Abstract
Obstructive sleep apnea has historically been considered a male disease. Although most studies have shown male predominance, obstructive sleep apnea is highly prevalent in women, increasing with age and varying with physiologic status among other factors. Obstructive sleep apnea is associated with significant symptoms and health consequences in women yet remains underdiagnosed in women in part due to differences in presenting symptoms, differences in polysomnographic findings, and/or sociocultural factors. This review will discuss the epidemiology, pathophysiology, clinical presentation, diagnostic findings, and treatment of obstructive sleep apnea, focusing on sex and gender differences.
Keywords: obstructive sleep apnea, gender, sex characteristics, polysomnography, women
Introduction
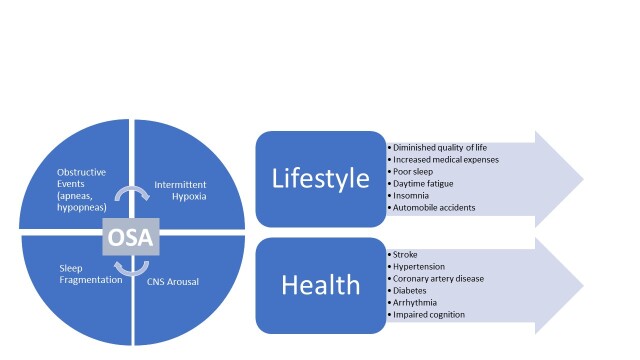
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by intermittent episodes of complete or partial collapse of the upper airway. The diagnosis of OSA is made when at least five obstructive events (apneas or hypopneas) occur per hour of sleep [1]. OSA presents with a variety of signs and symptoms including snoring, excessive daytime sleepiness, headache, and insomnia. Downstream effects of untreated OSA include hypertension, stroke, arrhythmia, automobile accidents, impaired cognition, metabolic syndrome, and diminished quality of life (Figure 1) [2-10]. Untreated OSA is associated with increased medical expenses, primarily due to the cost of associated cardiovascular comorbidities [11,12]. Historically thought of as a “male disease,” women have been underrepresented in clinical trials addressing OSA. While OSA does tend to affect men more than women, its prevalence is high in both sexes and increases with age [13,14]. OSA is generally underdiagnosed, but more so in women than men [15]. Diagnosis of OSA is particularly important in women as several studies have demonstrated that women with OSA experience higher rates of functional impairment at work, disability, adverse cardiovascular events, and sick leave compared to those without OSA [10,16-18]. In this review, we will address the epidemiology, pathophysiology, presentation, diagnosis, and treatment of OSA with an emphasis on sex- and gender-related differences.
Figure 1.
Pathogenesis and Potential Consequences of Obstructive Sleep Apnea. Abbreviations: CNS = central nervous system, OSA = obstructive sleep apnea.
Topics
Epidemiology
The prevalence of OSA is high despite under-diagnosis of the disorder [19-21], particularly in women [22]. Prevalence varies widely among studies in part related to the criteria used to define respiratory disturbances, the diagnostic test employed, and the population studied. Additionally, the majority of large epidemiological trials are biased toward men, making conclusions challenging to generalize. A review of the literature from 2003-2013 found that overall, 22% of men and 17% of women had OSA [13], likely an underestimate. The Wisconsin Sleep Cohort Study, which mostly consisted of non-Hispanic whites, found that 34% of men and 17% of women between the ages of 30 and 70 had OSA present on polysomnography [23]. When the subset of older men and women ages 50 to 70 were studied, the prevalence increased to 43% and 28%, respectively [23]. Another population-based study, which focused on African American adults, found that nearly 54% had at least mild OSA; the prevalence of OSA in men was 12% higher than in women [24].
At all ages, OSA is more common in men than women, but the prevalence increases throughout life in both sexes [14]. Franklin and colleagues sought to determine the prevalence of OSA in women in the general population and found that up to 50% of women between the ages of 20 and 70 had OSA [25]. Presence of OSA did not correlate with reported sleepiness. The difference in prevalence between men and women narrows in older individuals (> age 50) due to the increased prevalence of OSA in women after menopause [26].
Pathogenesis
Pathophysiology: OSA is characterized by intermittent episodes of upper airway collapse during sleep, which correlate with absent or diminished airflow during respiratory effort. These apneas or hypopneas lead to a cycle of abnormal physiology that includes intermittent hypoxia, sympathetic activation, hemodynamic disturbance, and sleep architecture disruption [27,28]. The patency of the upper airway in humans is largely maintained by muscle activation and surrounding soft tissue structures [29]. Pharyngeal patency is promoted by activation of the pharyngeal dilator muscles and increases in lung volume. The genioglossus muscle contracts with each inspiration to prevent collapse of the posterior aspect of the tongue while the levator and tensor palatine muscles elevate the soft palate and the geniohyoid and stylopharyngeus muscles oppose medial collapse of the lateral pharyngeal walls [30]. Collapse can occur with inspiration (negative pressure) and extrinsic compression (positive pressure). Thus, a predisposition to OSA hinges on perturbations in this fine balance.
Many individuals with OSA have functionally narrow upper airways due to obesity and/or structural abnormalities of the face and jaw, such as retrognathia or micrognathia [31,32]. Endoscopy studies performed in patients with and without OSA demonstrated smaller pharyngeal airways and increased collapsibility in those with OSA [33]. Another study found that, compared to women, men had longer upper airways, which were associated with increased collapsibility [34]. Of note, this finding is not present until after puberty, suggesting an effect of sex hormones. Additionally, it has been shown that aging is associated with increasing pharyngeal airway collapsibility during sleep, independent of body mass index and sex, which supports the finding that OSA prevalence increases with age [35].
The Role of Hormones: Estrogen, progesterone, and androgens play a role in the regulation of breathing [36]. Progesterone increases ventilatory responsiveness to hypoxia and hypercapnia [37]. In fact, high levels of progesterone in pregnancy are responsible for the increased ventilation during this physiologic state. It is thought that the “female” hormones, estrogen and progesterone, are protective against OSA due to their effect on the upper-airway dilator muscles [38]. Among women, the pre-menopausal period is the lowest risk for OSA and post-menopausal is highest [39]. Interestingly, polycystic ovary syndrome—a high androgen state—increases risk in pre-menopausal women and hormone replacement therapy decreases risk in post-menopausal women, supporting the notion that these hormones play an important role [39,40]. In the field of transgender medicine, there is a growing interest in the role of hormonal therapies on sleep. One case series described resolution of OSA in a transgender woman after initiation of estradiol and spironolactone [41]. Additionally, the authors described two cases of transgender men with pre- and post-testosterone polysomnograms demonstrating development of OSA following testosterone therapy.
Clinical Symptomatology
Presentation: The classic hallmark symptoms of OSA include snoring, gasping, and apneas. Women, however, tend to present in an atypical fashion with less frequent reports of snoring or witnessed apneas (Figure 2) [42,43]. At least one large study found that women are more likely than men to come to a clinical interview unaccompanied by their partner, raising the possibility that sociocultural factors may in part explain this finding [44]. Women are more likely to report non-specific symptoms of OSA, such as mood disturbance, lack of energy, daytime fatigue, morning headache, nightmares, and insomnia [42,45-48]. This discrepancy likely contributes to the underdiagnosis and delay in diagnosis of OSA in women relative to their male counterparts [49]. Additionally, although the prevalence of OSA significantly increases following menopause, the non-specific OSA symptoms commonly experienced by women are often attributed to menopausal symptoms, further delaying diagnosis of OSA [39,50]. Furthermore, one study found that the presence of severe vasomotor symptoms in menopause is an independent risk factor for OSA, highlighting the complexity of the relationship between menopause and OSA [51].
Figure 2.
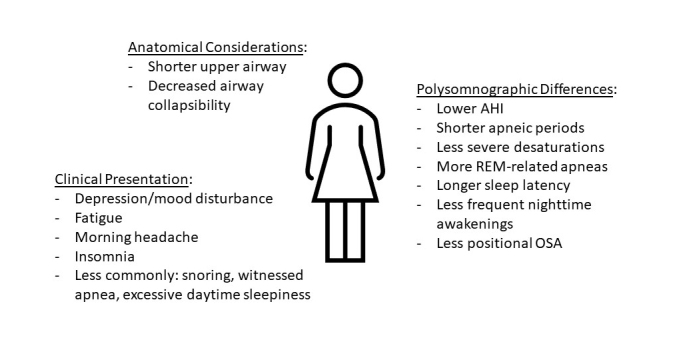
Female-Specific Obstructive Sleep Apnea Characteristics. Abbreviations: AHI = apnea-hypopnea index, REM = rapid eye movement, OSA = obstructive sleep apnea.
Questionnaires: Due to logistical challenges and cost, polysomnographic sleep evaluation is not possible in all patients with OSA risk factors. Thus, many tools and questionnaires have been created and validated to highlight those individuals at high risk who would most benefit from objective evaluation (Table 1). The Epworth Sleepiness Scale (ESS) was designed to objectively assess sleepiness. Questionnaires, such as STOP-BANG [52] and the Berlin questionnaire [53], have been created and validated to predict the likelihood of sleep-disordered breathing. Of note, the 2017 American Academy of Sleep Medicine guidelines strongly recommend against the use of clinical tools and questionnaires to diagnose OSA in the absence of objective sleep testing. The task force did, however, support their utility in non-sleep clinic settings to identify patients who are at increased risk for OSA [54].
Table 1. Common Obstructive Sleep Apnea Screening Tools.
| Tool | Description | Intended Use | Scoring |
| Epworth Sleepiness Scale | Assesses likelihood of falling asleep in 8 scenarios. | Objective assessment of sleepiness (not specific for OSA). | Score ≥10 indicates excessive sleepiness. |
| STOP-BANG Questionnaire | 8 items that address snoring, fatigue, apneas, hypertension, BMI, age, neck circumference, and sex. | Pre-operative screening for OSA. | Score of ≥3 suggests high risk of OSA. |
| Berlin Questionnaire | 3 categories: (1) snoring/apnea (2) somnolence (3) presence of hypertension/obesity |
Screening for OSA in the primary care setting. | One or more point in ≥2 categories suggests high risk of OSA. |
Abbreviations: OSA = obstructive sleep apnea, BMI = body mass index
The ESS is an eight-item tool designed to measure sleep propensity and may also be used to assess response to treatment [55]. It is often used in the primary care setting to screen for sleep-disordered breathing. Subjects are asked to rate their likelihood of falling asleep in different situations, and a point value of 0-3 is assigned to each question. A score of ≥10 is suggestive of a high burden of sleepiness. One study specifically looking at sex-related differences in ESS found that the tool did not correlate with the presence of mild-to-moderate OSA in women [56]. Furthermore, in those with severe OSA, the ESS had a smaller association in women relative to men. While this discrepancy suggests that routine screening for sleepiness in the primary care setting might erroneously sway providers from referring women for objective OSA testing, one study looking at ESS in pregnant women found a higher rate of unnecessary referral based on ESS score [57].
The STOP-BANG (Snoring, Tiredness, Observed apneas, high blood Pressure, Body mass index (BMI), Age, Neck circumference, and Gender) questionnaire was designed for preoperative screening. A meta-analysis performed demonstrated an overall acceptable performance of the questionnaire in the sleep clinic and surgical population for screening of OSA [52]. The authors found that higher scores correlated with greater probability of diagnosis of moderate-to-severe OSA on definitive testing. A more recent study aimed at comparing sex-specific diagnostic characteristics of the STOP-BANG questionnaire screened men and women with the questionnaire followed by objective testing with polysomnography [58]. The authors found that the sensitivity of the STOP-BANG questionnaire was unacceptably low in women as compared to men. The authors suggested sex-specific cut-offs for STOP-BANG and other questionnaires due to their skew toward men.
The Berlin questionnaire, designed as a screening tool in primary care, consists of 10 questions divided into three categories, including snoring/apnea, daytime somnolence, and presence of obesity or hypertension. A positive score in two or more categories suggests high risk for OSA [53]. A systemic review and meta-analysis demonstrated that the Berlin questionnaire has good overall sensitivity for detecting clinically relevant OSA in many patient populations, including the outpatient surgical, sleep, and primary care populations [59]. One study evaluated the effect of adding sex as a fourth category and assigned an additional point for male sex [60]. The authors found improved specificity and negative predictive value with the addition of sex in the score, however, they found overall insufficient validity to warrant use of the Berlin questionnaire.
Diagnostic Testing
Objective testing for OSA (Table 2) is recommended in patients with unexplained poor sleep or excessive daytime fatigue and should be considered in patients with nocturnal gastroesophageal reflux symptoms, headaches, recurrent persistent insomnia, and resistant hypertension. Given lack of consensus on utility of treatment in asymptomatic disease, the US Preventive Services Task Force does not recommend screening in asymptomatic patients [61]. Many experts agree, however, that consideration should be given to those who hold a commercial driver’s license [62]. These clinical guidelines are largely based on presentation characteristics stemming from male-predominant studies, which may drive underdiagnosis of OSA in women.
Table 2. Diagnostic Testing for Obstructive Sleep Apnea.
| Testing Modality | Parameters | Intended Use | Additional Factor |
| Polysomnography | Electroencephalogram, eye movements, chin tone, thoracic and abdominal excursion, airflow, pulse oximetry. | Criterion-standard tool for diagnosis of OSA and other sleep disorders. | Expensive; requires in-lab overnight stay. |
| Home Sleep Apnea Test | Different types of devices available Most common device includes: Airflow, respiratory effort, pulse oximetry. |
Often first-line test in patients with high pre-test probability of OSA. | Lower cost; does not differentiate between sleep and awake states; false negatives occur. |
Abbreviations: OSA = obstructive sleep apnea
The criterion-standard diagnostic test for OSA is the in-lab polysomnogram, which monitors sleep and respiratory patterns [1]. An in-lab polysomnogram requires an overnight stay at a sleep center and monitors nasal and oral air flow, respiratory and abdominal muscle efforts, oxygenation, heart rhythm, movements, and sleep stages. Disease severity is measured using the apnea-hypopnea index (AHI), ie, the average number of apneic and hypopneic events per hour. Apneas are defined as breathing pauses that last at least 10 seconds and hypopneas are reductions in airflow with associated desaturation by 3 or 4% or arousal from sleep. Home sleep apnea testing is a more cost-effective tool that is often used as an objective screening test for patients at high risk of OSA. While home sleep apnea testing can be more affordable and convenient, it is known to underestimate OSA presence and severity [63].
There are differences in polysomnographic findings in women compared to men (Figure 2). For example, women tend to have lower AHIs, shorter apneic episodes, less severe desaturations, a lower proportion of positional OSA, and apneas predominantly occurring during rapid eye movement (REM) sleep with relatively fewer respiratory disturbances in non-REM sleep [64-67]. Respiratory disturbances in women are less commonly associated with full collapse of the upper airway [64]. With regard to sleep architecture, one study found that women took longer to fall asleep than men but had fewer nighttime awakenings and more slow-wave sleep [66]. Despite a more benign-appearing polysomnographic phenotype, women do have significant OSA symptoms and comorbidities. Women tend to be symptomatic at lower AHIs than men. Possible explanations for this finding include more REM disruption or more episodes of partial upper airway obstruction in women compared with men [68].
Treatment and Outcomes
OSA is a chronic disease. The goals of treatment are to reduce symptoms, improve sleep quality, and potentially thwart the undesirable downstream cardiovascular effects associated with OSA. Untreated sleep apnea poses significant health risks, particularly for women who are at significantly increased risk of cardiovascular disease, diabetes, hyperlipidemia, and cognitive impairment [66,69,70].
Treatment of OSA is indicated in individuals with an AHI ≥5 and <15 plus symptoms or comorbidities caused or exacerbated by OSA or in those with an AHI ≥15 regardless of symptoms or comorbidities [71]. The most common treatment options (Table 3) include lifestyle modification, continuous positive airway pressure (CPAP) therapy, mandibular advancement devices, and surgery [27]. Since the decision to treat is based on AHI and women tend to have lower AHIs with more REM-predominant disease, women may be less likely to meet criteria for treatment. Underdiagnosis of OSA in women is even more pronounced when the threshold oxygen desaturation to define respiratory events is higher (ie, 4%) compared with a more inclusive definition of respiratory disturbances (ie, 3% or arousal) [67]. Conclusive data regarding sex-specific treatment outcomes is limited.
Table 3. Obstructive Sleep Apnea Treatment Options.
| Treatment | Description | Benefits | Disadvantages |
| Weight Loss | Goal of ≥10% decrease in total body weight. | Modest improvement in OSA severity in obese patients; many additional cardiovascular benefits. | Hard to maintain over time; lower efficacy than CPAP. |
| Continuous Positive Airway Pressure (CPAP) | Continuous positive pressure through airway to prevent collapse. | Highly effective (criterion-standard); improves quality of life, sleepiness, and blood pressure. | Requires adherence for benefit. |
| Mandibular Advancement Device | Dental appliance that advances the mandible forward during sleep. | Well-tolerated in those who are intolerant of CPAP. | Lower efficacy than CPAP; requires adequate dentition; variable insurance coverage. |
| Upper Airway Surgery | Surgical resection of pharyngeal soft tissue structures. | Improvement in OSA severity; ensures adherence. | Lower efficacy than CPAP; invasive and higher risk than alternatives. |
| Neurostimulation | Implanted electrode that stimulates the hypoglossal nerve to reduce airway collapse during inspiration. | Effective in select patients; well-tolerated. | Lower efficacy than CPAP; Highly selected patient population; requires favorable anatomy, BMI <32. |
Abbreviations: OSA = obstructive sleep apnea, CPAP = continuous positive airway pressure, BMI = body mass index
Lifestyle modification with weight loss should be recommended to overweight patients with OSA [72]. Weight loss of 10% total body weight has been shown to modestly improve the severity of OSA, however, it is challenging to maintain over time [73]. Meta-analyses looking at the role of bariatric surgery on OSA severity demonstrated a reduction in AHI following surgery, but residual average AHI consistent with moderate OSA [74-76]. There is significant gender disparity in weight loss surgery. Despite similar obesity rates in men and women, women comprise 80% of bariatric surgical patients [77]. In an observational cohort study comparing outcomes of bariatric surgery in men and women, of those with OSA preoperatively, 77.5% (31/40) men and 90% (36/40) women were able to discontinue CPAP postoperatively [78].
CPAP therapy is the criterion standard and most frequently prescribed treatment for OSA due to its high efficacy and safety [27]. As the name suggests, CPAP provides continuous positive pressure to the airway through the nose or mouth to improve airway collapsibility and decrease obstructive respiratory disturbances. Adherence and efficacy data can be objectively monitored to optimize therapy. A recent meta-analysis showed that patients with OSA treated with CPAP therapy had significant reduction in OSA severity, sleepiness, blood pressure, motor vehicle accidents, and sleep-related quality of life [79]. Despite these benefits, CPAP adherence, defined as use of the device for at least 4 hours per night for at least 70% of nights, remains a significant barrier [80]. Estimates of adherence in the literature range from 25-50%, but several studies have demonstrated improvement in CPAP adherence with the use of educational, behavioral, troubleshooting, and telemonitoring interventions [79,81]. Gender has been evaluated as a predictor of CPAP adherence, but results have not been consistent [82,83]. In a small study examining predictors of CPAP adherence in women (n=29), more symptomatic OSA (but not OSA severity by AHI) was associated with higher adherence. Additionally, adherent women were more likely than nonadherent women to be unmarried [84,85].
Mandibular advancement devices are an alternative therapy that can be considered in patients with OSA who do not tolerate CPAP [86]. Individual characteristics, such as lower BMI, lower AHI, small neck circumference, and female sex are predictors of positive response to mandibular advancement device treatment [87]. A meta-analysis comparing outcomes with CPAP versus mandibular advancement device found more significant AHI reduction with CPAP but better adherence with the mandibular advancement device [88]. The authors found no difference in quality of life, functional outcomes, or cognitive function between the two therapies. In a prospective study of oral appliance therapy in OSA, women were more likely to be successfully treated (defined as AHI <10) compared with men; gender did not impact adherence to therapy [89]. Rietz and colleagues assessed the impact of mandibular advancement devices on blood pressure in women versus men [90]. The authors found that women who used the device had a significant reduction in nocturnal systolic blood pressure compared to women who received a sham, whereas men had none [90]. The clinical relevance of this finding remains to be determined.
Surgical interventions for the treatment of OSA can be considered in patients who cannot tolerate first-line therapy or as an adjunct to CPAP in particularly severe cases [91]. Surgical candidacy depends on factors that include patient desire for surgery, medical fitness, and the existence of a surgically correctable problem. Upper pharyngeal procedures, such as uvulopalatopharyngoplasty, can be used to correct and reduce oropharyngeal structures leading to airway compromise during sleep. A systematic review and meta-analysis of uvulopalatopharyngoplasty demonstrated reduction in AHI on polysomnography, reduction in daytime sleepiness, and improved quality of life following surgery [92]. The vast majority of studies were male-predominant and the role of gender was not described. Maxillomandibular advancement and multilevel airway surgery may also be effective in carefully selected patients [93], but there is little data on the role of gender in surgical decision-making or outcomes.
More recently, upper airway neurostimulation with an implantable neurostimulator device has been offered to carefully selected patients with promising results [94]. Those eligible for the neurostimulator include adults with body mass index <32 with moderate or severe OSA, predominantly obstructive events, CPAP failure or intolerance, and no anatomical findings that would compromise performance of the device. The device stimulates both the upper and lower pharyngeal airway by activating the protrusion muscles of the tongue via branches of the hypoglossal nerve to open the lower pharyngeal airway. Most subjects in published studies have been male and the role of gender as a possible predictor of response has not been studied [95-97].
Conclusions and Outlook
Obstructive sleep apnea is a highly prevalent disease that causes significant morbidity if left untreated. Previously thought of as a predominantly male disease, OSA has more recently been shown to affect women at higher rates than previously thought. Furthermore, the incidence increases with increasing age. Additionally, women are less likely to be referred for diagnosis and treatment than their male counterparts [98]. Anatomical and physiological differences between men and women impact clinical symptomatology and utility of commonly used screening and diagnostic tests. Clinicians, therefore, should limit both implicit and explicit biases regarding OSA when evaluating patients with possible OSA. Future guidelines and screening tools should incorporate emerging data on sex and gender-related differences in OSA presentation since the literature is biased toward male subjects, which limits the generalizability of conclusions. Additionally, there is a need for investigators to focus on gender-related phenotypes, biomarkers, diagnostic criteria, and treatment decision-making and outcomes.
Glossary
- OSA
obstructive sleep apnea
- ESS
Epworth sleepiness scale
- BMI
body mass index
- AHI
apnea-hypopnea index
- REM
rapid eye movement
- CPAP
continuous positive airway pressure
References
- Berry RB, Quan SF, Abreu AR, Bibbs ML, DelRosso L, Harding SM, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version. 2.6 ed.Darien (IL): American Academy of Sleep Medicine; 2020. [Google Scholar]
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002May;165(9):1217–39. 10.1164/rccm.2109080 [DOI] [PubMed] [Google Scholar]
- Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000May;342(19):1378–84. 10.1056/NEJM200005113421901 [DOI] [PubMed] [Google Scholar]
- Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005November;353(19):2034–41. 10.1056/NEJMoa043104 [DOI] [PubMed] [Google Scholar]
- Alonderis A, Barbé F, Bonsignore M, Calverley P, De Backer W, Diefenbach K, et al. COST Action B-26. Medico-legal implications of sleep apnoea syndrome: driving license regulations in Europe. Sleep Med. 2008May;9(4):362–75. 10.1016/j.sleep.2007.05.008 [DOI] [PubMed] [Google Scholar]
- Hendrikx T, Sundqvist M, Sandström H, Sahlin C, Rohani M, Al-Khalili F, et al. Atrial fibrillation among patients under investigation for suspected obstructive sleep apnea. PLoS One. 2017February;12(2):e0171575. 10.1371/journal.pone.0171575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J, Cooperative Group Burgos-Santander. The association between sleep apnea and the risk of traffic accidents. N Engl J Med. 1999March;340(11):847–51. 10.1056/nejm199903183401104 [DOI] [PubMed] [Google Scholar]
- Lutsey PL, Bengtson LG, Punjabi NM, Shahar E, Mosley TH, Gottesman RF, et al. Obstructive Sleep Apnea and 15-Year Cognitive Decline: The Atherosclerosis Risk in Communities (ARIC) Study. Sleep. 2016February;39(2):309–16. 10.5665/sleep.5434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findley LJ, Barth JT, Powers DC, Wilhoit SC, Boyd DG, Suratt PM. Cognitive impairment in patients with obstructive sleep apnea and associated hypoxemia. Chest. 1986November;90(5):686–90. 10.1378/chest.90.5.686 [DOI] [PubMed] [Google Scholar]
- Chaudhary P, Goyal A, Goel SK, Kumar A, Chaudhary S, Kirti Keshri S, et al. Women with OSA have higher chances of having metabolic syndrome than men: effect of gender on syndrome Z in cross sectional study. Sleep Med. 2021;79:83-7. Epub 20210102. doi: 10.1016/j.sleep.2020.12.042. [DOI] [PubMed] [Google Scholar]
- Tarasiuk A, Reuveni H. The economic impact of obstructive sleep apnea. Curr Opin Pulm Med. 2013November;19(6):639–44. 10.1097/MCP.0b013e3283659e1e [DOI] [PubMed] [Google Scholar]
- Knauert M, Naik S, Gillespie MB, Kryger M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg. 2015;1(1):17-27. Epub 20150908. doi: 10.1016/j.wjorl.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. 2015August;7(8):1311–22. 10.3978/j.issn.2072-1439.2015.06.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbay IE, Lavie P. Age- and gender-related characteristics of obstructive sleep apnea. Sleep Breath. 2012June;16(2):453–60. 10.1007/s11325-011-0523-z [DOI] [PubMed] [Google Scholar]
- Lindberg E, Benediktsdottir B, Franklin KA, Holm M, Johannessen A, Jogi R, et al. Gender differences in sleep disordered breathing. Eur Respir J. 2015;46:PA2377. 10.1183/13993003.congress-2015.PA2377 [DOI] [Google Scholar]
- Grunstein RR, Stenlöf K, Hedner JA, Sjöström L. Impact of self-reported sleep-breathing disturbances on psychosocial performance in the Swedish Obese Subjects (SOS) Study. Sleep. 1995October;18(8):635–43. 10.1093/sleep/18.8.635 [DOI] [PubMed] [Google Scholar]
- Sjösten N, Kivimäki M, Oksanen T, Salo P, Saaresranta T, Virtanen M, et al. Obstructive sleep apnoea syndrome as a predictor of work disability. Respir Med. 2009July;103(7):1047–55. 10.1016/j.rmed.2009.01.014 [DOI] [PubMed] [Google Scholar]
- Rod NH, Kjeldgård L, Åkerstedt T, Ferrie JE, Salo P, Vahtera J, et al. Sleep Apnea, Disability Pensions, and Cause-Specific Mortality: A Swedish Nationwide Register Linkage Study. Am J Epidemiol. 2017September;186(6):709–18. 10.1093/aje/kwx138 [DOI] [PubMed] [Google Scholar]
- Simpson L, Hillman DR, Cooper MN, Ward KL, Hunter M, Cullen S, et al. High prevalence of undiagnosed obstructive sleep apnoea in the general population and methods for screening for representative controls. Sleep Breath. 2013September;17(3):967–73. 10.1007/s11325-012-0785-0 [DOI] [PubMed] [Google Scholar]
- Apps MC, Gillon JC, Stradling JR. Underdiagnosis of obstructive sleep apnea in Britain. Lancet. 1983May;1(8332):1054. 10.1016/S0140-6736(83)92686-7 [DOI] [PubMed] [Google Scholar]
- Lettieri CJ, Eliasson AH, Andrada T, Khramtsov A, Raphaelson M, Kristo DA. Obstructive sleep apnea syndrome: are we missing an at-risk population? J Clin Sleep Med. 2005October;1(4):381–5. 10.5664/jcsm.26366 [DOI] [PubMed] [Google Scholar]
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993April;328(17):1230–5. 10.1056/nejm199304293281704 [DOI] [PubMed] [Google Scholar]
- Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013May;177(9):1006–14. 10.1093/aje/kws342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DA, Guo N, Rueschman M, Wang R, Wilson JG, Redline S. Prevalence and correlates of obstructive sleep apnea among African Americans: the Jackson Heart Sleep Study. Sleep. 2018October;41(10): 10.1093/sleep/zsy154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin KA, Sahlin C, Stenlund H, Lindberg E. Sleep apnoea is a common occurrence in females. Eur Respir J. 2013March;41(3):610–5. 10.1183/09031936.00212711 [DOI] [PubMed] [Google Scholar]
- Schiza SE, Bouloukaki I. Does gender matter: sex-specific aspects of symptoms, outcome, and therapy of obstructive sleep apnea. Curr Opin Pulm Med. 2020November;26(6):642–9. 10.1097/mcp.0000000000000728 [DOI] [PubMed] [Google Scholar]
- Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009June;5(3):263–76. 10.5664/jcsm.27497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann DM, Bassetti CL. Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery. Neurology. 2016September;87(13):1407–16. 10.1212/wnl.0000000000003037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suratt PM, Dee P, Atkinson RL, Armstrong P, Wilhoit SC. Fluoroscopic and computed tomographic features of the pharyngeal airway in obstructive sleep apnea. Am Rev Respir Dis. 1983April;127(4):487–92. 10.1164/arrd.1983.127.4.487 [DOI] [PubMed] [Google Scholar]
- Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of Sleep Apnea (vol 90, pg 47, 2010). Physiol Rev. 2010;90(2):797–8. 10.1152/physrev.z9j-2526-corr.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, Darendeliler MA, et al. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep. 2010August;33(8):1075–80. 10.1093/sleep/33.8.1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan AS, White DP. Pharyngeal motor control and the pathogenesis of obstructive sleep apnea. Respir Physiol Neurobiol. 2008January;160(1):1–7. 10.1016/j.resp.2007.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, Nishino T. Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol. 1997April;82(4):1319–26. 10.1152/jappl.1997.82.4.1319 [DOI] [PubMed] [Google Scholar]
- Malhotra A, Huang Y, Fogel RB, Pillar G, Edwards JK, Kikinis R, et al. The male predisposition to pharyngeal collapse: importance of airway length. Am J Respir Crit Care Med. 2002November;166(10):1388–95. 10.1164/rccm.2112072 [DOI] [PubMed] [Google Scholar]
- Ronen O, Malhotra A, Pillar G. Influence of gender and age on upper-airway length during development. Pediatrics. 2007October;120(4):e1028–34. 10.1542/peds.2006-3433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargaglioni LH, Marques DA, Patrone LGA. Sex differences in breathing. Comparative Biochemistry and Physiology a-Molecular & Integrative Physiology. 2019;238. doi: 10.1016/j.cbpa.2019.110543. [DOI] [PubMed] [Google Scholar]
- Regensteiner JG, Woodard WD, Hagerman DD, Weil JV, Pickett CK, Bender PR, et al. Combined effects of female hormones and metabolic rate on ventilatory drives in women. J Appl Physiol. 1989February;66(2):808–13. 10.1152/jappl.1989.66.2.808 [DOI] [PubMed] [Google Scholar]
- Zhang L, Ou X, Zhu T, Lv X. Beneficial effects of estrogens in obstructive sleep apnea hypopnea syndrome. Sleep Breath. 2020March;24(1):7–13. 10.1007/s11325-019-01896-2 [DOI] [PubMed] [Google Scholar]
- Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001March;163(3 Pt 1):608–13. 10.1164/ajrccm.163.3.9911064 [DOI] [PubMed] [Google Scholar]
- Kahal H, Kyrou I, Uthman OA, Brown A, Johnson S, Wall PD, et al. The prevalence of obstructive sleep apnoea in women with polycystic ovary syndrome: a systematic review and meta-analysis. Sleep Breath. 2020March;24(1):339–50. 10.1007/s11325-019-01835-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson BD, Lerner BS, Collen JF, Smith PR. The Effects of Transgender Hormone Therapy on Sleep and Breathing: A Case Series. J Clin Sleep Med. 2019October;15(10):1529–33. 10.5664/jcsm.7992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levartovsky A, Dafna E, Zigel Y, Tarasiuk A. Breathing and Snoring Sound Characteristics during Sleep in Adults. J Clin Sleep Med. 2016March;12(3):375–84. 10.5664/jcsm.5588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enright PL, Newman AB, Wahl PW, Manolio TA, Haponik EF, Boyle PJ. Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep. 1996September;19(7):531–8. 10.1093/sleep/19.7.531 [DOI] [PubMed] [Google Scholar]
- Quintana-Gallego E, Carmona-Bernal C, Capote F, Sánchez-Armengol A, Botebol-Benhamou G, Polo-Padillo J, et al. Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med. 2004October;98(10):984–9. 10.1016/j.rmed.2004.03.002 [DOI] [PubMed] [Google Scholar]
- Wahner-Roedler DL, Olson EJ, Narayanan S, Sood R, Hanson AC, Loehrer LL, et al. Gender-specific differences in a patient population with obstructive sleep apnea-hypopnea syndrome. Gend Med. 2007December;4(4):329–38. 10.1016/s1550-8579(07)80062-3 [DOI] [PubMed] [Google Scholar]
- Shepertycky MR, Banno K, Kryger MH. Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome. Sleep. 2005March;28(3):309–14. [PubMed] [Google Scholar]
- Valipour A, Lothaller H, Rauscher H, Zwick H, Burghuber OC, Lavie P. Gender-related differences in symptoms of patients with suspected breathing disorders in sleep: a clinical population study using the sleep disorders questionnaire. Sleep. 2007March;30(3):312–9. 10.1093/sleep/30.3.312 [DOI] [PubMed] [Google Scholar]
- Nigro CA, Dibur E, Borsini E, Malnis S, Ernst G, Bledel I, et al. The influence of gender on symptoms associated with obstructive sleep apnea. Sleep Breath. 2018September;22(3):683–93. 10.1007/s11325-017-1612-4 [DOI] [PubMed] [Google Scholar]
- Basoglu OK, Tasbakan MS. Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath. 2018March;22(1):241–9. 10.1007/s11325-017-1482-9 [DOI] [PubMed] [Google Scholar]
- Anttalainen U, Saaresranta T, Aittokallio J, Kalleinen N, Vahlberg T, Virtanen I, et al. Impact of menopause on the manifestation and severity of sleep-disordered breathing. Acta Obstet Gynecol Scand. 2006;85(11):1381–8. 10.1080/00016340600935649 [DOI] [PubMed] [Google Scholar]
- Gao CC, Kapoor E, Lipford MC, Miller VM, Schroeder DR, Mara KC, et al. Association of vasomotor symptoms and sleep apnea risk in midlife women. Menopause. 2018April;25(4):391–8. 10.1097/gme.0000000000001020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, et al. Validation of the STOP-Bang Questionnaire as a Screening Tool for Obstructive Sleep Apnea among Different Populations: A Systematic Review and Meta-Analysis. PLoS One. 2015December;10(12):e0143697. 10.1371/journal.pone.0143697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Annals of Internal Medicine. 1999;131(7):485-+. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017March;13(3):479–504. 10.5664/jcsm.6506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991December;14(6):540–5. 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- Lipford MC, Wahner-Roedler DL, Welsh GA, Mandrekar J, Thapa P, Olson EJ. Correlation of the Epworth Sleepiness Scale and Sleep-Disordered Breathing in Men and Women. J Clin Sleep Med. 2019January;15(1):33–8. 10.5664/jcsm.7564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony KM, Agrawal A, Arndt ME, Murphy AM, Alapat PM, Guntupalli KK, et al. Obstructive sleep apnea in pregnancy: reliability of prevalence and prediction estimates. J Perinatol. 2014August;34(8):587–93. 10.1038/jp.2014.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauters FA, Loof S, Hertegonne KB, Chirinos JA, De Buyzere ML, Rietzschel ER. Sex-specific sleep apnea screening questionnaires: closing the performance gap in women. Sleep Med. 2020March;67:91–8. 10.1016/j.sleep.2019.10.023 [DOI] [PubMed] [Google Scholar]
- Senaratna CV, Perret JL, Matheson MC, Lodge CJ, Lowe AJ, Cassim R, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2017December;36:116–24. 10.1016/j.smrv.2017.04.001 [DOI] [PubMed] [Google Scholar]
- Yüceege M, Fırat H, Sever Ö, Demir A, Ardıç S. The effect of adding gender item to Berlin Questionnaire in determining obstructive sleep apnea in sleep clinics. Ann Thorac Med. 2015Jan-Mar;10(1):25–8. 10.4103/1817-1737.146856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas DE, Amick HR, Feltner C, Weber RP, Arvanitis M, Stine A, et al. Screening for Obstructive Sleep Apnea in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2017January;317(4):415–33. 10.1001/jama.2016.19635 [DOI] [PubMed] [Google Scholar]
- Gurubhagavatula I, Maislin G, Nkwuo JE, Pack AI. Occupational screening for obstructive sleep apnea in commercial drivers. Am J Respir Crit Care Med. 2004August;170(4):371–6. 10.1164/rccm.200307-968OC [DOI] [PubMed] [Google Scholar]
- Bianchi MT, Goparaju B. Potential Underestimation of Sleep Apnea Severity by At-Home Kits: Rescoring In-Laboratory Polysomnography Without Sleep Staging. J Clin Sleep Med. 2017April;13(4):551–5. 10.5664/jcsm.6540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapsimalis F, Kryger MH. Gender and obstructive sleep apnea syndrome, part 1: clinical features. Sleep. 2002June;25(4):412–9. 10.1093/sleep/25.4.409 [DOI] [PubMed] [Google Scholar]
- Kulkas A, Duce B, Leppänen T, Hukins C, Töyräs J. Gender differences in severity of desaturation events following hypopnea and obstructive apnea events in adults during sleep. Physiol Meas. 2017July;38(8):1490–502. 10.1088/1361-6579/aa7b6f [DOI] [PubMed] [Google Scholar]
- Bouloukaki I, Mermigkis C, Markakis M, Pataka A, Alexaki I, Ermidou C, et al. Cardiovascular Effect and Symptom Profile of Obstructive Sleep Apnea: Does Sex Matter? J Clin Sleep Med. 2019December;15(12):1737–45. 10.5664/jcsm.8074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Won CH, Reid M, Sofer T, Azarbarzin A, Purcell S, White D, et al. Sex differences in obstructive sleep apnea phenotypes, the multi-ethnic study of atherosclerosis. Sleep. 2020May;43(5):zsz274. 10.1093/sleep/zsz274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wimms A, Woehrle H, Ketheeswaran S, Ramanan D, Armitstead J. Obstructive Sleep Apnea in Women: Specific Issues and Interventions. BioMed Res Int. 2016;2016:1764837. 10.1155/2016/1764837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg-Dotan S, Reuveni H, Simon-Tuval T, Oksenberg A, Tarasiuk A. Gender differences in morbidity and health care utilization among adult obstructive sleep apnea patients. Sleep. 2007September;30(9):1173–80. 10.1093/sleep/30.9.1173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K, Laffan AM, Harrison SL, Redline S, Spira AP, Ensrud KE, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011August;306(6):613–9. 10.1001/jama.2011.1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2019February;15(2):335–43. 10.5664/jcsm.7640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudgel DW, Patel SR, Ahasic AM, Bartlett SJ, Bessesen DH, Coaker MA, et al. American Thoracic Society Assembly on Sleep and Respiratory Neurobiology. The Role of Weight Management in the Treatment of Adult Obstructive Sleep Apnea. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2018September;198(6):e70–87. 10.1164/rccm.201807-1326ST [DOI] [PubMed] [Google Scholar]
- Joosten SA, Hamilton GS, Naughton MT. Impact of Weight Loss Management in OSA. Chest. 2017July;152(1):194–203. 10.1016/j.chest.2017.01.027 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wang W, Yang C, Shen J, Shi M, Wang B. Improvement in Nocturnal Hypoxemia in Obese Patients with Obstructive Sleep Apnea after Bariatric Surgery: a Meta-Analysis. Obes Surg. 2019February;29(2):601–8. 10.1007/s11695-018-3573-5 [DOI] [PubMed] [Google Scholar]
- Wong AM, Barnes HN, Joosten SA, Landry SA, Dabscheck E, Mansfield DR, et al. The effect of surgical weight loss on obstructive sleep apnoea: A systematic review and meta-analysis. Sleep Med Rev. 2018December;42:85–99. 10.1016/j.smrv.2018.06.001 [DOI] [PubMed] [Google Scholar]
- Greenburg DL, Lettieri CJ, Eliasson AH. Effects of surgical weight loss on measures of obstructive sleep apnea: a meta-analysis. Am J Med. 2009June;122(6):535–42. 10.1016/j.amjmed.2008.10.037 [DOI] [PubMed] [Google Scholar]
- Aly S, Hachey K, Pernar LI. Gender disparities in weight loss surgery. Mini-invasive Surgery. 2020;4:21. 10.20517/2574-1225.2019.57 [DOI] [Google Scholar]
- Kennedy-Dalby A, Adam S, Ammori BJ, Syed AA. Weight loss and metabolic outcomes of bariatric surgery in men versus women - A matched comparative observational cohort study. Eur J Intern Med. 2014December;25(10):922–5. 10.1016/j.ejim.2014.10.020 [DOI] [PubMed] [Google Scholar]
- Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea With Positive Airway Pressure: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J Clin Sleep Med. 2019February;15(2):301–34. 10.5664/jcsm.7638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993April;147(4):887–95. 10.1164/ajrccm/147.4.887 [DOI] [PubMed] [Google Scholar]
- Wolkove N, Baltzan M, Kamel H, Dabrusin R, Palayew M. Long-term compliance with continuous positive airway pressure in patients with obstructive sleep apnea. Can Respir J. 2008October;15(7):365–9. 10.1155/2008/534372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010February;131(2):245–58. [PMC free article] [PubMed] [Google Scholar]
- Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002February;121(2):430–5. 10.1378/chest.121.2.430 [DOI] [PubMed] [Google Scholar]
- Libman E, Bailes S, Fichten C, Rizzo D, Creti L, Bailes M, et al. CPAP Treatment Adherence in Women with Obstructive Sleep Apnea. Sleep Disord. 2017;40:A302-A. doi: 10.1093/sleepj/zsx050.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye L, Pien GW, Ratcliffe SJ, Weaver TE. Gender differences in obstructive sleep apnea and treatment response to continuous positive airway pressure. J Clin Sleep Med. 2009December;5(6):512–8. 10.5664/jcsm.27650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: an Update for 2015. J Clin Sleep Med. 2015July;11(7):773–827. 10.5664/jcsm.4858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Eckert DJ, van der Stelt PF, Guo J, Ge S, Emami E, et al. Phenotypes of responders to mandibular advancement device therapy in obstructive sleep apnea patients: A systematic review and meta-analysis. Sleep Med Rev. 2020February;49:101229. 10.1016/j.smrv.2019.101229 [DOI] [PubMed] [Google Scholar]
- Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R. Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath. 2018September;22(3):555–68. 10.1007/s11325-017-1590-6 [DOI] [PubMed] [Google Scholar]
- Marklund M, Stenlund H, Franklin KA. Mandibular advancement devices in 630 men and women with obstructive sleep apnea and snoring: tolerability and predictors of treatment success. Chest. 2004April;125(4):1270–8. 10.1378/chest.125.4.1270 [DOI] [PubMed] [Google Scholar]
- Rietz H, Franklin KA, Carlberg B, Sahlin C, Marklund M. Nocturnal Blood Pressure Is Reduced by a Mandibular Advancement Device for Sleep Apnea in Women: Findings From Secondary Analyses of a Randomized Trial. J Am Heart Assoc. 2018June;7(13):13. 10.1161/jaha.118.008642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aurora RN, Casey KR, Kristo D, Auerbach S, Bista SR, Chowdhuri S, et al. American Academy of Sleep Medicine. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010October;33(10):1408–13. 10.1093/sleep/33.10.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuck BA, Ravesloot MJ, Eschenhagen T, de Vet HC, Sommer JU. Uvulopalatopharyngoplasty with or without tonsillectomy in the treatment of adult obstructive sleep apnea - A systematic review. Sleep Med. 2018October;50:152–65. 10.1016/j.sleep.2018.05.004 [DOI] [PubMed] [Google Scholar]
- Zhou N, Ho JT, Huang Z, Spijker R, de Vries N, Aarab G, et al. Maxillomandibular advancement versus multilevel surgery for treatment of obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2021June;57:101471. 10.1016/j.smrv.2021.101471 [DOI] [PubMed] [Google Scholar]
- Costantino A, Rinaldi V, Moffa A, Luccarelli V, Bressi F, Cassano M, et al. Hypoglossal nerve stimulation long-term clinical outcomes: a systematic review and meta-analysis. Sleep Breath. 2020June;24(2):399–411. 10.1007/s11325-019-01923-2 [DOI] [PubMed] [Google Scholar]
- Steffen A, Kilic A, König IR, Suurna MV, Hofauer B, Heiser C. Tongue motion variability with changes of upper airway stimulation electrode configuration and effects on treatment outcomes. Laryngoscope. 2018August;128(8):1970–6. 10.1002/lary.27064 [DOI] [PubMed] [Google Scholar]
- Strollo PJ Jr, Soose RJ, Maurer JT, de Vries N, Cornelius J, Froymovich O, et al. STAR Trial Group. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014January;370(2):139–49. 10.1056/NEJMoa1308659 [DOI] [PubMed] [Google Scholar]
- Eastwood PR, Barnes M, MacKay SG, Wheatley JR, Hillman DR, Nguyên XL, et al. Bilateral hypoglossal nerve stimulation for treatment of adult obstructive sleep apnoea. Eur Respir J. 2020January;55(1):1901320. 10.1183/13993003.01320-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindberg E, Benediktsdottir B, Franklin KA, Holm M, Johannessen A, Jögi R, et al. Women with symptoms of sleep-disordered breathing are less likely to be diagnosed and treated for sleep apnea than men. Sleep Med. 2017;35:17-22. Epub 20170423. doi: 10.1016/j.sleep.2017.02.032. [DOI] [PubMed] [Google Scholar]