Abstract
Objectives
To evaluate feasibility and acceptability of a group-based nature recreation intervention (nature hiking) and control condition (urban hiking) for military Veterans with post-traumatic stress disorder (PTSD).
Design and setting
A pilot randomised controlled trial conducted in the US Pacific Northwest.
Participants
Veterans with PTSD due to any cause.
Interventions
Twenty-six participants were randomised to a 12-week intervention involving either six nature hikes (n=13) or six urban hikes (n=13).
Primary and secondary outcome measures
Feasibility was assessed based on recruitment, retention and attendance. Questionnaires and postintervention qualitative interviews were conducted to explore intervention acceptability. Questionnaires assessing acceptability and outcomes planned for the future trial (eg, PTSD symptoms) were collected at baseline, 6 weeks, 12 weeks (immediately after the final hike) and 24 weeks follow-up.
Results
Of 415 people assessed for eligibility/interest, 97 were interested and passed preliminary eligibility screening, and 26 were randomised. Mean completion of all questionnaires was 91% among those in the nature hiking group and 68% in those in the urban hiking group. Over the course of the intervention, participants in the nature and urban groups attended an average of 56% and 58%, respectively, of scheduled hikes. Acceptability of both urban and nature hikes was high; over 70% reported a positive rating (ie, good/excellent) for the study communication, as well as hike locations, distance and pace. Median PTSD symptom scores (PTSD Checklist-5) improved more at 12 weeks and 24 weeks among those in the nature versus urban hiking group.
Conclusions
This pilot study largely confirmed the feasibility and acceptability of nature hiking as a potential treatment for Veterans with PTSD. Adaptations will be needed to improve recruitment and increase hike attendance for a future randomised controlled trial to effectively test and isolate the ways in which nature contact, physical activity and social support conferred by the group impact outcomes.
Trial registration number
Keywords: adult psychiatry, trauma management, complementary medicine, public health
Strengths and limitations of this study.
By using group-based urban hiking as a comparison group to control for the effects of physical activity and social cohesion (present in both interventions), this study was designed to isolate benefits specifically due to the environment (which differed between the interventions).
We used population-based recruitment methods to enroll a representative sample of Veterans with post-traumatic stress disorder.
Because of its small size and focus on feasibility, the study was not large enough to determine the effectiveness of nature hiking on outcomes.
Introduction
Post-traumatic stress disorder (PTSD) is a common, chronic mental health condition that affects up to 30% of military Veterans and is frequently comorbid with anxiety, depression and substance misuse.1–3 PTSD increases the risk of suicide as well as obesity, physical inactivity and cardiovascular and metabolic disorders.1–12 Clinical practice guidelines recommend treatment with several evidence-based psychotherapies and medications,13 but many Veterans who need PTSD treatment do not receive it.14 Barriers to obtaining treatment include concerns about medication side effects, desire for self-management approaches, stigma about receiving mental healthcare and a lack of confidence in mental health treatment in general.14–17 These and other factors adversely impact engagement, contributing to low initiation of14 18–22 and high drop-out rates from treatment.20 23 24 Identifying a wider range of approaches that are acceptable and effective is key to reducing the burden PTSD places on individuals and their communities.
There is growing interest in nature contact as a potential therapy for Veterans with PTSD and robust evidence that nature contact improves physical and psychological health among healthy individuals and those with mental health disorders.25 Nature contact has been shown to increase subjective well-being; decrease stress, anxiety, depression and negative affect; and promote adaptive shifts in emotion regulation.25 26 Benefits of nature contact are generally posited to occur based on two theories: attention restoration theory (ART) and stress recovery theory (SRT).27 28 ART theorises that nature contact improves cognitive function through a replenishment of ‘directed attention’, a capacity that is overly taxed in urban environments due to the need to block out distracting stimuli (eg, noise) to focus on a specific task or cognitive process. This depleted attention capacity can be restored in natural environments through the engagement of ‘soft fascination’, with implications for both cognitive and emotional well-being. SRT is based on psychoevolutionary principles, and posits that many types of nature exposure enhance psychological well-being through a precognitive, positive affective response and activation of the parasympathetic nervous system in ways that reduce stress and sympathetic nervous system arousal.26 29 30
Like nature contact, physical activity (PA) is considered to be a promising approach to improve outcomes for individuals with PTSD. PA reduces anxiety and depression and improves stress regulation, sleep and cognitive functioning in the general population,10 11 31 and in people with PTSD, though only 8 studies have involved randomised controlled trial (RCT) designs,4 32–39 and 5 of the RCTs were pilot studies or included fewer than 30 people.32 33 35 38 39 Furthermore, we are aware of only one RCT focused on Veterans.39 Group-based PA interventions may be particularly well-suited for military Veterans, due to (1) proportionally higher rates of PTSD among Veterans,40 (2) consistency of PA interventions with values cultivated during military service and (3) benefits of social interaction with veteran peers.41 To our knowledge, no PA interventions in those with PTSD investigated the PA environment as a component of treatment. This is an important omission, because the environment in which PA takes place may play an important role in its benefits.42
Green exercise, defined as activity that takes place in natural environments, is a burgeoning area of research.43–48 A number of studies have documented benefits from green exercise in Veteran populations and among individuals with PTSD.45–55 The specific interventions studied (from care farming to river rafting), dose/duration and inclusion of additional, explicit therapeutic components vary substantially among studies. A 2019 systematic review that examined evidence for the proposed additive effects of exercise in the presence of nature observed some benefits (eg, lower perceived exertion and enjoyment). Nevertheless, the authors concluded that there was a high risk of bias across trials and an overall low quality of evidence.44 Thus, uncertainty about the duration and impacts of green exercise remains due to methodological issues and because most interventional studies tested only a single bout of exercise.43 44 Furthermore, in the studies including Veterans, important limitations include low retention for follow-up, absence of control groups and insufficient statistical power.52–58
In addition to nature contact and PA, a third important constituent of many green exercise interventions is a group component. Some recent research suggests that increased social cohesion and connectedness may mediate benefits of green exercise,59 but findings are inconsistent.60 Social support forged through group activity could be particularly relevant for Veterans, as camaraderie and solidarity are critical components of military culture, and ones that are frequently lost in the return to civilian life.61 Social support is associated with reduced PTSD symptoms and improved treatment response62 and may directly impact stress response by increasing personal resources,63 and/or may indirectly impact PTSD symptom severity and response to treatment through buffering the potentially harmful impacts of stressful events.64
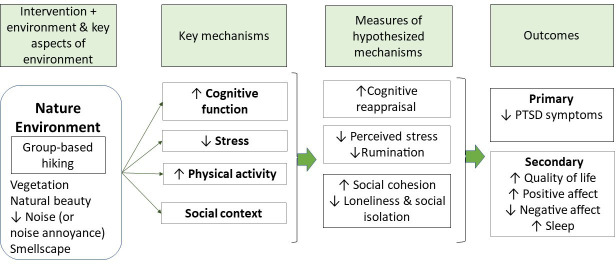
Adequately powered studies involving ongoing green exercise that are designed to distinguish between benefits due to PA and those due to the physical (eg, nature) and social (eg, group cohesion) environment are needed. Thus, our goal was to design and conduct a pilot study to test the feasibility and acceptability of a green exercise intervention for PTSD symptoms in military Veterans, regardless of PTSD aetiology. The intervention (nature hiking) and the active control (urban hiking) were group based and involved similar amounts of PA, to ensure control of the potential benefits of the group-based social support and of PA. Figure 1 depicts our conceptual model. This paper describes the results of the initial pilot study designed to emulate important elements of the future envisioned full-scale randomised trial.
Figure 1.
Conceptual model.
Methods
Identification and recruitment of participants
We used active and passive methods to identify and recruit Veterans to participate. While receiving care at a Department of Veterans Affairs (VA) healthcare facility was not an inclusion criterion, we used VA electronic medical records as a key source to identify potentially eligible Veterans. We identified VA enrollees (identified using electronic medical records) with at least one encounter with a diagnosis of PTSD in the prior 2 years; a zip code in one of three Seattle-Tacoma area counties (King, Snohomish and Pierce); no hospitalisations in the prior 3 months; and no diagnoses of schizophrenia, bipolar disorder or other psychotic disorder. We randomly selected 1001 individuals who met these criteria from a total of approximately 7000 and mailed them a letter informing them about the study and inviting them to participate. We followed the mailing with up to three phone calls until the recruitment period ended. We also placed study recruitment flyers in clinics in the VA Puget Sound and mailed flyers to four local organisations and clinics serving Veterans. Individuals who expressed an interest were mailed an invitation letter.
We initially screened all Veterans who expressed an interest in participating for eligibility over the phone; inclusion criteria assessed included a history of PTSD, ability/willingness to comply with study procedures (eg, complete questionnaires, wear and sync an activity monitor, drive to hikes and walk at least 2 hours at an easy/moderate pace over uneven terrain). Exclusion criteria assessed included a diagnosis of schizophrenia, bipolar disorder or other psychotic disorder; hospital admission in the prior 3 months and inability to perform unsupervised PA based on the PA Readiness Questionnaire.65 We invited those who passed all criteria except for the PA Readiness Questionnaire to obtain approval to participate from their primary care provider. Though some of this information was available in VA medical records, because we also included Veterans who did not have VA medical records, we employed methods that allowed us to evaluate eligibility without medical record access. Those who passed initial screening were mailed consent forms and given a link to complete a more extensive screening questionnaire online. Via the online screening questionnaire, PTSD symptoms, drug use, alcohol misuse and suicidality were assessed. PTSD was determined based on a PTSD-checklist-566 score >33. We excluded those with drug abuse in past year (Drug Abuse Screening Test-1067 score >=3); alcohol disorder/dependence (current/past year; Alcohol Use Disorders Identification Test-1068 score >16) and moderate/severe suicidality (past month; Mini International Neuropsychiatric Interview (MINI) Suicidality module69 score >5). Those who were eligible and returned signed consents were considered enrolled in the study.
Study design
We conducted a two-arm randomised controlled pilot trial. The two interventions were group nature and group urban hiking. The random 1:1 allocation sequence was generated using simple randomisation in random blocks of 2, 4 and 6. Randomisation assignments were placed in opaque sequentially numbered envelopes. Once an individual was determined to be eligible, the study coordinator selected the next envelope to determine the individual’s group assignment. We did not blind participants, the study coordinator or the study statistician to group assignment. Figure 2 presents an overview of the study, including timing of assessments.
Figure 2.
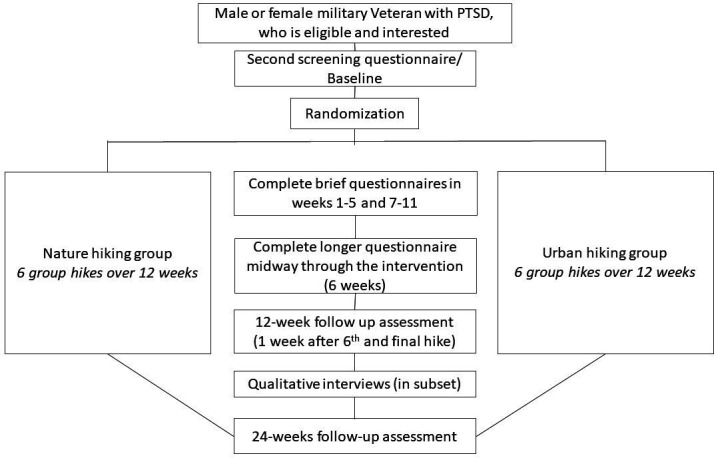
Depiction of study design and assessments. PTSD, post-traumatic stress disorder.
Description of hike locations and amenities
The criteria used to select the hike locations (which applied to both nature and urban hikes) included duration, elevation change, availability of facilities (eg, toilets and water), distance from participants’ homes and access to parking. Nature hikes were held in State Parks, National Wildlife Refuges and Natural Resources Conservation areas in the US Pacific Northwest. The nature hikes were in forest habitat, including old growth forest, saltwater shoreline, waterfalls and alpine lakes. Elevations ranged from sea level to 2200 feet above sea level. Urban hikes were held in primarily built environments, avoiding urban parks or primarily residential neighbourhoods with substantial greenery or water features. Urban hikes comprised areas that included sports stadiums, urban art and retail establishments and were mainly on sidewalks rather than separated bike/pedestrian paths/rail-trails. It was not feasible to match nature and urban hikes on elevation change; instead, we aimed to have similar hike durations to match total exertion. Generally, nature hikes involved somewhat shorter distances but included more elevation gain/loss.
Hiking intervention
A total of six hikes over 12 weeks (one every other week) were offered between August and October 2019. We chose to offer six hikes (vs more or fewer) because this number was thought to be feasible and would be sufficient to assess feasibility and acceptability. The standard structure for hikes was: (1) ‘ice breakers’ (short, guided conversations), (2) overview of the planned hike, including distance, unique features and planned stops, (3) hike and (4) posthike debrief and administration of questionnaires. There were no additional group/therapeutic activities.
Hike durations increased gradually to account for anticipated increases in participants’ physical fitness. Initial hikes were 60–90 min (2–3 miles), and later hikes were 2–3 hours (5–6 miles). To ensure safety and inclusion, one hike leader was in sight and hearing of the first participant and a second leader accompanied the last participant. The group stopped at least every 30 min to keep everyone together and offer opportunities to rest, regroup and inquire about and address any issues or concerns arising since the last check-in.
The same hike leaders, who were non-clinicians, led both nature and urban hikes to control for hike leader effects. On every hike, at least one of the leaders was a woman. Leaders were experienced outdoor educators who were employed by a Seattle-based outdoor organisation that provides outdoor recreation activities for people with disabilities. While the leaders were not Veterans, the organisation received grants from the VA as part of the Adaptive Sports Programme70 and had previously led programmes for Veterans. Leaders were trained to handle physical and mental health emergencies by the PIs (AJL and GNB) and a co-investigator who is a licensed clinical psychologist (KL). AJL and GNB supervised the hike leaders during the study.
To reduce barriers to attendance, a US$35 incentive was provided to defray parking costs. We provided a rain jacket and technical shirt as well as well as an activity monitor (Garmin vivosmart V.4) at the participant’s first hike.
Outcomes
The primary outcomes of interest were feasibility and acceptability. Feasibility was assessed based on recruitment statistics (the proportion of individuals who were contacted, eligible and enrolled, as well as reasons for ineligibility), retention (questionnaire completion), hike attendance and safety (eg, adverse events). We aimed to recruit 36–45 participants (12–15 people allocated to each of the three groups—nature hiking, urban hiking and a no-hiking control group) and complete enrolment by July 2019 (approximately 3 months after recruitment began) due to concerns about weather for hikes later in the fall. Because of lower-than-anticipated recruitment numbers, in late June, we decided to eliminate the no-hiking control group. At this time, only one person was randomised to the no-hiking control group and informed of their group assignment; that person was re-randomised after this decision was made. The target for retention and attendance was 70%, a commonly cited standard for trials.71 72
To assess acceptability, in the 6-week and 12 week questionnaires, we included questions created for the study about the difficulty of the hikes’ distance, pace and the terrain (rated on a 5-point scale from extremely difficult to effortless), and satisfaction with the locations of hikes (rated on a 5-point scale from extremely unsatisfied to very satisfied). Lastly, prehike and trailhead information and communication were assessed on a 5-point scale (eg, from very poor to excellent). We also included open-ended questions for participants to report what they thought went well and what could have been better. Additionally, after the final hike, the lead author (AJL) conducted semistructured telephone interviews, with a goal to interview 10–15 participants. To include a range of perspectives, we purposively sampled participants from both arms, aimed to include men and women, and participants who varied in terms of hike attendance. Questions inquired about participants’ impressions of the hikes, including difficulty, location, length of time, distance from home, hike leaders and reasons hikes were missed (if applicable); study communications; enrolment process; assessments and other thoughts/impressions.
Determination of efficacy was not a goal of this pilot RCT. The primary outcome of the future planned study is PTSD symptoms, assessed by the PTSD-Checklist for Diagnostic and Statistical Manual 5 (PCL-5), a 20-item instrument that assesses PTSD symptoms in the past month (range 0–80, with higher scores indicating greater symptom severity). Other outcome measures of interest for the future planned study, which are detailed in online supplemental table 1, include quality of life,73 positive and negative affect,74 75 sleep,76 rumination77 and cognitive reappraisal.78
bmjopen-2021-051885supp001.pdf (60.6KB, pdf)
Baseline and follow-up assessments
We conducted assessments online using commercial software (QuestionPro) at baseline (before hikes began), and then weekly for 12 weeks, starting with the week of the first hike and ending the week after the sixth hike, and finally at week 24; questionnaires completed immediately after the hikes were completed on paper. See figure 2 for an overview and online supplemental table 1 for measures at each time point. Questionnaires at weeks 6, 12 and 24 took approximately 30 min to complete. Questionnaires administered at weeks 1–5 and 7–11 included fewer measures and/or shortened versions and took 5–10 min to complete. Participants received gift cards worth US$10 for completing questionnaires in weeks 1–5 and 7–11, US$20 for the 6-week questionnaire, and US$50 for the 12-week and 24-week questionnaires. In addition to questionnaires, to obtain objective information about PA (a potential mechanism of benefit, which we would want to measure precisely in a future study), we asked participants to wear a wrist worn-activity monitor (Garmin vivosmart V.4) every day, for at least 10 hours per day, for the first 12 weeks of the study. No incentives were provided for wearing or synching the monitor.
Data analysis
Quantitative analysis
The primary purpose of the extensive data collection was to evaluate feasibility of data collection rather than to estimate effect sizes because estimating effect sizes from small pilot studies is inherently imprecise.79 Thus, instead of conducting hypothesis tests for effectiveness outcomes for which we were underpowered, we present descriptive statistics (eg, medians and IQRs) for the primary outcome (PCL-5) only. For acceptability measures related to communication, we categorised responses as positive if respondents chose one of the two most favourable response options (eg, satisfied/very satisfied; good/excellent) and not positive if they chose one of the other response options (extremely unsatisfied/unsatisfied/ neither satisfied or unsatisfied; inadequate/very poor/adequate). We then calculated the proportion of urban and nature participants with favourable responses for each question. In addition to proportions, we also calculated the mean scores for hike locations, distance, pace, prehike information, prehike communication and trailhead communication by group.
Qualitative analysis
All interviews were recorded, and the interviewer took notes during interviews. For both the comments shared via open-ended questions on the questionnaire and comments shared orally during the interviews, we conducted inductive content analysis, which involves open coding of data, organising codes and data into categories and comparing data across participants to identify patterns and themes in the data.80
Patient and public involvement
Patients were involved in the design and conduct of this study. The study question and design were informed by a Veteran with PTSD who served as a co-investigator. The design and messaging for this pilot study were also informed by a focus group of patients/Veterans who participated in a prior unpublished feasibility study.
Results
Feasibility
Recruitment statistics
Recruitment took place between April and August 2019 (16 weeks total). Of the 1001 patients mailed an invitation letter, we were unable to assess interest or eligibility in 586 (because they did not respond to the mailings and/or answer the phone when called; see figure 3 for Consolidated Standards of Reporting Trials diagram). Of the 436 with whom we made contact (including 21 who contacted the study), 159 were not interested, 102 had health conditions that limited their walking/hiking, 37 had time conflicts (eg, work or church on Sundays or travel that would prevent participation), and 41 had other reasons that they were unable to participate (eg, moving out of the area, did not have PTSD). Of the 97 (81 from letters+16 from passive recruitment) interested who passed initial screening, 48 completed the online screening questionnaire. Twenty individuals were not eligible, 2 decided that they no longer wanted to participate and 26 were eligible and randomised. Of the 20 who were not eligible, 13 were ineligible because of a moderate/high risk of suicide or skipping the question on suicidality, and 6 did not meet the threshold for PTSD. Compared with those contacted and not randomised, a greater proportion of those randomised were women (27% randomised vs 15% of those contacted), white (73% vs 63%) and Hispanic (8% vs 6%). Additionally, those who were randomised were younger (mean age=47, range 25–65) than those not randomised (mean age=52, range: 21–95).
Figure 3.
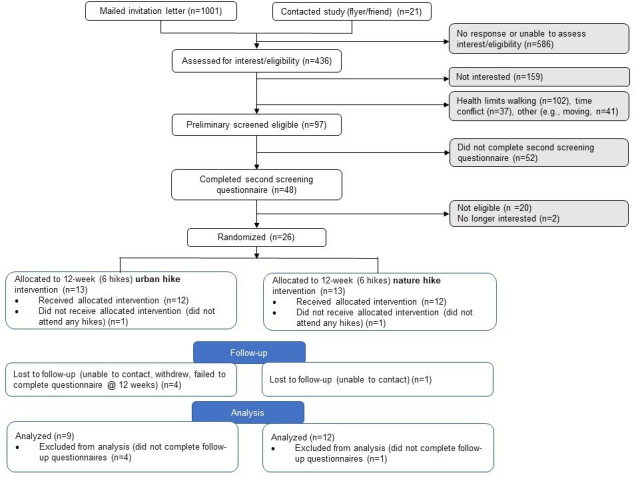
CONSORT diagram. CONSORT, Consolidated Standards of Reporting Trials.
Table 1 presents characteristics of Veterans who were randomised and includes self-reported race/ethnicity, which differed from race/ethnicity in the electronic medical record (reported above). Specifically, 42% of those randomised self-reported being white, whereas the electronic medical record data indicated that 73% were white. Thirty per cent had a college degree or more. Less than half worked full time and 46% had 100% VA service-connected disability, indicating severe impairment in ability to work. Nearly two-thirds of participants had served in combat and 68% had depressive symptoms based on the Patient Health Questionnaire (PHQ)-8. Based on self-report, nearly 70% met or exceeded PA guidelines of at least 75 min per week of vigorous-intensity activity or 150 min per week of moderate-intensity activity or an equivalent combination of the two. At baseline (prior to study initiation), 81% of participants reported hiking at least one time and 27% completed seven or more hikes in the prior year.
Table 1.
Baseline characteristics of Veterans in the urban and nature hiking groups
| Characteristic | Total (n=26) | Nature (n=13) | Urban (n=13) | |||
| N or mean | % or SD | N or mean | % or SD | N or mean | % or SD | |
| Age (years) | ||||||
| <30 | 2 | 8 | 1 | 8 | 1 | 8 |
| 30–39 | 5 | 19 | 2 | 15 | 3 | 23 |
| 40–49 | 6 | 23 | 4 | 31 | 2 | 15 |
| 50–59 | 11 | 42 | 6 | 46 | 5 | 38 |
| >60 | 2 | 8 | 0 | 0 | 2 | 15 |
| Gender | ||||||
| Male | 19 | 73 | 8 | 62 | 11 | 85 |
| Female | 7 | 27 | 5 | 38 | 2 | 15 |
| Race/ethnicity | ||||||
| Asian/Pacific Islander, NH | 3 | 12 | 2 | 15 | 1 | 8 |
| Black, NH | 2 | 8 | 0 | 0 | 2 | 15 |
| Hispanic | 3 | 12 | 1 | 8 | 2 | 15 |
| Native American, NH | 2 | 8 | 0 | 0 | 2 | 15 |
| Other | 1 | 4 | 0 | 0 | 1 | 7.7 |
| White, NH | 15 | 58 | 10 | 77 | 5 | 38 |
| Marital status | ||||||
| Single, never married | 4 | 15 | 3 | 23 | 1 | 8 |
| Married currently | 14 | 54 | 7 | 54 | 7 | 54 |
| Separated/divorced | 8 | 31 | 3 | 23 | 5 | 38 |
| Education | ||||||
| High school degree or equivalent | 4 | 15 | 1 | 8 | 3 | 23 |
| Some college, no degree | 10 | 38 | 7 | 54 | 3 | 23 |
| Associate degree | 4 | 15 | 1 | 8 | 3 | 23 |
| Bachelor’s degree | 4 | 15 | 2 | 15 | 2 | 15 |
| Masters, doctorate or professional degree | 4 | 15 | 2 | 15 | 2 | 15 |
| Annual household income | ||||||
| US$25 000–US$49 999 | 7 | 27 | 4 | 31 | 3 | 23 |
| US$50 000–US$74 999 | 11 | 42 | 4 | 31 | 7 | 54 |
| US$75 000–US$99 999 | 2 | 8 | 1 | 8 | 1 | 8 |
| US$100 000 or more | 4 | 15 | 3 | 23 | 1 | 8 |
| Prefer not to answer | 2 | 8 | 1 | 8 | 1 | 8 |
| Employment status | ||||||
| Full time | 12 | 46 | 6 | 46 | 6 | 46 |
| Part time | 1 | 4 | 1 | 8 | 0 | 0 |
| Not employed (disabled, retired, not looking for work, homemaker, other) | 13 | 50 | 6 | 46 | 7 | 54 |
| Highest military rank | ||||||
| Enlisted (E1–E4) | 9 | 35 | 4 | 31 | 5 | 38 |
| Non-commissioned officer (E5–E9) | 15 | 58 | 8 | 62 | 7 | 54 |
| Officer (O1–O4) | 2 | 8 | 1 | 8 | 1 | 8 |
| VA disability rating*†* | ||||||
| No rating | 2 | 8 | 0 | 0 | 2 | 15 |
| 30%–60% | 2 | 8 | 2 | 15 | 0 | 0 |
| 70%–90% | 8 | 31 | 4 | 31 | 4 | 31 |
| 100% | 12 | 46 | 6 | 46 | 6 | 46 |
| Self-reported health | ||||||
| Excellent/very good | 9 | 35 | 3 | 23 | 6 | 45 |
| Good | 11 | 42 | 7 | 54 | 4 | 31 |
| Fair (no one reported poor) | 6 | 23 | 3 | 23 | 3 | 23 |
| PCL-5 score‡ | ||||||
| Mean, SD | 47.1 | 10.9 | 46.0 | 11.4 | 48.2 | 10.8 |
| Served in combat (yes) | 17 | 65 | 8 | 62 | 9 | 69 |
| Combat Exposure Score; mean (SD)*†* | 16.6 | 7.9 | 15.6 | 8.2 | 17.7 | 7.9 |
| Patient Health Questionnaire-8 score** | ||||||
| <10 (no depression) | 8 | 32 | 4 | 33 | 4 | 31 |
| 10–19 (major depression) | 14 | 56 | 7 | 58 | 7 | 54 |
| >20 (severe major depression) | 3 | 12 | 1 | 8 | 2 | 15 |
| Physical activity level | ||||||
| Low | 8 | 31 | 5 | 38 | 3 | 23 |
| Moderate | 3 | 12 | 1 | 8 | 2 | 15 |
| High | 15 | 58 | 7 | 54 | 8 | 62 |
| Times gone hiking for 1+ hours in last year | ||||||
| Never | 5 | 19 | 3 | 23 | 2 | 15 |
| 1–3 | 9 | 35 | 4 | 31 | 5 | 38 |
| 4–6 | 5 | 19 | 2 | 15 | 3 | 23 |
| 7+ | 7 | 27 | 4 | 31 | 3 | 23 |
| Outdoor/nature-based activity experience | ||||||
| None (no experience in the outdoors) | 0 | 0 | 0 | 0 | 0 | 0 |
| Casual (done some day hiking on maintained trails and car camping) | 10 | 38 | 5 | 38 | 5 | 38 |
| Amateur (have experience with backpacking) | 11 | 42 | 6 | 46 | 5 | 38 |
| Expert (substantial backcountry experience) | 5 | 19 | 2 | 15 | 3 | 23 |
*Missing response for one nature participant.
†Missing response for one urban participant.
‡One person in the nature hiking group had a PCL-5 of 32 (below the eligibility threshold of 33) due to an undetected error in initial scoring.
NH, non-Hispanic; PCL-5, Post-Traumatic Stress Disorder Checklist for Diagnostic and Statistical Manual 5.;
Retention (questionnaire completion)
Mean completion of all questionnaires was 91% in the nature hiking group and 68% in the urban hiking group. Completion rates were similar for the shorter weekly questionnaires and the longer questionnaires.
Hike attendance
Over the course of the intervention, participants in the nature and urban groups attended an average of 56% and 58%, respectively, of scheduled hikes. In the nature group, one person attended no hikes, four (31%) attended 1–2 hikes, one attended 3 hikes and seven (54%) attended 4–6 hikes. In the urban group, one person attended no hikes, four (31%) attended 1–2 hikes, no one attended only 3 hikes and eight (62%) attended 4–6 hikes. Attendance was lower among women in the nature group (n=5, mean: 43%) than among women in the urban group (n=2, 67%), whereas among men, hike attendance was similar in the two groups (65% vs 56%). Common reasons for missing hikes included work, childcare and prior plans.
Safety/adverse events
One participant in the urban hiking group reported increased anxiety/PTSD symptoms in connection with hiking in the urban environment and withdrew from the study.
Acceptability
Quantitative findings
Acceptability of both the urban and nature hikes was high. Over 70% reported a positive rating for the hike locations, distance and pace; ratings were similar in the urban and nature hiking groups. Additionally, on average, prehike information, prehike communication and trailhead communication were rated as good to excellent. Scores related to communication were similar in the urban and nature hike groups at 6 weeks, but were lower in the urban hiking arm at 12 weeks (prehike information, mean scores: nature=4.4, urban=3.6; prehike communication: nature=4.6, urban=3.8; trailhead communication: nature=4.6, urban=4.1)
Qualitative findings
In response to the open-ended question on the questionnaire (‘What went well so far?’), participants shared positive comments such as ‘This group seems to mesh really well’, ‘all expectations were exceeded’ and ‘good planning, leadership and execution.’ In response to the question, ‘What do you think we can do better?’, suggestions included having regional groups, closer hikes or paying for gas; weekly (instead of every other week) hikes; more team building and opportunities to socialise with others; and including more women and/or women-only groups. Key themes from the qualitative interviewers, which are presented in table 2, echoed and elaborated on themes shared in the questionnaire. Most participants felt positively about their experience in the study. As noted above, they liked getting to know other Veterans and having a ‘mission’. Veterans wanted to find more ways of connecting with one another socially during hikes as well as outside of hikes. Hike logistics (eg, distance from home) were noted as potential barriers to attendance.
Table 2.
Key themes and findings from qualitative data
| Themes | Findings |
| A positive experience |
|
| Perceived benefits |
|
| Hike logistics |
|
| Difficulty of hikes |
|
| Location of hikes |
|
| Group composition |
|
| Incentives for completing questionnaires |
|
| Assessments |
|
| Activity monitors |
|
| Fostering interaction/connections between participants in a group |
|
Efficacy measures
Median PCL-5 scores decreased from baseline to week 12 and remained at the 12-week level at week 24 for those in the nature hiking group (baseline=41, 12-weeks=32, 24 weeks=31). Among those in the urban hiking group, PCL-5 scores decreased from baseline to 12 weeks but increased nearly back to baseline levels at 24 weeks (baseline=48, 12-weeks=43, 24 weeks=47) (online supplemental figure 1). We did not test the statistical significance of the changes because this pilot study was not designed to answer this question.81
bmjopen-2021-051885supp002.pdf (47.7KB, pdf)
Discussion
This study was an important step in establishing feasibility and acceptability and identifying changes to consider in the development of a rigorous, fully powered study to evaluate the impact of nature hiking on PTSD symptoms. The results of this pilot study generally supported feasibility and acceptability. Participants reported high acceptability, enjoyment and value, based on quantitative and qualitive data. In both arms, more than half of participants completed most hikes. Qualitative feedback about improving the social component supports the hypothesis that social connection is an important aspect of hikes, indicating a need to further develop the social component and continue to study group interventions like this one. Additionally, the decrease in median scores on the PCL-5 among those in the nature group after the 12-week hiking intervention, and 12 weeks later (week 24) is promising. This preliminary finding should be investigated more thoroughly in future, larger-scale versions of our study. The indication that improvements may persist after the conclusion of the intervention is especially compelling given the current unknowns regarding the duration of effects of nature interventions.
Nevertheless, several issues need to be considered related to feasibility and acceptability for the next iteration of this research.
Feasibility of recruitment
We fell short of our goal of recruiting at least 36 people over 4 months. Failing to meet recruitment goals in the planned timeframe is a common problem in RCTs.82 Barriers to recruitment included unexpected delays, insufficient resources and an inefficient recruitment process. Regarding delays, we had to wait weeks for institutional review board approval for each proposed modification to recruitment materials/protocol. Regarding resources, we only had 20 hours per week of paid staff time for recruitment. The addition of two volunteers in the final 2 months helped to accelerate enrolment, but more resources earlier in recruitment would have been necessary to meet our goal.
One contributor to inefficiency in recruitment was the broad, population-based approach we employed for active recruitment. To identify patients for the introductory mailing, the only inclusion criteria were having a single encounter in VA’s electronic medical record with a PTSD diagnosis and living in one of three Puget Sound counties. The only exclusion criteria were a diagnosis of schizophrenia, bipolar disorder or other psychotic disorder. Likely in part because of this broad approach, which did not include upper age limits, approximately one-quarter of contacted individuals reported a health condition that impaired their walking. Burdensome study procedures may have also impacted recruitment. About half of interested participants failed to complete the online screening questionnaire and others informed us that they had trouble completing the online questionnaire. Imposing an upper age limit (eg, 65 years) and restructuring the recruitment process to make it faster and easier for potential participants may be necessary.
Accessibility of the intervention and restrictive eligibility criteria may have also impacted recruitment. In addition to being able to walk over uneven ground for at least 2 hours, participants also had to be available during the times selected, have low suicide risk and be free from physical conditions such as high blood pressure (or obtain their primary care provider’s permission) among several other criteria. Changing inclusion criteria (eg, eliminating restrictions related to suicidality) might improve recruitment and generalisability, but would require trade-offs related to safety and retention that must be considered carefully.
Lastly, about 38% (159/415) of those for whom we were able to assess eligibility and interest declined participation. While some of these people may have declined because of the additional burdens of a research study, this statistic indicates that hiking may only appeal to a segment of the population, just as psychotherapy and pharmacotherapy only appeal to subsets of the population.83 Because of differences in treatment preferences, offering options is important and nature hiking merits consideration so that we can rigorously assess its efficacy.
Retention
Retention varied by group and was poorer for the wrist-worn activity monitor than for the questionnaires. The activity monitor had a substantial amount of missing data, which is a common problem for activity monitors,84 and may have been related to the number of technical steps required for setting up the monitor and syncing it, as many participants needed additional help to troubleshoot problems. Providing more support to set up the monitor and incentives to wear and sync it may help to obtain more complete data. While overall questionnaire completion was high, it was higher in the nature hiking group (91%) than in the urban hiking group (68%). Though the small sample and our inability to conduct interviews with those who did not complete follow-up measures makes inference difficult, the retention differences could be a marker of commitment to the study. Future studies should pay careful attention to marketing the study to ensure that both interventions are perceived as helpful. Enhancing the social aspects of the interventions may help achieve that goal. The difference in incentives provided for questionnaire completion vs the other aspects of the study may also have played a role in retention for different study aspects. However, many participants shared that they participated to help fellow Veterans, indicating altruistic/intrinsic motivators for participation, reinforcing the importance of understanding drivers of participation, and reducing barriers and enhancing facilitators.
Acceptability of the hiking interventions
Hike attendance (56%) was lower than our target (70%) and women had lower attendance in the nature hiking group than men. While we were unable to ascertain reasons for missing hikes for each person, some reasons reported (eg, other plans, work) were hard to avoid, while others (driving distance to hikes) could be addressed in the future by restricting the geographical area of recruitment and hikes and/or organising small groups at different times to accommodate individuals’ schedules. Our study, unfortunately, does not shed light on the optimal hike ‘dose’. We suspect that 8–12 hikes (similar to a standard psychotherapy course) may be optimal for achieving clinically meaningful results. Additional research will be necessary to examine this important question. There were also an indication of lower acceptability/ratings for information sharing in the urban hiking versus the nature hiking groups. For nature hikes, we listed a trail. For urban hikes, we shared information about the urban area, but did not provide an exact hiking route, which may have made it more difficult for participants to research urban hikes. Providing a map of the route might help participants feel prepared. Regarding differences in attendance by gender, a history of military sexual trauma, which is common among women Veterans,85 may have impacted some women participants’ comfort and perception of safety of hiking in nature with a majority male group. Ensuring a greater proportion of women in each group or organising women-only groups (as was suggested by some participants) could address this concern. These changes, would, however, result in additional costs and trade-offs that would need to be carefully considered.
Conclusions
This pilot study provided useful information related to feasibility and acceptability, including common factors that resulted in exclusion; resources and procedures needed for recruitment; factors to consider for selection of nature and urban hikes; and barriers and facilitators to achieving high completion in follow-up assessments and the hikes. These insights can be harnessed to increase participation and rigour in future, scaled-up iterations of the study and ensure that environments are safe (ie, non-triggering). Future studies with larger sample sizes are needed to isolate the ways nature contact, PA and social support conferred by the group impact outcomes to develop and provide well-tailored interventions.
Supplementary Material
Acknowledgments
We thank the Veterans who participated in this study for allowing us to learn from them, including the Veterans who participated in a prior unpublished feasibility study. We also thank Morgan Meadows and Gabrielle Fong for their help with recruitment. This material is the result of work supported by VA Puget Sound Healthcare System, Seattle, WA.
Footnotes
Contributors: AJL, GNB, CCE, JCF, KL, JB, and HF conceptualised the study and contributed to the intervention development and design. AJL and GNB oversaw the conduct of the trial all the authors contributed to the ongoing management of the trial. AJL, GNB, MM, AP, and CK oversaw data collection and data analysis. The manuscript was drafted by AJL. All the authors contributed to the interpretation of the findings and revised and reviewed the paper.
Funding: This work was funded by Recreational Equipment, Inc. (REI; Award/Grant number is not applicable) and supported by equipment and outfitting contributions from Outdoor Research.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the US Government, Recreational Equipment (REI), or Outdoor Research.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data are available upon reasonable request. Due to legal and ethical restrictions, we are unable to share data publicly because the data contain potentially identifying and/or sensitive patient information. Subject to IRB approval, de-identified data will be released to a local Department of Veterans Affairs (VA) Puget Sound Health Care System and/or national VA research data repository for release to non-VA protocols. The VA research data repository administrator will be responsible for reviewing and responding to requests to release data to non-VA requestors. A data use agreement compliant with Veterans Health Administration Handbooks 1200.12 and 1605.1 will be required between Veterans Health Administration and the requestor. Review and approval by VA privacy officer is required prior to disclosure. Data access requests will be reviewed by the IRB of the VA Puget Sound Health Care System (contact via Dr. Littman – alyson.littman@va.gov), via mail address: 1660 S Columbian Way, Building 101 – 5W41, Seattle, WA 98108.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the institutional review boards at the VA Puget Sound Healthcare System (MIRB 01738) and the University of Washington (6951).
References
- 1.Gates MA, Holowka DW, Vasterling JJ, et al. Posttraumatic stress disorder in veterans and military personnel: epidemiology, screening, and case recognition. Psychol Serv 2012;9:361–82. 10.1037/a0027649 [DOI] [PubMed] [Google Scholar]
- 2.Fulton JJ, Calhoun PS, Wagner HR, et al. The prevalence of posttraumatic stress disorder in operation enduring Freedom/Operation Iraqi freedom (OEF/OIF) veterans: a meta-analysis. J Anxiety Disord 2015;31:98–107. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- 3.Schlenger WE, Kulka RA, Fairbank JA, et al. The prevalence of post-traumatic stress disorder in the Vietnam generation: a multimethod, multisource assessment of psychiatric disorder. J Trauma Stress 1992;5:333–63. 10.1002/jts.2490050303 [DOI] [Google Scholar]
- 4.Hall KS, Hoerster KD, Yancy WS. Physical activity, and eating behaviors. Epidemiol Rev 2015;37:103–15. [DOI] [PubMed] [Google Scholar]
- 5.Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol 2017;32:541–56. 10.1097/HCO.0000000000000437 [DOI] [PubMed] [Google Scholar]
- 6.Veterans Health Administration . Analysis of Va health care utilization among operation enduring freedom (OEF), operation Iraqi freedom (OIF), and operation new dawn (OND) veterans, 2013: 1–13. http://www.publichealth.va.gov/epidemiology/reports/oefoifond/health-care-utilization/index.asp [Google Scholar]
- 7.Kang HK, Li B, Mahan CM, et al. Health of US veterans of 1991 Gulf war: a follow-up survey in 10 years. J Occup Environ Med 2009;51:401–10. 10.1097/JOM.0b013e3181a2feeb [DOI] [PubMed] [Google Scholar]
- 8.Magruder KM, McLaughlin KA, Elmore Borbon DL. Trauma is a public health issue. Eur J Psychotraumatol 2017;8:1375338. 10.1080/20008198.2017.1375338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta MA. Review of somatic symptoms in post-traumatic stress disorder. Int Rev Psychiatry 2013;25:86–99. 10.3109/09540261.2012.736367 [DOI] [PubMed] [Google Scholar]
- 10.Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J Affect Disord 2010;123:249–57. 10.1016/j.jad.2009.08.006 [DOI] [PubMed] [Google Scholar]
- 11.Frayne SM, Seaver MR, Loveland S, et al. Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med 2004;164:1306. 10.1001/archinte.164.12.1306 [DOI] [PubMed] [Google Scholar]
- 12.Dedert EA, Calhoun PS, Watkins LL, et al. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Ann Behav Med 2010;39:61–78. 10.1007/s12160-010-9165-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Management of Posttraumatic Stress Disorder Work Group . VA/DoD clinical practice guidelines for the management of posttraumatic stress disorder and acute stress disorder, 2017: 1–200. [Google Scholar]
- 14.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13–22. 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- 15.Sharp M-L, Fear NT, Rona RJ, et al. Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiol Rev 2015;37:144–62. 10.1093/epirev/mxu012 [DOI] [PubMed] [Google Scholar]
- 16.Wang PS, Berglund P, Olfson M, et al. Failure and delay in initial treatment contact after first onset of mental disorders in the National comorbidity survey replication. Arch Gen Psychiatry 2005;62:603–13. 10.1001/archpsyc.62.6.603 [DOI] [PubMed] [Google Scholar]
- 17.Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv 2013;64:280–3. 10.1176/appi.ps.001372012 [DOI] [PubMed] [Google Scholar]
- 18.Hoge CW, Grossman SH, Auchterlonie JL, et al. Ptsd treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. PS 2014;65:997–1004. 10.1176/appi.ps.201300307 [DOI] [PubMed] [Google Scholar]
- 19.Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of Veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv 2018;15:536–42. 10.1037/ser0000212 [DOI] [PubMed] [Google Scholar]
- 20.Goetter EM, Bui E, Ojserkis RA, et al. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J Trauma Stress 2015;28:401–9. 10.1002/jts.22038 [DOI] [PubMed] [Google Scholar]
- 21.Foa EB, McLean CP, Zang Y, et al. Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs Present-Centered therapy on PTSD symptom severity in military personnel: a randomized clinical trial. JAMA 2018;319:354–64. 10.1001/jama.2017.21242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rauch SAM, Kim HM, Powell C, et al. Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry 2019;76:117–26. 10.1001/jamapsychiatry.2018.3412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kehle-Forbes SM, Meis LA, Spoont MR, et al. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a Va outpatient clinic. Psychol Trauma 2016;8:107–14. 10.1037/tra0000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keefe JR, Wiltsey Stirman S, Cohen ZD, et al. In rape trauma PTSD, patient characteristics indicate which trauma-focused treatment they are most likely to complete. Depress Anxiety 2018;35:330–8. 10.1002/da.22731 [DOI] [PubMed] [Google Scholar]
- 25.Frumkin H, Bratman GN, Breslow SJ, et al. Nature contact and human health: a research agenda. Environ Health Perspect 2017;125:075001. 10.1289/EHP1663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bratman GN, Olvera‐Alvarez HA, Gross JJ. The affective benefits of nature exposure. Soc Personal Psychol Compass 2021;15:e12630. 10.1111/spc3.12630 [DOI] [Google Scholar]
- 27.Kaplan S. The restorative benefits of nature: toward an integrative framework. J Environ Psychol 1995;15:169–82. 10.1016/0272-4944(95)90001-2 [DOI] [Google Scholar]
- 28.Ulrich RS, Simons RF, Losito BD, et al. Stress recovery during exposure to natural and urban environments. J Environ Psychol 1991;11:201–30. 10.1016/S0272-4944(05)80184-7 [DOI] [Google Scholar]
- 29.van den Berg MMHE, Maas J, Muller R, et al. Autonomic nervous system responses to viewing green and built settings: differentiating between sympathetic and parasympathetic activity. Int J Environ Res Public Health 2015;12:15860–74. 10.3390/ijerph121215026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kobayashi H, Song C, Ikei H, et al. Analysis of individual variations in autonomic responses to urban and forest environments. Evid Based Complement Alternat Med 2015;2015:1–7. 10.1155/2015/671094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whitworth JW, Ciccolo JT. Exercise and post-traumatic stress disorder in military veterans: a systematic review. Mil Med 2016;181:953–60. 10.7205/MILMED-D-15-00488 [DOI] [PubMed] [Google Scholar]
- 32.Kim SH, Schneider SM, Bevans M, et al. Ptsd symptom reduction with mindfulness-based stretching and deep breathing exercise: randomized controlled clinical trial of efficacy. J Clin Endocrinol Metab 2013;98:2984–92. 10.1210/jc.2012-3742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitchell KS, Dick AM, DiMartino DM, et al. A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. J Trauma Stress 2014;27:121–8. 10.1002/jts.21903 [DOI] [PubMed] [Google Scholar]
- 34.van der Kolk BA, Stone L, West J, et al. Yoga as an adjunctive treatment for posttraumatic stress disorder: a randomized controlled trial. J Clin Psychiatry 2014;75:e559–65. 10.4088/JCP.13m08561 [DOI] [PubMed] [Google Scholar]
- 35.Powers MB, Medina JL, Burns S, et al. Exercise augmentation of exposure therapy for PTSD: rationale and pilot efficacy data. Cogn Behav Ther 2015;44:314–27. 10.1080/16506073.2015.1012740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand 2015;131:350–9. 10.1111/acps.12371 [DOI] [PubMed] [Google Scholar]
- 37.Goldstein LA, Mehling WE, Metzler TJ, et al. Veterans group exercise: a randomized pilot trial of an integrative exercise program for veterans with posttraumatic stress. J Affect Disord 2018;227:345–52. 10.1016/j.jad.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 38.Whitworth JW, Nosrat S, SantaBarbara NJ, et al. Feasibility of resistance exercise for posttraumatic stress and anxiety symptoms: a randomized controlled pilot study. J Trauma Stress 2019;32:977–84. 10.1002/jts.22464 [DOI] [PubMed] [Google Scholar]
- 39.Hall KS, Morey MC, Beckham JC, et al. Warrior wellness: a randomized controlled pilot trial of the effects of exercise on physical function and clinical health risk factors in older military veterans with PTSD. J Gerontol A Biol Sci Med Sci 2020;75:2130–8. 10.1093/gerona/glz255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lehavot K, Katon JG, Chen JA, et al. Post-Traumatic stress disorder by gender and veteran status. Am J Prev Med 2018;54:e1–9. 10.1016/j.amepre.2017.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hundt NE, Robinson A, Arney J, et al. Veterans' perspectives on benefits and drawbacks of peer support for posttraumatic stress disorder. Mil Med 2015;180:851–6. 10.7205/MILMED-D-14-00536 [DOI] [PubMed] [Google Scholar]
- 42.Pretty J, Peacock J, Sellens M, et al. The mental and physical health outcomes of green exercise. Int J Environ Health Res 2005;15:319–37. 10.1080/09603120500155963 [DOI] [PubMed] [Google Scholar]
- 43.Thompson Coon J, Boddy K, Stein K, et al. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol 2011;45:1761–72. 10.1021/es102947t [DOI] [PubMed] [Google Scholar]
- 44.Lahart I, Darcy P, Gidlow C, et al. The effects of green exercise on physical and mental wellbeing: a systematic review. Int J Environ Res Public Health 2019;16:1352. 10.3390/ijerph16081352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Annerstedt M, Währborg P. Nature-assisted therapy: systematic review of controlled and observational studies. Scand J Public Health 2011;39:371–88. 10.1177/1403494810396400 [DOI] [PubMed] [Google Scholar]
- 46.Barton J, Pretty J. What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environ Sci Technol 2010;44:3947–55. 10.1021/es903183r [DOI] [PubMed] [Google Scholar]
- 47.Wolsko C, Lindberg K, Reese R. Nature-Based physical Recreation leads to psychological well-being: evidence from five studies. Ecopsychology 2019;11:222–35. 10.1089/eco.2018.0076 [DOI] [Google Scholar]
- 48.Marselle M, Irvine K, Warber S. Walking for well-being: are group walks in certain types of natural environments better for well-being than group walks in urban environments? Int J Environ Res Public Health 2013;10:5603–28. 10.3390/ijerph10115603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kyriakopoulos A. How individuals with self-reported anxiety and depression experienced a combination of individual counselling with an adventurous outdoor experience: a qualitative evaluation. Couns Psychother Res 2011;11:120–8. 10.1080/14733145.2010.485696 [DOI] [Google Scholar]
- 50.Bennett JL, Lundberg NR, Zabriskie R. Addressing posttraumatic stress among Iraq and Afghanistan veterans and significant others: an intervention utilizing sport and recreation. Ther Recreation J 2014;48:74–93. [Google Scholar]
- 51.Bennett JL, Piatt JA, Van Puymbroeck M. Outcomes of a therapeutic Fly-Fishing program for veterans with combat-related disabilities: a community-based rehabilitation initiative. Community Ment Health J 2017;53:756–65. 10.1007/s10597-017-0124-9 [DOI] [PubMed] [Google Scholar]
- 52.Dustin DL, Dustin D, Bricker N. The promise of river running as a therapeutic medium for veterans coping with post-traumatic stress disorder. Ther Recreation J 2011:326–40. [Google Scholar]
- 53.Duvall J, Kaplan R. Enhancing the well-being of Veterans using extended group-based nature recreation experiences. J Rehabil Res Dev 2014;51:685–96. 10.1682/JRRD.2013.08.0190 [DOI] [PubMed] [Google Scholar]
- 54.Gelkopf M, Hasson-Ohayon I, Bikman M, et al. Nature adventure rehabilitation for combat-related posttraumatic chronic stress disorder: a randomized control trial. Psychiatry Res 2013;209:485–93. 10.1016/j.psychres.2013.01.026 [DOI] [PubMed] [Google Scholar]
- 55.Hyer L, Boyd S, Scurfield R, et al. Effects of outward bound experience as an adjunct to inpatient PTSD treatment of war veterans. J Clin Psychol 1996;52:263–78. [DOI] [PubMed] [Google Scholar]
- 56.Anderson CL, Monroy M, Keltner D. Awe in nature heals: evidence from military veterans, at-risk youth, and college students. Emotion 2018;18:1195–202. 10.1037/emo0000442 [DOI] [PubMed] [Google Scholar]
- 57.Poulsen DV, Stigsdotter UK, Refshage AD. Whatever happened to the soldiers? Nature-assisted therapies for veterans diagnosed with post-traumatic stress disorder: a literature review. Urban For Urban Green 2015;14:438–45. 10.1016/j.ufug.2015.03.009 [DOI] [Google Scholar]
- 58.Greenleaf AT, Roessger KM. Effectiveness of Care Farming on Veterans’ Life Satisfaction, Optimism, and Perceived Loneliness. J Humanist Couns 2017;56:86–110. 10.1002/johc.12046 [DOI] [Google Scholar]
- 59.Jennings V, Bamkole O. The relationship between social cohesion and urban green space: an avenue for health promotion. Int J Environ Res Public Health 2019;16:452. 10.3390/ijerph16030452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Johansson M, Hartig T, Staats H. Psychological benefits of walking: moderation by company and outdoor environment. Appl Psychol 2011;3:261–80. 10.1111/j.1758-0854.2011.01051.x [DOI] [Google Scholar]
- 61.Junger S. Tribe: on homecoming and belonging. New York, NY: Hatchette, 2016. [Google Scholar]
- 62.Price M, Lancaster CL, Gros DF, et al. An examination of social support and PTSD treatment response during prolonged exposure. Psychiatry 2018;81:258–70. 10.1080/00332747.2017.1402569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zang Y, Gallagher T, McLean CP, et al. The impact of social support, unit cohesion, and trait resilience on PTSD in treatment-seeking military personnel with PTSD: the role of posttraumatic cognitions. J Psychiatr Res 2017;86:18–25. 10.1016/j.jpsychires.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 64.Cohen S, Wills TA, Stress WTA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985;98:310–57. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- 65.Thomas S, Reading J, Shephard RJ. Revision of the physical activity readiness questionnaire (PAR-Q). Can J Sport Sci 1992;17:338–45. [PubMed] [Google Scholar]
- 66.Weathers FW, Litz BT, Keane TM. The PTSD checklist for DSM-5 (PCL-5). Natl Cent PTSD 2002;2013. [Google Scholar]
- 67.Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the drug abuse screening test. J Subst Abuse Treat 2007;32:189–98. 10.1016/j.jsat.2006.08.002 [DOI] [PubMed] [Google Scholar]
- 68.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (audit): who Collaborative project on early detection of persons with harmful alcohol Consumption-II. Addiction 1993;88:791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- 69.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22–33. [PubMed] [Google Scholar]
- 70.US Department of Veterans Affairs . Veterans Health Administration VA Adaptive Sports & Therapeutic Arts: Grant Program. Available: https://www.blogs.va.gov/nvspse/ [Accessed 28 Jun 2021].
- 71.Ribisl KM, Walton MA, Mowbray CT, et al. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: review and recommendations. Eval Program Plann 1996;19:1–25. 10.1016/0149-7189(95)00037-2 [DOI] [Google Scholar]
- 72.Solomon P, Cavanaugh MM, Draine J. Randomized controlled trials: design and implementation for community-based psychosocial interventions, 2009: 1–224. [Google Scholar]
- 73.Diener E, Emmons RA, Larsen RJ, et al. The satisfaction with life scale. J Pers Assess 1985;49:71–5. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- 74.Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 2004;43:245–65. 10.1348/0144665031752934 [DOI] [PubMed] [Google Scholar]
- 75.Thompson ER. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS). J Cross Cult Psychol 2007;38:227–42. 10.1177/0022022106297301 [DOI] [Google Scholar]
- 76.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 77.Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: distinguishing rumination from reflection. J Pers Soc Psychol 1999;76:284–304. 10.1037/0022-3514.76.2.284 [DOI] [PubMed] [Google Scholar]
- 78.Preece DA, Becerra R, Robinson K, et al. The emotion regulation questionnaire: psychometric properties in general community samples. J Pers Assess 2020;102:348–56. 10.1080/00223891.2018.1564319 [DOI] [PubMed] [Google Scholar]
- 79.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res 2011;45:626–9. 10.1016/j.jpsychires.2010.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 81.Kraemer HC, Mintz J, Noda A, et al. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry 2006;63:484–9. 10.1001/archpsyc.63.5.484 [DOI] [PubMed] [Google Scholar]
- 82.Walters SJ, Bonacho Dos Anjos Henriques-Cadby I, Bortolami O, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom health technology assessment programme. BMJ Open 2017;7:15276. 10.1136/bmjopen-2016-015276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Steenkamp MM, Litz BT, Marmar CR. First-Line psychotherapies for Military-Related PTSD. JAMA 2020;323:656. 10.1001/jama.2019.20825 [DOI] [PubMed] [Google Scholar]
- 84.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by Accelerometer. Med Sci Sports Exerc 2008;40:181–8. 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 85.Wilson LC. The prevalence of military sexual trauma: a meta-analysis. Trauma Violence Abuse 2018;19:584–97. 10.1177/1524838016683459 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-051885supp001.pdf (60.6KB, pdf)
bmjopen-2021-051885supp002.pdf (47.7KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data are available upon reasonable request. Due to legal and ethical restrictions, we are unable to share data publicly because the data contain potentially identifying and/or sensitive patient information. Subject to IRB approval, de-identified data will be released to a local Department of Veterans Affairs (VA) Puget Sound Health Care System and/or national VA research data repository for release to non-VA protocols. The VA research data repository administrator will be responsible for reviewing and responding to requests to release data to non-VA requestors. A data use agreement compliant with Veterans Health Administration Handbooks 1200.12 and 1605.1 will be required between Veterans Health Administration and the requestor. Review and approval by VA privacy officer is required prior to disclosure. Data access requests will be reviewed by the IRB of the VA Puget Sound Health Care System (contact via Dr. Littman – alyson.littman@va.gov), via mail address: 1660 S Columbian Way, Building 101 – 5W41, Seattle, WA 98108.