Abstract
Objective:
The aim of this study was to evaluate the sensitivity and specificity of electric pulp testing (EPT) using the bridging technique in comparison to a cold test on crowned teeth.
Methods:
Thirty teeth were included in this study. Only one crowned tooth from each subject was included. The adjacent teeth served as controls. The crowned teeth were tested for pulp vitality using a bridging EPT technique and cold test. Vitality was confirmed upon access based on bleeding or lack of bleeding from detected root canal systems. The data was statistically analyzed using the McNamara test (P<0.05).
Results:
The sensitivities of the cold test and bridging EPT were 87% and 66% respectively. Accuracy for cold and bridging EPT were 87% and 67% respectively. The cold test demonstrated a statistically significant higher accuracy and sensitivity than the bridging EPT. However, no significant difference was detected in the specificity between the two tests.
Conclusion:
Both EPT and cold test should be considered as an adjunctive diagnostic tool when determining pulp status in a crowned tooth. Pulp sensitivity tests are essential but the results should be interpreted in combination with other clinical signs/symptoms.
Keywords: Cold test, diagnosis, electric pulp test, sensitivity, specificity
HIGHLIGHTS.
In teeth with full-coverage restorations, the cold test had a statistically higher accuracy and sensitivity than the EPT, but there was no significant difference in the specificity between the two tests.
Ninety-five percent of necrotic teeth had no reaction with cold test and 66.7% of vital teeth had response. Eighty-eight percent of necrotic teeth had no reaction with EPT test and 38.4% of vital teeth had response.
No test should be taken in isolation and pulp test results should be interpreted in combination with other clinical signs and symptoms.
INTRODUCTION
An accurate pulpal diagnosis is an essential part of any endodontic treatment plan. Ideally, pulp tests needs to should be noninvasive, affordable, highly accurate in detecting disease, and clinically easy to perform (1). Mainkar and Kim (2) reported in a recent systematic review with meta-analysis that cold pulp testing has a high diagnostic accuracy. Jesperson et al (3) reported that both cold and EPT were reliable and accurate pulp tests that could be used to evaluate pulpal status. Many studies have evaluated the sensitivity and specificity of both cold and EPT. The sensitivity ranged from 53% to 90% (3-9) and the specificity ranged from 22% to 100% (3, 5-10) and this variation could be a result of the different inclusion criteria and methods that were used in each study. This variation could be a result of the different inclusion criteria and methods that were used in each study.
In teeth with full coverage crowns, Miller et al. (11) evaluated the temperature changes using various cold test methods. They reported that thermal conduction through crowns was similar to noncrowned teeth (11). Furthermore, the method of bridging EPT was introduced test teeth that were heavily restored or had full-coverage restorations (12). Bridging EPT utilizes a toothpaste-coated periodontal probe Qulix CP-15, HuFriedy, Chicago IL which is then placed in contact with tooth structure while the EPT probe simultaneously contacts the instrument.
To date, the accuracy of both tests has not been thoroughly investigated as methods to accurately determine a pulpal diagnosis of crowned teeth. The aim of this study was to evaluate the accuracy, sensitivity and specificity of the bridging EPT in comparison to the cold test on teeth with full coverage restrations indicated for nonsurgical root canal treatment (NS RCT).
MATERIALS AND METHODS
This cross sectional study was approved by the Institutional Review Board (# IRB20172107) and conducted in accordance with acceptable ethical standards. All patients signed a written informed consent form to participate. All patients with teeth with full coverage restorations from 11th December 2018 to 20th March 2019 were screened for possible inclusion in this study. Thirty patients meeting the inclusion criteria were included. The inclusion criteria were patients from 18 to 45 years old who had mature teeth with full coverage restorations, non-traumatized teeth, exposed dentin or enamel between the prosthetic crown and the gingiva, diagnosed by clinical (percussion and palpation) and radiographic evaluations (presence of a apical lesion) and no prior NS RCT. To minimize the confounders, only necrotic and vital teeth were included. Patients with medically compromising conditions (ASA III and above), trauma within the last six months, partially necrotic pulp determined based on direct visualization of blood in the canal, previous endodontic treatment or were excluded. All diagnostic procedure, test and treatment were done by an endodontic resident for standardization.
Included teeth were dried with 4x4 gauze then tested with a cold test using Endo-Ice (Hygenic Endo-Ice, Coltene Whaledent, Cuyahoga Falls, OH) and bridging EPT (Analytic Technology Pulp Tester; Analytic Technology, Redmond, WA). Both techniques were previously described (11, 12). Similar or adjacent teeth with no caries, restorations, or a history of previous injury served as controls for that patient. During the cold test, a medium size #2 cotton pellet was saturated with Endo-Ice (Hygenic Endo-Ice, Coltene Whaledent, Cuyahoga Falls, OH) and then shaken to remove any excess. The saturated cotton pellet was applied in the middle third for all teeth under evaluation starting with the control teeth. Participants were asked to lift their hand up if they felt cold and keep it raised until the sensation abated.
The bridging EPT test was accomplished as previously described by Pantera et al. (12). Toothpaste was used as a conductive medium. The tip of the explorer (17/23 Double End Tufts Stainless Steel, Henry Schein, Melville, NY) was placed on the dentine or enamel between the crown and the gingiva. Then, the EPT probe was touched to the other end of the explorer. Any response before 80 was recorded as positive.
Root canal therapy was initiated only in teeth with at least one negative response from either cold or bridging EPT, and other findings and techniques such as the presence of a sinus tract, periapical radiolucency, percussion, and palpation. Upon accessing the tooth, no bleeding was counted as necrotic and any presence of blood was counted as a vital pulp (8).
Statistical analysis
Sensitivity, specificity and accuracy for both tests were measured. Sensitivity was defined as the ability of the test to detect teeth with necrotic pulps. Specificity was defined as the ability to detect vital pulp, based on accessing the pulp and direct visualization of blood in the canal(s). Accuracy was defined as the proportion of either true positive or true negative, in a population, true necrotic pulps and which contained vital ones (13). The data was statistically analyzed using the McNemar test (P<0.05).
RESULTS
Root canal treatment was performed on 32 patients. Two teeth were excluded due to partially necrotic pulp. Thirty patients were included in this study and distributed as 17 females and 13 males. The majority of included teeth were molars (94%) and other were premolars (6%). The type of restorations were porcelain fused to metal in 80% and zirconia-based crown in 20% of the cases. The sensitivity for the cold test and bridging EPT was 87% and 66% respectively. The specificity was 86% for the cold test and 72% for bridging EPT (Fig. 1). The result was statistically significant (P=0.03). The accuracy for the cold test and bridging EPT was 87% and 67% respectively (Fig. 2). Positive predictive value (PPV) for cold test was 95% and negative predictive value (NPV) was 66.7%. Therefore, 95% of necrotic teeth represent no reaction with cold test and 66.7% of vital teeth had response. PPV and NPV for bridging EPT was 88% and 38.4% respectively (Fig. 3).
Figure 1.
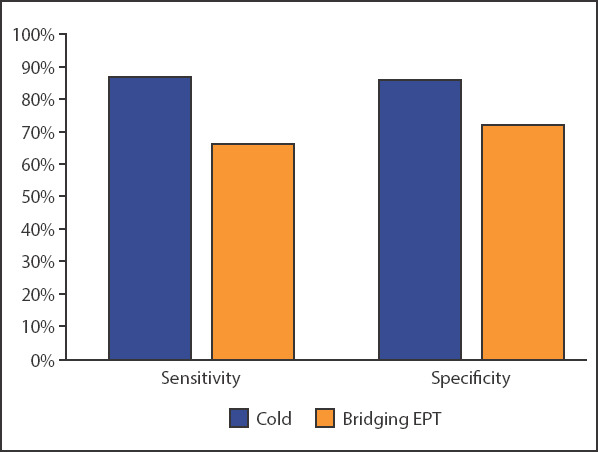
A bar graph showing both sensitivity and specificity for cold and bridging EPT
EPT: Electric pulp testing
Figure 2.
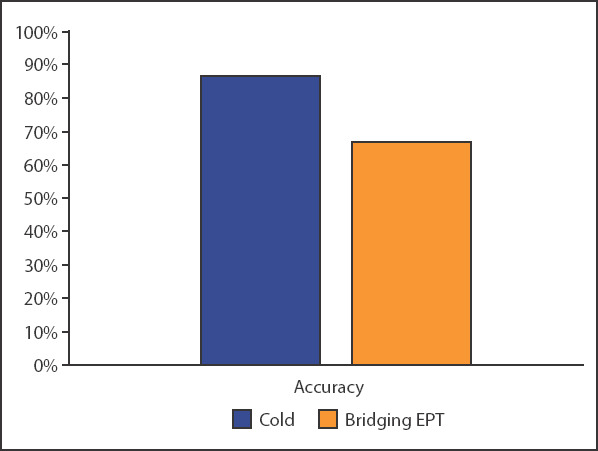
A bar graph showing the accuracy for cold and bridging EPT
EPT: Electric pulp testing
Figure 3.
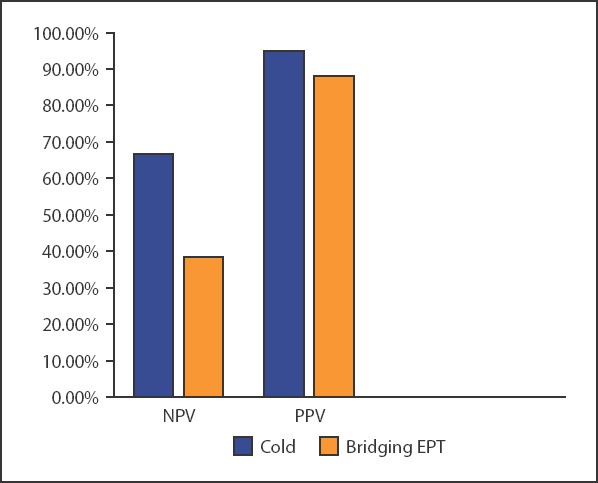
A bar graph showing Positive predictive value (PPV) and negative predictive value (NPV) for cold and bridging EPT
EPT: Electric pulp testing
DISCUSSION
Examining and evaluating teeth with accurate vitality tests is indicated during any endodontic evaluation. In this study the accuracy for the bridging EPT was 67%. Petersson et al. reported the accuracy as high as 81% for EPT (8) whereas other studies have reported 75% (3) and 76% (9) for the accuracy of EPT. The accuracy for the cold test in this investigation was 87%. Other studies have reported 90% (3) and 86% (8). In all these studies, only non-crowned teeth were included. Crown preparation can lead to the production of tertiary dentin as a defense mechanism from the pulp (14). This deposition might decrease the size of the pulp as well as the accuracy of diagnostic testing. Furthermore, drying the tooth before testing with EPT is a major step which is quite difficult to achieve in the cervical area with the presence of a crown. The thickness for the prosthetic material and the type that was used might also interfere with the tests result (11).
False responses, negative or positive, can affect the clinical decision whether to treat or not. An ideal diagnostic test should always give a positive response in the presence of a vital pulp and give a negative response in the presence of a necrotic pulp. In the current investigation, a false positive for the cold test and bridging EPT was seen in eleven teeth with necrotic pulps. The distribution 27% of false positive in this study were related to cold test (necrotic teeth and positive to cold) and 73% by bridging EPT. These results were comparable with another study that found a false negative in necrotic pulps, 30% with the cold test and 70% with EPT (6). In contrast, another study identified false responses in 12% with the cold test and 24% with the EPT (9). Multiple explanations have been proposed for false results (1, 15-18). For instance, since the cold and EPT tests rely on the subjective responses of a patient, an anxious patient might report a false positive response due to their exaggerated expectations. Also, the EPT may conduct the nerves in the periodontium and thus produce a perceived response in teeth with a necrotic pulp.
In this study, the agreement between both cold test and bridging EPT could not provide a more accurate result in comparing with each test separately. For teeth with both vital and non-vital pulps, the cold test was superior than bridging EPT in determining the pulp status. Jespersen et al (3) reported that by combining both cold and EPT tests the agreement was only 67.5%. Another study reported the agreement as low as 29.1% (6). This is in contrast with Weisleder et al (5) who suggested the use of both cold and EPT to provide a more accurate diagnostic result. In some cases, the cold test is not reliable and the EPT should be used in teeth with significant dental pulp calcification (1, 15, 19). Having an EPT as an adjunctive diagnostic tool along with clinician experience will lead to a more accurate diagnosis.
The visual inspection of the pulp tissue, has been considered as a gold standard (8). Although histological status of the dental pulp is the ideal standard for measuring pulp vitality, many studies considered direct inspection as a valid measurement of the pulp status (3, 5-9). Since there is a chance for the tooth to respond to pulp vitality tests in presence of partial necrosis, (20) a tooth was excluded from the study if partial necrosis was noticed in the pulp chamber.
Endo-Ice sprayed onto a medium-size cotton pellet was reported to be the effective method in temperature reduction (11, 21, 22). However, the type of prosthetic crown might interfere in conducting a thermal test. The authors in a previous in-vitro reported that some materials transfer cold rapidly and different than other materials (11). In our study, the majority of included teeth were porcelain fused to metal and another limitation was the number of included patients. Future studies might consider exploring the difference between PFM and other crown restorations in the accuracy of vitality tests.
CONCLUSION
The accuracy for bridging EPT and cold in presence of prosthetic crown was 67% and 87% respectively. Pulp sensitivity tests are essential but the results should be interpreted in combination with other clinical signs/symptoms and no test should be taken in isolation.
Footnotes
Conflict of Interest: The authors deny any conflicts of interest.
Ethics Committee Approval: This study was approved by the Institutional Review Board number: IRB20172107 and date 04/19/2018.
Peer-review: Externally peer-reviewed.
Financial Disclosure: There was no external funding for this study.
Authorship contributions: Concept – W.A., A.A., K.W., A.M.; Design – W.A., A.A., K.W., A.M.; Supervision – W.A., A.A., K.W., A.M.; Funding - None; Materials - None; Data collection &/or processing – W.A., A.A.; Analysis and/or interpretation – W.A., A.A.; Literature search – W.A.; Writing – W.A., A.A.; Critical Review – W.A., A.A., K.W., A.M.
REFERENCES
- 1.Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part I:general information and thermal tests. Int Endod J. 2010;43(9):738–62. doi: 10.1111/j.1365-2591.2010.01754.x. [DOI] [PubMed] [Google Scholar]
- 2.Mainkar A, Kim SG. Diagnostic accuracy of 5 dental pulp tests:A systematic review and meta-analysis. J Endod. 2018;44(5):694–702. doi: 10.1016/j.joen.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Jespersen JJ, Hellstein J, Williamson A, Johnson WT, Qian F. Evaluation of dental pulp sensibility tests in a clinical setting. J Endod. 2014;40(3):351–4. doi: 10.1016/j.joen.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Farid H, Khan FR, Pasha L, Shinwari MS. Are pulp sensibility tests still sensible? J Ayub Med Coll Abbottabad. 2015;27(4):874–7. [PubMed] [Google Scholar]
- 5.Weisleder R, Yamauchi S, Caplan DJ, Trope M, Teixeira FB. The validity of pulp testing:a clinical study. J Am Dent Assoc. 2009;140(8):1013–7. doi: 10.14219/jada.archive.2009.0312. [DOI] [PubMed] [Google Scholar]
- 6.Dastmalchi N, Jafarzadeh H, Moradi S. Comparison of the efficacy of a custom-made pulse oximeter probe with digital electric pulp tester, cold spray, and rubber cup for assessing pulp vitality. J Endod. 2012;38(9):1182–6. doi: 10.1016/j.joen.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 7.Gopikrishna V, Tinagupta K, Kandaswamy D. Evaluation of efficacy of a new custom-made pulse oximeter dental probe in comparison with the electrical and thermal tests for assessing pulp vitality. J Endod. 2007;33(4):411–4. doi: 10.1016/j.joen.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Petersson K, Söderström C, Kiani-Anaraki M, Lévy G. Evaluation of the ability of thermal and electrical tests to register pulp vitality. Endod Dent Traumatol. 1999;15(3):127–31. doi: 10.1111/j.1600-9657.1999.tb00769.x. [DOI] [PubMed] [Google Scholar]
- 9.Villa-Chávez CE, Patiño-Marín N, Loyola-Rodríguez JP, Zavala-Alonso NV, Martínez-Castañón GA, Medina-Solís CE. Predictive values of thermal and electrical dental pulp tests:a clinical study. J Endod. 2013;39(8):965–9. doi: 10.1016/j.joen.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Jafarzadeh H. Laser Doppler flowmetry in endodontics:a review. Int Endod J. 2009;42(6):476–90. doi: 10.1111/j.1365-2591.2009.01548.x. [DOI] [PubMed] [Google Scholar]
- 11.Miller SO, Johnson JD, Allemang JD, Strother JM. Cold testing through full-coverage restorations. J Endod. 2004;30(10):695–700. doi: 10.1097/01.don.0000125880.11248.74. [DOI] [PubMed] [Google Scholar]
- 12.Pantera EA, Jr, Anderson RW, Pantera CT. Use of dental instruments for bridging during electric pulp testing. J Endod. 1992;18(1):37–8. doi: 10.1016/S0099-2399(06)81141-6. [DOI] [PubMed] [Google Scholar]
- 13.Parikh R, Mathai A, Parikh S, Chandra Sekhar G, Thomas R. Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol. 2008;56(1):45–50. doi: 10.4103/0301-4738.37595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levin LG. Pulpal irritants. Endodontic Topics. 2003;5:2–11. [Google Scholar]
- 15.Lin J, Chandler NP. Electric pulp testing:a review. Int Endod J. 2008;41(5):365–74. doi: 10.1111/j.1365-2591.2008.01375.x. [DOI] [PubMed] [Google Scholar]
- 16.Myers JW. Demonstration of a possible source of error with an electric pulp tester. J Endod. 1998;24(3):199–200. doi: 10.1016/S0099-2399(98)80184-2. [DOI] [PubMed] [Google Scholar]
- 17.Cooley RL, Robison SF. Variables associated with electric pulp testing. Oral Surg Oral Med Oral Pathol. 1980;50(1):66–73. doi: 10.1016/0030-4220(80)90334-5. [DOI] [PubMed] [Google Scholar]
- 18.Gopikrishna V, Pradeep G, Venkateshbabu N. Assessment of pulp vitality:a review. Int J Paediatr Dent. 2009 Jan;19(1):3–15. doi: 10.1111/j.1365-263X.2008.00955.x. [DOI] [PubMed] [Google Scholar]
- 19.Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part II:electric pulp tests and test cavities. Int Endod J. 2010;43(11):945–58. doi: 10.1111/j.1365-2591.2010.01760.x. [DOI] [PubMed] [Google Scholar]
- 20.Abd-Elmeguid A, Yu DC. Dental pulp neurophysiology:part 2. Current diagnostic tests to assess pulp vitality. J Can Dent Assoc. 2009;75(2):139–43. [PubMed] [Google Scholar]
- 21.Fuss Z, Trowbridge H, Bender IB, Rickoff B, Sorin S. Assessment of reliability of electrical and thermal pulp testing agents. J Endod. 1986;12(7):301–5. doi: 10.1016/S0099-2399(86)80112-1. [DOI] [PubMed] [Google Scholar]
- 22.Jones DM. Effect of the type carrier used on the results of dichlorodifluoromethane application to teeth. J Endod. 1999;25(10):692–4. doi: 10.1016/S0099-2399(99)80358-6. [DOI] [PubMed] [Google Scholar]


