Abstract
Background: Indications for replantation following traumatic digit amputations are more liberal in the pediatric population than in adults, but delineation of patient selection within pediatrics and their outcomes have yet to be elucidated. This study uses a national pediatric database to evaluate patient characteristics and injury patterns involved in replantation and their outcomes. Methods: The Healthcare Cost and Utilization Project Kid’s Inpatient Database was queried for traumatic amputations of the thumb and finger from 2000 to 2012. Participants were separated into those who underwent replantation and those who underwent amputation. Patients undergoing replantation were further divided into those requiring revision amputation and/or microvascular revision. Patient age, sex, insurance, digit(s) affected, charges, length of stay, and complications were extracted for each patient. Results: Traumatic digit amputations occurred in 3090 patients, with 1950 (63.1%) undergoing revision amputation and 1140 (36.9%) undergoing replantation. Younger patients, those with thumb injuries, females, and those covered under private insurance were significantly more likely to undergo replantation. Cost, length of stay, and in-hospital complications were significantly greater in replantation patients than in those who had undergone amputation. Following replantation, 237 patients (20.8%) underwent revision amputation and 209 (18.3%) underwent vascular revision, after which 58 required revision amputation. Risk of revision following replantation involved older patients, males, and procedures done recently. Conclusions: Pediatric patients who underwent replantation were significantly younger, female, had thumb injuries, and were covered by private insurance. Our findings demonstrate that in addition to injury factors, demographics play a significant role in the decision for finger replantation and its outcomes.
Keywords: digits, amputation, trauma, diagnosis, replant, epidemiology, research and health outcomes, treatment, microsurgery
Introduction
Traumatic amputation to digits of the hand can result in psychosocial, body image, and functional difficulties that can be magnified in a pediatric population.1-3 Treatment options under such circumstances may involve revision amputation or replantation of the affected digit. The decision to replant a digit is often complex.4 With a lack of medical comorbidities, stable social circumstances, and psychological benefit, replantation has been a more liberal and aggressive treatment option in the pediatric population.5-8 In addition, the healing potential of nerves, skin, and tendons, with enhanced skin elasticity and vascularity in this young age group, decreases pain and stiffness and improves functional outcomes.9
Nonetheless, the frequency of microsurgery and replantation procedures has decreased in the United States over the past 2 decades as a result of multiple factors, including declining reimbursements, availability of microsurgery services, inconsistency of outcomes, and time commitment.10-12 Between 2000 and 2011, the proportion of pediatric patients who underwent replantation has varied between 16% and 40%.4,10 Conversely, revision amputation offers the benefits of a quicker healing course, shortened or lack of hospitalization, decreased need for postoperative therapy, and lower cost.13,14
Despite the abundance of literature demonstrating replantation outcomes in the pediatric population as a whole, few studies have investigated patient and injury characteristics that tend to undergo replantation compared with revision amputation. The purpose of this study was to conduct a retrospective cohort review using a large national pediatric database to identify patient factors associated with undergoing pediatric replantation as opposed to revision amputation. We then sought to compare outcomes between procedures through length of stay, charges, and complications including risk factors for revision procedures following replantation.
Materials and Methods
Data Source
The Healthcare Cost and Utilization Project (HCUP) Kid’s Inpatient Database (KID) was used to examine traumatic digit amputations in the United States from 2000 to 2012. The KID is sponsored by the Agency for Healthcare Research and Quality and is used to track and analyze national trends in pediatric health care. Every 3 years, deidentified data from inpatient discharges are released for patients aged 20 years or younger and include all payers (private, Medicaid, uninsured, and others). Data compiled from 2 to 3 million annual hospital stays are used to generate national estimates of pediatric admissions by using weight-based averages. Data released in 2000, 2003, 2006, 2009, and 2012 were used for this study. Due to the deidentified nature of the data, the study was exempt from institutional review board oversight.
Patient Cohorts
Pediatric patients with traumatic amputation of the thumb or finger were identified using International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes (885.0, 885.1, 886.0, 886.1). International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes were then used to identify the pediatric patients who were treated with either digit revision amputation (84.01, 84.02) or digit replantation (84.21, 84.22). Patients receiving neither revision amputation nor digit replantation were excluded. In addition, patients with more than 1 associated amputation code were excluded, given the inability to determine the procedure each digit underwent.
Patient Variables
For each patient, age, sex, digit involved, insurance, charge, length of stay, complication, and year of procedure were queried. Complications were a composite of diagnoses assessed by ICD-9 codes that include wound dehiscence, infection, hemorrhage, venous thrombosis, and cardiac, respiratory, and urinary complications. Outcomes involving length of stay, in-hospital mortality, total hospital charges, and complications were stratified for comparison between patients treated with digit replantation and revision amputation.
Revision procedures following replantation were assessed using ICD-9-CM procedure codes for revision amputation (84.01, 84.02) and microvascular revision (39.3, 39.4, 39.5) procedures. Patients who underwent microvascular revision and subsequent revision amputation were isolated with combined vascular revision and revision amputation ICD-9-CM codes.
Statistical Methods
χ2 test and univariate logistic regression were used to assess the differences between digit replantation and revision amputation, as well as patient factors associated with each procedure. Multivariate logistic regression determined variables associated with greater length of stay, total hospital charges, in-hospital mortality, complications, and revision procedures. Per protocol, numbers for analysis were based on the national estimates of incidence calculated from discharge-weighting.
Results
Patient Characteristics
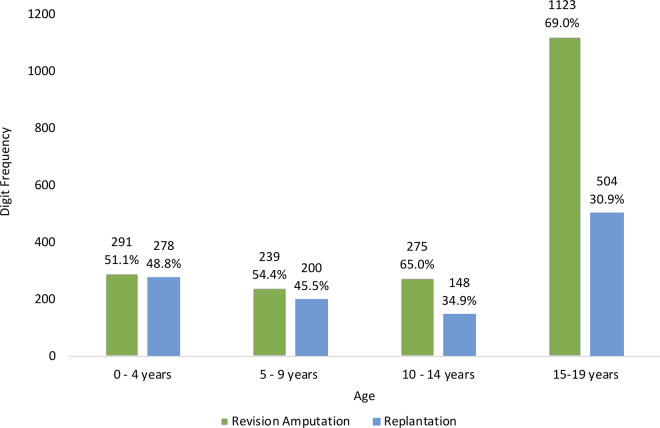
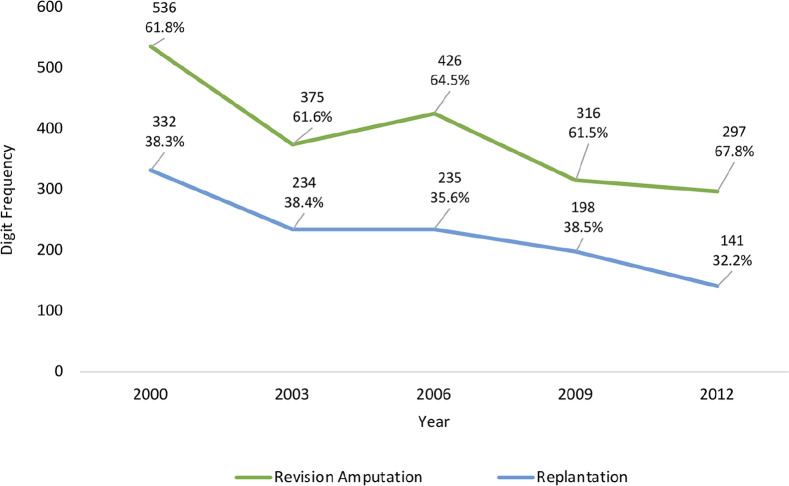
A total of 3090 patients who underwent surgical treatment for traumatic thumb or finger amputation were identified. Of these patients, 1950 were treated with revision amputation (63.1%) and 1140 with digit replantation (36.9%). Significant differences were found in sex, age, digit amputated, and insurance status for patients undergoing replantation versus revision amputation (P < .05) (Table 1). The proportion of patients undergoing replantation by age group was found to decrease with age, with the highest being 0 to 4 years (n = 278, 49.9%) and the lowest being 15 to 19 years (n = 504, 31.0%) (Figure 1). There was no significant difference in the proportion of digit replantations over the years—from 38.3% in 2000 to 32.2% in 2012 (P = .55) (Figure 2).
Table 1.
Demographics and Digits Involved in Digit Replantation and Revision Amputation.
| Demographics | Replantation, No. (%) | Revision amputation, No. (%) | P value |
|---|---|---|---|
| Total Patients | 1140 (36.9) | 1950 (63.1) | |
| Male | 828 (73.9) | 1579 (82.4) | <.001* |
| Mean age, y | 11.6 | 13.6 | <.001* |
| White | 546 (47.9) | 828 (42.5) | .0524 |
| Fingers | 884 (77.5) | 1681 (86.2) | <.001* |
| Thumbs | 281 (24.6) | 342 (17.5) | |
| Private insurance | 577 (50.5) | 816 (41.8) | <.001* |
P < .05 indicates statistical significance.
Figure 1.
Frequency of digit revision amputation and replantation following traumatic digit amputations by age group between 2000 and 2012.
Figure 2.
Trend of digit replantation and revision amputation following traumatic digit amputations between 2000 and 2012.
Patient Factors
The χ2 analyses demonstrated that insurance status, digit amputated, age, and sex were significant factors for patients who underwent replantation (P < .05) (Table 2). Following multivariate regression analyses, those with thumb injuries, females, and patients with private insurance underwent significantly more replantations (P < .05) (Table 3). Patients had a significantly decreased likelihood for replantation with age (odds ratio = 0.955 with each additional year, 95% confidence interval = 0.935-0.975, P < .0001) (Table 3).
Table 2.
The χ2 Analyses of Factors Associated With Pediatric Digit Replantation.
| Digit replantation | P value | ||
|---|---|---|---|
| Factors | No. | % | |
| Insurance type | |||
| Private | 577 | 41.4 | .0004* |
| Other | 563 | 33.2 | |
| Digit | |||
| Finger | 884 | 34.5 | <.0001* |
| Thumb | 281 | 45.2 | |
| Age | |||
| 0-4 | 278 | 48.8 | <.0001* |
| 5-9 | 199 | 45.5 | |
| 10-14 | 148 | 34.9 | |
| 15-19 | 504 | 30.9 | |
| Missing | 11 | ||
| Year | |||
| 2000 | 332 | 38.2 | .5474 |
| 2003 | 234 | 38.4 | |
| 2006 | 235 | 35.5 | |
| 2009 | 198 | 38.6 | |
| 2012 | 141 | 32.2 | |
| Sex | |||
| Male | 828 | 34.4 | <.0001* |
| Female | 293 | 46.5 | |
| Race | |||
| White | 546 | 39.7 | .0524 |
| Nonwhite | 594 | 34.6 | |
P < .05 indicates statistical significance.
Table 3.
Multivariate Logistic Regression of Factors Associated With Pediatric Digit Replantation.
| Factors | OR | 95% CI | P value |
|---|---|---|---|
| Thumb (vs finger) | 1.82 | 1.39-2.38 | <.0001* |
| Female (vs male) | 1.39 | 1.08-1.80 | .010* |
| Private insurance (vs other) | 1.28 | 1.04-1.57 | .019* |
| Age | 0.95 | 0.93-0.97 | <.0001* |
| Year of admission | 0.98 | 0.95-1.01 | .109 |
| White (vs nonwhite) | 1.21 | 0.96-1.52 | .110 |
Note. OR = odds ratio; CI = confidence interval.
P < .05 indicates statistical significance.
Charges, Complications, and Revision Procedures
The mean total hospital charges for replantation were $40 468, compared with $25 185 for amputation (P < .001). The average length of stay was 4.81 days for replantation and 2.76 days for amputation (P < .001). Complication rates were 13.3% following replantation and 3.22% following amputation (P < .001) (Table 4).
Table 4.
Differences in Outcomes Between Revision Amputation and Digit Replantation.
| Outcomes | Revision amputation | 95% CI | Replantation | 95% CI | P value |
|---|---|---|---|---|---|
| Total charges, $ | 25 185.00 | 22 793.64-27 576.36 | 40 468.00 | 36 096.18-44 839.82 | .0001* |
| Length of stay, d | 2.75 | 2.51-3.01 | 4.81 | 4.44-5.18 | .0001* |
| Complication rate, % | 3.22 | 2.04-4.40 | 13.3 | 10.8-15.7 | .0001* |
Note. CI = confidence interval.
P < .05 indicates statistical significance.
Following replantation, 237 patients (20.8%) required revision amputation, and 209 (18.3%) required vascular revision. Of the 209 patients undergoing microvascular revision, 58 patients (27.8%) required revision amputation. Multivariate regression demonstrated that older age, male sex, nonthumb replant, and procedures performed in more recent years were associated with an increased rate of revision procedures following replantation (P < .05) (Table 5). Overall, given the 295 patients captured as requiring an eventual revision amputation from a total of 1140 attempted replantations, the overall success rate of replantation was 74.1% (n = 845).
Table 5.
Factors Associated With Revision Following Digit Replantation.
| Factors | OR | 95% CI | P value |
|---|---|---|---|
| Age | 1.06 | 1.02-1.09 | <.001* |
| Thumb (vs finger) | 0.566 | 0.351-0.912 | .019* |
| Female (vs male) | 0.517 | 0.308-0.868 | .013* |
| Year | 1.06 | 1.01-1.11 | .030* |
| Private (vs other) | 0.821 | 0.530-1.27 | .38 |
| White (vs nonwhite) | 0.929 | 0.614-1.41 | .73 |
Note. OR = odds ratio; CI = confidence interval.
P < .05 indicates statistical significance.
Discussion
Following a national analysis of 3090 pediatric patients with traumatic digit amputations, our study found that 36.9% of them underwent replantation with little change in this proportion over 13 years of analysis. Younger patients, females, thumb injuries, and private insurance were found to have an increased likelihood of replantation. The proportion of patients undergoing replantation was also found to decline with age. In comparison with revision amputation, total charges, length of stay, and complication rates were significantly higher with replantation. Revision replantation or amputation procedures after replantation tended to occur in older, male patients and for replantation performed in more recent years.
Pediatric replantation rates have been demonstrated in other studies at similar rates. Berlin et al10 used the National Inpatient Sample to report a 27% replantation rate. Squitieri et al4 using earlier years of the KID, between 2000 and 2006, found a replantation rate of 40%, which was consistent with our analysis of 36.9%. These findings demonstrate that despite microsurgical advancements over the past decades, the indications for pediatric patients to undergo replantation have remained relatively consistent.
However, despite this consistency, a decreasing trend for replantation over the course of analysis, from 38.2% to 32.2%, was recognized. Adult digit replantation has demonstrated similar decreasing numbers in replantation as well.11,15 Studies have outlined stricter replantation indications, given increased experiences with poor outcome, as well as declining reimbursement rates, disruption of work schedule, and a lack of training as possible causes of decline and increased rates of revision procedures.16-19
In accordance with our findings of replantation occurring in privately insured patients and women, Squitieri et al4 also commented on treatment disparities in sex, race, and insurance status. They found that black, Hispanic, and uninsured patients were significantly less likely to undergo replantation than white and privately insured patients. Using the National Inpatient Sample for adult patients, Cho et al20 found that patients with private insurance were twice more likely to undergo replantation than those with Medicare or Medicaid. These trends have been demonstrated among other conditions as well, with decreased access to appropriate treatment centers and worse trauma outcomes.21-23
Pediatric replantation success rates have been reported to be between 63% and 97%.10,24-26 In comparison, success rates for adult replantation have been reported to be 57% to 90%.27-29 Studies on adult replantation have cited age, patients with more than 3 comorbidities, drug abuse, electrolyte imbalances, and chronic obstructive pulmonary disease as significant risk factors for replantation failure.30-32 Li et al33 found mechanism, platelet count, smoking, amputation preservation, and vein grafting to be risk factors for failure. Berlin et al10 elicited that children have significantly lower procedure-related complications and microvascular revisions compared with adults. This is in accordance with our investigation whereby older patients demonstrated increased risk for revision procedures following replantation, and younger patients were identified to be more likely to undergo replantation. These findings further support that younger patients demonstrate a more robust healing of soft tissues, nerve, and bone following replantation and are associated with fewer complications.34-38 In addition, this demographic of patients is less affected by stiffness, joint contractures, and pain syndromes.36
The finding of the increased cost and length of stay in replantation compared with revision amputation was supported within the adult population. Friedrich et al14 used the State Inpatient Database, part of HCUP, to find that the mean replantation charges were $42 561 compared with the revision amputation charges of $27 541. They noted a mean length of stay of 5.8 days for replantation compared with 3.5 days for amputation. In a retrospective analysis from a single institution in China, the replantation cost of $2977 was significantly greater than the revision amputation cost of $480.23.39 They also noted a significant increase in length of stay of 8.3 days after replantation, compared with 0.21 days for revision amputation. In conjunction, our demonstration of an increase in complications with replantation may also influence the cost and length of stay for such procedures. Overall, these studies and ours demonstrate that replantation carries a higher risk of complication with greater costs and length of stay compared with revision amputations. Despite these potential outcomes, the psychological and functional benefits from successful replantation have shown to hold a significant impact in the pediatric population.2
However, a critical view of our data demonstrating a 74.1% success of replantation may be deemed a less than ideal result given the identified importance of replantation for childhood development and previously published success rates of up to 90%.1,2,24 With the lower rate of pediatric replantation performed across the country as shown within our article and lower reported success of digit replantation in recent years, some researchers have proposed the need for regionalization of replant centers to be staffed by highly competent replantation surgeons to maximize the success of these difficult operations.1,11,12,27 A retrospective study by Brown et al15 using the 2008 and 2012 State Inpatient Databases from the HCUP demonstrated increased odds of success for replantation in hospitals with higher annual replantation volume. Overall, a continued evaluation of maximizing replantation success, especially in the pediatric population, should be addressed whether through increase in resources to training a subset of hand surgeons with strong microvascular skills for replantation and/or forming regionalization centers to specialize in replantation to establish a higher success rate of pediatric digit replantation.
This study benefits from a large sample size over the course of many years, but brings several limitations associated with administrative databases. Coding and billing errors in addition to variation from individual hospitals place data reliability at risk. The clinical depth that cannot be captured in coding data is not able to deliver details such as number of digits amputated, level of amputation, position of digit amputated, or mechanism of injury, all of which play significant roles in decisions for replantation. In addition, with the inability to delineate specific procedures performed for patients with multiple finger amputations, these patients were excluded. Another limitation is that the KID only captures inpatient admissions. As a result, we are unable to review patients discharged from a hospital emergency department following digit amputation, including those who had primary revision amputation. In addition, we are unable to capture patients discharged from the hospital following replantation and admitted for a revision procedure. Furthermore, this database does not capture the whole clinical episode, including the need for rehabilitation, return to school, subsequent outpatient-related procedures, or patient-reported outcomes.
Despite these limitations, we believe our study fittingly uses a national pediatric database to determine patient and injury factors that may influence management of traumatic pediatric digit amputations. By comparing pediatric patients undergoing replantation or revision amputation, our study demonstrates that females, younger age, thumb injury, and private insurance are significant characteristics for undergoing replantation. Conversely, we identified that older age, males, finger injuries, and procedures performed in more recent years had a significantly increased risk of undergoing a revision procedure following replantation. These findings demonstrate that within a pediatric population, patient selection and counseling are paramount to forming agreed-upon outcomes with a firm understanding of the risk of failure or complication from replantation. With the current health care landscape driven by value and patient-reported outcome standards, providing efficient, timely, well-informed, trustworthy, and resourceful care in the face of injury is paramount toward obtaining a successful treatment in a vulnerable population of patients and families.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: As these are publicly available data that have been deidentified, this study is exempt from institutional review board oversight. This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: No consent was obtained for this study as these are publicly available data that have been deidentified.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Neill Y. Li  https://orcid.org/0000-0001-9149-4859
https://orcid.org/0000-0001-9149-4859
References
- 1.Buncke GM, Buntic RF, Romeo O. Pediatric mutilating hand injuries. Hand Clin. 2003;19(1):121-131. doi: 10.1016/S0749-0712(02)00076-8. [DOI] [PubMed] [Google Scholar]
- 2.Meyer TM. Psychological aspects of mutilating hand injuries. Hand Clin. 2003;19(1):41-49. doi: 10.1016/S0749-0712(02)00056-2. [DOI] [PubMed] [Google Scholar]
- 3.Sagiv P, Shabat S, Mann M, et al. Rehabilitation process and functional results of patients with amputated fingers. Plast Reconstr Surg. 2002;110(2):497-503; discussion 504-505. doi: 10.1097/00006534-200208000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Squitieri L, Reichert H, Kim HM, et al. Patterns of surgical care and health disparities of treating pediatric finger amputation injuries in the United States. J Am Coll Surg. 2011;213(4):475-485. doi: 10.1016/j.jamcollsurg.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Abzug JM, Kozin SH. Pediatric replantation. J Hand Surg Am. 2014;39(1):143-145. doi: 10.1016/j.jhsa.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Borne A, Porter A, Recicar J, et al. Pediatric traumatic amputations in the United States. J Pediatr Orthop. 2017;37(2):e104-e107. doi: 10.1097/BPO.0000000000000693. [DOI] [PubMed] [Google Scholar]
- 7.Hostetler SG, Schwartz L, Shields BJ, et al. Characteristics of pediatric traumatic amputations treated in hospital emergency departments: United States, 1990–2002. Pediatrics. 2005;116(5):e667-e674. http://pediatrics.aappublications.org/content/116/5/e667.abstract. Accessed August 19, 2019. [DOI] [PubMed] [Google Scholar]
- 8.Marchessault JA, McKay PL, Hammert WC. Management of upper limb amputations. J Hand Surg Am. 2011;36(10):1718-1726. doi: 10.1016/J.JHSA.2011.07.025. [DOI] [PubMed] [Google Scholar]
- 9.Mohan R, Panthaki Z, Armstrong MB. Replantation in the pediatric hand. J Craniofac Surg. 2009;20(4):996-998. doi: 10.1097/SCS.0b013e3181ae21e5. [DOI] [PubMed] [Google Scholar]
- 10.Berlin NL, Tuggle CT, Thomson JG, et al. Digit replantation in children: a nationwide analysis of outcomes and trends of 455 pediatric patients. Hand (N Y). 2014;9(2):244-252. doi: 10.1007/s11552-014-9628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hustedt JW, Bohl DD, Champagne L. The detrimental effect of decentralization in digital replantation in the United States: 15 years of evidence from the national inpatient sample. J Hand Surg Am. 2016;41(5):593-601. doi: 10.1016/j.jhsa.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Mahmoudi E, Swiatek PR, Chung KC, et al. Racial variation in treatment of traumatic finger/thumb amputation: a national comparative study of replantation and revision amputation. Plast Reconstr Surg. 2016;137(3):576e-585e. doi: 10.1097/01.prs.0000479969.14557.9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conner KA, McKenzie LB, Xiang H, et al. Pediatric traumatic amputations and hospital resource utilization in the United States, 2003. J Trauma. 2010;68(1):131-137. doi: 10.1097/TA.0b013e3181a5f2ec. [DOI] [PubMed] [Google Scholar]
- 14.Friedrich JB, Poppler LH, Mack CD, et al. Epidemiology of upper extremity replantation surgery in the United States. J Hand Surg Am. 2011;36(11):1835-1840. doi: 10.1016/j.jhsa.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Brown M, Lu Y, Chung KC, et al. Annual hospital volume and success of digital replantation. Plast Reconstr Surg. 2017;139(3):672-680. doi: 10.1097/PRS.0000000000003087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen MW, Narayan D. Economics of upper extremity replantation: national and local trends. Plast Reconstr Surg. 2009;124(6):2003-2011. doi: 10.1097/PRS.0b013e3181bf8008. [DOI] [PubMed] [Google Scholar]
- 17.Chung KC, Kowalski CP, Walters MR. Finger replantation in the United States: rates and resource use from the 1996 healthcare cost and utilization project. J Hand Surg Am. 2000;25(6):1038-1042. doi: 10.1053/jhsu.2000.16356. [DOI] [PubMed] [Google Scholar]
- 18.Payatakes AH, Zagoreos NP, Fedorcik GG, et al. Current practice of microsurgery by members of the American society for surgery of the hand. J Hand Surg Am. 2007;32(4):541-547. doi: 10.1016/j.jhsa.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Squitieri L, Steggerda J, Yang LJ, et al. A national study to evaluate trends in the utilization of nerve reconstruction for treatment of neonatal brachial plexus palsy. Plast Reconstr Surg. 2011;127(1):277-283. doi: 10.1097/PRS.0b013e3181f95c1e. [DOI] [PubMed] [Google Scholar]
- 20.Cho HE, Zhong L, Kotsis SV, et al. Finger replantation optimization study (FRONT): update on national trends. J Hand Surg Am. 2018;43(10):903.e1-912.e1. doi: 10.1016/j.jhsa.2018.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flores G. Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4):e979-e1020. doi: 10.1542/peds.2010-0188. [DOI] [PubMed] [Google Scholar]
- 22.Li NY, Bruce WJ, Joyce C, et al. Obesity’s influence on operative management of pediatric supracondylar humerus fractures. J Pediatr Orthop. 2018;38(3):e118-e121. doi: 10.1097/BPO.0000000000001126. [DOI] [PubMed] [Google Scholar]
- 23.Rosen H, Saleh F, Lipsitz SR, et al. Lack of insurance negatively affects trauma mortality in U.S. children. J Pediatr Surg. 2009;44(10):1952-1957. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 24.Cheng GL, Pan DD, Yang ZX, et al. Digital replantation in children. Ann Plast Surg. 1985;15(4):325-331. doi: 10.1097/00000637-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Ikeda K, Yamauchi S, Hashimoto F, et al. Digital replantation in children: a long-term follow-up study. Microsurgery. 1990;11(4):261-264. [DOI] [PubMed] [Google Scholar]
- 26.Michalko KB, Bentz ML. Digital replantation in children. Crit Care Med. 2002;30(suppl 11):S444-S447. doi: 10.1097/00003246-200211001-00009. [DOI] [PubMed] [Google Scholar]
- 27.Fufa D, Calfee R, Wall L, et al. Digit replantation: experience of two U.S. J Bone Joint Surg Am. 2013;95(23):2127-2134. doi: 10.2106/JBJS.L.01219. [DOI] [PubMed] [Google Scholar]
- 28.Waikakul S, Sakkarnkosol S, Vanadurongwan V, et al. Results of 1018 digital replantations in 552 patients. Injury. 2000;31(1):33-40. doi: 10.1016/S0020-1383(99)00196-5. [DOI] [PubMed] [Google Scholar]
- 29.Wang T, Zhao G, Rui YJMJ. An analysis of factors predicting failure after single digit replantation. J Hand Surg Eur Vol. 2019;44:NP2-NP7. [DOI] [PubMed] [Google Scholar]
- 30.Hustedt JW, Chung A, Bohl DD, et al. Evaluating the effect of comorbidities on the success, risk, and cost of digital replantation. J Hand Surg Am. 2016;41(12):1145.e1-1152.e1. doi: 10.1016/j.jhsa.2016.09.013. [DOI] [PubMed] [Google Scholar]
- 31.Kwon GD, Ahn BM, Lee JS, et al. The effect of patient age on the success rate of digital replantation. Plast Reconstr Surg. 2017;139(2):420-426. doi: 10.1097/PRS.0000000000002939. [DOI] [PubMed] [Google Scholar]
- 32.Ma Z, Guo F, Qi J, et al. Effects of non-surgical factors on digital replantation survival rate: a meta-analysis. J Hand Surg Eur Vol. 2016;41(2):157-163. doi: 10.1177/1753193415594572. [DOI] [PubMed] [Google Scholar]
- 33.Li J, Guo Z, Zhu Q, et al. Fingertip replantation: determinants of survival. Plast Reconstr Surg. 2008;122(3):833-839. doi: 10.1097/PRS.0b013e318180ed61. [DOI] [PubMed] [Google Scholar]
- 34.Faivre S, Lim A, Dautel G, et al. Adjacent and spontaneous neurotization after distal digital replantation in children. Plast Reconstr Surg. 2003;111(1):159-165. doi: 10.1097/01.PRS.0000037758.54135.4B. [DOI] [PubMed] [Google Scholar]
- 35.Kim JYS, Brown RJ, Jones NF. Pediatric upper extremity replantation. Clin Plast Surg. 2005;32:1-10. doi: 10.1016/j.cps.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Taghinia AH. Pediatric replantation and revascularization. Hand Clin. 2019;35:155-178. doi: 10.1016/j.hcl.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 37.Wen G, Xu J, Chai YM. Fingertip replantation with palmar venous anastomoses in children. Ann Plast Surg. 2017;78(6):692-696. doi: 10.1097/SAP.0000000000000948. [DOI] [PubMed] [Google Scholar]
- 38.Zhu ZW, Zou XY, Huang YJ, et al. Evaluation of sensory function and recovery after replantation of fingertips at zone I in children. Neural Regen Res. 2017;12(11):1911-1917. doi: 10.4103/1673-5374.219053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu H, Bao B, Zheng X. A comparison of functional outcomes and therapeutic costs: single-digit replantation versus revision amputation. Plast Reconstr Surg. 2017;141:244e-249e. [DOI] [PubMed] [Google Scholar]