Abstract
Study objective
We aimed to evaluate and characterize the scale and relationships of emergency department (ED) visits and excess mortality associated with the early phase of the COVID-19 pandemic in the territory of Hong Kong.
Methods
We conducted a territory-wide, retrospective cohort study to compare ED visits and the related impact of the COVID-19 pandemic on mortality. All ED visits at 18 public acute hospitals in Hong Kong between January 1 and August 31 of 2019 (n=1,426,259) and 2020 (n=1,035,562) were included. The primary outcome was all-cause mortality in the 28 days following an ED visit. The secondary outcomes were weekly number of ED visits and diagnosis-specific mortality.
Results
ED visits decreased by 27.4%, from 1,426,259 in 2019 to 1,035,562 in 2020. Overall period mortality increased from 28,686 (2.0%) in 2019 to 29,737 (2.9%) in 2020. The adjusted odds ratio for 28-day, all-cause mortality in the pandemic period of 2020 relative to 2019 was 1.26 (95% confidence interval 1.24 to 1.28). Both sexes, age more than 45 years, all triage categories, all social classes, all ED visit periods, epilepsy (odds ratio 1.58, 95% confidence interval 1.20 to 2.07), lower respiratory tract infection, and airway disease had higher adjusted ORs for all-cause mortality.
Conclusion
A significant reduction in ED visits in the first 8 months of the COVID-19 pandemic was associated with an increase in deaths certified in the ED. The government must make provisions to encourage patients with alarming symptoms, mental health conditions, and comorbidities to seek timely emergency care, regardless of the pandemic.
Introduction
Background
Coronavirus disease 2019 (COVID-19) represents the third coronavirus-associated epidemic to emerge from a species leap from wild animals to humans.1 , 2 This coronavirus causes a spectrum of presentations, from asymptomatic through mild disease with respiratory symptoms to life-threatening acute respiratory illness.3 , 4 By the end of 2020, worldwide, there were at least 80 million cases with positive Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) serology and more than 1.5 million reported SARS-CoV-2–associated deaths.5
Editor’s Capsule Summary.
What is already known on this topic
Emergency department census dramatically declined during the early waves of the COVID-19 pandemic, potentially signifying that individuals missed necessary medical care.
What question this study addressed
This retrospective observational study assessed the change in ED visit numbers and 28-day all-cause mortality following ED visits before and during the pandemic across all hospitals in Hong Kong.
What this study adds to our knowledge
The COVID-19 pandemic was associated with a decreased number of overall ED visits but an increase in overall 28-day mortality and ED mortality.
How this is relevant to clinical practice
These data suggest that missed ED care due to pandemic-related concerns resulted in increased 28-day mortality. Further work is needed to ensure this phenomenon is not repeated in future pandemics.
Importance
Emergency departments (EDs) are on the front line of the COVID-19 pandemic and need to manage both COVID-19 and the full spectrum of non-COVID cases, such as myocardial infarction, acute-onset leukemia, and trauma and injuries.6, 7, 8 In some jurisdictions, reduced hospital visits helped alleviate the rising pressure on health systems due to the pandemic. For example, there was a reduction in total ED visits in the United States, the United Kingdom, and Spain.8, 9, 10 In the United States, reductions in ED visits ranged from 41.5% in Colorado to 63.5% in New York.11 The factors contributing to these reductions await clarification. However, the early message in the United Kingdom was that the system was under huge pressure and that there was a need to “Protect the National Health Service.”12 It is likely that fear of the virus, concern that hospitals may not be healthy and safe places, and a strong public health message discouraging “unnecessary” ED visits contributed to some of the reductions.
The reduced hospital and ED visits during the pandemic outside Hong Kong included patients with heart attacks (23%), strokes (20%), and hyperglycemic crises (10%).13 Increased non-COVID mortality affected patients with heart disease, Alzheimer disease, and dementia.14 , 15 In general, these reports reflect communities that were directly overwhelmed by COVID-19.15, 16, 17, 18, 19, 20 Hong Kong has experienced 3 small waves of COVID-19, which were well contained by public health measures.21
Goals of This Investigation
We aimed to evaluate and characterize the scale and relationships of ED visits and excess mortality associated with the COVID-19 pandemic in Hong Kong that were not directly caused by SARS-CoV-2. We compared the 2019 and 2020 (January through August) Hong Kong territory-wide ED visits, ED deaths, 28-day mortality rates, demographics, and diagnostic groups in all 18 public EDs. On the basis of previous studies, we hypothesized that the COVID-19 pandemic would be associated with a decrease in ED visits and a higher 28-day non–COVID-19 mortality rate in 2020 compared with 2019.15, 16, 17, 18, 19
Materials and Methods
Study Design and Setting
We performed a territory-wide, retrospective cohort study using data from an electronic administrative health care repository—the Clinical Data Analysis and Reporting System (CDARS), which is managed by the Hospital Authority in Hong Kong.22 The Hospital Authority is the only public body overseeing all public hospitals and clinics in Hong Kong. CDARS retrieves territory-wide data from a centralized medical record system that is generated during the delivery of public health care services. This includes patients’ demographics, ward movements, deaths, diagnoses, procedures, drug prescriptions, dispensing histories, and laboratory results taken from all attendees at public clinics and hospitals in Hong Kong. The data in this system is stored in different data centers in Hong Kong. The diagnostic coding is performed by physicians. The information technology team in each hospital monitors the coding performance of each physician and issues serial reminders for coding each admitted patient if any missing code is found. It includes the inpatient and outpatient data of 80% of the 7.47 million people in Hong Kong, the remainder being in the private system.23 , 24
Full-scale emergency medicine services providing 24-hour emergency physician-led care are only available in the EDs of 18 public hospitals. In 2019, the total number of attendees at these EDs was 2.2 million, equivalent to a total attendance rate of 290 per 1,000 population.25 We followed the Strengthening the Reporting of Observational Studies in Epidemiology statement for reporting observational studies.26 The institutional review board of the University of Hong Kong/Hospital Authority West Cluster (UW 20-112) approved the study and waived participant consent.
Selection of Participants
China announced the outbreak of a novel viral pneumonia on December 31, 2020. The Hong Kong government launched its contingency plan within days after that, although the first confirmed case was not identified until January 23, 2020. All patients attending the EDs of the 18 public hospitals in Hong Kong during the prepandemic period of January 1, 2019 to August 31, 2019 (denoted as “2019”) and during the pandemic period of January 1, 2020 to August 31, 2020 (denoted as “2020”) were included. For year-to-year comparison, ED data recorded on February 29, 2020 was excluded from the analysis. Data extraction was undertaken on October 10, 2020, so all patients were followed up for at least 28 days. We excluded hospital episodes with missing data for triage category and residential district, which represented a limited proportion of ED visits (1.04% in 2019 and 1.17% in 2020). As the epidemic and later pandemic evolved, the implementation of active and enhanced surveillance was escalated. Hong Kong has rigorous testing systems and is likely to have recognized most of the confirmed cases on hospitalization.
Data included sex, age, race, residential districts, arrival time, triage category (1, critical; 2, emergency; 3, urgent; 4, semi-urgent; and 5, nonurgent), institutional residents, ambulance utilization, comprehensive social security assistance recipients, discharge destination (hospital admission, discharge, left without being seen, certified dead in the ED), pandemic attendance period, and the diagnoses.27 The diagnoses included lower respiratory tract infection, airway disease, coronary heart disease, cerebrovascular disease, sepsis, trauma, cancer, diabetes mellitus, chronic kidney diseases, epilepsy, deliberate self-harm, mental disorders, and poisoning. Diagnoses defined by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes recorded in each episode are listed in Table E1 (available at http://www.annemergmed.com). Another set of diagnostic codes that are available in CDARS and used in public hospitals in Hong Kong is the Hospital Authority Master Disease Code Table (HAMDCT). The HAMDCT extends the ICD-9-CM system with additional, locally relevant terms and associated codes. A code number “519.8:8” was added to the HAMDCT, indicating that COVID-19 was present.
The social deprivation index for each residential district was calculated by taking the average of 6 selected variables from the census in 2016 in Hong Kong—namely, unemployment, monthly household income less than US $250, no schooling at all, one-person household, never-married status, and subtenancy. It was developed to measure the social disadvantage of each local urban area in Hong Kong. The area with the highest index values was correlated with high standardized mortality rates and reduced hospital access. The index has been adopted as a measure of the socioeconomic status of patients.28
Outcome Measures
The primary outcome was all-cause mortality in the 28 days following an ED visit. The “28-day mortality” covers all deaths (ie, ED mortality, hospital mortality, and out-of-hospital mortality) up to 28 days. ED mortality was defined as any death certified in the ED (dead before arrival or dead after arrival). Hospital mortality was defined as any death occurring after admission to the hospital ward from the ED up to 28 days. Secondary outcomes were weekly number of ED visits and diagnosis-specific mortality.
Analysis
Descriptive statistics were used to show the number of deaths, the distributions of baseline covariates, and outcomes of ED visits in 2019 and 2020. A complete-case analysis was performed. We adopted the standard population in Hong Kong (as estimated by the Census and Statistics Department) as the denominator in order to determine the 28-day, annualized, age-adjusted estimate of excess mortality rate.29 Age was divided into 5-year age groups from 0 to 85 years old or more.
To minimize potential confounding biases due to discrepancy in baseline covariates of ED visits between years, we applied propensity score covariate adjustment to account for covariate imbalances for ED visits in 2019 and 2020. The propensity scores of all enrolled patients were calculated using multivariable logistic regression, adjusting for baseline variables with open causal pathway to death, including sex, race, age group, residential region, ED arrival time, wave period, ambulance utilization, institutional residents, comprehensive social security assistance recipients, social deprivation index, and triage category. In addition to linear terms of continuous variables, restricted cubic splines on continuous variables were used for propensity score estimation. The estimated propensity score represented the predicted probability of attending EDs before or after pandemic (ED visit in 2019 versus 2020) for each person given their covariates.
We compared study outcomes between the pandemic COVID-19 outbreak period in 2020 and the same prepandemic period in 2019, overall and by covariates, as mentioned above. We calculated the percentage drops in ED visits from 2019 to 2020, overall and by other covariates. Weekly ED visits during the different phases of the pandemic period in 2020 vis-á-vis corresponding period in 2019 were visualized overall and by attendance characteristics and disease subgroups. Natural cubic splines with 95% confidence intervals (CIs) and equally spaced knots were fitted through the weekly ED visits by disease subgroup. We estimated adjusted odds ratios (ORs) of COVID-19 effects in 2020 on 28-day mortality by multivariable logistic regression models adjusted propensity score as covariate. To assess heterogeneity of COVID-19 effects, we conducted repeated analyses considering subgroups based on weeks and different levels of covariates above. All the statistical analyses and figure generations were performed using Stata version 16.0 (StataCorp LLC).
Results
Characteristics of Study Subjects
A total of 1,035,562 ED visits occurred in the pandemic period (January 1 to August 31, 2020), compared with 1,426,259 ED visits during the equivalent prepandemic period in 2019 (a 27.4% reduction) (Table E2, available at http://www.annemergmed.com).
Main Results
Comparison of mortality between 2019 and 2020
Table E3 (available at http://www.annemergmed.com) shows the numbers of deaths of ED attendees during the 2 periods. In 2019, there were 28,686 deaths (3,453 ED certifications; 15,903 hospital certifications; 9,330 out-of-hospital certifications), compared with 29,737 deaths in 2020 (4,508 ED certifications; 15,884 hospital certifications; 9,345 out-of-hospital certifications)—a 3.7% increase in overall mortality and a 30.6% increase in ED mortality. Big differences between 2019 and 2020 occurred in all assessed categories except for the 18-to-less-than-35 year group and several diagnostic categories (trauma, dementia, poisoning, bronchiectasis, and Parkinson disease). The change of mortality per 100,000 population varied in different districts (Figure E1, available at http://www.annemergmed.com).
The estimated total population in Hong Kong at the end of 2019 was 7,520,800; at the end of 2020, it was 7,474,200. The 28-day annualized, age-adjusted all-cause mortality in 2019 (the prepandemic year) was 1,155.448 per 100,000 population, and in 2020 (the pandemic year), it was 1,565.232 per 100,000 population (in Hong Kong). Thus, the overall excess mortality per 100,000 population was 409.784. The 28-day annualized, age-adjusted mortality for respiratory conditions (lower respiratory tract infection, airway disease, bronchiectasis) in 2019 was 314.123 per 100,000 population, compared with 419.747 per 100,000 population in 2020. The excess mortality for respiratory conditions was 105.624. By comparison, the 28-day annualized, age-adjusted mortality for nonrespiratory conditions was 841.325 in 2019 and 1145.485 in 2020, giving an excess mortality of 304.160. Table E3 provides the raw 28-day mortality counts for respiratory conditions in both years.
Comparison of ED visits between 2019 and 2020
The reduction in ED visits (Table E2) occurred in all subgroups, especially for patients aged less than 18 years and patients with airway disease and bronchiectasis. While most marked during the waves of COVID-19 infection, it persisted during the interwave periods (wave, −31.6% versus nonwave, −22.8%). However, associated with this reduction in ED visits was a 30.6% increase in death certifications in the ED.
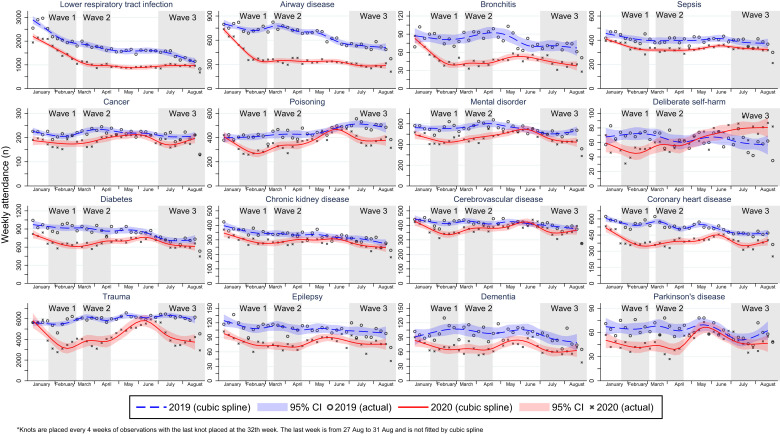
Figure 1 shows the variation in weekly ED visits associated with 16 diagnostic categories. There were significant reductions in ED visits during the first 2 waves across all diagnostic groups. The first interwave period was brief, with no return to 2019 levels. The third wave period saw persistent reductions in ED visits except for cerebrovascular disease, cancer and Parkinson’s diseases that trended to 2019 levels. The major change was in deliberate self-harm, which significantly increased.
Figure 1.
Natural cubic splines with 95% confidence intervals (CIs) and equally spaced knots were fitted through the weekly ED visits by disease subgroup. 2020 (red line) and the same period in 2019 (blue line). Three waves were shown in gray shading.
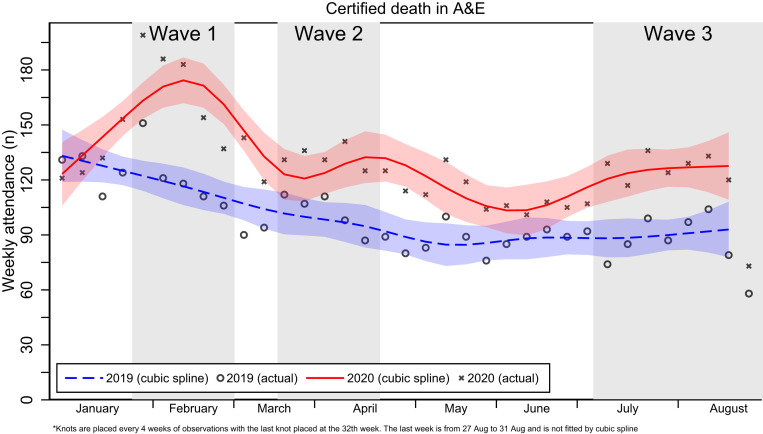
Excess deaths certified in the EDs between 2019 and 2020
Figure 2 shows the dynamic changes in actual weekly count of certified deaths in the EDs. Apart from early January and a short period in late June, there was a significant increase in overall ED death certifications between the cubic spline and weekly counts throughout the period. The dynamic changes, ebbs, and flows in weekly count were similar in both the prepandemic and pandemic periods.
Figure 2.
Natural cubic splines with 95% confidence intervals (CIs) and equally spaced knots were fitted through the weekly count of certified deaths in the EDs (red shading area for 2020 and blue shading area for 2019). Three waves were shown in gray shading.
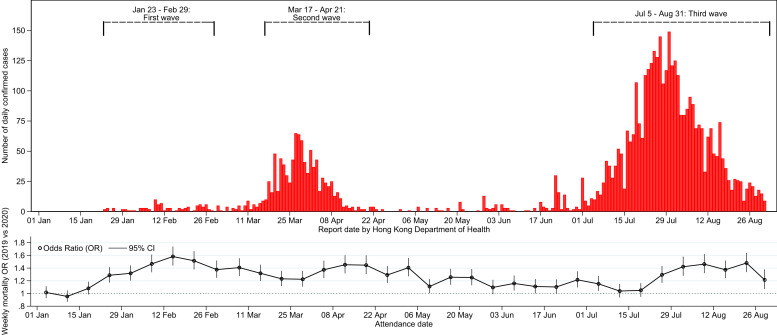
Odds ratios for 28-day (ED and hospital deaths) mortality between 2019 and 2020
Figure 3 shows the dynamic relationships between the number of new COVID-19 cases reported to the Centre for Disease Control in Hong Kong and the adjusted weekly mortality ORs of COVID-19 and non–COVID-19 cases attending EDs. The adjusted OR of 28-day all-cause mortality was highest during the first wave, despite extremely few COVID-19 cases, and reflects a change in the balance of absolute number of deaths (increased) and a reduction in ED visits (decreased) compared with 2019. Apart from a few isolated weeks during the second interwave and early third wave period, the ORs remained significantly elevated throughout the pandemic.
Figure 3.
The first confirmed COVID-19 case in Hong Kong has announced on 23 January 2020: the first wave from 23 January to 29 February; the second wave from 17 March to 21 April; the third wave from 5 July to 31 August 2020. We estimated adjusted odds ratios (ORs) of COVID-19 effects in 2020 on 28-day mortality by multivariable logistic regression models adjusted propensity score as covariate by week.
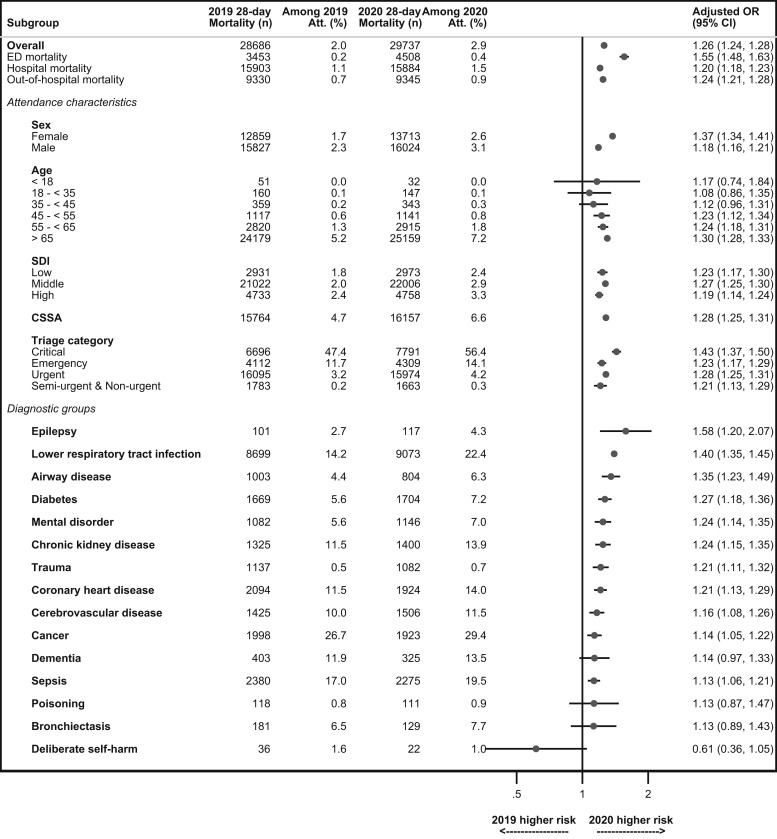
Figure 4 shows the adjusted OR of 28-day, all-cause ED and hospital mortality among patients attending EDs in 2020 compared with 2019. The adjusted OR for 28-day mortality for all parameters was significantly higher in 2020 compared with 2019, except for age 45 years or less, dementia, poisoning, bronchiectasis, Parkinson disease, and deliberate self-harm. For patients admitted to the hospitals, counts and ORs for 28-day mortality were increased for lower respiratory tract infection, followed by diabetes, chronic kidney disease, and cerebrovascular disease. However, among patients who died in the ED, only one third of the deaths were assigned diagnostic codes. Of these, more than 97% were classified as “cardiac arrest,” “instantaneous death,” “unattended death,” or “other unknown and unspecified cause of morbidity and mortality” (Table E4, available at http://www.annemergmed.com), and fewer diagnostic groups were included with wide CIs (Figures E2 and E3, available at http://www.annemergmed.com). Trauma was the only group with an increased count and OR for 28-day mortality in 2020. In Hong Kong, patients who die in the ED are reported to the coroners for investigation, including autopsy, subject to the application of waiver by the relatives. The autopsy reports are not available in the hospital database.
Figure 4.
Subgroups analysis was conducted based on disease groups and different levels of covariates. Multivariable logistic regression models, adjusting propensity score as covariate, were performed to estimate adjusted odds ratios (ORs) of COVID-19 effects in 2020 on 28-day mortality. CSSA, comprehensive social security assistance; SDI, social deprivation index.
Limitations
There are limitations in this study. Firstly, this was a retrospective cohort study and may include inaccurate and incomplete documentation as well as variance in the quality of the information recorded by physicians. However, in this territory-wide study, all patients who registered for ED service in the Hospital Authority were captured; the study findings are highly valid and reliable. Secondly, the findings may not be generalizable beyond Hong Kong. Thirdly, the attendance data in 2019 should be interpreted with caution because of the large-scale social unrest that year. Fourthly, our data set only captured attendance records from the EDs of the 18 public hospitals in Hong Kong. Any information on health care services provided in the private sector is not accessible. However, the private sector focuses on nonemergency care, so the contribution to territory-wide mortality is likely to be low. Finally, it is difficult to objectively determine the degree of certainty of COVID-associated illness. However, during the pandemic, all patients attending EDs who satisfied the clinical and epidemiological criteria for COVID-19, including all deaths, were tested for SARS-CoV-2 by RT-PCR. Further, Hong Kong has robust testing processes that are equal to anywhere in the world. Thus, the degree of certainty is at least equal to any other clinically related COVID-19 publication in the literature.
Discussion
The Fall in ED Visits as a Response in a Public Health Emergency
This study aimed to describe the change in ED visits and associated change of non–COVID-19 mortality during the early phase of the pandemic in Hong Kong. The reduction of ED visits in Hong Kong is compatible with observations in other countries and regions.11 , 30 , 31 However, this is the first report on this phenomenon in a region with low COVID-19 incidence, where traveling within the territory was not restricted. The cumulative number of COVID-19 cases over time for Hong Kong, the United States, the United Kingdom, and New Zealand are compared in Figure E4 (available at http://www.annemergmed.com). Meanwhile, our study confirms the notion that there was hospital avoidance during the pandemic, and it also shows that there was a larger reduction of ED visits among women (−30.1%) compared with that among men (−24.5%) in our setting.32
The greatest degree of reduction was seen among children and adolescents (−60.1%). Otherwise, the reduction across different age groups was similar. We observed that patients with emergencies (critical, emergency, and urgent categories) were less affected (−2.2% to −25.5%) than those categorized as semi-urgent and nonurgent (−29.5%). This suggests that critical and emergency patients in Hong Kong continued to attend EDs in usual numbers during the pandemic. What is not clear is whether there were significant delays in ED visits and whether this was a factor affecting increased mortality rates.
The degree of reduction was not uniform among different clinical conditions or patient groups. The authors analyzed the reduction from 3 different perspectives—namely, respiratory diseases, general emergencies, and long-term medical conditions. ED visits for respiratory problems (namely, lower respiratory tract infection, airway diseases [chronic obstructive pulmonary diseases and asthma], and bronchitis) fell rapidly from the beginning of 2020. The reduction continued throughout the study period and may be explained by the early adoption of precautionary measures in the community.21 , 33
The impact on emergencies was variable. There were small reductions among patients with cerebrovascular disease (stroke) and sepsis but more pronounced changes among patients with coronary heart disease and trauma throughout the study period. The reductions in trauma and poisoning were more significant during the initial 3 months (waves 1 and 2) but returned to prepandemic levels by July 2020, when a local outbreak of COVID-19 started (wave 3). In Hong Kong, the number of patient visits for deliberate self-harm was low, but this rose from July 2020 despite a third wave.
Patients with chronic diseases (cancer, diabetes, chronic kidney diseases, epilepsy, dementia, and Parkinson disease) demonstrated a similar degree of reduction in general. Changes were largest during waves 1 and 2 and then returned toward prepandemic, seasonal-variation levels after wave 2. The differences were less obvious among patients with cancer and chronic renal diseases, whose treatment continued as normal, even though outpatient clinic and community nursing services were suspended during the period.
The Impact of Reduction of ED Visits on Mortality
Early reports suggested that reductions in ED visits might lead to delayed disease presentation and treatment.9 Studies from Hong Kong indicated that during the pandemic, there were delays in presentation for both stroke and coronary heart disease that led to treatment delays and a deterioration in patient outcomes.34 , 35 In the current study, there was a significant increase in ED deaths (classified as out-of-hospital cardiac arrest) during 2020 that was not associated with SARS-CoV-2 infection.
In Hong Kong, emergency medical service professionals are empowered by law to certify the death of a person if certain characteristics are identified, such as decapitation and transection, incineration, rigor mortis, decomposition, and apnea, in conjunction with destruction and/or functional separation from the body of the heart, brain, liver, or lungs. The law and the practice did not change throughout the pandemic.
The 28-day mortality rate was higher in 2020 than in 2019. It mainly affected patients aged 65 years or older, those in critical and emergency categories, and those not living in residential homes for elderly. The increase in out-of-hospital cardiac arrest in 2020 represents an increase in non–COVID-19 disease severity and mortality and may be a result of delays in seeking medical care rather than the effect of fewer acute ED category attendances.
Implications
This study provides an overview on the early impact of COVID-19 on emergency care in Hong Kong. The data suggests increases in mortality in the ED and 28-day mortality among elderly patients and those with chronic medical conditions, possibly due to delayed presentations and hospital avoidance. While it is important to advise patients on social distancing measures, patients should be encouraged to seek medical advice if they have a significant illness. High-quality telephone advisory centers could help to triage patients and advise on the appropriateness of attending an ED while maintaining early social distancing.
In conclusion, our data suggests that the impact of the pandemic in different groups can be highly variable. The reasons underlying variable attitudes to ED visits during a pandemic should be investigated further, using both quantitative and qualitative approaches.
Acknowledgments
The authors wish to dedicate this report to the patients they have described. The authors are also indebted to the many members of the frontline medical and nursing staff, who demonstrated selfless and heroic devotion to duty in the face of this outbreak, both inside and outside hospitals, despite the potential threat to their own lives and those of their families.
Footnotes
Please see page 149 for the Editor’s Capsule Summary of this article.
Supervising editor: Kristin L. Rising, MD, MS. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: AW and CW contributed equally as cofirst authors. AW, JW, OC, and CW reviewed the literature, designed the statistical analysis, conducted analyses, and wrote the manuscript. AW, OC, and CW collected and compiled data. CW, JW, XX, MT, and TR provided critical input to the statistical analyses and design. AW acted as guarantor for the study. All authors contributed to the interpretation of the analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. AW takes responsibility for the paper as a whole.
Authorship: All authors attest to meeting the 4 ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Fundingandsupport: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. The authors report this article did not receive any outside funding or support.
Readers: click on the link to go directly to a survey in which you can provide feedback to Annals on this particular article.
A podcast for this article is available at www.annemergmed.com.
Supplementary Data
References
- 1.Azhar E.I., Hui D.S.C., Memish Z.A., et al. The Middle East respiratory syndrome (MERS) Infect Dis Clin North Am. 2019;33:891–905. doi: 10.1016/j.idc.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui D.S.C., Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am. 2019;33:869–889. doi: 10.1016/j.idc.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peeri N.C., Shrestha N., Rahman M.S., et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49:717–726. doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ritchie H., Beltekian D., Mathieu E., et al. Coronavirus Pandemic (COVID-19). Vol 2020. Our World in Data. https://ourworldindata.org/coronavirus Accessed 1 July, 2021.
- 6.Tam C.F., Cheung K.S., Lam S., et al. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lazzerini M., Barbi E., Apicella A., et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nuñez J.H., Sallent A., Lakhani K., et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51:1414–1418. doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vollmer M.A.C., Radhakrishnan S., Kont M.D., et al. The impact of the COVID-19 pandemic on patterns of attendance at emergency departments in two large London hospitals: an observational study. BMC Health Serv Res. 2021;21:1008. doi: 10.1186/s12913-021-07008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeffery M.M., D’Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prime Minister's Office Prime Minister's statement on coronavirus (COVID-19): 25 March 2020. Vol 2020. https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-25-march-2020 Accessed 1 July, 2021.
- 13.Lange S.J., Ritchey M.D., Goodman A.B., et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu J., Mamas M., Rashid M., et al. Patient response, treatments, and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes. 2021;7:238–246. doi: 10.1093/ehjqcco/qcaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Havenon A., Ney J.P., Callaghan B., et al. Excess neurological death in New York City after the emergence of COVID-19. J Neurol. 2021;268:2026–2028. doi: 10.1007/s00415-020-10084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mannucci E., Nreu B., Monami M. Factors associated with increased all-cause mortality during the COVID-19 pandemic in Italy. Int J Infect Dis. 2020;98:121–124. doi: 10.1016/j.ijid.2020.06.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sjödin H., Johansson A.F., Brännström Å., et al. COVID-19 healthcare demand and mortality in Sweden in response to non-pharmaceutical mitigation and suppression scenarios. Int J Epidemiol. 2020;49:1443–1453. doi: 10.1093/ije/dyaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solano-López J., Zamorano J.L., Pardo Sanz A., et al. Risk factors for in-hospital mortality in patients with acute myocardial infarction during the COVID-19 outbreak. Article in Spanish. Rev Esp Cardiol. 2020;73:985–993. doi: 10.1016/j.rec.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vieira A., Peixoto V.R., Aguiar P., et al. Rapid estimation of excess mortality during the COVID-19 pandemic in Portugal -beyond reported deaths. J Epidemiol Glob Health. 2020;10:209–213. doi: 10.2991/jegh.k.200628.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woolf S.H., Chapman D.A., Sabo R.T., et al. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwok K.O., Li K.K., Chan H.H.H., et al. Community responses during early phase of COVID-19 epidemic, Hong Kong. Emerg Infect Dis. 2020;26:1575–1579. doi: 10.3201/eid2607.200500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng M., Tong Y., Kwok T., et al. Development journey of clinical data analysis and reporting system (CDARS) in hospital authority of Hong Kong. MedInfo. 2010:1468. [Google Scholar]
- 23.Hong Kong Hospital Authority Introduction: Caring for our community's health. Vol 2020. https://www.ha.org.hk/visitor/ha_visitor_index.asp?Parent_ID=10004&Content_ID=10008&Ver=HTML Accessed 1 July, 2021.
- 24.Wong A.Y., Wong I.C., Chui C.S., et al. Association between acute neuropsychiatric events and Helicobacter pylori therapy containing clarithromycin. JAMA Intern Med. 2016;176:828–834. doi: 10.1001/jamainternmed.2016.1586. [DOI] [PubMed] [Google Scholar]
- 25.Controlling Officer . The Government of the Hong Kong Special Administrative Region; 2020. Government Secretariat: Food & Health Bureau Controlling Officer (Health Branch): Controlling Officer’s Report 2019-20.https://www.budget.gov.hk/2019/eng/pdf/head140.pdf Accessed 1 July, 2021. [Google Scholar]
- 26.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 27.Heyworth J. Academic Emergency Medicine; 2011. Emergency medicine-quality indicators: the United Kingdom perspective; pp. 1239–1241. [DOI] [PubMed] [Google Scholar]
- 28.Wong C.M., Ou C.Q., Chan K.P., et al. The effects of air pollution on mortality in socially deprived urban areas in Hong Kong, China. Environ Health Perspect. 2008;116:1189–1194. doi: 10.1289/ehp.10850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kitagawa E.M. Standardized comparisons in population research. Demography. 1964;1:296–315. [Google Scholar]
- 30.Lucero A.D., Lee A., Hyun J., et al. Underutilization of the emergency department during the COVID-19 pandemic. West J Emerg Med. 2020;21:15–23. doi: 10.5811/westjem.2020.8.48632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wongtanasarasin W., Srisawang T., Yothiya W., et al. Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: a hospital-based study. Emerg Med Australas. 2021;33:316–323. doi: 10.1111/1742-6723.13666. [DOI] [PubMed] [Google Scholar]
- 32.Hung KK, Walline JH, Chan EYY, et al. Health service utilization in Hong Kong during the COVID-19 pandemic—a cross-sectional public survey. Int J Health Policy Manag. Published online October 19, 2020. https://doi.org/10.34172/ijhpm.2020.183 [DOI] [PMC free article] [PubMed]
- 33.Lam H.Y., Lam T.S., Wong C.H., et al. The epidemiology of COVID-19 cases and the successful containment strategy in Hong Kong–January to May 2020. Int J Infect Dis. 2020;98:51–58. doi: 10.1016/j.ijid.2020.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teo K.C., Leung W.C.Y., Wong Y.K., et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Jaghbeer M.J., Justo J.A., Owens W., et al. Risk factors for pneumonia due to beta-lactam-susceptible and beta-lactam-resistant Pseudomonas aeruginosa: a case–case–control study. Infection. 2018;46:487–494. doi: 10.1007/s15010-018-1147-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.