Abstract
This study evaluated the feasibility and efficacy of integrating mindfulness training into a phone-based weight loss program to improve outcomes in those with high levels of emotional eating. Participants were 75 enrollees into an employer-sponsored weight loss program who reported high levels of overeating in response to thoughts and feelings. Seventy-five overweight and obese participants (92% female, 65% Caucasian, aged 26 to 68) were randomized to the new mindfulness weight loss program (n = 50) or the standard behavioral weight loss program (n = 25). Both programs consisted of 11 coaching calls with health coaches and registered dietitians with supplemental online materials. Satisfaction, engagement, and percent weight lost did not significantly differ for intervention vs. control at six months. Intervention participants had significantly better scores at six month follow-up on mindful eating, binge eating, experiential avoidance, and one mindfulness subscale. Exploratory analyses showed that improvements on several measures predicted more weight loss in the intervention group. This pilot study found that integrating mindfulness into a brief phone-based behavioral weight loss program was feasible and acceptable to participants, but did not produce greater weight loss on average, despite hypothesized changes in mindful eating. Only one third of intervention participants reported participating in mindfulness exercises regularly. Mechanisms of change observed within the intervention group suggest that for adults with high levels of emotional eating those who embrace mindful eating and meditation may lose more weight with a mindfulness intervention.
Keywords: Mindfulness, weight loss, obesity, emotional eating, phone-based treatment
INTRODUCTION
Obesity continues to be a significant health problem in the US with nearly 40% of adults in the US reporting a body mass index (BMI; kg/m2) in the obese range.1 Behavioral weight loss programs have proven effective at reducing body weight and preventing negative health outcomes such as diabetes and kidney disease.2–4 However, there are substantial individual differences in response to such interventions with some participants losing significantly more than the 5–10% clinical target while others do not lose or even gain weight.4,5 One group with more difficulty losing weight and keeping it off are those who overeat in response to internal cues such as unpleasant thoughts or emotions, a state characterized as a high “internal disinhibition”6 or simply known as emotional eating. Higher levels of emotional eating, are related to higher BMI7,8 and individuals with higher baseline levels of emotional eating lose less weight during weight loss programs. 7 Further, reductions in emotional eating during participation in a weight loss program predict better weight loss maintenance.9
One prominent theory concerning eating disorders posits that people overeat as an attempt to escape or cope with negative affect.10 “Experiential avoidance” refers to an unwillingness to experience uncomfortable internal stimuli such as thoughts and feelings.11 Those with high experiential avoidance are more likely to engage in emotional eating and binge eating and those that decrease experiential avoidance lose more weight.12 Experiential avoidance also mediates the relationship between negative affect (e.g., anxiety, shame) and problematic eating behaviors such as binge eating.13,14 While little research has focused on interventions for those who struggle with emotional overeating,6 interventions that directly address emotional eating could improve outcomes for affected individuals.6,15 Mindfulness directly teaches skills to increase emotional acceptance and decrease experiential avoidance and thus may have the potential to decrease binge and emotional eating. For example, mindful eating training (a core component of mindfulness interventions for weight management) predicts eating fewer sweets, decreased fasting glucose,16 and weight loss.17 Mindfulness and mindful eating require a deliberate conscious approach to food and decreased reactivity to uncomfortable emotions and, thus, appear to be a well matched intervention for emotional overeating.
The present randomized controlled pilot study integrated mindfulness into an existing commercial phone-based behavioral weight loss program. Specifically, we evaluated the hypotheses that the new intervention would have equivalent acceptability and feasibility to the existing program. Further, we conducted a preliminary evaluation of weight loss outcomes and changes in variables such as mindfulness, mindful eating, and experiential avoidance as compared to the standard behavioral weight loss program.
METHOD
Participants
Participants were 75 adult enrollees of the phone-based employer-sponsored behavioral weight loss program, Weight Talk™ (WT), between August 2014 and June 2015. WT enrollees from five employers who agreed to participate in the study and who met initial criteria of starting Body Mass Index (BMI) between 25 kg/m2 and 35 kg/m2 were invited for screening. The five employers represented a range of blue- and white-collar industries, included large and small companies, and included participants living across the US. Interested participants completed telephone screenings to assess for stress- and emotion-related overeating and only those with high emotional eating scores were eligible. Other inclusion criteria included regular access to email and the internet, being over 18 years of age, and willingness and ability to complete study and intervention procedures. Exclusion criteria were pregnancy, diabetes, bariatric surgery in the past 12 months or planned within next 6 months, diagnosis of anorexia or bulimia nervosa, and use of weight loss medications.
Procedure
All procedures were approved in advance by the Western IRB. Participants were screened and consented via phone. Upon completion of the web-based baseline questionnaire (which took about 30 minutes), participants were randomized to either the standard WT group (control) or the experimental intervention, Mind Your Weight (MYW) at a 2:1 ratio with the MYW group receiving two participants for every one participant in the control group. Randomization utilized a random numbers table. The purpose of the unequal randomization was to gather more data on the experimental program which was newly developed. Study staff was not privy to the randomization sequence. The participants received a $40 gift card after completing the baseline and two intervention calls. Follow-up surveys were collected via web six months after enrollment. Sixty-nine of the 75 study participants completed the follow-up, a 92% follow-up rate (90% in the intervention group and 96% in the control group). Participants were sent a gift card after completing the follow-up.
Interventions
Control condition:
The Weight Talk™ (WT) weight loss program is based on the National Institute of Health (NIH) Clinical Guidelines on Identification, Evaluation, and Treatment of Overweight and Obesity in Adults,18 the Diabetes Prevention Program3 and includes nutrition recommendations based on the NIH-developed “Dietary Approaches to Stop Hypertension” (DASH) eating plan.19 Physical activity recommendations are from the American College of Sports Medicine and the Physical Activity Guidelines for Americans.20 Table 1 describes the content of the WT intervention.
Table 1.
Call Content of the Weight Talk Weight Loss Program (WT) and Mind Your Weight Integrated Weight Talk/Mindfulness program (MYW)
| Call | Weight Talk (WT) | Mind Your Weight (MYW) (call topics + weekly practice activities) |
|---|---|---|
| 1 | Goal setting and tracking food and weight | Same as WT |
| 2 | Nutrition basics and setting calorie goal (with RD) |
Same as WT plus discussion of stress eating and mindful eating (with RD). |
| eLesson: Mindful weight loss | ||
| MP3: Body Scan | ||
| 3 | Increase physical activity, decrease sedentary time |
Same as WT plus introducing yoga as physical activity for stress reduction. |
| eLesson: None. Links to online yoga videos. | ||
| MP3: 5 minute breath-focused meditation | ||
| 4 | CBT-based stress management | Mindfulness rationale, discussion of meditation and practice benefits. |
|
eLesson: Introduction to meditation, mindfulness at first and last bite exercise | ||
| MP3: None | ||
| 5 | CBT-based approach to negative thoughts | Mindful approach to thoughts: Discussion of noticing thoughts and letting them go |
| eLesson: Accepting thoughts & values-based action. | ||
| MP3: 15 minute breath-focused meditation | ||
| 6 | Structuring the environment to support weight loss (with RD) |
Mindful eating (with RD) |
| eLesson: Video-based mindful eating experiential exercise | ||
| MP3: None | ||
| 7 | Managing time to increase ability to plan meals and cook |
Emotions and eating, alternatives to eating for coping with stress, planned emotional eating |
| eLesson: Effective emotional eating | ||
|
MP3: Emotion-focused meditation | ||
| 8 | How to navigate difficult situations such as holidays, parties, vacation |
Mindfulness in daily activities |
| eLesson: Mindfulness in everyday life | ||
| MP3: Walking meditation | ||
| 9 | Weight maintenance strategies (e.g., increase physical activity) |
Mindful choices & coping with cravings |
| eLesson: Cravings and urges | ||
| MP3: Surf the urge | ||
| 10 | Rebounding from lapses | Acceptance and self-compassion, body image, & weight stigma. |
|
eLesson: Self-compassion. | ||
| MP3: Loving kindness meditation | ||
| 11 | Maintaining motivation over the long- term and plan for future |
Lapse and relapse, self-acceptance, discussion of applying mindfulness moving forward. |
WT consists of 11 proactive phone-based counseling sessions (i.e., program calls) as well as unlimited inbound support calls. Two of the 11 program calls are conducted by registered dietitians (RDs) and the other calls are with a health coach. WT calls are scheduled at the participant’s convenience, with most participants choosing to schedule calls weekly or biweekly The overall program lasts six months and during that time participants can call a coach at any point after their 11 calls are completed. WT calls are brief with Calls 1 to 4 averaging about 30 minutes and the remaining calls 20 minutes each. The WT program includes an integrated website and participants are sent a printed program guide, a Fitbit Zip activity tracker (Fitbit, Inc., San Francisco, CA), a tape measure for assessing waist circumference, and a food journal. As part of study participation, all participants were sent a Fitbit Aria wireless scale (Fitbit, Inc., San Francisco, CA) and data were viewable on the WT website.
Experimental intervention.
The Mind Your Weight (MYW) weight loss program follows the same structure as WT, offering 11 proactive coaching calls, two of which were with an RD Starting with Call 2, participants were introduced to the treatment rationale and basic mindfulness concepts. Each MYW call started with a “mindful moment” (a 60 second mindfulness exercise). The coach would check in with the participant about weight and progress towards the weight loss goal, food tracking, and physical activity followed by a discussion of the mindfulness topic for the call. Call topics included mindfulness meditation, mindfulness of everyday activities, mindful eating, acceptance of thoughts and emotions, and self-compassion. In addition, participants were emailed links to brief educational eLessons which included links to resources and downloadable mindfulness exercises (which were also available on iTunes). Table 1 contains additional details about the content of the intervention. Coaches monitored use of the eLessons and mindfulness exercises and encouraged participants to practice mindfulness between calls.
Health coaches, training, and fidelity monitoring
Telephonic health coaching was carried out by WT health coaches, including RD and non-RD coaches, who receive more than 200 hours of training as part of their employment. In addition to the WT training, the MYW coaches participated in additional training on the mindfulness intervention, including didactic instruction, experiential mindfulness exercises, and rehearsal of call topic discussions. Each call for both the MYW and WT participants was recorded and 15% were randomly selected for fidelity monitoring. Calls were rated using a checklist and the 3– 6 required elements of each call (e.g., delivering the mindful moment, describing mindful eating, asking about progress towards weight goal) was coded as present or absent. Ninety four percent of the required call elements were coded as present.
Measures
Screening measure.
In order to screen participants for emotional eating/internal disinhibition we used seven items from the Internal Disinhibition subscale of the Eating Inventory.7 These items include statements such as, “When I feel lonely, I console myself by eating.” Items are scored as true or false (1 or 0). A minimum score of 5 (out of 7) was required for entrance into the study.
Feasibility and acceptability.
Feasibility and acceptability were measured by the number of people who declined to consent to the study and who did not complete their baseline assessment (passive refusal), by intervention engagement (number of calls completed), and by satisfaction. Satisfaction questions developed for the study were used to compare satisfaction of participants in both groups and included questions about overall impression of the program, willingness to recommend to a friend, and agreement that the program had been helpful with regard to emotional eating. Weight loss outcomes and mechanisms. Weight was self-reported by participants at enrollment and on the six-month survey. All participants were sent a wireless digital scale (Fitbit Aria) to increase accuracy of self-report. Participants who did not complete the survey, but had self-reported weight during a call (n = 5) or weight from the wireless scale (n = 1) within 6 weeks of the survey date in the system were included in the weight analysis.
Instruments used in the study to measure attitudes and behavior, include:
Binge Eating Scale (BES):
The BES 21 is a 16-item scale that was used to assess the severity level of the behavioral and emotional/cognitive characteristics of binge eating. This scale has been shown to have good construct reliability and convergent validity.22 We used a version of the BES with revised and updated language. Mindful Eating Questionnaire (MEQ): The MEQ23 evaluates level of awareness and nonjudgment when eating. The MEQ is a 28-item questionnaire with five subscales: disinhibition, awareness, external cues, emotional response, and distraction. The MEQ has been shown to have good psychometric properties.23 Short Form Perceived Stress Scale (PSS-4): The PSS-424 is a 4-item questionnaire that measures one’s assessment of stressful situations during the past month. The PSS-4 has been shown to be reliable and have acceptable psychometric properties.24 Generalized Anxiety Disorder −7 (GAD-7). 25 Anxiety was measured with the GAD-7, a 7-item scale used to screen for Generalized Anxiety Disorder (GAD) and assess severity of anxiety. The tool asks frequency of GAD symptoms in the past two weeks. The GAD-7 has demonstrated good procedural and convergent validity and test-retest reliability. Using a cut off of 10 maximizes specificity and sensitivity for a diagnosable anxiety disorder.25
Acceptance and Action Questionnaire for Weight-Related Difficulties (AAQ-W).26 The AAQ-W is a 22-item scale that evaluates acceptance and psychological flexibility when experiencing challenging emotions and thoughts concerning weight and the extent to which weight-related emotions and thoughts inhibit one’s valued actions. The AAQ-W has shown good initial psychometrics in a weight loss seeking population and was sensitive to change that occurred during an acceptance-based weight control program.26 The Five Facet Mindfulness Questionnaire –Short Form (FFMQ-SF).27 The FFMQ-SF is a 24-item, Likert-type scale examining the five facets of mindfulness: observing, describing, acting with awareness, nonjudging of inner experience, and nonreactivity to inner experience.27–29 The FFMQ-SF has been reported to have good validity and psychometric properties.27 Patient Health Questionnaire-2 (PHQ-230): The PHQ-2 is a widely-used 2-item questionnaire that measures the incidence of depressed mood over the previous two weeks. The PHQ-2 has demonstrated good construct and criterion validity.30
Analysis
Means, proportions, and 95% confidence intervals were used to describe participant characteristics and baseline measures for the groups. The primary study outcomes were treatment engagement (call completion) and satisfaction, which were hypothesized to be equivalent between the two groups. We used confidence intervals and non-inferiority margins to examine non-inferiority for MYW on these measures, as outlined in FDA guidelines (FDA, 2010). Non-inferiority margins for measures with better outcomes at larger values were established as the upper bound of the 95% CI for the difference between the control and MYW means (i.e. the mean of the control group minus the mean of the MYW group). For example, a non-inferiority margin of 2.0 would be interpreted as being 95% confident that the mean value of the outcome measure for the control group is no more than 2.0 units better than the mean value for the MYW group. Secondary outcomes were exploratory in nature and included weight change and mindfulness and psychological functioning measures. We used ANCOVAs to examine differences for MYW versus control on 6-month outcomes, controlling for age, race/ethnicity, and baseline scores on the outcome measure. Additionally, baseline FFMQ Acting with Awareness was included as a covariate for analyses examining 6-month outcomes theoretically related to that subscale (i.e., MEQ, AAQ-W, all FFMQ subscales) as it significantly differed between the groups at baseline. Finally, we conducted exploratory analyses to examine potential mechanisms and moderators of treatment effects on percent weight loss. Kendall’s tau b correlations were used for these exploratory analyses due to the non-normal distribution of percent weight loss. All analyses were conducted in SAS 9.3.
RESULTS
Participants
Participant characteristics and baseline assessment measures are reported for all randomized participants in Table 2. Participants ranged in age from 26 to 68, were predominately female (92%) with some college education or higher (95%), and had a mean BMI (31.5 kg/m2) in the obese range. Nearly half (46.6%) of the total sample had GAD-7 scores of 10 or greater at baseline. Overall, 65.3% of participants were white non-Hispanic. Although not statistically significant, 32% of MYW participants were Black, non-Hispanic, compared to 16% of control participants. There was a significant difference on the baseline FFMQ Acting with Awareness subscale between the MYW (mean = 14.9, SD = 4.1) and control group (m = 17.4, SD = 2.8, p = 0.008), showing that the control group was higher in this aspect of mindfulness than the intervention group.
Table 2.
Baseline Characteristics of Study Participants by Treatment Group
| Mind Your Weight (MYW) (n=50) |
Weight Talk (WT; control) (n=25) |
Total Sample (n=75) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Demographics | n | % | 95% CI | n | % | 95% CI | n | % | 95% CI |
| Sex, Female | 46 | 92.0 | [80.8, 97.8] | 23 | 92.0 | [74.0, 99.0] | 69 | 92.0 | [83.4, 97.0] |
| Race/ethnicity | |||||||||
| White nonhispanic | 31 | 62.0 | [47.2, 75.4] | 18 | 72.0 | [50.6, 87.9] | 49 | 65.3 | [53.5, 76.0] |
| Black nonhispanic | 16 | 32.0 | [19.5, 46.7] | 4 | 16.0 | [4.5, 36.1] | 20 | 26.7 | [17.1, 38.1] |
| Hispanic | 2 | 4.0 | [0.5, 13.7] | 3 | 12.0 | [2.6, 31.2] | 5 | 6.7 | [2.2, 14.9] |
| Asian | 1 | 2.0 | [0.1, 10.7] | 0 | 0.0 | 1 | 1.3 | [0.0, 7.2] | |
| Education | |||||||||
| High school/GED or less | 3 | 6.0 | [1.3, 16.6] | 1 | 4.0 | [0.1, 20.4] | 4 | 5.3 | [1.5, 13.1] |
| Some college | 18 | 36.0 | [22.9, 50.8] | 10 | 40.0 | [21.1, 61.3] | 28 | 37.3 | [26.4, 49.3] |
| College graduate | 29 | 58.0 | [43.2, 71.8] | 14 | 56.0 | [34.9, 75.6] | 43 | 57.3 | [45.4, 68.7] |
| M | SD | 95% CI | M | SD | 95% CI | M | SD | 95% CI | |
|
|
|||||||||
| Age (in years) | 45.5 | 9.4 | [42.8, 48.2] | 50.8 | 10.5 | [46.5, 55.1] | 47.3 | 10.0 | [44.9, 49.6] |
| Baseline Measures | |||||||||
| BMI | 31.6 | 2.3 | [30.9, 32.2] | 31.4 | 2.4 | [30.5, 32.5] | 31.5 | 2.3 | [31.0, 32.1] |
| Confidence (reported at first coaching call) |
7.3 | 2.3 | [6.6, 8.0] | 6.9 | 2.4 | [5.8, 7.9] | 7.1 | 2.3 | [6.6, 7.7] |
| Acceptance and Action Questionnaire for Weight (AAQ-W) |
89.3 | 17.2 | [84.3, 94.2] | 84.6 | 17.3 | [77.4, 91.7] | 87.7 | 17.3 | [83.7, 91.7] |
| Binge Eating Scale (non- standard) (BES) |
19.4 | 6.8 | [17.4, 21.3] | 17.9 | 7.4 | [14.9, 20.9] | 18.9 | 7.0 | [17.2, 20.5] |
| Perceived Stress Scale-4 (PSS) |
7.7 | 2.5 | [7, 8.4] | 7.7 | 3.3 | [6.4, 9.1] | 7.7 | 2.8 | [7.1, 8.4] |
| GAD-7 | 10.1 | 6.1 | [8.3, 11.8] | 8.3 | 5.1 | [6.2, 10.4] | 9.4 | 5.8 | [8.1, 10.8] |
| PHQ-2 | 1.9 | 1.6 | [1.5, 2.4] | 1.7 | 1.7 | [1, 2.4] | 1.9 | 1.6 | [1.5, 2.2] |
| Mindful Eating Questionnaire Summary Score (MEQ) |
2.4 | 0.3 | [2.3, 2.5] | 2.4 | 0.3 | [2.3, 2.5] | 2.4 | 0.3 | [2.3, 2.5] |
| Awareness | 2.4 | 0.6 | [2.2, 2.6] | 2.3 | 0.5 | [2.1, 2.5] | 2.4 | 0.6 | [2.2, 2.5] |
| Distraction | 2.5 | 0.6 | [2.3, 2.6] | 2.5 | 0.7 | [2.2, 2.7] | 2.5 | 0.6 | [2.3, 2.6] |
| Disinhibition | 2.3 | 0.6 | [2.2, 2.5] | 2.2 | 0.6 | [2, 2.4] | 2.3 | 0.6 | [2.2, 2.4] |
| Emotion | 2.2 | 0.6 | [2.1, 2.4] | 2.3 | 0.7 | [2.0, 2.6] | 2.2 | 0.6 | [2.1, 2.4] |
| External | 2.7 | 0.3 | [2.6, 2.8] | 2.8 | 0.4 | [2.6, 2.9] | 2.7 | 0.4 | [2.6, 2.8] |
|
Five-Facet Mindfulness
Questionnaire (FFMQ) |
|||||||||
| Describing | 16.4 | 4.0 | [15.3, 17.6] | 18.1 | 3.4 | [16.7, 19.5] | 17 | 3.9 | [16.1, 17.9] |
| Non-reactivity to inner experience |
15.0 | 2.8 | [14.2, 15.8] | 15.2 | 3.0 | [14, 16.5] | 15.1 | 2.9 | [14.4, 15.8] |
| Non-judging of inner experience |
14.9 | 3.4 | [13.9, 15.8] | 16.1 | 4.6 | [14.2, 18] | 15.3 | 3.9 | [14.4, 16.2] |
| Observing | 13.8 | 3.3 | [12.9, 14.8] | 14.2 | 2.3 | [13.3, 15.2] | 14 | 3.0 | [13.3, 14.7] |
| Acting with awareness** | 14.9 | 4.1 | [13.7, 16] | 17.4 | 2.8 | [16.2, 18.5] | 15.7 | 3.9 | [14.8, 16.6] |
Significant difference between control and intervention groups at baseline, p=0.008
Screening and Study Acceptability
Of the 183 participants screened for study inclusion, 86 were eligible (47%). Of those 86 participants who were eligible, four (5%) declined to participate. An additional 7 (8%) did not complete their baseline assessment which could be considered a passive refusal to participate. Of the 177 who completed the emotional eating screening 50% (n = 89) met inclusion criteria of high levels of emotional eating.
Treatment Engagement
MYW participants completed 6.0 (SD = 4.2) intervention calls (including program and support calls) on average versus 6.6 (SD = 3.7) for control participants. Our hypothesis was that MYW participants would not take significantly fewer calls than the control group. MYW was non-inferior to control for call completion with a non-inferiority margin of 2.1 calls or greater (i.e., we can be 95% confident that the control group did not follow a distribution with a mean number of calls more than 2.1 greater than the MYW group). One participant (4%) in the control group and 4 participants (8%) in the intervention group completed zero intervention calls and were excluded from some analyses as noted below.
Treatment Satisfaction
Forty-five MYW participants (response rate = 90%) and 23 control participants (response rate = 92%) reported treatment satisfaction data on the 6-month survey, Fisher’s p = 1.00. MYW and WT participants provided similar ratings (1 to 5 Likert scale where 5 is positive) on program satisfaction for the following domains: overall program impression (MYW: M = 3.8 (0.9) 95% CI [3.5, 4.1]; WT: M = 3.7 (0.9), CI [3.3 – 4.1]); recommend program to friend wanting to lose weight (MYW: M = 3.91.0) CI [ 3.6 – 4.2]; WT: M = 3.8 (1.0) CI [3.4 – 4.3]), and program helped realize when I was eating due to stress (MYW: M = 3.9 (1.0) CI [3.6 – 4.2], WT: M = 3.8 (1.1) CI [ 3.3 – 4.3]). MYW was non-inferior to WT on the first and third items with non-inferiority margins of 0.3 or greater and was non-inferior to WT on recommending the program to a friend with a non-inferiority margin of 0.4 or greater (i.e., we can be 95% confident that the WT group did not follow a distribution with mean satisfaction ratings more than 0.3–0.4 greater on the 5-point Likert scale than the MYW group).
Satisfaction and engagement with MYW additional components
MYW participants reported their frequency practicing meditation and their likelihood of continuing to practice in the future. About one third (33.3%) reported practicing multiple times per week, and 26% reported never or almost never practicing meditation. Slightly more than half (55.5%) reported being likely or very likely to practice in the future and 18% reported being unlikely to practice in the future. Sixty percent of participants found the eLessons helpful or very helpful, 11% found them not helpful.
Weight
Weight data at 6-months was available for 45 MYW (90% response rate) and 24 WT (96% response rate) participants (Table 3). Percent weight lost for MYW versus WT did not significantly differ: MYW participants lost 2.7% (SD 4.9%) of their weight from baseline to follow-up, on average, compared to WT participants who lost 3.1% (SD 3.7%), on average.
Table 3.
Baseline and Follow-up Scores for Study Participants by Treatment Group (Respondents to 6-month assessment)
| Mind Your Weight (MYW) | Weight Talk (WT; control) | Treatment Group Effect2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Measure | n | Baseline M (SD) |
Follow-up M (SD) |
n | Baseline M (SD) |
Follow-up M (SD) |
F | DF | p | Effect size: Hedges g (approx. 95% CI) |
| % weight loss * | 45 | -- | 2.7 (4.9) | 24 | -- | 3.1 (3.7) | 0.33 | (1,68) | 0.57a | −0.15 (−0.64, 0.35) |
| Weight loss (kgs) * | 45 | -- | 2.4 (4.4) | 24 | -- | 2.6 (3.2) | 0.18 | (1,68) | 0.68a | −0.11 (−0.60, 0.39) |
| AAQ-W | 42 | 88.3 (17.6) | 69.4 (23.6) | 22 | 84.6 (18.2) | 77.7 (19.1) | 8.55 | (1,63) | 0.005c | −0.62 (−1.15, −0.09) |
| BES | 42 | 19.2 (6.8) | 11.5 (8.1) | 22 | 18.0 (7.5) | 15.9 (7.3) | 8.29 | (1,63) | 0.006b | −0.61 (−1.14, −0.08) |
| PSS-4 | 42 | 7.4 (2.4) | 6.1 (2.9) | 22 | 7.7 (3.4) | 6.5 (3.1) | 0 | (1,63) | 0.97b | −0.01 (−0.52, 0.51) |
| GAD-7 | 42 | 9.8 (6.0) | 7.1 (6.3) | 22 | 8.5 (5.2) | 8.9 (6.0) | 3.39 | (1,63) | 0.07b | −0.40 (−0.92, 0.12) |
| PHQ-2 | 43 | 1.8 (1.6) | 1.2 (1.5) | 22 | 1.7 (1.8) | 1.5 (1.8) | 1.25 | (1,64) | 0.27b | −0.26 (−0.77, 0.26) |
| MEQ* | 44 | 2.4 (0.3) | 2.7 (0.4) | 23 | 2.4 (0.3) | 2.5 (0.3) | 9.3 | (1,66) | 0.003c | 0.71 (0.19, 1.23) |
| Awareness* | 44 | 2.4 (0.6) | 2.7 (0.6) | 23 | 2.3 (0.5) | 2.4 (0.5) | 8.72 | (1,66) | 0.005c | 0.66 (0.14, 1.18) |
| Distraction* | 44 | 2.4 (0.6) | 2.6 (0.7) | 23 | 2.5 (0.7) | 2.5 (0.6) | 0.76 | (1,66) | 0.39c | 0.21 (−0.3, 0.71) |
| Disinhibition* | 44 | 2.3 (0.6) | 2.8 (0.6) | 23 | 2.2 (0.6) | 2.5 (0.6) | 5.18 | (1,66) | 0.03c | 0.51 (0, 1.02) |
| Emotion* | 44 | 2.2 (0.6) | 2.7 (0.7) | 23 | 2.3 (0.7) | 2.4 (0.7) | 5.08 | (1,66) | 0.03c | 0.53 (0.02, 1.04) |
| External* | 44 | 2.7 (0.3) | 2.6 (0.4) | 23 | 2.8 (0.4) | 2.7 (0.4) | 1.31 | (1,66) | 0.26c | −0.31 (−0.82, 0.19) |
| (FFMQ) | ||||||||||
| Describing* | 42 | 16.4 (4.3) | 18.3 (4.3) | 22 | 18.0 (3.5) | 18.3 (3.5) | 2.16 | (1,63) | 0.15c | 0.3 (−0.22, 0.82) |
| Non-reactivity to inner experience* | 42 | 15.3 (2.7) | 17.0 (2.9) | 22 | 14.8 (2.8) | 14.4 (2.6) | 21.63 | (1,63) | <0.001c | 1.14 (0.58, 1.69) |
| Non-judging of inner experience* | 42 | 14.6 (3.6) | 16.4 (4.0) | 22 | 15.9 (4.7) | 16.1 (4.2) | 1.57 | (1,63) | 0.21c | 0.31 (−0.21, 0.83) |
| Observing* | 42 | 13.9 (3.4) | 15.0 (3.3) | 22 | 14.6 (2.1) | 14.5 (2.9) | 2.43 | (1,63) | 0.12c | 0.35 (−0.17, 0.87) |
| Acting with awareness* | 42 | 15.3 (4.2) | 16.2 (4.3) | 22 | 17.5 (2.9) | 16.5 (3.3) | 1.28 | (1,63) | 0.26b | 0.25 (−0.27, 0.77) |
Higher mean values represent poorer functioning on all measures, except for % weight loss, weight loss, MEQ, and FFMQ scales; these measures are marked with asterisks (*) in the table.
Analysis of covariance on 6-month follow-up outcome measure controlling for variables specified with superscripts a-c.
Controlled for age, race/ethnicity (white vs. non-white or Hispanic), and baseline BMI.
Controlled for age, race/ethnicity (white vs. non-white or Hispanic), and baseline score on outcome measure.
Controlled for age, race/ethnicity (white vs. non-white or Hispanic), baseline score on outcome measure, and FFMQ Acting with Awareness subscale.
Mindfulness and other psychological measures
Outcome data on mindfulness and other psychological measures were reported by 42–44 MYW participants (84–92% response rates) and by 22–23 WT participants (88–92% response rates) (Table 3). There were no significant differences between groups in response rates, Fisher’s ps = 0.71 – 1.00. As shown in Table 3, MYW participants exhibited significantly better scores at follow-up with regard to mindful eating (MEQ total score), three of the five mindful eating subscales (MEQ Awareness, MEQ Disinhibition, MEQ Emotion), binge eating (BES), acceptance and psychological flexibility related to weight (AAQ-W), and the non-reactivity to inner experience mindfulness subscale (FFMQ non-reactivity), compared to WT participants. There was a non-significant trend for MYW participants to have better anxiety scores (GAD-7) at follow-up compared to WT participants. At follow-up, 25.6% (95% CI [13.5%, 41.2%] of MYW participants met or exceeded a cutoff score of 10 on the GAD-7 compared to 45.5% (95% CI [24.4%, 67.8%] of WT participants, χ2(1, N = 65) = 2.63, p = 0.11. There were no significant differences between MYW and WT participants on perceived stress (PSS-4), depression (PHQ-2), or on the remaining four mindfulness subscales (FFMQ describing, non-judging of inner experience, observing, and acting with awareness) at the 6-month assessment.
Mechanisms/Moderators
We explored potential mechanisms of the mindfulness treatment among participants who completed one or more intervention calls by correlating changes from baseline to follow-up (baseline minus follow-up score) with percent weight loss. For MYW participants, improvement in MEQ summary scores from baseline to follow-up was associated with higher percent weight loss, rτ (n = 40) = −0.24, p = 0.03. When looking at the individual subscales, the MEQ Disinhibition subscale showed a significant association between improvement from baseline to follow-up and higher percent weight loss for the MYW group, rτ (n = 40) = −0.26, p = 0.02 There was also a non-significant trend for improvement in the MEQ Distraction subscale from baseline to follow-up being associated with higher percent weight loss, rτ (n = 40) = −0.22, p = 0.05. Similarly, for MYW participants, improvement in AAQ-W scores from baseline to follow-up was associated with higher percent weight loss, rτ (n = 38) = 0.25, p = 0.03. A non-significant trend for higher percent weight loss in MYW participants was associated with improvement in binge eating (BES) from baseline to follow-up, rτ (n = 38) = 0.20, p = 0.08. None of these patterns was observed in the control group. Changes in FFMQ, GAD-7, PSS-4, and PHQ-2 scores were not related to percent weight loss for either group.
We also looked at engagement in treatment to see if more engagement was related to more weight loss. The number of calls completed was significantly associated with increased percent weight loss for MYW participants, rτ (n = 45) = 0.28, p = 0.008, but not for control participants. We also saw a pattern of more weight loss in those who reported more frequent meditation practice in the MYW participants. We compared percent weight loss for those who reported practicing multiple times per week (n = 15, m = 4.39%, se = 1.28%) to those who reported practicing less frequently or never (n = 23, m = 1.96%, se = 1.08%). This difference was not statistically significant (p = .11).
Finally, we explored whether the MYW treatment was more effective for subgroups of participants with regard to percent weight loss. There were no significant relationships between baseline scores on the MEQ, AAQ-W, BES, FFMQ subscales, or GAD-7 and percent weight loss for the MYW group. There were also no significant differences in percent weight loss for MYW participants based on race/ethnicity, education, baseline age, or BMI.
DISCUSSION
The present study gives preliminary evidence that participation in a mindfulness intervention as part of an evidence-based behavioral weight loss program produced significant changes in mindful eating and binge eating, as well as changes in overall mindfulness when compared to the control condition. There was no indication, however, that the mindfulness intervention produced greater weight loss at 6-months, although we did find relationships between weight loss and positive changes in mindful eating and psychological flexibility around weight (acceptance). Our results also show that mindfulness can be integrated into a phone-based weight loss program without impacting participant engagement or satisfaction, and that health coaches and dietitians can deliver a mindfulness intervention with good fidelity.
Weight loss outcomes were not significantly different between the intervention and control groups and, overall, weight loss was modest in both groups (averaging about 3% of body weight). The stated program goal was to achieve weight loss of at least 5% and only 25% of participants achieved this goal. It should be noted that we selected only participants with high scores on the emotional eating screening measure. This group has more difficulty losing weight7,31 and, therefore, these results should not be compared to results from other, non-screened, groups. About 50% of those screened for study eligibility met the inclusion criteria, making those with high levels of emotional eating a substantial population of concern. Further, although weight loss was modest, we did see greater decreases in anxiety and binge eating for MYW participants that could be clinically significant based on effect sizes.
The finding that mindfulness training does not necessarily lead to increased weight loss aligns with recent literature.32 Four reviews have been conducted since 2014 and have found consistent positive effects of mindfulness-based interventions on binge eating as well as on emotional eating and emotional distress (when measured), but less consistent effects on weight loss.33–36 Olson and Emery’s review of mindfulness interventions for weight loss35 reported that 13 of 19 studies found significant weight loss in the mindfulness groups. However, they also noted substantial limitations this research, including single group or a wait list control designs and researchers neglecting to show that changes in mindfulness and/or mindful eating are related to weight loss outcomes. The current study tested MYW against an active behavioral weight loss treatment; comparable outcomes between the two groups does not indicate that MYW was ineffective for weight loss. Further, there is preliminary evidence that other metabolic indicators, such as fasting glucose, may be improved with mindfulness and that changes in mindful eating are particularly important.16 Finally, we saw a pattern of greater weight loss in those who reported meditating the most (two or more times per week). It may be that mindfulness promotes weight loss only for those who embrace it and comply with practice recommendations. A larger study would allow us to further explore this finding.
In developing this intervention, our goal was to improve weight loss outcomes by integrating critical components of a behavioral weight loss intervention with a mindfulness and mindful eating training program. Unlike other mindfulness interventions for weight loss,34 we retained a focus on goal setting, regular weighing, tracking food, increasing physical activity, and following the DASH diet recommendations. We did not increase the length of treatment (number or duration of sessions): thus in adding mindfulness, we took out elements of the standard program, including cognitive restructuring (replaced with acceptance), time management, stimulus control, weight loss maintenance strategies, etc. It is possible that eliminated content impacted weight loss outcomes to about the same degree as the added mindfulness components, resulting in equivalent weight loss across groups. Although engagement did not differ significantly between conditions, because the bulk of the mindfulness-specific content was in the second half of the intervention, half of the participants in the intervention group did not receive much of the mindfulness content.
A strength of this study is the translation of mindfulness into a low intensity phone-based weight loss program. Mindfulness interventions are typically in-person group interventions with sessions lasting 1 to 2.5 hours each.16 In contrast, the MYW intervention was minimal, and yet the observed changes in mindful eating and binge eating suggest this low intensity version was effective in changing some behaviors or attitudes toward behavior. Many people cannot afford the time needed to attend long weekly group sessions. Developing versions of mindfulness interventions that can be disseminated more broadly will allow us to evaluate the usefulness of the approach with groups that may never have consented to attend a high intensity intervention. Another strength of the study is examination of mechanisms and the finding that positive changes in mindful eating and binge eating are related to weight loss in MYW. This suggests some promise of improvements in outcomes, if those changes can be expanded upon. Additionally, this study used an effective weight loss program as a control, an approach sorely lacking in the published literature and a stringent test of a newly developed intervention.35 Finally, while there are difficulties conducting research in a real-world setting, by using actual working coaches and formats already acceptable and affordable to purchasers we can potentially increase the speed with which interventions are disseminated.
There were also a number of limitations to the study. As expected in any pilot feasibility study our sample size was too small to allow for drawing definitive conclusions. The (planned) unequal group sizes may have resulted in seeing patterns in the intervention and not the control group. Overall, the amount of mindfulness practice reported by participants was lower than expected despite efforts to make guided exercises available, convenient, and brief. Future iterations of the treatment could make more specific recommendations regarding a “dose” of meditation expected to have an impact (rather than allowing participants to select goals with minimal guidance). Other limitations include a sample that was 92% women, limiting generalizability to men; no longer term follow-up that might allow us to see differences in weight loss maintenance; no administration of the emotional eating screening measure at follow up; and no assessment of mindfulness activities in the control group.
Finally, we were limited to self-reported weight, which is an imprecise outcome measure. Weighing participants in person is difficult in a phone-based study of participant and we attempted to use wireless scale data as a more objective measurement. Participants struggled with the technology, however, and rates of connecting the scale to the website were low. Future studies should look at methods to overcome this limitation, including simpler scales or weighing participants at local sites.
In sum, this pilot study shows that mindfulness and mindful eating training can be integrated into a phone-based weight loss program without any adverse impact on treatment satisfaction, engagement, or weight loss outcomes, and with improvements in mindful eating, binge eating, anxiety, and measures of mindfulness and that health coaches can be trained to deliver mindfulness interventions. Anecdotally, we note wide variation in compliance with mindfulness practice, although our exploratory analysis did not yield insight as to what qualities might predict response. Future research with larger samples could investigate who might benefit more from a cognitive behavioral approach versus a mindfulness approach. Further work is certainly needed to examine the potential for mindfulness to have a delayed impact on weight loss and maintenance as postulated by others.9, 37
CONCLUSIONS
Mindfulness can be integrated into phone-based behavioral weight loss program and delivered by health coaches and did not negatively impact treatment engagement, satisfaction or weight loss. Improvements in binge eating and .mindful eating were related to more weight loss. A minority of participants complied with mindfulness practice recommendations despite efforts to make practice easy to access, simple, and brief. More research is needed to determine who will benefit from an acceptance-based approach to weight loss.
Figure 1.
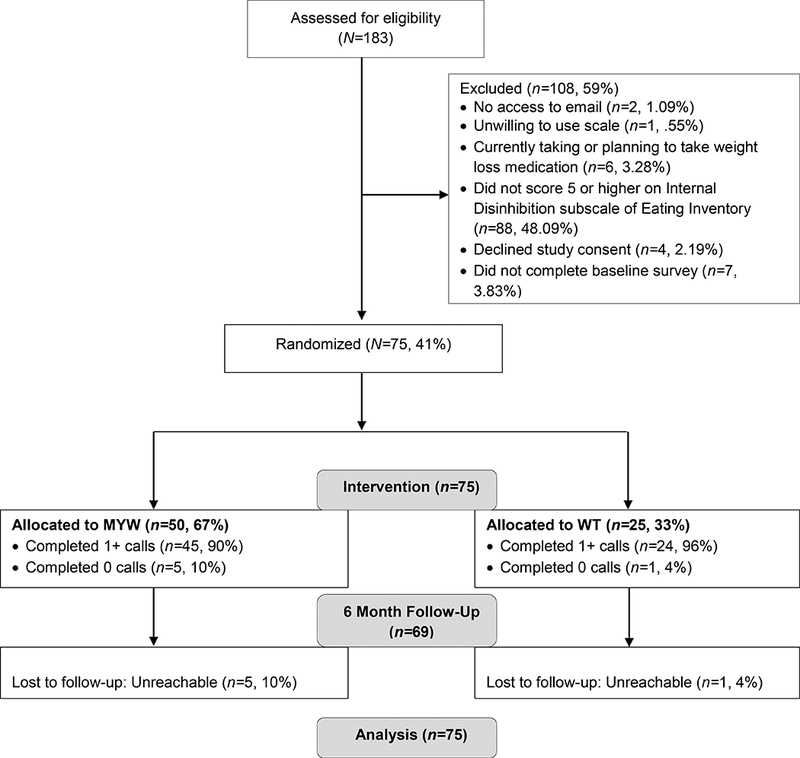
Consort Diagram
References
- 1.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. TRends in obesity among adults in the united states, 2005 to 2014. JAMA. 2016;315(21):2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2014;2(10):801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacLean PS, Wing RR, Davidson T, et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obesity (Silver Spring). 2015;23(1):7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125(9):1157–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lillis J, Niemeier HM, Ross KM, et al. Weight loss intervention for individuals with high internal disinhibition: design of the Acceptance Based Behavioral Intervention (ABBI) randomized controlled trial. BMC Psychology. 2015;3(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity (Silver Spring). 2007;15(10):2485–2494. [DOI] [PubMed] [Google Scholar]
- 8.Wilkinson LL, Rowe AC, Bishop RJ, Brunstrom JM. Attachment anxiety, disinhibited eating, and body mass index in adulthood. Int J Obes (Lond). 2010;34(9):1442–1445. [DOI] [PubMed] [Google Scholar]
- 9.Butryn ML, Thomas JG, Lowe MR. Reductions in internal disinhibition during weight loss predict better weight loss maintenance. Obesity (Silver Spring). 2009;17(5):1101–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stice E, Agras WS, Telch CF, Halmi KA, Mitchell JE, Wilson T. Subtyping binge eating-disordered women along dieting and negative affect dimensions. Int J Eat Disord. 2001;30(1):11–27. [DOI] [PubMed] [Google Scholar]
- 11.Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experimental avoidance and behavioral disorders: a functional dimensional approach to diagnosis and treatment. J Consult Clin Psychol. 1996;64(6):1152–1168. [DOI] [PubMed] [Google Scholar]
- 12.Niemeier HM, Leahey T, Palm Reed K, Brown RA, Wing RR. An acceptance-based behavioral intervention for weight loss: a pilot study. Behav Ther. 2012;43(2):427–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mendes AL, Ferreira C, Marta-Simoes J. Experiential avoidance versus decentering abilities: the role of different emotional processes on disordered eating. Eat Weight Disord. 2016. [DOI] [PubMed] [Google Scholar]
- 14.Rosenbaum DL, White KS. Does cognitive avoidance mediate the relation of anxiety and binge eating? Eat Weight Disord. 2016. [DOI] [PubMed] [Google Scholar]
- 15.Braden A, Flatt SW, Boutelle KN, Strong D, Sherwood NE, Rock CL. Emotional eating is associated with weight loss success among adults enrolled in a weight loss program. Journal of Behavioral Medicine. 2016;39(4):727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mason AE, Epel ES, Kristeller J, et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. J Behav Med. 2016;39(2):201–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung S, Zhu S, Friedmann E, et al. Weight loss with mindful eating in African American women following treatment for breast cancer: a longitudinal study. Support Care Cancer. 2016;24(4):1875–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6Suppl 2:51s–209s. [PubMed] [Google Scholar]
- 19.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–1124. [DOI] [PubMed] [Google Scholar]
- 20.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. [DOI] [PubMed] [Google Scholar]
- 21.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. [DOI] [PubMed] [Google Scholar]
- 22.Duarte C, Pinto-Gouveia J, Ferreira C. Expanding binge eating assessment: Validity and screening value of the Binge Eating Scale in women from the general population. Eat Behav. 2015;18:41–47. [DOI] [PubMed] [Google Scholar]
- 23.Framson C, Kristal AR, Schenk JM, Littman AJ, Zeliadt S, Benitez D. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009;109(8):1439–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warttig SL, Forshaw MJ, South J, White AK. New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). J Health Psychol. 2013;18(12):1617–1628. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 26.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med. 2009;37(1):58–69. [DOI] [PubMed] [Google Scholar]
- 27.Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308–320. [DOI] [PubMed] [Google Scholar]
- 28.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. [DOI] [PubMed] [Google Scholar]
- 29.Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. [DOI] [PubMed] [Google Scholar]
- 31.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? J Consult Clin Psychol. 1999;67(2):177–185. [DOI] [PubMed] [Google Scholar]
- 32.Daubenmier J, Moran PJ, Kristeller J, et al. Effects of a mindfulness-based weight loss intervention in adults with obesity: A randomized clinical trial. Obesity (Silver Spring). 2016;24(4):794–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Godfrey KM, Gallo LC, Afari N. Mindfulness-based interventions for binge eating: a systematic review and meta-analysis. J Behav Med. 2015;38(2):348–362. [DOI] [PubMed] [Google Scholar]
- 34.Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014;15(2):197–204. [DOI] [PubMed] [Google Scholar]
- 35.Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med. 2015;77(1):59–67. [DOI] [PubMed] [Google Scholar]
- 36.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barnes RD, Tantleff-Dunn S. A preliminary investigation of sex differences and the mediational role of food thought suppression in the relationship between stress and weight cycling. Eat Weight Disord. 2010;15(4):e265–269. [DOI] [PubMed] [Google Scholar]


