Abstract
Presentation and mortality of coronary artery disease (CAD) substantially differs in both sexes. Most of the existing data analyzing sex differences is older than 10 years and mostly was retrieved in clinical trials, which are potentially structured with a bias against the inclusion of women, leading to a potential selection-bias. Meanwhile, with better diagnostic and therapeutic options, actual data analyzing sex differences in emergency CAD patients is rare.
Data on all emergency case numbers with CAD diagnosis in Germany 2017 was retrieved from the German Institute for Medical Documentation and Information. DRG, OPS, and ICD codes were used to determine comorbidities, in-hospital course, and outcome. Competing risk regression analysis for in-hospital mortality was performed analyzing age, European System for Cardiac Operative Risk Evaluation (EuroSCORE), severity of CAD, clinical presentation type and sex.
264,742 patients were included. Female patients were older and had more comorbidities. Three-vessel CAD was significantly less present in female patients (36.5% vs 47.5%; P < .001). After adjusting for age, EuroSCORE and severity of CAD, female sex was an independent predictor of lower in-hospital mortality (subdistribution hazard ratio [sHR] 0.94, 95% CI: 0.90–0.98, P = .002) in the whole cohort and in non-ST-segment elevation myocardial infarction (NSTEMI) patients (sHR 0.85, 95% CI: 0.79–0.92, P < .001), whereas in ST-segment elevation myocardial infarction (STEMI) patients, female sex was associated with a higher in-hospital mortality (sHR 1.07, 95% CI: 1.01–1.14, P = .029).
In all patients admitted as emergency with CAD diagnosis and in all NSTEMI patients, female sex is protective, whereas in STEMI patients, females show a higher in-hospital mortality risk.
Keywords: acute coronary syndrome, coronary artery disease, emergency, female, outcome, sex
1. Introduction
Presentation and mortality of coronary artery disease (CAD) substantially differs in male and female patients. This obvious distinction even leads to periodic publications of scientific statements concerning those differences.[1] Although cardiovascular mortality in women decreased rapidly in the last twenty years, the mortality for women with acute coronary syndrome is higher than for men.[1–6] Additionally, while mortality decreased in all age groups for men, mortality increased in women younger than 55 years.[7] The declining mortality in the whole female cohort might be attributed to increased awareness and greater focus on sex differences in CAD patients.[1] Nevertheless, women still have a worse outcome than men which can be explained by many different factors, including biological differences, but also delays in presentation, diagnosis and treatment as well as insufficient gender-specific studies.[8]
In this study we analyzed emergency CAD patients receiving coronary angiography to detect whether differences in in-hospital mortality still exist and whether these differences are independent of age and comorbidities.
2. Methods
2.1. Study design
Data on all emergency case numbers receiving coronary angiography with CAD diagnosis in Germany 2017 was retrieved from the German Institute for Medical Documentation and Information (Deutsches Institut für Medizinische Dokumentation und Information, DIMDI; Cologne, Germany; http://www.dimdi.de). DRG-, OPS, and ICD codes were used to determine comorbidities, in-hospital course, and outcome.
In this study, the researchers had no direct access to the data of individual patients - only to the fully anonymized, summarized results provided by the Research Data Center. Approval by an ethics committee and informed consent were therefore not required under German law.
2.2. Data acquisition
German hospitals transfer patient data (ICD and DRG codes) of all interventions to the Hospital Remuneration System (InEK), as required by the German Institute for Medical Documentation and Information. The diagnoses and procedures retrieved were coded according to the International Statistical Classification of Diseases (ICD-10-GM) and Operation and Procedure Classification (OPS). The strategy used to determine comorbidities and outcomes has been described previously.[9] The logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) was calculated using the available information (admission status, ICD codes of comorbidities obtained from the Federal Bureau of Statistics), but critical preoperative state and left ventricular function were unavailable and were thus assumed to be inconspicuous, that is, no critical preoperative state and no left ventricular dysfunction. We therefore calculated a best-case scenario for the EuroSCORE. We used the current anamnestic or acute distinctive codes for all other comorbidities and complications. OPS and ICD codes were discussed in greater detail previously.[10] In total we analyzed 264,742 case numbers. These are not exclusive patient- but case-based records, meaning that a given patient may have experienced multiple admissions and procedures.
2.3. Bias
The administrative data we relied on is of high quality and completeness, since coding is crucial for the financial health of clinics and hospitals. Nevertheless, since the database is a registry, the possibility of reporting bias cannot be excluded. The large sample size may reduce this reporting bias.
2.4. Statistical analysis
First, we compared female and male patients concerning their baseline characteristics. Then we analyzed type of CAD (one-vessel-disease, two-vessel-disease, three-vessel disease, left main artery stenosis) and clinical presentation: ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI), unstable angina pectoris and stable angina pectoris, in absolute numbers and their impact on mortality in both sexes. We then analyzed the age and comorbidity independent influence on in-hospital mortality of these variables by adding age and EuroSCORE in a competing risk regression analysis. Previous coronary artery bypass graft (CABG) and previous cardiac surgery were additionally added. We performed this analysis 4 times, 1 time for all patients, 1 time for STEMI patients, 1 time for NSTEMI patients and 1 time for patients with unstable angina pectoris. Data are given as n (%), mean ± standard deviation or subdistribution hazard ratio (sHR) with 95% confidence interval (CI) if not stated otherwise. Differences were assessed by Chi-Squared test (or Fisher exact test if needed) for qualitative variables, and Student t test for quantitative variables. Cumulative incidences of mortality were calculated using competing risk regression (Fine and Gray method) with discharge alive as a competing event. All analyses were carried out using Stata 14 (Stata Corp, College Station, Texas, USA) and Prism (version 8, GraphPad Software, San Diego, USA).
3. Results
3.1. Study population
264,742 emergency case numbers with CAD diagnosis receiving coronary angiography were included. Of these, 18.8% presented with STEMI, 29.8% with NSTEMI and 15.3% with unstable angina pectoris.
Among all patients, 79,342 patients (30.0%) were female. Women were older (73.2 ± 11.0 vs 68.0 ± 11.9; P < .001). Prevalence of hypertension, pulmonary hypertension, chronic kidney disease (GFR <30 mL/min), atrial fibrillation and diabetes was higher in women. Men had a higher prevalence of prior myocardial infarction and previous CABG. Further baseline characteristics are shown on Table 1.
Table 1.
Baseline characteristics.
| Baseline characteristics | All patients (N = 264,742) | Male (N = 185,384) | Female (N = 79,342) | P value |
| Age in y, mean / SD | 69.56 | 68.0 ± 11.9 | 73.2 ± 11.0 | <.001 |
| Logistic EuroSCORE, mean / SD | 10.99 | 9.4 ± 8.8 | 14.7 ± 10.8 | <.001 |
| NYHA II | 8.40% | 8.49% | 8.19% | .012 |
| NYHA III/IV | 19.55% | 18.97% | 20.90% | <.001 |
| Hypertension | 58.01% | 57.90% | 58.28% | <.001 |
| Myocardial infarct less than 4m ago | 1.43% | 1.50% | 1.28% | <.001 |
| Myocardial infarct less than 1y ago | 1.26% | 1.30% | 1.16% | .002 |
| Myocardial infarct >1y ago | 8.92% | 9.76% | 6.94% | <.001 |
| Previous CABG | 8.51% | 9.66% | 5.81% | <.001 |
| Previous cardiac surgery | 9.83% | 10.93% | 7.24% | <.001 |
| Atherosclerosis | 5.68% | 5.90% | 5.17% | <.001 |
| Carotid disease | 1.97% | 1.99% | 1.92% | .229 |
| COPD | 8.39% | 8.36% | 8.44% | .444 |
| Pulmonary hypertension | 5.05% | 4.39% | 6.58% | <.001 |
| Chronic kidney disease GFR <30 mL/min | 1.44% | 1.92% | 3.36% | <.001 |
| Atrial fibrillation | 2.35% | 20.61% | 23.44% | <.001 |
| Diabetes | 21.46% | 29.58% | 31.91% | <.001 |
3.2. Distribution of men and women in different manifestations of coronary artery disease
STEMI occurred slightly fewer in female patients (17.7% vs 19.3%; P < .001). Women had more often 1 vessel CAD (34.9% vs 25.0%; P < .001) and less often 3 vessel CAD than men (36.5% vs 47.5%; P < .001). Left main artery stenosis occurred less often in female patients (5.8% vs 7.7%, P < .001). Hospital mortality was significantly higher in women (4.7% vs 4.2%; P < .001) (Table 2).
Table 2.
Diagnosis and outcome.
| Diagnosis and outcome | All Patients (N = 264,742) | Male (N = 185,384) | Female (N = 79,342) | P value |
| 1-vessel CAD | 27.99% | 25.04% | 34.87% | <.001 |
| 2-vessel CAD | 28.05% | 27.68% | 28.91% | <.001 |
| 3-vessel CAD | 44.23% | 47.54% | 36.50% | <.001 |
| Left main artery stenosis | 7.08% | 7.65% | 5.77% | <.001 |
| Stable angina pectoris | 1.05% | 0.98% | 1.21% | <.001 |
| Unstable angina pectoris | 15.26% | 15.29% | 15.17% | .428 |
| Nstemi | 29.77% | 29.69% | 29.94% | .197 |
| Stemi | 18.83% | 19.31% | 17.71% | <.001 |
| In-stent stenosis | 4.36% | 4.75% | 3.47% | <.001 |
| Mortality | 4.33% | 4.16% | 4.74% | <.001 |
3.3. Risk factors for in-hospital mortality
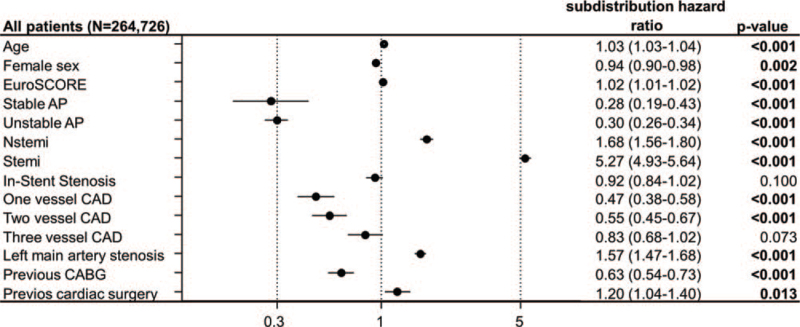
To adjust for the differences, as age, comorbidities and severity of CAD in both sexes, a competing risk regression analysis including age, clinical presentation, CAD severity and sex was performed. To adjust for comorbidities the EuroSCORE was included. Since previous CABG and previous cardiac surgery differentiated significantly, these variables were included as well. In the whole cohort, women had a significantly lower in-hospital mortality compared to men (sHR 0.94 (0.90 – 0.98); P = .002) (Fig. 1).
Figure 1.
Competing risk regression analysis for in-hospital mortality in all emergency patients with diagnosis of coronary artery disease. Figure shows competing risk regression analysis with subdistribution hazard ratio (95% confidence interval).
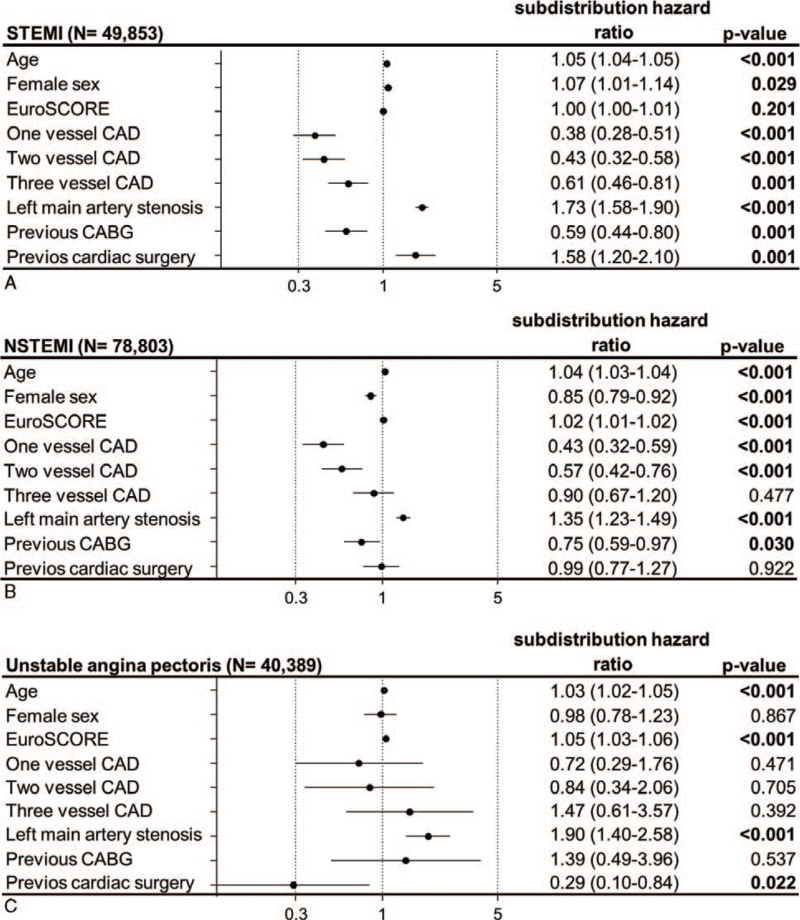
To identify sex differences in different clinical presentation types of CAD, the same competing risk regression analysis was performed in all subsets of acute coronary syndromes (ACS): STEMI, NSTEMI and unstable angina pectoris.
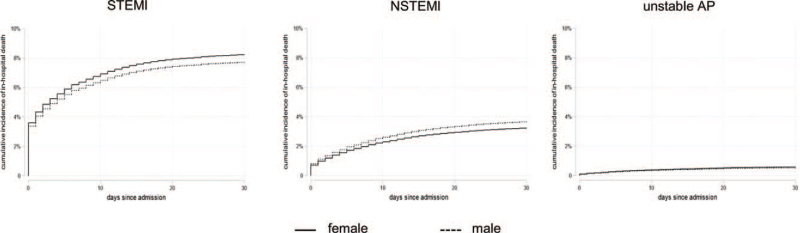
In the cohort of STEMI patients, women had a significantly higher in-hospital mortality risk than men (sHR 1.07 (1.01–1.14); P = .029), whereas in NSTEMI patients, women had a significantly lower in-hospital mortality risk (sHR 0.85 (0.79–0.92); P < .001) (Fig. 2A, B). No significant differences concerning men and women were seen in the group of patients presenting with unstable angina pectoris (Fig. 2C). Cumulative incidences of in-hospital mortality are shown in Figure 3.
Figure 2.
Competing risk analysis for in-hospital mortality in subsets of acute coronary syndromes: STEMI, NSTEMI and unstable angina pectoris. Figure shows competing risk regression analysis with subdistribution hazard ratio (95% confidence interval) in (A) STEMI, (B) NSTEMI and (C) unstable angina pectoris.
Figure 3.
Cumulative incidences for in-hospital mortality in patients with acute coronary syndromes.
4. Discussion
The present study is the largest analysis of patients with CAD including more than 260,000 emergency patients receiving coronary angiography in Germany. As main results, we show that, after adjustment for confounders, female sex is protective regarding the whole cohort of emergency patients, whereas in the STEMI group, female patients show a higher mortality risk.
Only ∼30 percent of all emergency patients with CAD were female and mortality in absolute numbers was clearly higher in male patients. This is in line with results from other studies.[2,11]
Additionally, we report higher one-vessel disease rates in women, while men have higher rates of three-vessel disease and thereby confirm the data of a previous meta-analysis of an ACS cohort.[11] Clinical presentation types of ACS show similar rates, while STEMI in women occurs slightly less often. Hochman et al also report lower rates of female STEMI patients compared to male STEMI patients.[12] However, these ratios may be biased, since women are less present in clinical trials. By reporting all registry data of the German Institute for Medical Documentation and Information we do not have any bias concerning this matter in our analysis.
By analyzing the baseline characteristics of all emergency patients with CAD, we show that emergency female patients with CAD are older and have more comorbidities (Prevalence of hypertension, pulmonary hypertension, chronic kidney disease, atrial fibrillation and diabetes). This is conclusive to a large meta-analysis analyzing sex differences in STEMI patients using data from 35 studies involving 18 555 women and 49 981 men with STEMI treated with primary PCI and other studies analyzing patients with acute coronary syndromes.[2,11–14] Prior research suggested that these baseline differences may contribute to the different mortality in both sexes which we also assume.[14] Indeed, mortality rates were higher in women as has been shown before in patients with ACS.[2] However, after adjustment, female sex showed a protective effect in the whole cohort.
In our NSTEMI analysis female sex seems to be protective whereas mortality in unstable angina pectoris seems to be sex independent. In contrast to STEMI patients, studies comparing adjusted mortality in patients with unstable angina or myocardial infarction without ST elevation are rarer and case numbers are lower. Some have demonstrated a gender independent mortality.[12,13] Most of the mentioned studies are older than ten years. Meanwhile, with better diagnostic and therapeutic options, we report actual data showing a lower in-hospital mortality risk for female patients after NSTEMI.
The mortality risk for women with STEMI is higher in our analysis. These findings are well in line with a meta-analysis showing higher short-term and long-term mortality in women when treated with PCI, which was declining after adjusting for comorbidities.[14]
So, why is in-hospital mortality higher in female STEMI but not in other CAD presentation types? The first, and maybe the crucial hypothesis is, that women present later and incidence of presentation to a non–PCI capable hospital is higher, leading to a delayed time to PCI and prolonged ischemic time.[15,16] Considering that 30% of all women with myocardial infarction present without typical symptoms, this supports the point that STEMI in women is often missed preclinically.[15,17] While urgent recanalization is absolutely necessary in STEMI patients, it is not that strictly regulated and necessary in patients without ST-elevation, partly explaining the higher mortality risk in STEMI patients but not in other CAD presentation types. We therefore conclude that a myocardial infarction should always be considered in women with unclear symptoms and the indication for a 12-lead electrocardiogram should be made generously.
Another hypothesis is a different severity of CAD in both sexes. Berger et al. showed a protective effect of NSTEMI and unstable angina in female ACS patients compared to their male counterparts after adjustment. Interestingly, those differences disappeared when angiographic severity was included in their analysis suggesting that mortality is related to the difference in CAD severity among women and men.[11] By including the angiographic severity in our multivariate analysis, we cannot support this finding. The third hypothesis is a different pathophysiology and biology. While plaque erosion is more common in female patients, plaque rupture is more common in male patients.[18] Differences in angiogenesis and collateralization between both sexes may contribute, enhancing mortality in women with an abrupt coronary occlusion.[11,12,19]
Due to the retrospective nature of our study, we cannot fully explain the presented difference and are only hypothesising. Therefore, we report a differential mortality risk between the sexes depending on the clinical type of CAD presentation. Consequently, the different CAD presentation types should be evaluated separately and special attention should be paid to women with STEMI. Further research is needed to analyze which factors affect the differences in outcome.
4.1. Limitations
When discussing the presented results, some limitations have to be considered. One limitation is that the EuroSCORE is a score to predict the cardiac operative risk and is not simply a measurement of comorbidities. Additionally, some variables of the score were unknown. Therefore, a best-case scenario was calculated, which may have affected the results. Nevertheless, some relevant comorbidities (i.e., chronic obstructive pulmonary disease, peripheral artery disease, chronic kidney disease, pulmonary hypertension, neurological disease) are included and a higher EuroSCORE is associated with adverse cardiac events in patients receiving coronary angiography.[20] We therefore decided to include the EuroSCORE in our competing risk regression analysis for relative risk adjustment.
Additionally, analysis included emergency patients only, meaning that patients who were electively admitted to hospitals were not included in the analysis. However, we believe that the majority of patients with acute coronary syndrome, and in particular STEMI patients, were included in this study, as these patients are naturally admitted as emergencies. Because the database was a registry, we cannot exclude the possibility of reporting bias because diagnoses and procedures were coded by independent hospitals. This may have led to misclassification of ACS diagnoses and under- or over-reporting of comorbidities. However, the administrative data we relied on is of high quality and completeness, since such coding is crucial for the financial health of clinics and hospitals. Most of preanalytical data is conclusive to previous publications concerning incidence and ratios, showing the representativity of our study. Furthermore, we present retrospective data regarding only the in-hospital course. Unfortunately, we could not assess long-term follow-up data. Nevertheless, the big strength of our study is the huge sample size. We are able to present data from a nation-wide registry including more than 260,000 patients, all equally analyzed. Concerning the discussed publications, even the meta-analysis analyzing pooled data did not reach our sample size by far. For these meta-analyzes, a major source for information is the data derived from randomized clinical trials. Cardiovascular clinical trials often are structured with a bias against the inclusion of women leading to a potential selection-bias. For example, in a pooled analysis of patients with non-ST-segment elevation ACS, only 29% of all patients were female.[21] We do not assume a selection bias in our analysis of a nation-wide registry and therefore present actual “real world data”.
5. Conclusion
In emergency patients, after adjusting for age, CAD severity and EuroSCORE, risk of in-hospital mortality is lower for women with NSTEMI than for men, whereas risk of in-hospital mortality is higher for women with STEMI than for men. It remains unclear if this difference is a difference in biology or can be explained by different (pre-) clinical treatment in our health care system. Further research is needed to analyze which factors affect the differences in outcome.
Author contributions
Conceptualization: Markus Jäckel, Klaus Kaier, Peter Stachon.
Data curation: Markus Jäckel, Katrin Roth, Dawid Leander Staudacher.
Formal analysis: Markus Jäckel, Klaus Kaier, Jonathan Rilinger, Dennis Wolf, Alexander Peikert, Dawid Leander Staudacher, Manfred Zehender, Christoph Bode, Constantin Von Zur Mühlen, Peter Stachon.
Investigation: Vera Oettinger.
Methodology: Klaus Kaier, Dennis Wolf, Alexander Peikert, Dawid Leander Staudacher, Peter Stachon.
Project administration: Markus Jäckel, Christoph Bode, Peter Stachon.
Software: Klaus Kaier, Jonathan Rilinger.
Supervision: Dennis Wolf, Manfred Zehender, Christoph Bode, Constantin von zur Mühlen, Peter Stachon.
Validation: Markus Jäckel, Klaus Kaier, Alexander Peikert, Katrin Roth, Vera Oettinger, Manfred Zehender, Christoph Bode, Constantin Von Zur Mühlen, Peter Stachon.
Visualization: Markus Jäckel, Dawid Leander Staudacher, Peter Stachon.
Writing – original draft: Markus Jäckel.
Writing – review & editing: Klaus Kaier, Jonathan Rilinger, Dennis Wolf, Alexander Peikert, Katrin Roth, Vera Oettinger, Dawid Leander Staudacher, Manfred Zehender, Christoph Bode, Constantin Von Zur Mühlen, Peter Stachon.
Footnotes
Abbreviations: CABG = coronary artery bypass graft, CAD = coronary artery disease, EuroSCORE = European System for Cardiac Operative Risk Evaluation, NSTEMI = non-ST-segment elevation myocardial infarction, sHR = subdistribution hazard ratio, STEMI = ST-segment elevation myocardial infarction.
How to cite this article: Jäckel M, Kaier K, Rilinger J, Wolf D, Peikert A, Roth K, Oettinger V, Dawid Leander S, Zehender M, Bode C, Constantin VZM, Stachon P. Outcomes of female and male patients suffering from coronary artery disease: a nation-wide registry of patients admitted as emergency. Medicine. 2021;100:38(e27298).
The article processing charge was funded by the Baden-Wuerttemberg Ministry of Science, Research and Art and the University of Freiburg in the funding programme Open Access Publishing.
The authors have no conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Mehta LS, Beckie TM, DeVon HA, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation 2016;133:916–47. [DOI] [PubMed] [Google Scholar]
- [2].Neumann JT, Goßling A, Sörensen NA, Blankenberg S, Magnussen C, Westermann D. Sex-specific outcomes in patients with acute coronary syndrome. J Clin Med 2020;9: doi:10.3390/jcm9072124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Puymirat E, Simon T, Steg PG, et al. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA 2012;308:998–1006. [DOI] [PubMed] [Google Scholar]
- [4].Leurent G, Garlantézec R, Auffret V, et al. Gender differences in presentation, management and inhospital outcome in patients with ST-segment elevation myocardial infarction: data from 5000 patients included in the ORBI prospective French regional registry. Arch Cardiovasc Dis 2014;107:291–8. [DOI] [PubMed] [Google Scholar]
- [5].Gabet A, Danchin N, Juillière Y, Olié V. Acute coronary syndrome in women: rising hospitalizations in middle-aged French women, 2004-14. Eur Heart J 2017;38:1060–5. [DOI] [PubMed] [Google Scholar]
- [6].Heer T, Hochadel M, Schmidt K, et al. Sex differences in percutaneous coronary intervention-insights from the coronary angiography and PCI Registry of the German Society of Cardiology. J Am Heart Assoc 2017;6: doi:10.1161/JAHA.116.004972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol 2007;50:2128–32. [DOI] [PubMed] [Google Scholar]
- [8].Davis E, Gorog DA, Rihal C, Prasad A, Srinivasan M. “Mind the gap” acute coronary syndrome in women: a contemporary review of current clinical evidence. Int J Cardiol 2017;227:840–9. [DOI] [PubMed] [Google Scholar]
- [9].Reinöhl J, Reinecke H, Zehender M. Transcatheter aortic-valve replacement in clinical practice. N Engl J Med 2016;374:1691–2. [DOI] [PubMed] [Google Scholar]
- [10].Reinöhl J, Kaier K, Reinecke H, et al. Effect of availability of transcatheter aortic-valve replacement on clinical practice. N Engl J Med 2015;373:2438–47. [DOI] [PubMed] [Google Scholar]
- [11].Berger JS, Elliott L, Gallup D, et al. Sex differences in mortality following acute coronary syndromes. JAMA 2009;302:874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hochman JS, Tamis JE, Thompson TD, et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global use of strategies to open occluded coronary arteries in acute coronary syndromes IIb investigators. N Engl J Med 1999;341:226–32. [DOI] [PubMed] [Google Scholar]
- [13].Hochman JS, McCabe CH, Stone PH, et al. Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI IIIB. TIMI investigators. thrombolysis in myocardial infarction. J Am Coll Cardiol 1997;30:141–8. [DOI] [PubMed] [Google Scholar]
- [14].Pancholy SB, Shantha GPS, Patel T, Cheskin LJ. Sex differences in short-term and long-term all-cause mortality among patients with ST-segment elevation myocardial infarction treated by primary percutaneous intervention: a meta-analysis. JAMA Intern Med 2014;174:1822–30. [DOI] [PubMed] [Google Scholar]
- [15].Mahmoud KD, Gu YL, Nijsten MW, et al. Interhospital transfer due to failed prehospital diagnosis for primary percutaneous coronary intervention: an observational study on incidence, predictors, and clinical impact. Eur Heart J Acute Cardiovasc Care 2013;2:166–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Radovanovic D, Nallamothu BK, Seifert B, et al. Temporal trends in treatment of ST-elevation myocardial infarction among men and women in Switzerland between 1997 and 2011. Eur Heart J Acute Cardiovasc Care 2012;1:183–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest 2004;126:461–9. [DOI] [PubMed] [Google Scholar]
- [18].Arbustini E, Dal Bello B, Morbini P, et al. Plaque erosion is a major substrate for coronary thrombosis in acute myocardial infarction. Heart 1999;82:269–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Johansson S, Bergstrand R, Schlossman D, Selin K, Vedin A, Wilhelmsson C. Sex differences in cardioangiographic findings after myocardial infarction. Eur Heart J 1984;5:374–81. [DOI] [PubMed] [Google Scholar]
- [20].Watanabe Y, Mitomo S, Demir OM, et al. Clinical outcomes of dialysis patients treated with drug-eluting stent for left main distal bifurcation lesions. Cardiorenal Med 2021;11:99–108. [DOI] [PubMed] [Google Scholar]
- [21].Sarma AA, Braunwald E, Cannon CP, et al. Outcomes of women compared with men after non-st-segment elevation acute coronary syndromes. J Am Coll Cardiol 2019;74:3013–22. [DOI] [PubMed] [Google Scholar]