Abstract
Sepsis is a dysregulated immune response to infection and potentially leads to life-threatening organ dysfunction, which is often seen in serious Covid-19 patients. Disulfiram (DSF), an old drug that has been used to treat alcohol addiction for decades, has recently been identified as a potent inhibitor of the gasdermin D (GSDMD)-induced pore formation that causes pyroptosis and inflammatory cytokine release. Therefore, DSF represents a promising therapeutic for the treatment of inflammatory disorders. Lactoferrin (LF) is a multifunctional glycoprotein with potent antibacterial and anti-inflammatory activities that acts by neutralizing circulating endotoxins and activating cellular responses. In addition, LF has been well exploited as a drug nanocarrier and targeting ligands. In this study, we developed a DSF-LF nanoparticulate system (DSF-LF NP) for combining the immunosuppressive activities of both DSF and LF. DSF-LF NPs could effectively block pyroptosis and inflammatory cytokine release from macrophages. Treatment with DSF-LF NPs showed remarkable therapeutic effects on lipopolysaccharide (LPS)-induced sepsis. In addition, this therapeutic strategy was also applied to treat ulcerative colitis (UC), and substantial treatment efficacy was achieved in a murine colitis model. The underlying mode of action of these DSF-LF-NPs may contribute to efficiently suppressing macrophage-mediated inflammatory responses and ameliorating the complications caused by sepsis and UC. As macrophage pyroptosis plays a pivotal role in inflammation, this safe and effective biomimetic nanomedicine may offer a versatile therapeutic strategy for treating various inflammatory diseases by repurposing DSF.
Keywords: disulfiram, lactoferrin, macrophage-targeting delivery, sepsis, ulcerative colitis, pyroptosis, inflammation
Introduction
Sepsis, a global public health problem, is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” [1]. The shocking global estimates of 48.9 million incident cases of sepsis and 11 million sepsis-related deaths in 2017 were reported recently [2]. The incidence of sepsis among patients in the intensive care unit (ICU) in mainland China is 20.6%, and the 90-day mortality rate for patients with sepsis is 35.5% [3]. Moreover, coronavirus disease 2019 (COVID-19) can also be described as “viral sepsis” [4, 5], because many patients with COVID-19 meet the diagnostic criteria for sepsis [6, 7]. Fundamentally, sepsis is an inflammatory disease mediated by the activation of the innate immune system due to the inappropriate presence of microorganisms (usually bacteria) and their products [8]. Many microbial factors can activate innate immunity and cause a typical septic inflammatory cascade, including flagellin, peptidoglycans, viral RNAs, and the most widely studied of these, lipopolysaccharide (LPS) [9]. These pathogen-associated molecular patterns (PAMPs) are recognized by the pattern recognition receptors (PRRs) of the innate immune system, thus initiating various pathways such as the TNF-α/NF-κB signaling cascade and the NLRP3 inflammasome, leading to the production of inflammatory cytokines (e.g., IL-1β and IL-18) [10]. Multiple cell-derived mediators, termed damage-associated molecular patterns (DAMPs), may be released after tissue injury, including HMGB1 [11], heat shock proteins, and mitochondrial DNA, thus further amplifying the initial host immune responses [10, 12]. In severe sepsis, these immoderate inflammatory responses can serve as the predominant target of early intervention [8].
During sepsis, recognition of extracellular PAMPs and DAMPs by PRRs mediates the assembly of the canonical NLRP3 inflammasome, subsequently activating the cysteine protease caspase-1, which cleaves pro-IL-1β, pro-IL-18, and gasdermin D (GSDMD) [13, 14], leading to the production of a cytokine storm and pyroptosis [15]. An FDA-approved drug disulfiram (DSF) that has been used to treat alcoholism for over six decades, was reported to inhibit pyroptosis by blocking GSDMD-mediated pore formation [16] and suppress LPS-induced sepsis in mice [17]. DSF was also reported to inhibit NLRP3 inflammasome activation and reduce the levels of reactive oxygen species (ROS) [18].
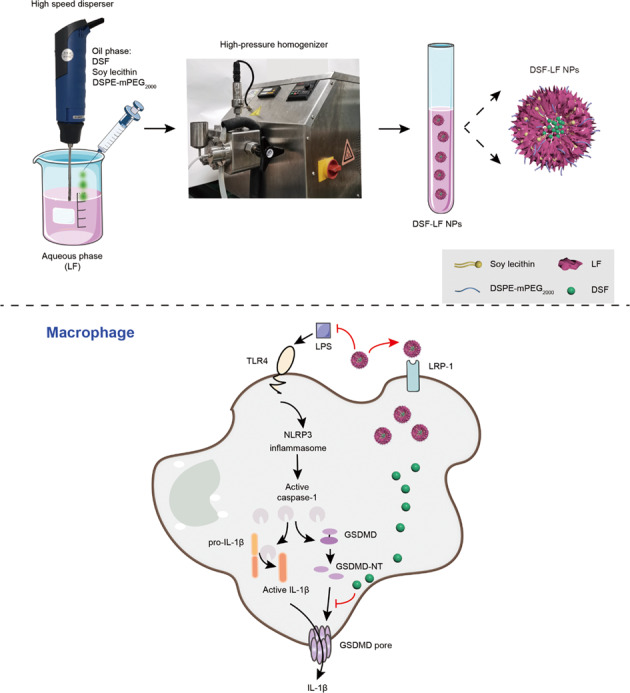
To facilitate the treatment of serious patients or those in a state of septic shock, systemic administration is preferential. However, DSF is water-insoluble and unstable in an acidic gastric environment [19]. After intravenous administration of free DSF, plasma DSF was shown to be eliminated rapidly within 2 h [20]. We therefore developed a lactoferrin (LF)-based nano-biomimetic DSF delivery system (DSF-LF NP) embedded with soy lecithin as a stabilizer and coated with DSPE-mPEG2000 for prolonging systemic circulation of DSF. LF can specifically bind with the low-density lipoprotein receptor-related protein (LRP-1) that is overexpressed in inflammatory macrophages [21]. In addition, LF possesses potent anti-microbial and anti-inflammatory activities [22, 23]. Therefore, LF serves as a nanocarrier, a targeting delivery ligand, and a combinatory agent to DSF.
Ulcerative colitis (UC) is a chronic and incurable inflammatory bowel disease (IBD) that affects millions of people worldwide [24, 25]. Long-standing UC is associated with an increased risk of colorectal cancer [26, 27]. In this study, the application of DSF-LF NPs for UC treatment was also investigated.
Materials and methods
Materials
Disulfiram (DSF) was purchased from Dalian Meilun Biotech Co., Ltd. (Dalian, China). Lactoferrin (LF) was purchased from Nanjing Jingruijiuan Biotechnology Co., Ltd. (Nanjing, China). Soy lecithin and DSPE-mPEG2000 were purchased from AVT (Shanghai) Pharmaceutical Tech Co., Ltd. (Shanghai, China). Dulbecco’s Modified Eagle’s Medium (DMEM) cell culture medium and fetal bovine serum (FBS) were purchased from Gibco (Thermo Fisher Scientific, Waltham, MA, USA). Recombinant murine macrophage colony-stimulating factor (M-CSF) was purchased from PeproTech (Rocky Hill, NJ, USA). Mouse interleukin 1 beta (IL-1β) Elisa Kit was purchased from Shanghai Dakewe Biotech Co., Ltd. (Shanghai, China). Enhanced ATP Assay Kit was purchased from Beyotime Institute of Biotechnology (Haimen, China). Lipopolysaccharide (LPS) was purchased from Sigma-Aldrich (St. Louis, MO, USA). Nigericin sodium salt was purchased from MedChemexpress Co., Ltd. (Shanghai, China). Dextran sulfate sodium salt (DSS) was purchased from Yeasen Biotechnology (Shanghai) Co., Ltd. All other reagents (analytical grade) were obtained from Sinopharm Chemical Reagent Co., Ltd. (Shanghai, China) and were used without further purification.
Animal
C57BL/6 (female, 6–7 weeks) and BALB/c mice (female, 6–7 weeks) were supplied by the Shanghai Laboratory Animal Center (SLAC) Co., Ltd. (Shanghai, China), and housed at the SPF care facility under a 12 h light-dark cycle. Food and water were available ad libitum. The animal experimental procedures were approved by Institutional Animal Care and Use Committee, Shanghai Institute of Materia Medica (SIMM), Chinese Academy of Sciences.
Preparation of blank LF NPs and DSF-LF NPs
DSF-LF NPs were prepared using an emulsion solvent evaporation method. Briefly, 400 mg of LF was dissolved in 16 mL of purified water, and the solution was maintained in an ice-water bath. A mixture of ethanol and chloroform at a volume ratio of 2:1 was used as an organic solvent. The organic solution (4 mL of soy lecithin at 100 mg/mL, DSPE-mPEG2000 at 20 mg/mL, and DSF at 10 mg/mL) was dropwise added to the LF solution under vigorous dispersion. After this addition, the emulsion was further homogenized using a high-pressure homogenizer at 1200 bar and subjected to treatment in a rotary evaporator to remove organic solvents. The thus-formed nanoparticle suspensions were centrifuged at 8000 rpm (Heraeus Multifuge X1R, Thermo Fisher, Osterode am Harz, Germany) for 10 min and filtered with a 0.22 μm membrane filter to remove the unloaded drug. Blank LF NPs were prepared in the same manner without the addition of DSF.
Characterization of blank LF NPs and DSF-LF NPs
The particle size distribution and ζ potential of these nanoparticles were measured using dynamic light scattering (DLS) and electrophoretic light scattering (ELS), respectively (Malvern Nano-ZS90, Malvern, UK). The nanoparticles were also negatively stained with 1% uranyl acetate and examined by transmission electron microscopy (TEM, Talos L120C, Thermo Fisher, Waltham, MA, USA) for morphology. The encapsulation efficiency and drug-loading capacity of DSF-LF NPs were determined using high-performance liquid-phase chromatography (HPLC) (1260 Infinity, Agilent technologies, Santa Clara, CA, USA), and calculated according to the following formula:
Stability of nanoparticles and in vitro drug release
Blank LF NPs and DSF-LF NPs were dispersed in PBS (pH 7.4) containing 10% FBS to evaluate the stability of these nanoparticles. The particle size of these nanoparticles was measured at different preset time points.
The in vitro drug release from the nanoparticles in the release medium (PBS, pH 7.4, containing 0.5% w/v SDS) was studied using dialysis (MWCO 8–14 kDa) in a 37 °C shaker (150 r/min). At the preset time points, 200 μL of the release medium was sampled for measurement, and an equivalent amount of fresh release medium was supplemented. The concentration of DSF in the release medium was determined by HPLC using the condition as follows: Agilent C18 column (250 × 4.6 mm, 5 μm; 1260 Infinity, Agilent Technologies) with a column temperature of 25 °C. Isocratic elution with a mixture of methanol (85%) and ultra-pure water (15%) at a flow rate of 1.0 mL/min and detection wavelength of 216 nm were used.
Preparation and culture of bone marrow-derived macrophages (BMDMs)
The bone marrow cells were collected from the C57BL/6 mice (female, 6–7 weeks) using the standard procedures. Briefly, the bone marrow cells were washed and collected from the femur and tibia of sacrificed mice. The harvested cells were incubated in DMEM, supplemented with 20% FBS, antibiotics (100 μg/mL of streptomycin and 100 U/mL of penicillin), and M-CSF (20 ng/mL), and cultured at 37 °C in a humidified incubator with 5% CO2 for 96 h to induce differentiation.
Cell viability assays
NLRP3 inflammasome activation assay with mouse BMDMs (1 × 104 cells/well) was performed in 24-well plates under serum-free conditions, using DMEM as the cell culture medium. The cells were primed for 4 h with LPS (1 μg/mL) and subsequently incubated with various concentrations of test agents or vehicles for 1 h before the addition of nigericin, an inducer of pyroptosis. These BMDMs were then stimulated with 5 μM nigericin for 2 h for pyroptosis induction.
Cell viability was determined by measuring ATP levels using an enhanced ATP Assay Kit (Beyotime), according to the manufacturer’s instructions. ATP content is an indicator of the physiological state of cells, and thereby ATP levels can be used for measuring the cell viability to evaluate the protective effects of an agent against pyroptosis.
Measurement of cytokines
Concentrations of IL-1β in culture supernatants were measured by ELISA using specific kits (Dakewe) according to the manufacturer’s instructions.
In vivo prevention of sepsis
C57BL/6 mice were randomly allocated to each experimental group. The mice of the DSF group were dosed with DSF (50 mg/kg) by intraperitoneal injection 24 h before and simultaneously with intraperitoneal challenge with LPS (10 mg/kg). The others were intravenously administered PBS, DSF-LF NPs (11 mg/kg of DSF), or LF (with an equivalent mass of LF as in DSF-LF NPs) simultaneously with intraperitoneal challenge with LPS for a survival study (n = 9 for PBS group, n = 10 for the others).
The protective effect of these DSF-LF NPs was further evaluated using a different pretreatment time prior to LPS challenge. The C57BL/6 mice were randomly allocated to each experimental group and were pretreated with PBS, DSF-LF NPs (15 mg/kg), or blank LF NPs (with an equivalent mass of LF as in DSF-LF NPs, Fig. S1) by intravenous injection 24 and 4 h before intraperitoneal challenge with LPS (15 mg/kg) and followed by survival analysis (n = 10 mice per group).
In vivo treatment for colitis
BALB/c mice were randomly allocated to each experimental group and were provided with water or 3% DSS-containing water throughout the entire experiment. The mice were intravenously administered PBS, DSF (15 mg/kg), DSF-LF NPs (15 mg/kg of DSF), or blank LF NPs (with an equivalent mass of LF as in DSF-LF NPs, Fig. S1) at indicated times (n = 8 mice per group). The stock solution of DSF was prepared by dissolving DSF in DMSO, which was then diluted to the desired concentration in PBS (with 5% (w/v) hydroxypropyl-β-cyclodextrin) before use with a final concentration of DMSO not higher than 5% (v/v), a safe dosage suggested by the manufacturer’s instructions.
Statistical analysis
All data were analyzed by GraphPad Prism 6 software. The results were shown as mean ± SD (n ≥ 3). Statistical analysis was performed by Student’s t test or one-way ANOVA. Survival analysis was assessed using the Kaplan–Meier method. Statistical difference was defined as *P < 0.05, **P < 0.01, and ***P < 0.001.
Results
Preparation and characterization of DSF-LF NPs
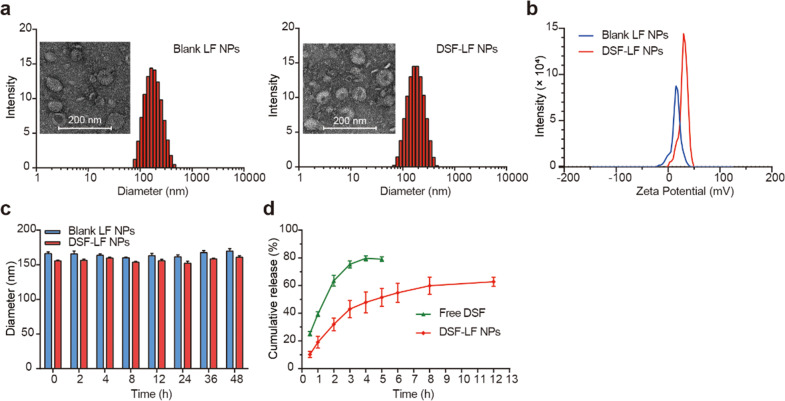
DSF-LF NPs and blank LF NPs were prepared using an emulsion solvent evaporation method. Their particle size was about 160 nm (Fig. 1a), with a narrow particle size distribution (polymer dispersity index around 0.1, Supporting Information Table S1). Transmission electron microscopy (TEM) showed that these nanoparticles were spherical (Fig. 1a). The ζ potential of these DSF-LF NPs was around +10 mV (Fig. 1b). These nanoparticles exhibited good stability and a sustained-release pattern (Fig. 1c, d). The encapsulation efficiency and drug-loading capacity of these DSF-LF NPs are listed in Table S1.
Fig. 1. Characterization of the NPs.
a Size distribution and TEM of the blank LF NPs and DSF-LF NPs. b ζ potential of the blank LF NPs and DSF-LF NPs. c Stability of blank LF NPs and DSF-LF NPs in PBS containing 10% FBS. d In vitro release of DSF from the DSF-LF NPs. Data are presented by mean ± SD (n = 3).
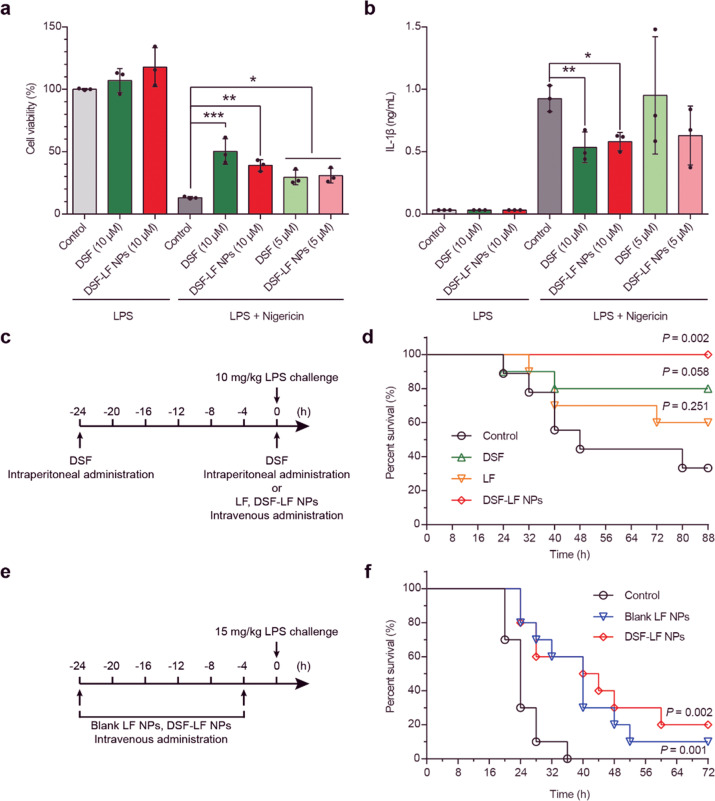
DSF-LF NPs inhibit pyroptosis in BMDMs
Both free DSF and DSF-LF NPs blocked nigericin-induced pyroptosis in LPS-primed BMDMs in a dose-dependent manner (Fig. 2a), and the inhibition efficacy was indicated by cell viability, as assessed by measuring ATP levels. In addition, nigericin-induced IL-1β secretion was also efficiently inhibited (Fig. 2b). Of note, free DSF exhibited a slightly better effect in these cases, and this might have been attributable to the slow release of DSF from the DSF-LF NPs (Fig. 1d).
Fig. 2. DSF-LF NPs inhibit pyroptosis and protect against LPS-induced sepsis.
a Anti-pyroptosis effect of DSF-LF-NPs, reflected by cell viability determined by ATP levels. b Anti-pyroptosis effect of DSF-LF-NPs, reflected by IL-1β secretion. c, e Schematic diagram of sepsis induction and treatment. d Survival curve after a treatment regimen illustrated in (c). f Survival curve after a treatment regimen illustrated in (e). Data (mean ± SD, n = 3) was analyzed using one-way ANOVA (a, b) or log-rank (Mantel–Cox) test (d, f). *P < 0.05, **P < 0.01, ***P < 0.001.
Of note, LF can bind with LRP-1 that is overexpressed in inflammatory macrophages [21]. Therefore, the DSF-LF NPs can preferentially act on the macrophages via LF-mediating binding (Fig. S2).
Efficacy against LPS-induced sepsis in mice
To investigate the in vivo effect of DSF-LF NPs, the C57BL/6 mice were pretreated with DSF, LF, or DSF-LF NPs before challenge with a lethal dose of LPS (Fig. 2c). While six of nine mice died in the PBS control group after 88 h, free DSF and LF provided moderate protection against LPS-induced sepsis, with only two and four out of ten mice killed, respectively (Fig. 2d). Significantly, all of the mice treated with DSF-LF NPs survived (P = 0.002) (Fig. 2d). Interestingly, the blank LF NPs also showed substantial efficacy, while the DSF-LF NPs yielded a higher survival rate (Fig. 2f, Table S3). DSF is a commonly-used drug and easily accessible and available, and its safety has been well documented. Therefore, the prophylactic administration of DSF would be clinically meaningful for lowering the mortality rate caused by sepsis.
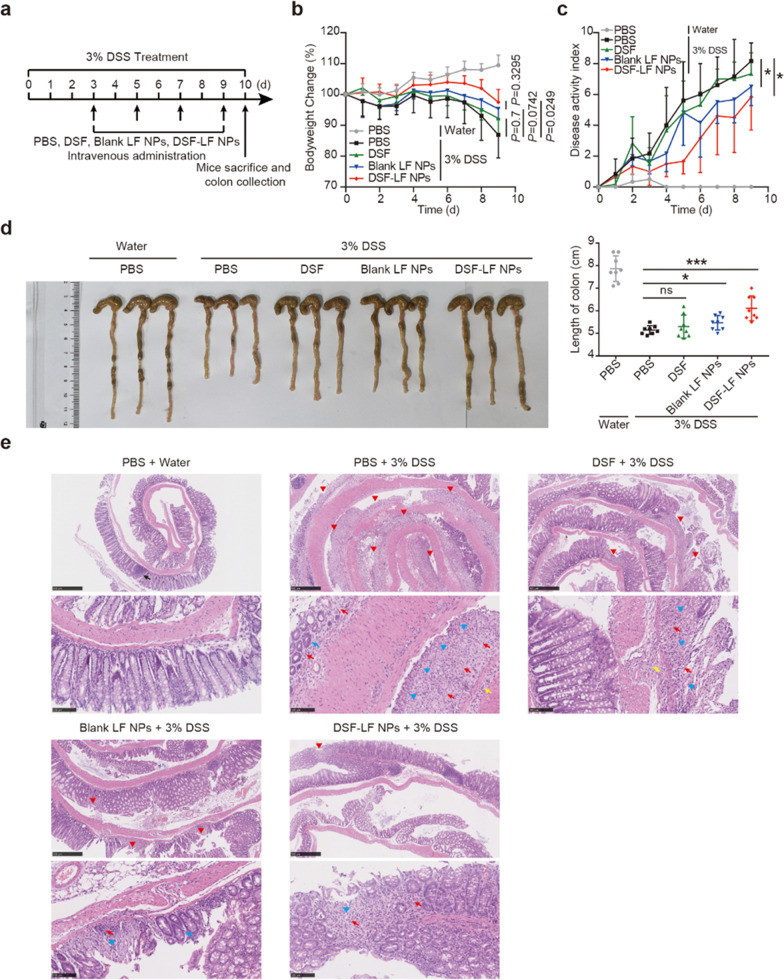
Efficacy against DSS-induced colitis in mice
Next, the therapeutic efficacy of DSF-LF NPs against DSS-induced colitis was investigated. Compared with the PBS control group, treatment with DSF-LF NPs significantly protected the mice against DSS-induced body weight loss and decreased the disease activity index (DAI) (Fig. 3a–c). Shortening of colon length was also restrained by treatment with DSF-LF NPs (Fig. 3d). Blank LF NP treatment also alleviated the symptoms in the DSS-induced colitis mice, as evidenced by the improved DAI and colon length (Fig. 3c, d). Free DSF moderately protected against DSS-induced colitis but without statistical difference compared with the PBS group (Fig. 3b–d). Both DSF-LF NP and blank LF NP treatments also protected the colonic epithelium against pathological damage (Fig. 3e). DSS induced multiple large ulcers (≥10 crypt widths) throughout the intestinal segment, wherein the epithelium of the colonic mucosa was lost, which was coupled with severe goblet cell and crypt loss and enormous inflammatory cell infiltration in the mucosa and submucosa (Fig. 3e). Both DSF-LF NPs and blank LF NPs effectively protected against the epithelial damage and inflammatory cell infiltration associated with DSS-induced colitis, which was manifested as relatively fewer and less severe ulcers (Fig. 3e). However, free DSF only exhibited very limited efficacy, with the compromised integrity of the colonic epithelium (Fig. 3e). The DSF-LF NPs had the best treatment outcomes in this colitis murine model.
Fig. 3. In vivo treatment of DSS-induced colitis.
a Schematic diagram of colitis induction and treatment. b The body weight change in each group during each treatment. c Disease activity index (DAI) record for each group. d The colon length of each group was measured and statistically analyzed. e Histological examination of colons. Scale bar: 500 μm (upper panel), 100 μm (lower panel); red arrowhead: ulceration; blue arrowhead: crypt loss; red arrow: inflammatory cell infiltration of the colonic wall; yellow arrow: inflammatory cell infiltration of the sublayer of the colonic wall; blue arrow: goblet cell loss; black arrow: normal lymphoid tissue. Data were analyzed using two-tailed Student’s t test. Graphs in (b, d) show mean ± SD (n = 8 mice per group). The graph in (c) shows mean ± SD (n = 6 mice per group). *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant.
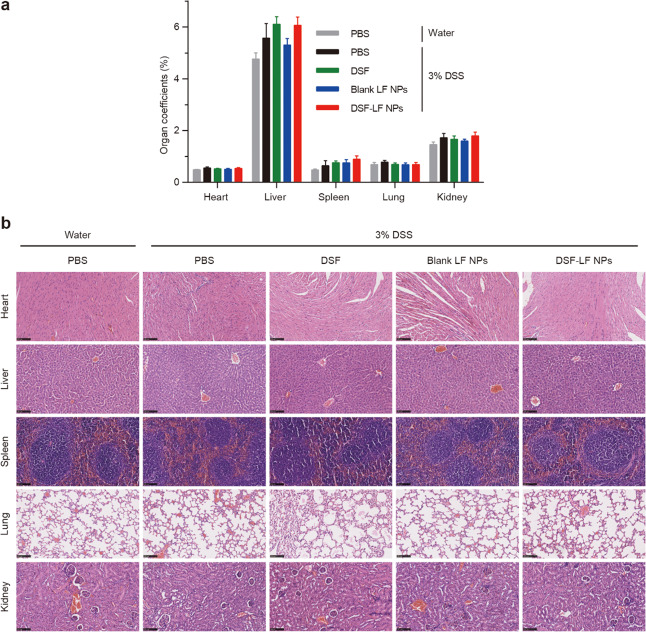
Safety profiles of DSF-LF NPs
The side effects and toxicities of the DSF-LF NPs were preliminarily evaluated using organ coefficient measurements and histopathological examination. No significant difference in the organ coefficients from each group was observed after treatment (Fig. 4a). The histological examination showed no obvious pathological changes in the major organs of each group after treatment (Fig. 4b). This indicated the safety of the proposed biomimetic delivery system and the conducted treatment strategy.
Fig. 4. The preliminary evaluation of biosafety.
a Organ coefficients. b Histological examination of the major organs (scale bar = 100 μm). Data are expressed as mean ± SD (n = 5).
Discussion
Sepsis and septic shock are medical emergencies. Although substantial developments have been made in understanding the pathophysiology of sepsis, there currently are no approved specific anti-septic treatments [28, 29]. To block the activation of the innate immune system can be a part of early treatment for sepsis [30]. However, these inflammatory responses also play a critical role in the host defense against the invading microorganisms [31]. Accordingly, anti-inflammatory therapy is regarded as a double-edged sword that ameliorates the organ failure caused by excessive inflammation, but also potentially compromises a host’s capacity to fight infections [31]. It is thus appealing to develop a multifunctional therapy that is capable of eradicating infection, modulating inflammation, and ameliorating the complications associated with sepsis.
Initially, we attempted to use LF as a drug carrier for targeting the delivery of DSF. However, blank LF NPs also exhibited substantial efficacy in both disease models. In fact, the anti-bacteria and anti-inflammation effects of LF have been previously explored. LF can neutralize LPS and thus inhibit the pro-inflammatory activity of LPS [32]. LF administration reduced TNF-α and IL-6 in serum during LPS-induced sepsis [33] and moderated LPS-induced hypotensive responses and gut injury [34]. LF can protect against oxidative stress-induced cellular damage and attenuate innate immune responsiveness [35]. Therefore, the DSF-LF NPs actually served as a combination therapy.
UC is a chronic relapsing inflammatory colon disease, with characteristic symptoms including bloody diarrhea, abdominal pain, malaise, and weight loss [36, 37]. The pathogenesis of UC might be attributed to genetic susceptibility, impaired intestinal mucosal barrier, dysregulated mucosal immune responses, and environmental factors [24], but it is still far from being completely understood. Current treatments for UC include 5-aminosalicylic acid, corticosteroids, and immunosuppressants [37], but these yield limited efficacy with inadequate response rates [38]. Intestinal macrophages play a key role in establishing and maintaining gut homeostasis [39]. Intestinal macrophages can drive the expansion of regulatory T cells via the production of IL-10 and thus prevent excessive inflammation [40]. Therapeutic targeting of macrophages represents an appealing strategy for potentiating epithelial barrier integrity and restoring intestinal immune homeostasis after inflammation [39]. Our previous work revealed that targeting macrophages to remodel the intestinal immune balance could be a potential therapy for UC [41]. Increasing evidence suggests that activation of the NLRP3 inflammasome and pyroptosis is also involved in the inflammatory process of UC [42, 43]. Studies have shown that therapies inhibiting the activation of the NLRP3 inflammasome and pyroptosis could attenuate inflammation in a DSS-induced colitis model [43, 44]. Of note, there have been no studies on evaluating the therapeutic potential of DSF on UC. The DSF-LF NPs were firstly demonstrated to have potent efficacy in UC treatment.
Conclusions
In summary, we developed a safe, potent, and multifunctional drug delivery system combining the therapeutic effects of both DSF and LF. The DSF-LF NPs could effectively block nigericin-induced pyroptosis and IL-1β release and protected the mice from LPS-induced septic death. Moreover, the DSF-LF NPs also potently protected the mice from DSS-induced colitis by alleviating body weight loss and disease activity, colon length shrinkage, and colonic damage in the mice. Although further studies should be conducted to decipher the detailed mechanisms, this study provides a promising and versatile therapeutic strategy for the treatment of various inflammatory diseases.
Supplementary information
Acknowledgements
We are thankful for the support from National Key Research and Development Program of China (2021YFE0103100, China), NFSC (81925035 and 81521005), and National Special Project for Significant New Drugs Development (2018ZX09711002-010-002), and Shanghai SciTech Innovation Initiative (19431903100, 18430740800) and Shanghai Collaborative Innovation Group of Early Diagnosis and Precise Treatment of Hemangiomas and Vascular Malformations (SSMU-ZDCX20180701) for the support. We thank the Molecular Imaging Center and TEM Facility at SIMM and the National Center for Protein Science Shanghai, CAS, for the technical support at flow cytometry and MALDI-TOF MASS Facility.
Author contributions
ATO: Investigation, Data curation, Formal analysis, Writing original draft. JXZ and YFF: Investigation, Visualization, Methodology. RW and XPT: Investigation, Validation. PFZ, YGZ, MZ: Methodology, Validation. YZH: Formal analysis, Project administration, Supervision, Writing—review & editing.
Competing interests
The authors declare no competing interests.
Supplementary information
The online version contains supplementary material available at 10.1038/s41401-021-00770-w.
References
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315:801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395:200–11. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xie J, Wang H, Kang Y, Zhou L, Liu Z, Qin B, et al. The epidemiology of sepsis in Chinese ICUs: a national cross-sectional survey. Crit Care Med. 2020;48:e209–e18. doi: 10.1097/CCM.0000000000004155. [DOI] [PubMed] [Google Scholar]
- 4.Lin GL, McGinley JP, Drysdale SB, Pollard AJ. Epidemiology and immune pathogenesis of viral sepsis. Front Immunol. 2018;9:2147. doi: 10.3389/fimmu.2018.02147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li H, Liu L, Zhang D, Xu J, Dai H, Tang N, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395:1517–20. doi: 10.1016/S0140-6736(20)30920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ponsford MJ, Gkatzionis A, Walker VM, Grant AJ, Wootton RE, Moore LSP, et al. Cardiometabolic traits, sepsis, and severe COVID-19: a mendelian randomization investigation. Circulation. 2020;142:1791–3. doi: 10.1161/CIRCULATIONAHA.120.050753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Remy KE, Brakenridge SC, Francois B, Daix T, Deutschman CS, Monneret G, et al. Immunotherapies for COVID-19: lessons learned from sepsis. Lancet Respir Med. 2020;8:946–9. doi: 10.1016/S2213-2600(20)30217-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hotchkiss RS, Moldawer LL, Opal SM, Reinhart K, Turnbull IR, Vincent JL. Sepsis and septic shock. Nat Rev Dis Prim. 2016;2:16045. doi: 10.1038/nrdp.2016.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lelubre C, Vincent JL. Mechanisms and treatment of organ failure in sepsis. Nat Rev Nephrol. 2018;14:417–27. doi: 10.1038/s41581-018-0005-7. [DOI] [PubMed] [Google Scholar]
- 10.Ma KC, Schenck EJ, Pabon MA, Choi AMK. The role of danger signals in the pathogenesis and perpetuation of critical illness. Am J Respir Crit Care Med. 2018;197:300–9. doi: 10.1164/rccm.201612-2460PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139–62. doi: 10.1146/annurev-immunol-030409-101323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deutschman CS, Tracey KJ. Sepsis: current dogma and new perspectives. Immunity. 2014;40:463–75. doi: 10.1016/j.immuni.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Sborgi L, Rühl S, Mulvihill E, Pipercevic J, Heilig R, Stahlberg H, et al. GSDMD membrane pore formation constitutes the mechanism of pyroptotic cell death. EMBO J. 2016;35:1766–78. doi: 10.15252/embj.201694696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu X, Zhang Z, Ruan J, Pan Y, Magupalli VG, Wu H, et al. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature. 2016;535:153–8. doi: 10.1038/nature18629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamkanfi M, Dixit VM. Mechanisms and functions of inflammasomes. Cell. 2014;157:1013–22. doi: 10.1016/j.cell.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 16.He WT, Wan H, Hu L, Chen P, Wang X, Huang Z, et al. Gasdermin D is an executor of pyroptosis and required for interleukin-1beta secretion. Cell Res. 2015;25:1285–98. doi: 10.1038/cr.2015.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu JJ, Liu X, Xia S, Zhang Z, Zhang Y, Zhao J, et al. FDA-approved disulfiram inhibits pyroptosis by blocking gasdermin D pore formation. Nat Immunol. 2020;21:736–45. doi: 10.1038/s41590-020-0669-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng W, Yang Z, Yue H, Ou Y, Hu W, Sun P. Disulfiram suppresses NLRP3 inflammasome activation to treat peritoneal and gouty inflammation. Free Radic Biol Med. 2020;152:8–17. doi: 10.1016/j.freeradbiomed.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Johansson B. A review of the pharmacokinetics and pharmacodynamics of disulfiram and its metabolites. Acta Psychiatr Scand Suppl. 1992;86:15–26. doi: 10.1111/j.1600-0447.1992.tb03310.x. [DOI] [PubMed] [Google Scholar]
- 20.Duan X, Xiao J, Yin Q, Zhang Z, Yu H, Mao S, et al. Smart pH-sensitive and temporal-controlled polymeric micelles for effective combination therapy of doxorubicin and disulfiram. ACS Nano. 2013;7:5858–69. doi: 10.1021/nn4010796. [DOI] [PubMed] [Google Scholar]
- 21.Deng N, Li M, Shen D, He Q, Sun W, Liu M, et al. LRP1 receptor-mediated immunosuppression of alpha-MMC on monocytes. Int Immunopharmacol. 2019;70:80–7. doi: 10.1016/j.intimp.2019.01.036. [DOI] [PubMed] [Google Scholar]
- 22.Manzoni P, Dall’Agnola A, Tomé D, Kaufman DA, Tavella E, Pieretto M, et al. Role of lactoferrin in neonates and infants: an update. Am J Perinatol. 2018;35:561–5. doi: 10.1055/s-0038-1639359. [DOI] [PubMed] [Google Scholar]
- 23.Elzoghby AO, Abdelmoneem MA, Hassanin IA, Abd Elwakil MM, Elnaggar MA, Mokhtar S, et al. Lactoferrin, a multi-functional glycoprotein: active therapeutic, drug nanocarrier & targeting ligand. Biomaterials. 2020;263:120355. doi: 10.1016/j.biomaterials.2020.120355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kobayashi T, Siegmund B, Le Berre C, Wei SC, Ferrante M, Shen B, et al. Ulcerative colitis. Nat Rev Dis Prim. 2020;6:74. doi: 10.1038/s41572-020-0205-x. [DOI] [PubMed] [Google Scholar]
- 25.Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769–78. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 26.Olén O, Erichsen R, Sachs MC, Pedersen L, Halfvarson J, Askling J, et al. Colorectal cancer in ulcerative colitis: a Scandinavian population-based cohort study. Lancet. 2020;395:123–31. doi: 10.1016/S0140-6736(19)32545-0. [DOI] [PubMed] [Google Scholar]
- 27.Bopanna S, Ananthakrishnan AN, Kedia S, Yajnik V, Ahuja V. Risk of colorectal cancer in Asian patients with ulcerative colitis: a systematic review and meta-analysis. Lancet. Gastroenterol Hepatol. 2017;2:269–76. doi: 10.1016/S2468-1253(17)30004-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen J, Vincent JL, Adhikari NK, Machado FR, Angus DC, Calandra T, et al. Sepsis: a roadmap for future research. Lancet Infect Dis. 2015;15:581–614. doi: 10.1016/S1473-3099(15)70112-X. [DOI] [PubMed] [Google Scholar]
- 29.Gotts JE, Matthay MA. Sepsis: pathophysiology and clinical management. BMJ. 2016;353:i1585. doi: 10.1136/bmj.i1585. [DOI] [PubMed] [Google Scholar]
- 30.Steinhagen F, Schmidt SV, Schewe JC, Peukert K, Klinman DM, Bode C. Immunotherapy in sepsis - brake or accelerate? Pharmacol Ther. 2020;208:107476. doi: 10.1016/j.pharmthera.2020.107476. [DOI] [PubMed] [Google Scholar]
- 31.Fink MP. Animal models of sepsis and its complications. Kidney Int. 2008;74:991–3. doi: 10.1038/ki.2008.442. [DOI] [PubMed] [Google Scholar]
- 32.Drago-Serrano ME, de la Garza-Amaya M, Luna JS, Campos-Rodriguez R. Lactoferrin-lipopolysaccharide (LPS) binding as key to antibacterial and antiendotoxic effects. Int Immunopharmacol. 2012;12:1–9. doi: 10.1016/j.intimp.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Kruzel ML, Harari Y, Mailman D, Actor JK, Zimecki M. Differential effects of prophylactic, concurrent and therapeutic lactoferrin treatment on LPS-induced inflammatory responses in mice. Clin Exp Immunol. 2002;130:25–31. doi: 10.1046/j.1365-2249.2002.01956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doursout MF, Horton H, Hoang L, Liang Y, Hwang SA, Boyd S, et al. Lactoferrin moderates LPS-induced hypotensive response and gut injury in rats. Int Immunopharmacol. 2013;15:227–31. doi: 10.1016/j.intimp.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Kruzel ML, Zimecki M, Actor JK. Lactoferrin in a context of inflammation-induced pathology. Front Immunol. 2017;8:1438. doi: 10.3389/fimmu.2017.01438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011;365:1713–25. doi: 10.1056/NEJMra1102942. [DOI] [PubMed] [Google Scholar]
- 37.Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389:1756–70. doi: 10.1016/S0140-6736(16)32126-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peyrin-Biroulet L, Lémann M. Review article: remission rates achievable by current therapies for inflammatory bowel disease. Aliment Pharmacol Ther. 2011;33:870–9. doi: 10.1111/j.1365-2036.2011.04599.x. [DOI] [PubMed] [Google Scholar]
- 39.Na YR, Stakenborg M, Seok SH, Matteoli G. Macrophages in intestinal inflammation and resolution: a potential therapeutic target in IBD. Nat Rev Gastroenterol Hepatol. 2019;16:531–43. doi: 10.1038/s41575-019-0172-4. [DOI] [PubMed] [Google Scholar]
- 40.Mowat AM. To respond or not to respond - a personal perspective of intestinal tolerance. Nat Rev Immunol. 2018;18:405–15. doi: 10.1038/s41577-018-0002-x. [DOI] [PubMed] [Google Scholar]
- 41.Zhao Y, Yang Y, Zhang J, Wang R, Cheng B, Kalambhe D, et al. Lactoferrin-mediated macrophage targeting delivery and patchouli alcohol-based therapeutic strategy for inflammatory bowel diseases. Acta Pharm Sin B. 2020;10:1966–76. doi: 10.1016/j.apsb.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davis EM, Zhang D, Glover SC, Stappenbeck TS, Liu JJ. Su1832 – inhibition of intestinal epithelial cell pyroptosis and associated mucosal barrier defects is a potential therapeutic mechanism of action for mesalamine in Ibd. Gastroenterology. 2019;156:S–627. [Google Scholar]
- 43.Ren TH, Lv MM, An XM, Leung WK, Seto WK. Activation of adenosine A3 receptor inhibits inflammatory cytokine production in colonic mucosa of patients with ulcerative colitis by down-regulating the nuclear factor-kappa B signaling. J Dig Dis. 2020;21:38–45. doi: 10.1111/1751-2980.12831. [DOI] [PubMed] [Google Scholar]
- 44.Wu X, Pan S, Luo W, Shen Z, Meng X, Xiao M, et al. Roseburia intestinalis‑derived flagellin ameliorates colitis by targeting miR‑223‑3p‑mediated activation of NLRP3 inflammasome and pyroptosis. Mol Med Rep. 2020;22:2695–704. doi: 10.3892/mmr.2020.11351. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.