Abstract
Background: Median nerve entrapment in the forearm (MNEF) without motor paralysis is a challenging diagnosis. This retrospective study evaluated the clinical presentation, diagnostic studies, and outcomes following surgical decompression of MNEF. Methods: The study reviewed 147 patient medical charts following MNEF surgical decompression. With exclusion of patients with combined nerve entrapments (radial and ulnar), polyneuropathy, neurotmetic nerve injury, or median nerve motor palsy, the study sample included 27 patients. Data collected include: clinical presentation and pain, strength, provocative testing, functional outcomes, and Disabilities of the Arm, Shoulder and Hand (DASH) scores. Results: The study included 27 patients (mean follow-up = 7 months), and 13 patients had previous carpal tunnel release (CTR). Clinical presentation included pain (n = 27) (forearm, n = 22; median nerve innervated digits, n = 21; and palm, n = 21) and positive clinical tests (forearm scratch collapse test, n = 27; pain with compression over the flexor digitorum superficialis arch/pronator, n = 24; Tinel sign, n = 11). Positive electrodiagnostic studies were found for MNEF (n = 2) and carpal tunnel syndrome (n = 11). Primary CTR was performed in 10 patients and revision CTR in 7 patients. Postoperatively, there were significant (P < .05) improvements in strength, pain, quality of life, and DASH scores. Conclusions: The MNEF without motor paralysis is a clinical diagnosis supported by pain drawings, pain quality, and provocative tests. Patients with persistent forearm pain and median nerve symptoms (especially after CTR) should be evaluated for MNEF. Surgical decompression provides satisfactory outcomes.
Keywords: median nerve compression, pronator syndrome, recurrent carpal tunnel syndrome, nerve compression syndromes, follow-up studies, surgical decompression, electrodiagnostic studies
Introduction
First described in 1951 by Seyffarth,1 median nerve entrapment in the forearm (MNEF), commonly referred to as pronator syndrome, typically presents as aching pain in the forearm and sensory disturbance in the median nerve distribution. Persistent symptoms following a carpal tunnel release (CTR) should prompt evaluation of possible proximal median nerve entrapment. Double crush syndrome is present in about 8.8% of patients with carpal tunnel syndrome (CTS).2 In patients with MNEF, physical findings are subtle, and nerve conduction studies are usually normal.3,4 Ultrasonography has been reported to help identify the median nerve entrapment site by identifying median nerve diameter changes5 or abnormalities of the pronator muscle.3 Because of the lack of objective findings in patients with proximal median nerve entrapment, a detailed history and physical examination are essential to confirm this diagnosis.
The unique anatomy of the median nerve in the upper limb contributes to nerve compression and MNEF. The median nerve leaves the axilla and travels distally in the medial bicipital sulcus of the arm together with the brachial artery. Proximal to the medial epicondyle (approximately 5 cm), the median nerve and brachial artery can be entrapped via the deep layer of the tunnel formed by the supracondylar process and ligament of Struthers.6 The median nerve then passes through the cubital fossa and into the proximal forearm where there are 3 structures that can cause compression: the bicipital aponeurosis or lacertus fibrosus; the superficial pronator teres (PT) muscle and the tendon of the deep head of the PT; and the tendinous leading edge of the flexor digitorum superficialis (FDS). The median nerve then continues distally in the forearm between the flexor digitorum profundus and FDS muscles.7 We believe that MNEF results from dynamic ischemia of the median nerve as the multiple anatomical entrapment points interact with the excursion of the nerve during upper extremity activities. In keeping with dynamic ischemia, we believe that electrodiagnostic (EDX) tests would be normal and that position and provocative tests would be positive. Surgical treatment of MNEF requires complete release of the median nerve at all entrapment locations in the proximal forearm: the lacertus fibrosus (bicipital aponeurosis), the superficial PT muscle and tendon of the deep PT, and FDS arch.8,9 Less commonly encountered entrapment points include the Gantzer muscle and Struthers ligament.6 The purpose of this study was to present our approach for establishing the diagnosis of MNEF, to describe our surgical technique for decompression, and to report postoperative patient outcomes.
Materials and Methods
After institutional review board approval, a retrospective chart review was performed of all patients diagnosed with MNEF and treated surgically between July 2007 and May 2017. The diagnosis of MNEF was based on patient history, pain evaluation questionnaire and drawing, and physical examination, including response to pronator compression/positional test, resisted flexion of the long finger, and resisted forearm pronation-supination. The scratch collapse test (SCT) was performed as previously described.10,11 Patients with vague pain in the forearm without positive provocative signs in the forearm were not diagnosed with MNEF and did not have proximal decompression of the median nerve. Associated CTS was diagnosed based on patient history and physical examination with supportive evidence of nerve conduction abnormalities on EDX studies. All preoperative and follow-up examinations were performed by 1 author (S.E.M.). Medical chart data also included sex, age, duration of symptoms, reported symptoms, physical examination findings, EDX results, and grip and pinch strength. All patients completed the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire (0-100 points)12 and visual analog scale (VAS) for pain and quality of life (QOL) (0-10)13 before surgery and at final follow-up. Surgical decompression was performed in patients with persistent symptoms after nonoperative treatment. Surgical treatment was carried out by 1 surgeon (S.E.M.), and operative findings were recorded.
Surgical Technique
Using standard operative technique, a lazy S incision was made immediately distal to elbow flexion crease. The interval between the flexor carpi radialis and brachioradialis was exposed distally, and the sensory branch of the radial nerve and the radial vessels were identified. The tendon of the superficial head of the PT was identified just lateral to the radial vessels and medial to the radial sensory nerve. Lengthening of the tendon of the PT superficial head was done in a step-cut fashion proximal to the musculotendinous junction (Figure 1). The lacertus fibrosus was released proximally, and then the median nerve was identified medial to the brachial vessels adjacent to the flexor/pronator muscle. The median nerve was followed distally to the deep head of the PT. The muscle of the PT deep head was divided to identity the deep PT tendon which was then resected (Figure 2). The FDS muscle (Figure 3) was then visualized and divided by radially scoring the tendinous leading edge. The median nerve could be visualized through its course in the proximal forearm, and any residual constricting fibrous bands and vessels crossing over the nerve was divided (Figure 2). A common prominent landmark that can be noted as a surrogate for compression is the presence of a tortuous vasa nervorum proximal to the compressive site (Figure 3). After distal decompression, an attempt should be made to palpate a supracondylar process or ligament of Struthers proximally. After adequate decompression, the surgeon should be able to easily run a finger proximally and distally along the median nerve (see Supplemental Video).
Figure 1.

The step-cut lengthening of the superficial head of the pronator teres (dashed line); division of the deep head of the pronator teres and the underlying tendinous portion (arrows); note the flattened appearance of the median nerve (double arrows).
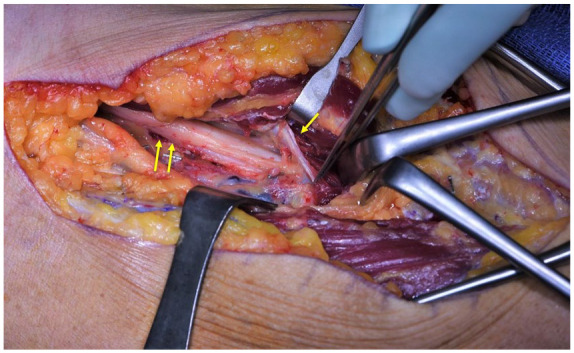
Figure 2.

Note the vascular leash (single arrow) readily seen following the division of the deep head of the pronator teres and the underlying tendinous arch, just proximal to the flexor digitorum superficialis arch (double arrow).
Figure 3.
Following division of the vascular leash, the flexor digitorum superficialis arch (single arrow) is the next to be divided. Note the increased tortuosity of the vasa nervorum proximal to the compressive site (double arrow), with the paucity of vasculature distally.
Statistical Analyses
Summary statistics were tabulated for patient variables (age, sex, hand dominance, symptom duration, body mass index) and surgery variables (simultaneous primary or revision CTR, prior CTR). The main outcomes were VAS pain and QOL, DASH score, and grip and pinch strength. The DASH score was calculated (higher scores indicating higher levels of disability). The preoperative and postoperative scores were compared using paired 2-tailed Student t test. The level of significance was α = .05.
Results
There were 147 patients surgically treated for MNEF during the study period (2007-2017); 120 patients were excluded due to a diagnosis of multiple nerve entrapments (radial or ulnar nerve), anterior interosseous nerve palsy, or traumatic injury involving the upper extremity. The study sample included 27 patients with MNEF (Table 1), and typically, individuals were in the fifth decade of life, overweight, female, and dominant hand affected. Clinical symptoms and signs are presented in Table 2. Only 4 patients (15%) presented with isolated MNEF, and 23 patients (85%) were diagnosed with MNEF and CTS. Thirteen patients (48%) had a history of a previous CTR that failed to improve the primary symptoms. Six of the 13 patients underwent proximal median nerve decompression, and the additional 7 patients underwent revision CTR surgery at the time of their proximal decompression. Ten patients (37%) underwent primary simultaneous CTR.
Table 1.
Patient Demographics.
| Age, y, mean ± SD | 56 ± 3 |
| Gender, No. (%) | Female = 17 (59) |
| Male = 10 (41) | |
| Hand affected, No. (%) | Dominant hand = 19 (70) |
| Nondominant hand = 8 (30) | |
| Symptom duration, mo, mean ± SD | 31 ± 11 |
| Body mass index, kg/m2, mean ± SD | 29 ± 2 |
Table 2.
Presenting Signs and Symptoms.
| Presenting Signs and Symptoms | No. (%) |
|---|---|
| Clinical symptoms | |
| Forearm pain | 22 (81) |
| Median nerve finger involvement | 21 (77) |
| Tingling | 16 (59) |
| Numbness | 19 (70) |
| Pain descriptors | |
| Aching | 20 (74) |
| Throbbing | 13 (48) |
| Shooting | 11 (40) |
| Burning | 9 (33) |
| Cramping | 8 (30) |
| Clinical signs | |
| Index finger static 2PD >6 mm | 8 (30) |
| Thenar atrophy | 5 (18) |
| Forearm: positive Tinel sign | 11 (40) |
| Forearm: provocative testing | 24 (89) |
| Wrist: positive Tinel sign | 13 (48) |
| Wrist: provocative testing | 18 (67) |
| Grip strength, kga | 18.4 ± 2.2 |
| Grip strength ratioa,b | 0.7 ± 0.1 |
| Key pinch, kga | 4.6 ± 0.4 |
| Key pinch ratioa,b | 1.1 ± 0.02 |
Note. 2PD = 2-point discrimination.
Mean ± SD.
Ratio between affected and nonaffected hand.
Forearm pain, median nerve innervated fingers as well as palm (palmar cutaneous distribution) pain, numbness, and tingling were the most common presenting symptoms. Using the pain evaluation questionnaire, pain quality and location were evaluated (Figure 4); aching was the most common descriptor (81%), followed by throbbing (48%), shooting (40%), burning (33%), and cramping (30%). On physical examination, the SCT was positive at the proximal forearm in all patients, forearm pressure/positional provocative tests were positive in 24 patients (89%), and the Tinel sign at the wrist and forearm was positive in less than half of the cases. The EDX studies were positive for MNEF in only 2 patients and for CTS in 10 patients. Preoperative grip and pinch strength were within 74% of the contralateral limb.
Figure 4.
(a) Pre- and (b) postoperative pain diagrams.
Note. Preoperative pain diagram demonstrates pain upon presentation with complaints of median nerve entrapment in the forearm and carpal tunnel syndrome. Following the decompression of the median nerve entrapment in the forearm and carpal tunnel release, pain was reduced significantly.
Following operative release of the median nerve, there were significant improvements (from preoperative to postoperative) in the VAS pain (2.2 ± 0.6 vs 6.0 ± 0.5, P < .001), DASH scores (33 ± 3.6 vs 51 ± 5.8, P = .02), and QOL (31.7 ± 5.7 vs 67.2 ± 5.5, P < .001). Only 2 patients reported no symptom improvement after surgery. Strength significantly increased: grip (47.4 ± 5.2 vs 40.8 ± 4.9, P = .02) and pinch (12.9 ± 1.2 vs 10.1 ± 0.80, P = .006) (Table 3).
Table 3.
Change in Clinical Outcomes.
| Clincal Outcomes | Preoperativea | Postoperativea | P value |
|---|---|---|---|
| Visual analog scale | 6.4 ± 0.6 | 1.7 ± 0.4 | <.001 |
| Quality of life metric | 67.2 ± 5.5 | 31.7 ± 5.7 | <.001 |
| Grip, kg | 18.4 ± 2.2 | 22.8 ± 2.4 | .02 |
| Key pinch, kg | 4.6 ± 0.4 | 5.8 ± 0.5 | .006 |
Mean ± SEM.
Discussion
The MNEF is a diagnosis based on comprehensive clinical examination and not exclusively on EDX studies. A careful history and physical examination are necessary to identify proximal median nerve compression and for selection of nonoperative and operative management. In our study, complete decompression of the median nerve in the proximal forearm resulted in improved symptoms in 93% of patients with significant improvements in the DASH, pain, and QOL scores. In our study sample, approximately half of these patients had a previous CTR that failed to improve their symptoms.
The diagnosis of MNEF is challenging due to the lack of objective findings. Patients with MNEF present with aching pain in the forearm, and numbness and tingling to the median nerve innervated digits, including the distribution of the palmar cutaneous branch of the median nerve.4,8,14 In our study, pain diagrams provided an excellent tool to evaluate patients with MNEF, especially in those who present with concomitant CTS or have persistent symptoms following previous CTR.3,15 As in prior studies, we found that patients with MNEF were older, female, and overweight.16-18 Abnormal EDXs with MNEF have been reported in only 7% to 31% of the surgically treated patients.3,4,19 Similarly, our study had a low prevalence of positive EDX studies for MNEF. Tenderness3 and reproduction of symptoms with forearm supination combined with direct pressure over the PT heads and FDS arch (pronator compression/positional test) were the most common provocative tests.8,20 In our study, the SCT was positive for MNEF in all patients. Previous studies have provided evidence of the usefulness of the SCT for other entrapment neuropathies (CTS and cubital tunnel syndrome) and are helpful in localizing the level of entrapment.10,11 Jiménez and Delgado21 described using the SCT to diagnose MNEF and reported that the test was positive in the affected forearm in all cases.
Various surgical approaches have been described to decompress the median nerve in the proximal forearm, such as oblique,4 transverse,22 and the lazy S-shaped incisions, and also minimally invasive techniques19 and endoscopic release.23 There is no consensus on the optimal surgical technique for the management of MNEF. Seitz et al24 evaluated patients (n = 7) with acute compression of the median nerve in the proximal forearm, and lacertus fibrosus release alone resulted in immediate relief in all patients. Using a minimally invasive approach to release the deep fascia of the superficial PT head, Zancolli et al19 reported 93% of patients had relief of their preoperative pain. Hartz et al treated 32 patients (36 forearms) with release of the lacertus fibrosus and the PT and release of the FDS arch if there was compression by a tight falciform edge. Symptoms were resolved in 8 forearms: reduced (n = 20), persistent (n = 5), and unchanged (n = 3).3 Mujadzic et al25 evaluated 61 patients following release of the lacertus fibrosus, PT, and the FDS arch and reported complete relief in 39 patients. In a previous anatomical study, the FDS arch was found to be tendinous in most cases with direct fibrous attachments to the underlying median nerve and increased compression seen with forearm extension.9 In our surgical cases, the FDS arch was a prominent compressive site, and therefore, decompression of the lacertus fibrosus, step lengthening of the superficial head of the PT tendon, division of the tendon and muscle of the deep head of the PT, and release of the FDS leading edge were always done, in addition to dividing the 2 transverse distal vascular leashes when visualized. This extensive decompression allowed for direct visualization of the median nerve for possible other constricting fibrous bands, Struthers ligament26 and Gantzer muscle,27 as well as the crossing vascular leashes. It is not possible to predict preoperatively which structure or structures are causing compression of the median nerve in the forearm, and it is thus our practice to perform a complete release of all potential entrapment points at the first surgery to maximize potential recovery and minimize the potential need for reoperation.
The limitations of this study include the retrospective study design and the potential for selection bias and small study sample. A retrospective study design is limited by the available data in the medical charts and the criteria used for selection of patients who undergo surgery. The mean follow-up of just 7 months is in keeping with the prompt resolution of symptoms, expected with the satisfactory surgical decompression. The pathophysiology of MNEF is dynamic neural ischemia without demyelination or axonal injury; therefore, the symptom relief is rapid. Our study supports surgical decompression of the MNEF in the appropriately selected patients with improved pain, DASH scores, and QOL.
Median nerve compression in the forearm without motor paralysis is a clinical diagnosis. Pain diagrams and pain quality provide valuable information for the diagnosis of MNEF. The SCT is a useful tool for localizing the nerve entrapment points. The MNEF should be considered in the differential diagnosis of patients with forearm pain and median nerve symptoms, especially in patients with persistent median nerve symptoms after CTR. Surgical decompression addressing the compressive structures provides satisfactory outcomes.
Supplemental Material
Supplemental material, Supplemental_Video for Median Nerve Compression in the Forearm: A Clinical Diagnosis by Madi El-Haj, Wei Ding, Ketan Sharma, Christine Novak, Susan E. Mackinnon and J. Megan M. Patterson in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Madi El-Haj  https://orcid.org/0000-0002-3428-7076
https://orcid.org/0000-0002-3428-7076
J. Megan M. Patterson  https://orcid.org/0000-0001-7748-7759
https://orcid.org/0000-0001-7748-7759
References
- 1.Seyffarth H. Primary myoses in the M. pronator teres as cause of lesion of the N. medianus (the pronator syndrome). Acta Psychiatr Neurol Scand Suppl. 1951;74:251-254. [PubMed] [Google Scholar]
- 2.Asheghan M, Hollisaz MT, Aghdam AS, et al. The prevalence of pronator teres among patients with carpal tunnel syndrome: cross-sectional study. Int J Biomed Sci. 2016;12(3):89-94. [PMC free article] [PubMed] [Google Scholar]
- 3.Hartz CR, Linscheid RL, Gramse RR, et al. The pronator teres syndrome: compressive neuropathy of the median nerve. J Bone Joint Surg Am. 1981;63(6):885-890. [PubMed] [Google Scholar]
- 4.Olehnik WK, Manske PR, Szerzinski J.Median nerve compression in the proximal forearm. J Hand Surg Am. 1994;19(1):121-126. [DOI] [PubMed] [Google Scholar]
- 5.Kodama A, Sunagawa T, Ochi M.Early treatment of anterior interosseous nerve palsy with hourglass-like fascicular constrictions by interfascicular neurolysis due to early diagnosis using ultrasonography: a case report. J Hand Surg Eur Vol. 2015;40(6):642-643. doi: 10.1177/1753193413518692. [DOI] [PubMed] [Google Scholar]
- 6.Shon HC, Park JK, Kim DS, et al. Supracondylar process syndrome: two cases of median nerve neuropathy due to compression by the ligament of Struthers. J Pain Res. 2018;11:803-807. doi: 10.2147/JPR.S160861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wertheimer A, Kiel J.Anatomy, Shoulder and Upper Limb, Forearm Anterior Interosseous Nerve. Treasure Island, FL: StatPearls; 2018. [PubMed] [Google Scholar]
- 8.Rodner CM, Tinsley BA, O’Malley MP.Pronator syndrome and anterior interosseous nerve syndrome. J Am Acad Orthop Surg. 2013;21(5):268-275. [DOI] [PubMed] [Google Scholar]
- 9.Tubbs RS, Marshall T, Loukas M, et al. The sublime bridge: anatomy and implications in median nerve entrapment. J Neurosurg. 2010;113(1):110-112. doi: 10.3171/2009.10.JNS091251. [DOI] [PubMed] [Google Scholar]
- 10.Davidge KM, Gontre G, Tang D, et al. The “hierarchical” Scratch Collapse Test for identifying multilevel ulnar nerve compression. Hand (N Y). 2015;10(3):388-395. doi: 10.1007/s11552-014-9721-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahn LC, Yee A, Mackinnon SE.Important details in performing and interpreting the Scratch Collapse Test. Plast Reconstr Surg. 2018;141(2):399-407. [DOI] [PubMed] [Google Scholar]
- 12.Rosales RS, Delgado EB, Diez de la Lastra-Bosch I.Evaluation of the Spanish version of the DASH and carpal tunnel syndrome health-related quality-of-life instruments: cross-cultural adaptation process and reliability. J Hand Surg Am. 2002;27(2):334-343. [DOI] [PubMed] [Google Scholar]
- 13.Stonner MM, Mackinnon SE, Kaskutas V.Predictors of disability and quality of life with an upper-extremity peripheral nerve disorder. Am J Occup Ther. 2017;71(1):7101190050p1-7101190050p8. doi: 10.5014/ajot.2017.022988. [DOI] [PubMed] [Google Scholar]
- 14.Johnson RK, Spinner M, Shrewsbury MM.Median nerve entrapment syndrome in the proximal forearm. J Hand Surg Am. 1979;4(1):48-51. [DOI] [PubMed] [Google Scholar]
- 15.Hsiao CW, Shih JT, Hung ST.Concurrent carpal tunnel syndrome and pronator syndrome: a retrospective study of 21 cases. Orthop Traumatol Surg Res. 2017;103(1):101-103. doi: 10.1016/j.otsr.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Tetro AM, Pichora DR.High median nerve entrapments. An obscure cause of upper-extremity pain. Hand Clin. 1996;12(4):691-703. [PubMed] [Google Scholar]
- 17.Howard FM.Compression neuropathies in the anterior forearm. Hand Clin. 1986;2(4):737-745. [PubMed] [Google Scholar]
- 18.Lee MJ, LaStayo PC.Pronator syndrome and other nerve compressions that mimic carpal tunnel syndrome. J Orthop Sports Phys Ther. 2004;34(10):601-609. doi: 10.2519/jospt.2004.34.10.601. [DOI] [PubMed] [Google Scholar]
- 19.Zancolli ER, III, Zancolli EP, IV, Perrotto CJ.New mini-invasive decompression for pronator teres syndrome. J Hand Surg Am. 2012;37(8):1706-1710. doi: 10.1016/j.jhsa.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 20.Gainor BJ.The pronator compression test revisited. A forgotten physical sign. Orthop Rev. 1990;19(10):888-892. [PubMed] [Google Scholar]
- 21.Jimenez I, Delgado PJ.The scratch collapse test in the diagnosis of compression of the median nerve in the proximal forearm. J Hand Surg Eur Vol. 2017;42(9):937-940. doi: 10.1177/1753193417726214. [DOI] [PubMed] [Google Scholar]
- 22.Tsai TM, Syed SA.A transverse skin incision approach for decompression of pronator teres syndrome. J Hand Surg Br. 1994;19(1):40-42. [DOI] [PubMed] [Google Scholar]
- 23.Lee AK, Khorsandi M, Nurbhai N, et al. Endoscopically assisted decompression for pronator syndrome. J Hand Surg Am. 2012;37(6):1173-1179. [DOI] [PubMed] [Google Scholar]
- 24.Seitz WH, Jr, Matsuoka H, McAdoo J, et al. Acute compression of the median nerve at the elbow by the lacertus fibrosus. J Shoulder Elbow Surg. 2007;16(1):91-94. doi: 10.1016/j.jse.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 25.Mujadzic M, Papanicolaou G, Young H, et al. Simultaneous surgical release of ipsilateral pronator teres and carpal tunnel syndromes. Plast Reconstr Surg. 2007;119(7):2141-2147. doi: 10.1097/01.prs.0000260703.56453.06. [DOI] [PubMed] [Google Scholar]
- 26.Smith RV, Fisher RG.Struthers ligament: a source of median nerve compression above the elbow. J Neurosurg. 1973;38(6):778-779. doi: 10.3171/jns.1973.38.6.0778. [DOI] [PubMed] [Google Scholar]
- 27.Al-Qattan MM.Gantzer’s muscle. An anatomical study of the accessory head of the flexor pollicis longus muscle. J Hand Surg Br. 1996;21(2):269-270. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_Video for Median Nerve Compression in the Forearm: A Clinical Diagnosis by Madi El-Haj, Wei Ding, Ketan Sharma, Christine Novak, Susan E. Mackinnon and J. Megan M. Patterson in HAND



