Abstract
Objective:
The aim of this study was to determine the effect of empowerment-based interventions on glucose metabolism control and psychosocial self-efficacy in people with type 2 diabetes mellitus (T2DM).
Methods:
The Cochrane Library, Embase, PubMed, and Web of Science electronic databases were searched up to 22 February 2021 for randomized controlled trials (RCTs) that evaluated the effectiveness of empowerment-based intervention versus conventional treatment in type 2 diabetes cases. At least two investigators independently screened the literature, extracted data and evaluated the methodological quality. We calculated the pooled effect size using the mean difference (MD) or standard mean difference (SMD) with 95% confidence intervals (CIs) through RevMan V 5.4.1.
Results:
Fifteen randomized controlled trials (RCTs) were eligible for inclusion in the present study. A total of 2344 adults (1128 in the intervention groups and 1216 in the control) were covered. Five of these studies involved 671 cases of psychosocial self-efficacy, and 4 studies included 622 cases of diabetes knowledge. The meta-analysis showed that compared to routine care, empowerment-based intervention was associated with reduced glycated hemoglobin levels (SMD −0.20; 95% CI −0.31 to −0.08; Z = 3.40, P < .001, I2 = 42%), increased diabetes empowerment scores (SMD 0.24; 95% CI 0.10–0.37; Z = 3.42, P < .001, I2 = 0%), and increased diabetes knowledge scores (SMD 0.96; 95% CI 0.55–1.36; Z = 4.61, P < .001, I2 = 80%).
Conclusions:
Empowerment-based intervention in adults with T2DM results in improvements in glycated hemoglobin, psychosocial self-efficacy and diabetes knowledge.
Keywords: empowerment, glycated hemoglobin, meta-analysis, self-efficacy, systematic review, type 2 diabetes mellitus
1. Introduction
Type 2 diabetes mellitus (T2DM) is characterized by defects in both insulin secretion and insulin action, leading to high blood glucose levels. Long-term poor glycemic control can lead to dysfunction and failure of the eyes, nerves, heart, kidneys and blood vessels, resulting in complications of diabetes.[1] In 2017, there were 451 million cases of diabetes mellitus worldwide (18–99 years of age). It is predicted that there will be 693 million adults with diabetes by 2045. The prevalence of T2DM is rapidly increasing worldwide, leading to increased health care costs and mortality and reduced quality of life.[2] Individuals with diabetes usually provide 95% or more of the daily care by themselves.[3] Hence, diabetes education is a fundamental prerequisite for self-management.
Traditional diabetes education focuses on providing patients with the knowledge and skills to adhere to the treatment recommendations of health care professionals, and the educational goal is patient metabolic control and compliance. Care providers of diabetes education acted as experts and had full responsibility for patient care. The “compliance” strategy makes patients feel powerless during their diabetes control.[4] The traditional didactic approach is health care provider-centered, which determines the content of the diabetes education. Conventional compliance-based diabetes education has not been found to be an effective approach to help diabetic patients manage their self-care, and it was an inappropriate conceptual structure for the practice and assessment of diabetes education.[5]
Anderson et al introduced an empowerment approach to diabetes education in the 1990s. They deemed that empowerment is a workable philosophy that leads to effective interventions for addressing the psychosocial components of living with diabetes.[3] Empowerment can be viewed as a process in which individuals gain the knowledge, skills, attitudes, and self-awareness necessary to influence their own behavior, thereby improving responsibility and autonomy and obtaining power to make informed decisions.[6] The empowerment approach emphasizes care that considers patients’ needs and that aims at behavior change. It requires a shift in roles from a provider-centered to a patient-centered approach.[7] The role of the care provider is to be a facilitator or collaborator, rather than an authority or directive, encouraging and assisting cases with diabetes to take control of their lives. Empowerment programs can be designed to follow the five-step empowerment model: problem definition; identification and handling of feelings; goal setting; elaboration of a self-care plan to achieve these goals; and evaluation of the experience and the plan.[8] Providers assist the participants identifying self-management problems and concerns, elicit participants’ goals and help participants to formulate their own action plans, to integrate new knowledge and skills in overcoming barriers, and to reflect on at the end of the empowerment process. Health care providers engaged in appropriate, natural dialog with patients about all aspects of self-management behavior. Open communication is essential for building equal partnerships between health care providers and patients. The patients feel free to share their experiences and opinions with educators.[9] The topics and content of each session varied based on the individual needs and the concerns of the participants.
Several studies have reported that empowerment-based education for individuals with T2DM can reduce the level of glycated hemoglobin (HbA1c) and improve patients’ self-awareness and control ability of the disease through psychological, habitual and behavioral changes.[1,3,9–15] However, other studies have not found the same results using an empowerment approach in T2DM.[7,8,16–19] There is considerable controversy regarding the effectiveness of empowerment-based interventions in T2DM. One previous meta-analysis suggested that there was significant evidence that indicated reduced HbA1c levels with group empowerment strategies in cases of type 1 and type 2 diabetes.[20] Another systematic review showed that individual empowerment strategies in cases with type 1 and type 2 diabetes were not effective in reducing HbA1c.[21] Instead, this study indicated that different forms of empowerment had different effects on patients with diabetes. However, systematic reviews and meta-analyses regarding the effectiveness of empowerment-based education interventions among patients with T2DM have not been reported. Hence, we performed a meta-analysis of randomized controlled trials (RCTs) to determine the effect of empowerment in T2DM cases.
2. Materials and methods
Present study was performed and reported in accordance with the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.[22]
2.1. Literature and search strategy
We performed a detailed search using the Cochrane Library, Embase, PubMed and Web of Science databases for reports of RCTs about empowerment in T2DM, which were published from the database inception up to February 22, 2021. The following search terms “type 2 diabetes mellitus,” “type 2 diabetes,” “type two diabetes,” “T2DM,” “DM2,” and “empowerment,” “empowerment-based,” “empowered,” “patient-centered” were combined with ORs. Additionally, the above search keywords of population and intervention were linked with AND. Reference lists from the relevant reviews and included studies were screened, and the authors were contacted for further information if necessary. All analyses were based on published studies; therefore, no informed consent or ethical approval was required.
2.2. Study Selection
The following inclusion criteria were predefined according to the PICOS acronym for the studies that were included in the present meta-analysis: P (Population): study population consisting of adult participants >18 years of age who were diagnosed with T2DM. I (Intervention): individual or collective empowerment strategies were performed for cases with 2TDM. Empowerment-based intervention was explicitly proposed, such as “empowerment-based, empowerment program, empowerment approach, empowerment strategy, empowerment model, and the theory of empowerment”. Diabetes empowerment processes included at least awareness, action and reflection phases. Health providers were specifically trained for patient empowerment strategies before the trial or had experience using an empowerment approach successfully in previous intervention studies to guarantee that facilitators would actually act in accordance with the empowerment philosophy. The empowerment intervention was delivered by a physician, nurse, dietitian, or certified diabetes educator. C (Comparison): the control group must have been given routine diabetes care or waiting list control. They regularly visited the primary care centers and conducted biochemical tests and examinations in accordance with regional diabetes guidelines and then received individual counseling and recommendations by physicians and nurses based on the results of the examinations, biochemical tests and their self-monitoring of blood glucose. Furthermore, a resource manual was given to the participants at the beginning of the course. The participants received collective diabetes health education lectures from diabetes educators according to the guidelines regarding diet, exercising, blood sugar control, foot care, and so on. Follow-up was also performed by telephone or home visit. O (Outcome): for evaluation outcomes, the primary outcome included at least glycated hemoglobin (HbA1c). S (Study design): the design of the study must be RCT. The exclusion criteria were as follows: “empowerment” was only as an outcome or as a measuring instrument, use of additional interventions offered by health professionals that could affect outcomes, and the original data from the article could not be converted or used.
Two investigators respectively reviewed the titles and abstracts of each record retrieved, and then, the full text of the remaining articles was reviewed based on eligibility criteria. Any disagreements between the 2 researchers were resolved by consensus with a third researcher if necessary.
2.3. Data extraction and quality assessment
Standard data extraction templates were adopted to extract data by 2 reviewers independently, with any discrepancy solved by consensus or the third reviewer. Since there was no evidence that blinding could reduce bias in the process of systematic reviews and meta-analysis, extraction was not blinded to the author or institution.[23] Data were abstracted on the studies, sample size, participant characteristics, empowerment-based intervention (eg, content and duration), outcome measures and main findings. The quality of the included RCTs was assessed by 2 researchers independently according to the Cochrane Collaboration's tool.
2.4. Outcome measures and data analysis
The outcomes were the changes in HbA1c, the scores of the diabetes empowerment scale and diabetes knowledge. Each study contributed only 1 outcome measure to each follow-up stratum, using the result with the longest follow-up duration if the study reported more than once regarding the scores of diabetes empowerment scale and diabetes knowledge, selecting HbA1c near 6 months of follow-up if there were multiple HbA1c follow-up results.
Statistical analysis was conducted with Review Manger (RevMan) software, version 5.4.1. The outcomes were analyzed as continuous variables and pooled by MD or SMD with 95% confidence interval (CI). Where outcomes were measured on different scales, SMD was combined. We extracted MD and standard deviations (SDs) between the intervention and control groups from each study. The heterogeneity among the included studies was tested using Cochran Q and I2 statistics. If P < .1 or I2 > 50%, the heterogeneity was considered to be statistically significant. The I2 values ranged from 0 to 100% (I2 = 0–25%, no heterogeneity; I2 = 25%–50%, moderate heterogeneity; I2 = 50%–75%, large heterogeneity; and I2 = 75%–100%, extreme heterogeneity).[24] If there was no heterogeneity (I2 ≦ 25%), a fixed-effects model was employed; otherwise, we adopted the random-effects model. Finding a P value <0.05 was considered to suggest statistical significance. Subgroup analysis was performed according to the patients’ follow-up duration (≦6 vs >6 months) to explore potential heterogeneity. Sensitivity analysis was conducted to evaluate the robustness of the findings for the meta-analysis by excluding 1 study at a time and calculating pooled estimates for the remaining studies. Specific for a single result with a cumulative count of >10 included studies, a funnel plot was generated to qualitatively check for publication bias.
3. Results
3.1. Study selection and characteristics
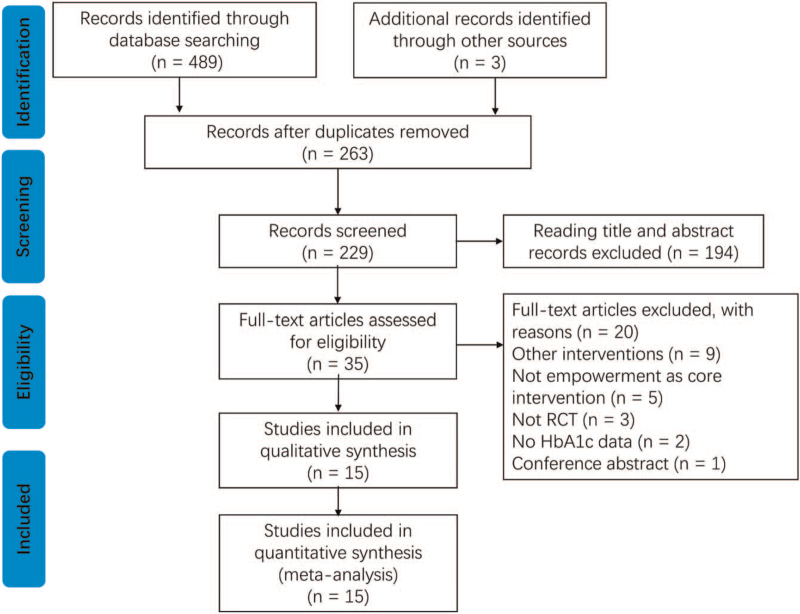
The study selection process is summarized in Figure 1. We initially identified 492 articles. A total of 229 articles were retained after eliminating duplicates by using the literature management software EndNoteX9. After exclusion of studies that did not fulfill the eligibility criteria by perusing the title and abstract, 35 remaining trials appeared to be relevant to the present meta-analysis. The full texts of 35 potential studies were checked, and we further excluded 20 articles because they did not satisfy the inclusion criteria: other interventions (n = 9), no empowerment as a core intervention (n = 5), no RCTs (n = 3), no results for HbA1c (n = 2), and conference abstracts (n = 1). Finally, 15 articles about RCTs with 2344 T2DM cases were included in the meta-analysis.
Figure 1.
Flow diagram of the literature selection procedure.
Table 1 demonstrates the characteristics of the included studies. They were published between 1995 and 2019. The articles were gathered from several countries: 4 in the United States[3,8,15,16]; 2 in the United Kingdom;[10,12] 2 in China[9,17]; 2 in Brazil[11,13]; 1 in Sweden[7]; 1 in Iceland[18]; 1 in Qatar[14]; 1 in Iran[1]; and 1 in Denmark.[19] The sample size of the included studies were in the range of 46 to 430 cases. Seven of the 15 studies had a sample size of >200 subjects. Fourteen studies reported a mean duration of diabetes, with an average course of disease ranging from 6 to 17 years. The average age of the participants in the presented studies ranged from 50 to 66 years. In this study, the duration of empowerment-based intervention ranged from 6 weeks to 12 months, and the follow-up ranged from 6 weeks to 12 months after the intervention.
Table 1.
Characteristics of randomized controlled trails in this meta-analysis.
| Study: author, year, country | Sample size (I/C) | Mean age (SD) | Duration of diabetes, y | Intervention/duration, mo | Indicator/ the assessment tool | Main findings |
| Anderson et al[3] (1995) USA | 22/23 | 50 | not described | I: 6-wk Empowerment Program. Six 2-h group sessions offered weekly. C: 6-wk Control Period/6 wks | HbA1c self-efficacy subscales DAS t0: Baseline t1: Follow-up, 6 wk | The intervention group showed a significant reduction in HbA1c levels, and gains over the control group on 4 of the eight self-efficacy subscales and 2 of the 5 diabetes attitude subscales. |
| Anderson et al[16] (2005) USA | 125/114 | 61.0 (11.4) | 8.5 (8.6) | I: 6-wk Empowerment Program. Six weekly 2-h group sessions. C: 6-wk Control period/6 wks | HbA1c, TC, SBP, DBP, DES t0: Baseline t1: Post, 6 wk | No significant difference in change in HbA1c was found between groups during the first 6 weeks. |
| Deakin et al[12] (2006) UK | 157/157 | I = 61.3 (9.7) C = 61.8 (11.0) | I = 6.7 (6.4) C = 6.7 (6.7) | I: Six weekly group sessions, each lasted 2 h of self-management education, based on theories of empowerment and discovery learning C: Routine care + diabetes education and review/6 wk | HbA1c, TC, SBP, DBP, HDL, LDL, BMI DES Diabetes knowledge score Self-care activity t0: Baseline t1: Follow-up, 4 mo t2: Follow-up, 14 mo | By 14 mo the X-PERT group compared with the control group showed significant improvements in the mean HbA1c, BMI, total cholesterol, self-empowerment, diabetes knowledge. |
| Adolfsson et al[7] (2007) Sweden | 42/46 | I = 62.4 (8.9) C = 63.7 (9.0) | I = 6.5 (3.9) C = 6.7 (4.2) | I: 4–5 Empowerment group education sessions, each lasted 2.5 h + routine diabetes care C: Routine diabetes care/not described | HbA1c, BMI diabetes knowledge self-efficacy satisfaction with daily life t0: Baseline t1: Follow-up, 12 mo | No significant differences were found in self-efficacy, BMI and HbA1c between the intervention and control group. |
| Cooper et al[10] (2008) UK | 23/36 30/36 | 59 | 6 | I: Empowerment-based educational system, sessions weekly for 8 wk lasting 2 h C: Routine diabetes care/8 wk | HbA1c, BMI self-care activities t0: Baseline t1: Follow-up, 6 mo t2: Follow-up, 12 mo | The educational program was associated with benefits in HbA1c levels at 6 mo follow-up compared to controls. |
| Anderson et al[25] (2009) USA | 156/154 | I = 55.5 (11.3) C = 55.7 (11.5) | I = 8.6 (8.1) C = 8.0 (7.8) | I: Empowerment-based Diabetes Self-Management Consultant (DSMC). C: Mailed metabolic Assessments Only (MAO)/not described | HbA1c DES-SF, PAID, PHQ-9, DSMC t0: Baseline t1: Follow-up, 24 mo | HbA1c values remained stable for the DSMC group but increased significantly for the MAO Group at the end of the 2-y trial. There were no significant between-group differences in any of the self-care behaviors. |
| Sigurdardottir et al[18] (2009) Iceland | 28/25 | I = 57.8 (10.9) C = 63.5 (9.3) | I = 9.7 (6.6) C = 7.6 (5.6) | I: Based on an empowerment approach, 1 individual session at baseline and telephone calls once a wk for the 5 following wk. C: Routine diabetes care/6 wk | HbA1c, BMI Diabetes Knowledge Test DES, PAID t0: Baseline t1: Follow-up, 3 mo t2: Follow-up, 6 mo | No statistically significant differences between groups were found in HbA1c, BMI, scores for empowerment, well-being and distress. |
| Spencer et al[15] (2011) USA | 72/92 | I = 50 (10.8) C = 55 (9.8) | I = 8 (6.5) C = 9 (9.8) | I: Using an empowerment-based approach, community health workers provided participants with diabetes self-management education and regular home visits, and accompanied them to a clinic visit. C: routine care/6 mo | HbA1c, BMI, SBP, DBP, LDL PAID, self-efficacy t0: Baseline t1: Post, 6 mo | Participants in the intervention group had a mean HbA1c value of 8.6% at baseline, which improved to a value of 7.8% at 6 mo. There was no change in mean HbA1c among the control group (8.5%). |
| Mohamed et al[14] (2013) Qatar | 215/215 | I = 52 (8.9) C = 55 (10.7) | I = 11.5 (9.0) C = 10.3 (8.4) | I: The intervention consisted of four educational sessions for each group of patients (10–20 patients per session), lasting for 3–4 h, based on theory of empowerment. C: Routine care/not described | HbA1c, TC, SBP, DBP, HDL, LDL, BMI, TG KAP t0: Baseline t1: Follow-up, 12 mo | After 12 mo participation in the intervention was shown to have led to a statistically significant reduction in HbA1c, BMI and blood pressure. The intervention group also had improvement in Diabetes knowledge, attitude and practice. |
| Chen et al[9] (2015) China | 36/36 | I = 62.12 (7.51) C = 61.72 (8.79) | I = 8.12 (3.25) C = 7.45 (3.83) | I: 3-mo empowerment program, a 5-step MAGIC empowerment program was developed. C: Routine care/3 mo | HbA1c DES, DQOL Diabetes Self-care Scale t0: Baseline t1: Post, 3 mo t2: Follow-up, 6 mo | The experimental group had significantly decreased HbA1c and improved self-care behaviors, self-efficacy, and quality of life at 3 mo after the end of the intervention. |
| Ebrahimi et al[1] (2016) Iran | 53/53 | I = 46.97 (5.54) C = 48.15 (6.52) | <5 y (%): 28/30.2; 5–10 y (%): 51/52.8; >10 y (%): 21/17 | I: Empowerment approach training. C: Routine care/8 wk | HbA1c, TC, HDL, LDL, TG t0: Baseline t1: Post, 3 mo | HbA1c and other metabolic indicators except for LDL showed significant differences in the experimental group compared to the control group. |
| Cortez et al[11] (2017) Brazil | 127/111 | I = 58 (9.2) C = 57.5 (9.7) | not described | I: Empowerment program based on a behavior change protocol. C: routine care/12 mo | HbA1c, TC, SBP, DBP, HDL, LDL, BMI, TG t0: Baseline t1: Follow-up, 12 mo | Levels of HbA1c and other metabolic indicators showed a significant difference in the experimental group compared to the control group. |
| Macedo et al[13] (2017) Brazil | 72/111 | I = 60.4 (8.0) C = 57.5 (9.7) | ≤5 y (%): 38.9/18.9; >5 y (%): 61.1/81.1 | I: Empowerment approach, based on the Behavior Change Protocol. Seven group meetings, each one lasting around 2 h. C: routine care /6 mo | HbA1c DES-SF t0: Baseline t1: Post, 6 mo | A statistically significant decrease in the value of HbA1c and an increase in the score of empowerment scale were found for participants in the intervention group. |
| Cheng et al[17] (2019) China | 121/121 | I = 56.13 (10.72) C = 53.91 (13.01) | I = 8.15 (5.91) C = 7.79 (6.19) | I: A 6-wk empowerment-based self-management program, grounded on the principles of the Empowerment Process Model. C: routine care/6 wk | HbA1c Self-management behavior t0: Baseline t1: Follow-up, 5 mo | Compared with the attention control group, the intervention group showed a nonsignificant HbA1c reduction. |
| Varming et al[19] (2019) Denmark | 49/48 | I = 63 (11) C = 66 (9) | I = 16 (7) C = 17 (8) | I: Four one-on-one and 1 telephone consultations in which the EMMA tools were applied. EMMA builds on the 5step empowerment model of goal setting. C: routine care/not described | HbA1c, SBP, DBP, BMI PAID, SDSCA t0: Baseline t1: Post, 3 mo t2: Follow-up, 6 mo | The intervention was not superior to usual care in terms of glycemic control. |
BMI = body mass index, C = control group, DAS = Diabetes Attitude Scale, DBP = diastolic blood pressure, DCP = Diabetes Care Profile, DES = Diabetes Empowerment Scale, DQOL = Diabetes Quality of Life, DSMC = Diabetes Self-Management Competence Questionnaire, HDL = High density lipoprotein, I = intervention group, KAP = Knowledge, Attitude, Practice questionnaire, LDL = low-density lipoprotein, PAID = problem areas in diabetes scale, PHQ-9 = Patient Health Questionnaire, SBP = systolic blood pressure, SDSCA = Summary of Diabetes Self-Care Activities, TC = total cholesterol, TG = triglycerides.
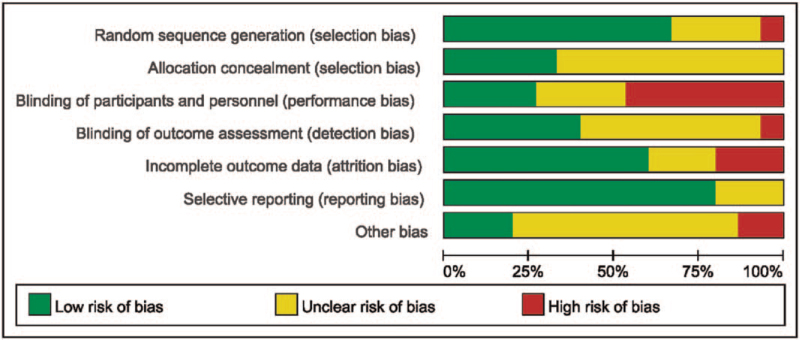
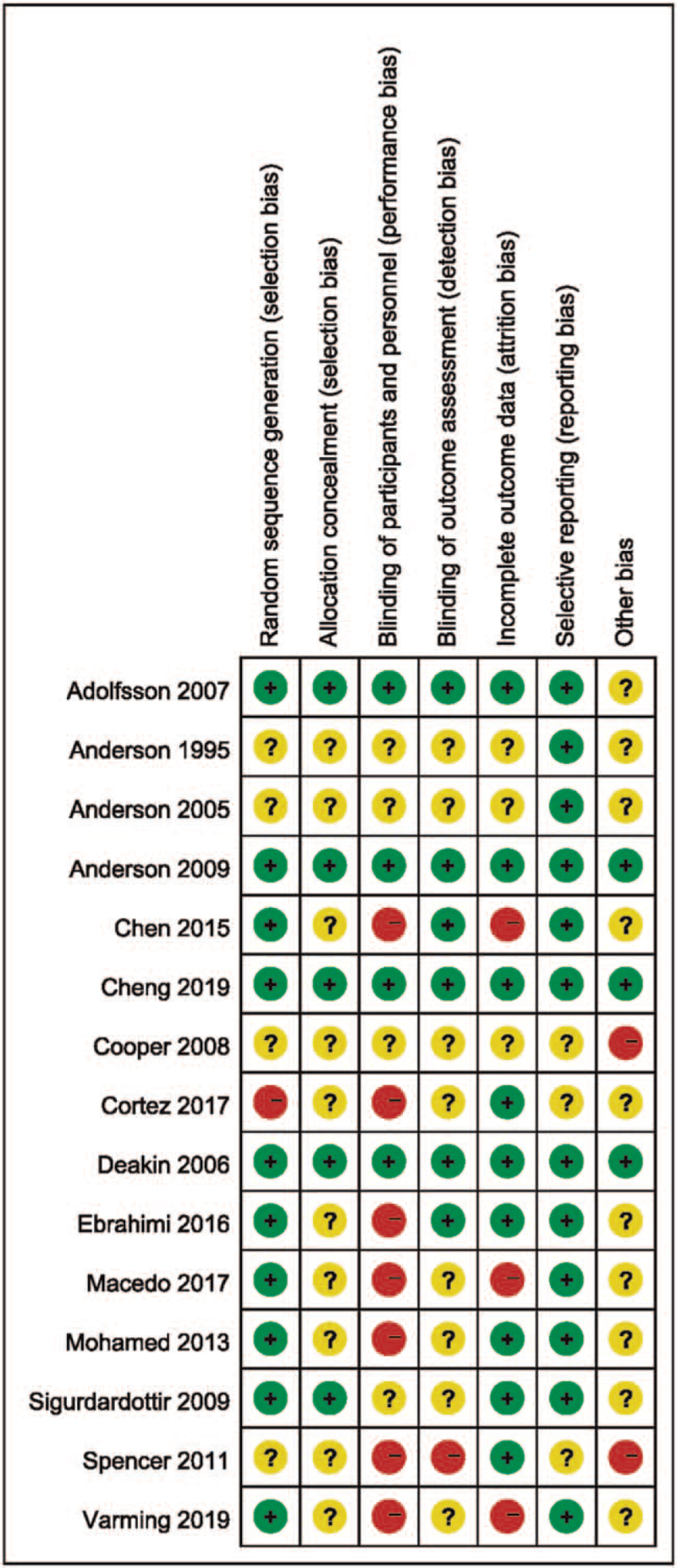
3.2. Quality assessment
All of the included RCTs reported the baseline condition of the patients, and the baselines were comparable across all included trials. Ten articles adequately described the random sequence generation.[1,7–9,12–14,17–19] Allocation was properly concealed in 5 studies,[7,8,12,17,18] and the other studies were unclear. Only 4 studies blinded the investigators, participants, and results analyzers.[7,8,12,17] Nine studies described the reason for incomplete outcome data and performed intent-to-treat analysis.[1,7,8,11,12,14,15,17,18] No other apparent risk of bias was found in any of the included studies. A summary of the detailed quality assessment results is shown in Figures 2 and 3.
Figure 2.
Risk of bias graph by percentage for fifteen included studies.
Figure 3.
Risk of bias summary (red, yellow and green solid circle represents high risk of bias, unclear risk of bias and low risk of bias respectively).
3.3. Results of meta-analysis
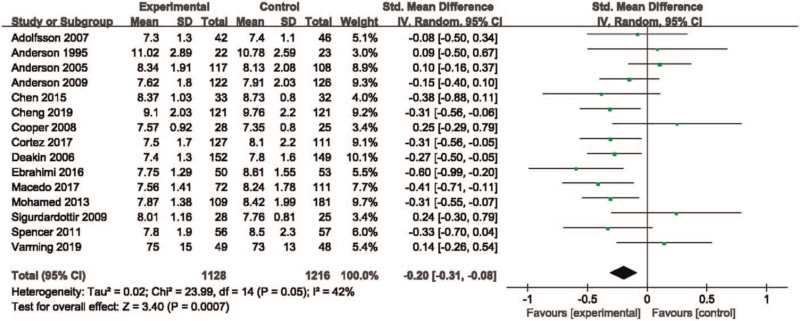
3.3.1. Effects of empowerment-based education on HbA1c level
All of the included studies,[1,3,7–19] including 2344 participants (1128 vs 1216), reported changes in HbA1c. We observed mild heterogeneity among the included studies (P = .05, I2 = 42%). Pooled results indicated a statistically significant reduction in HbA1c between the intervention group and the control group in the random-effects model (SMD −0.20; 95% CI, −0.31 to −0.08; Z = 3.40, P < .001, Fig. 4), favoring the intervention group. Subgroup analysis was performed according to the patients’ follow-up time (≦6 vs > 6 months), with the results that studies with a length of follow-up ≦6 months (SMD, −0.20; 95% CI −0.35 to −0.05; Z = 2.54, P = .01, I2 = 49%) and studies with a length of follow-up >6 months (SMD −0.26; 95% CI −0.41 to −0.10; Z = 3.18, P = .001, I2 = 44%). The pooled analyses of both short-term (≦6 months) and long-term (>6 months) follow-up showed significant improvement in HbA1c levels in the intervention group compared with routine care.
Figure 4.
Evaluation of HbA1c reduction after empowerment-based intervention in patients with type 2 diabetes compared with routine care.
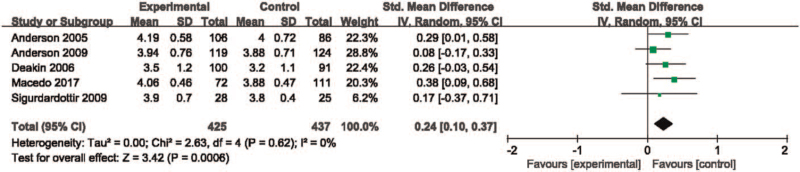
3.3.2. Effects of empowerment-based education on psychosocial self-efficacy
Five studies[8,12,13,16,18] with 671 (425 vs 437) subjects elucidated the psychosocial self-efficacy by the scores of Diabetes Empowerment Scales (DES). No heterogeneity was observed among the studies (P = .62, I2 = 0%). According to the result of the fixed-effect model analysis, the scores of patient empowerment improved significantly in the intervention group as compared with the control (SMD 0.24; 95% CI 0.10–0.37; Z = 3.42, P < .001, Fig. 5).
Figure 5.
Meta-analysis of the score of diabetes empowerment scale between the two groups.
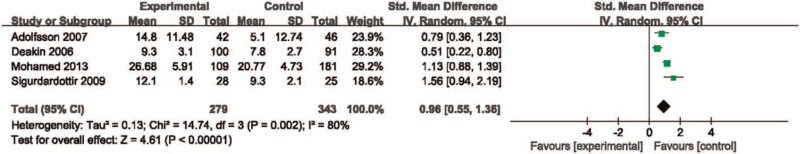
3.3.3. Effects of empowerment-based education on diabetes knowledge
Four studies[7,12,14,18] involving 622 (279 vs 343) cases provided the scores of diabetes knowledge after intervention. There was obvious heterogeneity across the studies (P = .002, I2 = 80%). Using a random-effect model for the analysis (SMD 0.96; 95% CI 0.55–1.36; Z = 4.61, P < .001, Fig. 6), which suggested that the score of diabetes knowledge was significantly higher in the intervention group than the control.
Figure 6.
Forest plot of meta-analysis of diabetes knowledge results.
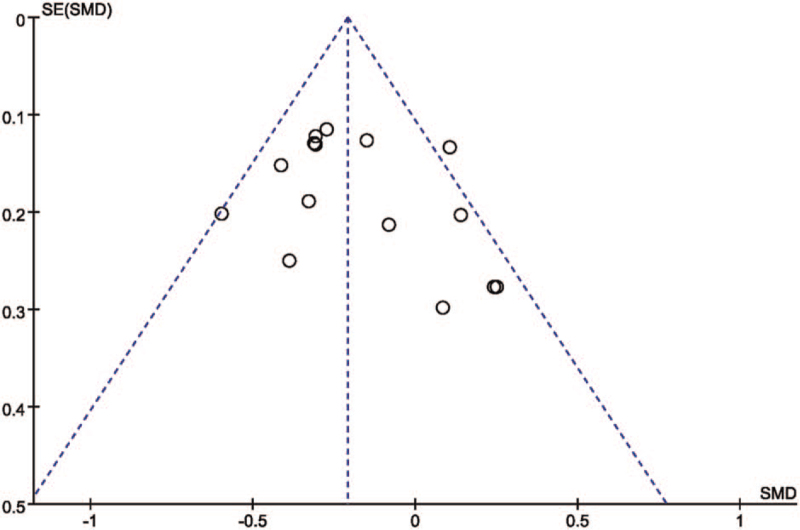
3.4. Sensitivity analysis and publication bias
We checked the robustness of the results by sensitivity analysis. In sensitivity analysis, omitting any single study, there were no significant changes in the pooled results of HbA1c levels, the scores of diabetes empowerment scale and diabetes knowledge scores. In the present meta-analysis, 15 studies reported the measurements of HbA1c. Thus, a funnel plot was generated to inspect potential publication bias, which showed that there was a slight publication bias based on the shape of funnel plot (Fig. 7).
Figure 7.
Funnel plot of the changes of HbA1c among the included studies.
4. Discussion
According to the results of the present meta-analysis, empowerment-based diabetes education can effectively reduce patients’ HbA1c levels and improve psychosocial self-efficacy as well as the diabetes knowledge required for self-management of the disease in T2DM compared with routine care. Any single study was removed, and the empowerment intervention effect on HbA1c levels, knowledge and empowerment were not significantly altered. This result indicated that the results of the present study were stable.
Previously, a systematic review of group-based empowerment strategies in cases with diabetes suggested that the intervention group showed an advantage of −0.26 in the pooled HbA1c versus the control group.[20] This result was consistent with our findings. Our meta-analysis revealed that the combined effect of empowerment-based intervention versus routine care on HbA1c was −0.20 (−0.31 to −0.08), which was in contrast with that reported in the meta-analysis of the effect of individual empowerment strategies on HbA1c in diabetic patients (MD −0.05; −0.19 to 0.09).[21] The inclusion criteria in the aforementioned 2 reviews were that “empowerment” was only a measuring instrument or an outcome, and most of the studies did not conduct empowerment-based education interventions. However, the intervention in the present study was based on empowerment theory, which emphasizes a collaborative approach to promoting self-directed behavior change in individuals.[25] A recent meta-analysis synthesized the effectiveness of theory-based self-management education for people with T2DM. Finally, the pooled main outcomes demonstrated significant improvements in HbA1c, diabetes knowledge, and self-efficacy.[26] This finding proves that theory-based interventions can produce more effects.
The interventions used in all of the included studies were based on the theory of empowerment, since most interventions that elaborated on how the intervention was conducted were grounded on the principles of empowerment. The main differences were the use of health education strategies, the contact frequency, the duration of each session, the duration of the intervention, and the number of cases per group. The interventions in 4 studies[3,10,12,16] were 6 to 8 weekly 2-hour group sessions for 6 to 8 weeks. A study's[7] intervention was 4 to 5 empowerment group education sessions, each lasting 2.5 hours, while the intervention in another study[14] was four educational sessions for each group (10–20 patients per group), lasting for 3 to 4 hours. One study[1] was a 5 to 7 weekly meeting, and each session lasted 60 to 90 minutes, with 10 patients per group. Only 1 study[15] was conducted in a community setting, and the intervention consisted of 11 2-hour group sessions held every 2 weeks, with each group consisting of 8 to 10 participants. Furthermore, only 2 studies[8,18] used one-to-one meetings, whereas the others used group sessions. Therefore, future studies should focus on the same empowerment intervention method.
The length of the follow-up period, the form and the frequency were different from each other. The frequency of follow-up was a monthly phone call in two studies,[8,16] once every 2 weeks in 1 study,[15] once a week in a study,[18] and 3 weekly telephone interviews in one study.[9] The length of the follow-up period was short term (≦6 months) in 9 studies,[1,3,9,13,15–19] and long term (> 6 months) in 6 studies.[7,8,10–12,14] According to the follow-up period, subgroup analysis was conducted for HbA1c. For diabetes knowledge and empowerment scores, fewer studies were included, and no subgroup analysis was performed. Moreover, variation in the timing of the follow-up measurements associated with the end of treatment could have introduced heterogeneity. However, according to the results of subgroup analysis based on the follow-up time, the effect of empowerment on HbA1c was not significantly related to the follow-up time, and thus, time to follow-up was ruled out as a significant source of variance.
HbA1c is the primary relevant parameter in patients with diabetes, since it is the gold standard for metabolic control of blood glucose, capturing the average glycemia during the previous 6 to 8 weeks.[27] Each 1% reduction in HbA1c levels is associated with reductions in the risk of 21% for diabetes-related death and 37% for microvascular complications over 10 years.[28] The ideal HbA1c level can be achieved through a healthy diet, physical activity, health education and self-monitoring of blood sugar, not solely medication.[29] Therefore, we conceived that if individuals were able to reduce HbA1c levels, it means that the empowerment-based intervention was effective for the management of T2DM. In the present meta-analysis, the outcomes of all of the included studies must include measurements of HbA1c. Five studies[8,12,13,16,18] measured diabetes-related psychosocial self-efficacy using the Diabetes Empowerment Scale-Short Form (DES-SF) or DES.[30,31] Diabetes knowledge was evaluated by the Diabetes Knowledge Test (DKT) or Knowledge, Attitude, Practice (KAP) Questionnaire in four studies.[7,12,14,18] The pooled analysis demonstrated that the empowerment-based intervention could effectively improve metabolic aspects, diabetes knowledge, and psychosocial outcomes. Based on the results of the present study, it can be inferred that the diabetes empowerment approach has considerable potential for the effective management and control of T2DM by enhancing patients’ ability to participate in disease management and thereby reducing HbA1c levels. The empowerment approach is designed to identify and promote an individual's strengths and ability to make informed choices that are tailored to the individual's needs as well as reflect their life experience in the management of T2DM.[32] The improvement in self-efficacy in the intervention group could be due to their repeated success in problem solving processes, which then increases their confidence, because mastery of an experience increases psychosocial self-efficacy.[33,34] Increased knowledge of diabetes and self-efficacy could be responsible for the decrease in HbA1c. In addition, high-intensity and fidelity interventions might contribute to the positive effects of empowerment-based interventions. Further research regarding empowerment-based interventions is needed to determine how reducing the frequency or length of face-to-face or group interviews affects the outcome variables.
To date, our meta-analysis is the most updated review of RCTs performed on this subject. It should be acknowledged that there are some limitations that could influence the outcome of our review. First, we might not have found some studies that were not published or published in other languages. Second, unlike drug or placebo trials, it is difficult to blind the patient and provider for an empowerment intervention. Most of the studies were not double-blind, which could have influenced the treatment from health care professionals participating in the trial. Third, our review concentrated only on interventions that directly empower patients. Thus, the level of empowerment of health care providers[35] is beyond the scope of the present study. Finally, some of the included studies had relatively small sample sizes that might not have been sufficiently powered to detect significant changes in outcomes of interest. In future studies, we hope to draw conclusions about empowerment education interventions for T2DM cases using multicenter, large-scale samples, similar intervention durations, forms, frequencies and methods, and randomized methodologies.
5. Conclusions
In conclusion, findings from the present meta-analysis indicated that empowerment-based education intervention is superior to routine treatment in improving HbA1c, psychosocial self-efficacy, and diabetes knowledge in the type 2 diabetes population. This finding suggests that empowerment-based diabetes education is effective in the management of T2DM. It is worthwhile to note that a thorough understanding of the concept of patient empowerment is necessary to ensure the fidelity of empowerment interventions. In addition, better design and more targeted empowerment are needed to improve other aspects of diabetes.
Author contributions
Conceptualization: Yanyan Chen, Yao Tian.
Data curation: Yanyan Chen, Yao Tian, Xiaohong Sun.
Investigation: Boqiao Wang, Xiao Huang.
Methodology: Yao Tian, Xiaohong Sun, Boqiao Wang.
Software: Yanyan Chen, Xiao Huang.
Writing – original draft: Yanyan Chen, Yao Tian.
Footnotes
Abbreviations: CIs = confidence intervals, DES-SF = Diabetes Empowerment Scale-Short Form, HbA1c = glycated hemoglobin, MD = mean difference, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCTs = randomized controlled trials, SMD = standard mean difference, T2DM = type 2 diabetes mellitus.
How to cite this article: Chen Y, Tian Y, Sun X, Wang B, Huang X. Effectiveness of empowerment-based intervention on HbA1c and self-efficacy among cases with type 2 diabetes mellitus: A meta-analysis of randomized controlled trials. Medicine. 2021;100:38(e27353).
Funding: This study was supported by the School Fund Project of Tianjin Vocational Institute (grant number 20162114).
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Ebrahimi H, Sadeghi M, Amanpour F, Vahedi H. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Prim Care Diabetes 2016;10:129–35. [DOI] [PubMed] [Google Scholar]
- [2].Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018;138:271–81. [DOI] [PubMed] [Google Scholar]
- [3].Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment. Results of a randomized controlled trial. Diabetes Care 1995;18:943–9. [DOI] [PubMed] [Google Scholar]
- [4].Anderson RM, Funnell MM. Patient empowerment: myths and misconceptions. Patient Educ Couns 2010;79:277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ 2000;26:597–604. [DOI] [PubMed] [Google Scholar]
- [6].Funnell MM, Anderson RM, Arnold MS, et al. Empowerment: an idea whose time has come in diabetes education. Diabetes Educ 1991;17:37–41. [DOI] [PubMed] [Google Scholar]
- [7].Adolfsson ET, Walker-Engstrom ML, Smide B, Wikblad K. Patient education in type 2 diabetes: a randomized controlled 1-year follow-up study. Diabetes Res Clin Pract 2007;76:341–50. [DOI] [PubMed] [Google Scholar]
- [8].Anderson RM, Funnell MM, Aikens JE, et al. Evaluating the efficacy of an empowerment-based self-management consultant intervention: results of a two-year randomized controlled trial. Ther Patient Educ 2009;1:03–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chen MF, Wang RH, Lin KC, Hsu HY, Chen SW. Efficacy of an empowerment program for Taiwanese patients with type 2 diabetes: a randomized controlled trial. Appl Nurs Res 2015;28:366–73. [DOI] [PubMed] [Google Scholar]
- [10].Cooper H, Booth K, Gill G. A trial of empowerment-based education in type 2 diabetes—global rather than glycaemic benefits. Diabetes Res Clin Pract 2008;82:165–71. [DOI] [PubMed] [Google Scholar]
- [11].Cortez DN, Macedo MM, Souza DA, et al. Evaluating the effectiveness of an empowerment program for self-care in type 2 diabetes: a cluster randomized trial. BMC public health 2017;17:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med 2006;23:944–54. [DOI] [PubMed] [Google Scholar]
- [13].Macedo MML, Cortez DN, Santos JCD, Reis IA, Torres HC. Adherence to self-care practices and empowerment of people with diabetes mellitus: a randomized clinical trial. Rev Esc Enferm USP 2017;51. [DOI] [PubMed] [Google Scholar]
- [14].Mohamed H, Al-Lenjawi B, Amuna P, Zotor F, Elmahdi H. Culturally sensitive patient-centred educational programme for self-management of type 2 diabetes: a randomized controlled trial. Primary Care Diabetes 2013;7:199–206. [DOI] [PubMed] [Google Scholar]
- [15].Spencer MS, Rosland AM, Kieffer EC, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health 2011;101:2253–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Anderson RM, Funnell MM, Nwankwo R, Gillard ML, Oh M, Fitzgerald JT. Evaluating a problem-based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethn Dis 2005;15:671–8. [PubMed] [Google Scholar]
- [17].Cheng L, Sit JWH, Choi KC, et al. The effects of an empowerment-based self-management intervention on empowerment level, psychological distress, and quality of life in patients with poorly controlled type 2 diabetes: a randomized controlled trial. Int J Nurs Stud 2009;116:103407. [DOI] [PubMed] [Google Scholar]
- [18].Sigurdardottir AK, Benediktsson R, Jonsdottir H. Instruments to tailor care of people with type 2 diabetes. J Adv Nurs 2009;65:2118–30. [DOI] [PubMed] [Google Scholar]
- [19].Varming AR, Rasmussen LB, Husted GR, Olesen K, Gronnegaard C, Willaing I. Improving empowerment, motivation, and medical adherence in patients with poorly controlled type 2 diabetes: a randomized controlled trial of a patient-centered intervention. Patient Educ Counsel 2019;102:2238–45. [DOI] [PubMed] [Google Scholar]
- [20].Baldoni NR, Aquino JA, Sanches-Giraud C, et al. Collective empowerment strategies for patients with diabetes mellitus: a systematic review and meta-analysis. Prim Care Diabetes 2017;11:201–11. [DOI] [PubMed] [Google Scholar]
- [21].Aquino JA, Baldoni NR, Flor CR, et al. Effectiveness of individual strategies for the empowerment of patients with diabetes mellitus: a systematic review with meta-analysis. Prim Care Diabetes 2018;12:97–110. [DOI] [PubMed] [Google Scholar]
- [22].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Berlin JA. Does blinding of readers affect the results of meta-analyses? University of Pennsylvania Meta-analysis Blinding Study Group. Lancet (London, England) 1997;350:185–6. [DOI] [PubMed] [Google Scholar]
- [24].Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed) 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Anderson RM. Patient empowerment and the traditional medical model. A case of irreconcilable differences? Diabetes Care 1995;18:412–5. [DOI] [PubMed] [Google Scholar]
- [26].Zhao FF, Suhonen R, Koskinen S, Leino-Kilpi H. Theory-based self-management educational interventions on patients with type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. J Adv Nurs 2017;73:812–33. [DOI] [PubMed] [Google Scholar]
- [27].Jeppsson JO, Kobold U, Barr J, et al. Approved IFCC reference method for the measurement of HbA1c in human blood. Clin Chem Lab Med 2002;40:78–89. [DOI] [PubMed] [Google Scholar]
- [28].Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ (Clinical research ed) 2000;321:405–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Association AD. Lifestyle management: standards of medical care in diabetes-2018. Diabetes Care 2018;41: (suppl 1): S38–s50. [DOI] [PubMed] [Google Scholar]
- [30].Anderson RM, Fitzgerald JT, Gruppen LD, Funnell MM, Oh MS. The Diabetes Empowerment Scale-Short Form (DES-SF). Diabetes Care 2003;26:1641–2. [DOI] [PubMed] [Google Scholar]
- [31].Anderson RM, Funnell MM, Fitzgerald JT, Marrero DG. The Diabetes Empowerment Scale: a measure of psychosocial self-efficacy. Diabetes Care 2000;23:739–43. [DOI] [PubMed] [Google Scholar]
- [32].Tang TS, Funnell MM, Brown MB, Kurlander JE. Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ Couns 2010;79:178–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Gillard ML, Nwankwo R, Fitzgerald JT, et al. Informal diabetes education: impact on self-management and blood glucose control. Diabetes Educ 2004;30:136–42. [DOI] [PubMed] [Google Scholar]
- [34].Tang TS, Gillard ML, Funnell MM, et al. Developing a new generation of ongoing: Diabetes self-management support interventions: a preliminary report. Diabetes Educ 2005;31:91–7. [DOI] [PubMed] [Google Scholar]
- [35].Bravo P, Edwards A, Barr PJ, Scholl I, Elwyn G, McAllister M. Conceptualising patient empowerment: a mixed methods study. BMC Health Serv Res 2015;15:252. [DOI] [PMC free article] [PubMed] [Google Scholar]