follow-up.6,7,22-24 Lee et al11 reported an NRS for pain of 1.7 in a cohort of only rheumatoid arthritis patients undergoing HIT arthroplasty, whereas 2 other studies14,21 found pain scores of 3.9 and 5.4 in cohorts only or predominately consisting of patients with posttraumatic arthritis. In our cohort, patients with posttraumatic arthritis had more frequently a higher NRS for pain (NRS of 5 compared with 0). Patients with posttraumatic arthritis are usually younger (previous described ages between 39 and 53 years), more active, and did not have complaints of the wrist prior to the trauma and also have different outcome expectations.6,11,14,23 These findings are similar for patients who underwent a Darrach procedure, where patients with posttraumatic arthritis describe more postoperative pain at long-term follow-up compared with those with inflammatory arthritis.25
We found that PIN neurectomy was associated with reduced pain. Patients with PIN neurectomy scored 0 on the NRS for pain compared with a score of 4 by patients who did not undergo PIN neurectomy. It is unclear whether this procedure improves outcomes because of denervation of the radiocarpal joint and helps resolve other pathology, or PIN neurectomy denervates the DRUJ.26-28 It is also possible the PIN neurectomy is a surrogate for other technical factors that are unable to be captured in the data available.
Ninety-four percent of the patients reported they were satisfied, which is in line with prior studies of satisfaction (84%-93%).11,24 Two previous studies assessing the NRS for satisfaction reported scores of 6.4 and 6.9.14,21 One of these studies had a relatively high rate of radioulnar impingements (41%), whereas the other study consisted of mostly relatively young patients with posttraumatic arthritis, resulting in a population with different expectations of the surgery.14,21
Our complication rate was 14%, which is comparable to the reported historical complication rates that vary between 3% and 44%.6,7,23 The reoperation rate is also in line with previous described reoperation rates (0%-13%), with persistent pain and stylocarpal impingement being the primary indications for reoperation.4,7,21,23 Complications in our cohort were mainly related to persistent pain, joint instability, and wound complications. Minami et al had a complication rate of 44% that they attributed to extensor carpi ulnaris tendonitis secondary to retinacular reconstruction performed. Complication rates only assessing stylocarpal impingement vary between 8% and 41%.14,21 In this study, persistent pain due to stylocarpal impingement occurred in 2 patients (3%)—in both cases, a reoperation with the Darrach procedure was performed.
Conclusion
Overall, we found that patients expressed satisfaction with HIT arthroplasty, despite a mean QuickDASH score of 31. In our cohort, patients with inflammatory arthritis had higher satisfaction and pain scores. Patients who had prior trauma, prior surgery, or DRUJ subluxation are generally less satisfied. Men, older patients, and posttraumatic patients have less pain relief; however, PIN neurectomy is associated with improved pain relief. Overall, the indications for HIT arthroplasty should take into account etiology, age, and TFCC status. In addition, PIN neurectomy may be beneficial in improving clinical outcomes.
Supplemental Material
Supplemental material, Supplement_files for Hemiresection Interposition Arthroplasty of the Distal Radioulnar Joint: A Long-term Outcome Study by Femke Nawijn, Svenna H. W. L. Verhiel, Jesse B. Jupiter and Neal C. Chen in HAND
Acknowledgments
The authors acknowledge Dr H. Lee for his statistical assistance.
Footnotes
Supplemental material is available in the online version of the article.
Authors’ Note: All research data are available upon request.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Chen received grants from Miami Device Solutions, OMeGA, and Acumed. All other authors have no conflicts of interest to declare.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Femke Nawijn  https://orcid.org/0000-0001-8390-4483
https://orcid.org/0000-0001-8390-4483
Svenna H. W. L. Verhiel  https://orcid.org/0000-0002-4194-9031
https://orcid.org/0000-0002-4194-9031
Neal C. Chen  https://orcid.org/0000-0001-7527-1110
https://orcid.org/0000-0001-7527-1110
References
- 1.Murray PM.Current concepts in the treatment of rheumatoid arthritis of the distal radioulnar joint. Hand Clin. 2011;27(1):49-55. [DOI] [PubMed] [Google Scholar]
- 2.Glowacki K.Hemiresection arthroplasty of the distal radioulnar joint. Hand Clin. 2005;21(4):591-601. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed SK, Cheung JPY, Fung BK-K, et al. Long term results of matched hemiresection interposition arthroplasty for DRUJ arthritis in rheumatoid patients. Hand Surg. 2011;16(2):119-125. [DOI] [PubMed] [Google Scholar]
- 4.Bowers W.Distal radioulnar joint arthroplasty: current concepts. Clin Orthop Relat Res. 1992;275:104-109. [PubMed] [Google Scholar]
- 5.Srikanth KN, Shahane SA, Stilwell JH.Modified matched ulnar resection for arthrosis of distal radioulnar joint in rheumatoid arthritis. Hand Surg. 2006;11(1-2):15-19. [DOI] [PubMed] [Google Scholar]
- 6.Bowers WH.Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. J Hand Surg Am. 1985;10(2):169-178. [DOI] [PubMed] [Google Scholar]
- 7.Watson HK, Ryu J, Burgess RC.Matched distal ulnar resection. J Hand Surg Am. 1986;11(6):812-817. [DOI] [PubMed] [Google Scholar]
- 8.Scheker LR.Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(9):1639-1644. http://www.ncbi.nlm.nih.gov/pubmed/18984351. Accessed June 10, 2019. [DOI] [PubMed] [Google Scholar]
- 9.Rekant M.Distal ulna arthroplasties. Hand Clin. 2012;28(4):611-615. [DOI] [PubMed] [Google Scholar]
- 10.Sauerbier M, Fujita M, Hahn M, et al. The dynamic radioulnar convergence of the Darrach procedure and the ulnar head hemiresection interposition arthroplasty: a biomechanical study. J Hand Surg Br. 2002;27(4):307-316. [DOI] [PubMed] [Google Scholar]
- 11.Lee CH, Chung US, Lee BG, et al. Long-term results of simple hemiresection arthroplasty in the rheumatoid distal radio-ulnar joint. J Hand Surg Eur Vol. 2013;38(7):719-726. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy CA, Beaton DE, Smith P, et al. Measurement properties of the QuickDASH (Disabilities of the Arm, Shoulder and Hand) outcome measure and cross-cultural adaptations of the QuickDASH: a systematic review. Qual Life Res. 2013;22(9):2509-2547. [DOI] [PubMed] [Google Scholar]
- 13.Williamson A, Hoggart B.Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798-804. [DOI] [PubMed] [Google Scholar]
- 14.Van Schoonhoven J, Kall S, Schober F, et al. The hemiresection-interposition arthroplasty as a salvage procedure for the arthrotically destroyed distal radioulnar joint. Handchir Mikrochir Plast Chir. 2003;35(3):175-180. [DOI] [PubMed] [Google Scholar]
- 15.Zimmerman RM, Jupiter JB.Instability of the distal radioulnar joint. J Hand Surg Eur Vol. 2014;39(7):727-738. [DOI] [PubMed] [Google Scholar]
- 16.Zimmermann R, Gschwentner M, Arora R, et al. Treatment of distal radioulnar joint disorders with a modified Sauvé-Kapandji procedure: long-term outcome with special attention to the DASH questionnaire. Arch Orthop Trauma Surg. 2003;123(6):293-298. [DOI] [PubMed] [Google Scholar]
- 17.Grawe B, Heincelman C, Stern P.Functional results of the Darrach procedure: a long-term outcome study. J Hand Surg Am. 2012;37(12):2475-2480.e1. doi: 10.1016/j.jhsa.2012.08.044. [DOI] [PubMed] [Google Scholar]
- 18.Daecke W, Martini AK, Schneider S, et al. Amount of ulnar resection is a predictive factor for ulnar instability problems after the Sauvé-Kapandji procedure: a retrospective study of 44 patients followed for 1-13 years. Acta Orthop. 2006;77(2):290-297. [DOI] [PubMed] [Google Scholar]
- 19.George MS, Kiefhaber TR, Stern PJ.The Sauvé-Kapandji procedure and the Darrach procedure for distal radio-ulnar joint dysfunction after Colles’ fracture. J Hand Surg Br. 2004;29(6):608-613. [DOI] [PubMed] [Google Scholar]
- 20.Minami A, Iwasaki N, Ishikawa J, et al. Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures. Hand Surg. 2005;10(2-3):243-248. [DOI] [PubMed] [Google Scholar]
- 21.Bain GI, Pugh DMW, MacDermid JC, et al. Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg Am. 1995;20(6):944-950. [DOI] [PubMed] [Google Scholar]
- 22.Imbriglia JE, Matthews D.Treatment of chronic post-traumatic dorsal subluxation of the distal ulna by hemiresection-interposition arthroplasty. J Hand Surg Am. 1993;18(5):899-907. [DOI] [PubMed] [Google Scholar]
- 23.Minami A, Kaneda K, Itoga H.Hemiresection-interposition arthroplasty of the distal radioulnar joint associated with repair of triangular fibrocartilage complex lesions. J Hand Surg Am. 1991;16(6):1120-1125. [DOI] [PubMed] [Google Scholar]
- 24.Faithfull DK, Kwa S.A review of distal ulnar hemi-resection arthroplasty. J Hand Surg Br. 1992;17(4):408-410. [DOI] [PubMed] [Google Scholar]
- 25.Fraser KE, Diao E, Peimer CA, et al. Comparative results of resection of the distal ulna in rheumatoid arthritis and post-traumatic conditions. J Hand Surg Br. 1999;24(6):667-670. [DOI] [PubMed] [Google Scholar]
- 26.Hohenberger GM, Maier MJ, Dolcet C, et al. Sensory nerve supply of the distal radio-ulnar joint with regard to wrist denervation. J Hand Surg Eur Vol. 2017;42(6):586-591. [DOI] [PubMed] [Google Scholar]
- 27.Grechenig S, Lidder S, Dreu M, et al. Wrist denervation of the posterior interosseous nerve through a volar approach: a new technique with anatomical considerations. Surg Radiol Anat. 2017;39(6):593-599. [DOI] [PubMed] [Google Scholar]
- 28.Van den Berge DJ, Kusnezov NA, Rubin S, et al. Outcomes following isolated posterior interosseous nerve neurectomy: a systematic review. Hand (N Y). 2017;12(6):535-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplement_files for Hemiresection Interposition Arthroplasty of the Distal Radioulnar Joint: A Long-term Outcome Study by Femke Nawijn, Svenna H. W. L. Verhiel, Jesse B. Jupiter and Neal C. Chen in HAND