Abstract
Intermittent hypoxemia (IH) events are well described in extremely preterm infants, but the occurrence of IH patterns in more mature preterm infants remains unclear. The objective of this study was to characterize the effect of gestational age on early postnatal patterns of IH in extremely (<28wks), very (28–<32wks), and moderately (32–<34wks) preterm infants. As expected, extremely preterm infants had a significantly higher frequency of IH events of longer durations and greater time with hypoxemia versus very and moderately preterm infants. In addition, the postnatal decrease in IH duration was comparable in the very and moderately preterm infants. This progression of IH events should assist clinicians and families in managing expectations for resolution of IH events during early postnatal life.
Keywords: Intermittent Hypoxemia, Preterm Infants, Gestational Age
Introduction
Intermittent hypoxemia (IH) events are ubiquitous in extremely preterm infants and have been associated with impaired outcomes1. However, there is a paucity of data characterizing IH events in very and moderately preterm infants. Preterm infants exhibit periods of apnea and accompanying hypoxemia as a result of immature respiratory control superimposed upon a limited respiratory reserve. Interestingly, IH events may persist while on caffeine and respiratory support 2,3. The last trimester marks a period of substantial neuronal and lung development suggesting that gestational age (GA) at birth plays a role in respiratory instability and oxygenation during early postnatal life. Studies in extremely preterm infants have shown postnatal patterns of IH encompassing a low frequency of IH events during the first week after birth, followed by a progressive increase peaking at approximately 4–5 weeks of life. Little is known about how these events are altered with increasing maturation at birth. Therefore, the objective of this study was to characterize the relationship between gestational age and postnatal alterations of IH events during the first month of life in infants of <34 weeks gestation.
Materials and Methods
This retrospective multi-center analysis included 314 infants (23 0/7 to 33 6/7 weeks gestation) from Rainbow Babies & Children’s Hospital, Cleveland OH (n=128) and Kentucky Children’s Hospital, Lexington KY (n=186). Infants were enrolled regardless of the need for respiratory support. Exclusion criteria included major congenital anomalies. Oxygen saturation (SpO2) waveforms were continuously recorded (0.5–1Hz sample rate, 2–8 seconds averaging time) from the bedside oximeters (Radical 7: Masimo, Irvine, CA) over the first month of life using custom data acquisition systems (National Instrument, Hungary, Labview, Austin, TX and Matlab, Natick, MA or Acumen Instruments Corp. and Matlab, Natick, MA). Very and moderately preterm infants were targeted between SpO2 90–95%. In extremely preterm infants SpO2 targets ranged between 85–95% (mainly 90–95%) depending on the time period and center. Alarm limits approximated target ranges. Daily summaries of the incidence and duration of IH (SpO2 <80% for >10sec and <3min in duration) events and percent time in hypoxemia (SpO2 <80%) were documented. Written informed or waiver of consent was approved by the internal review boards and the institutes’ committees on human research approved the study protocols (Cleveland, OH #021814 and Lexington, KY #44278). Maturation was defined as extremely preterm (<28wks), very preterm (28 0/7–31 6/7wks), and moderately preterm (32 0/7– 33 6/7wks) per World Health Organization guidelines.
Statistical Analyses
Daily summaries of the number of IH events per day, duration of IH events, and percent time with SpO2 <80% were presented by week of gestation then stratified into extremely, very, and moderately preterm groups for statistical comparisons. A Box-Cox transformation was applied in the case of skewed distributions. Linear mixed-effects models with splines were used after adjusting for postnatal age, race, birthweight and sex. Random intercept, slope (associate with time, day variable) and B-spline basis were used in the mixed-effects model. Knots were manually chosen based on the curvature of each outcome variable (R version 3.6.2).
Results
Of the 314 infants included 212, 58, and 44 were extremely, very and moderately preterm infants, respectively. Subjects were 50% female and 67% white. All extremely, 98% of very and 30% of moderately preterm infants received caffeine therapy. The lowest IH frequency and percent time with hypoxemia consistently occurred during the first week of life and the overall increases in peak incidence diminished with subsequent weeks of gestational maturity (Figure 1). Extremely preterm infants had the highest overall frequency of IH events compared to very (p<0.0001) and moderately (p<0.002) preterm infants (Figure 2). Very preterm infants had a modest increase in IH during the first weeks of life with relatively few IH events in the moderate preterm infant cohort and no difference in overall IH frequency between these two infant groups (p=0.89).
Figure 1.
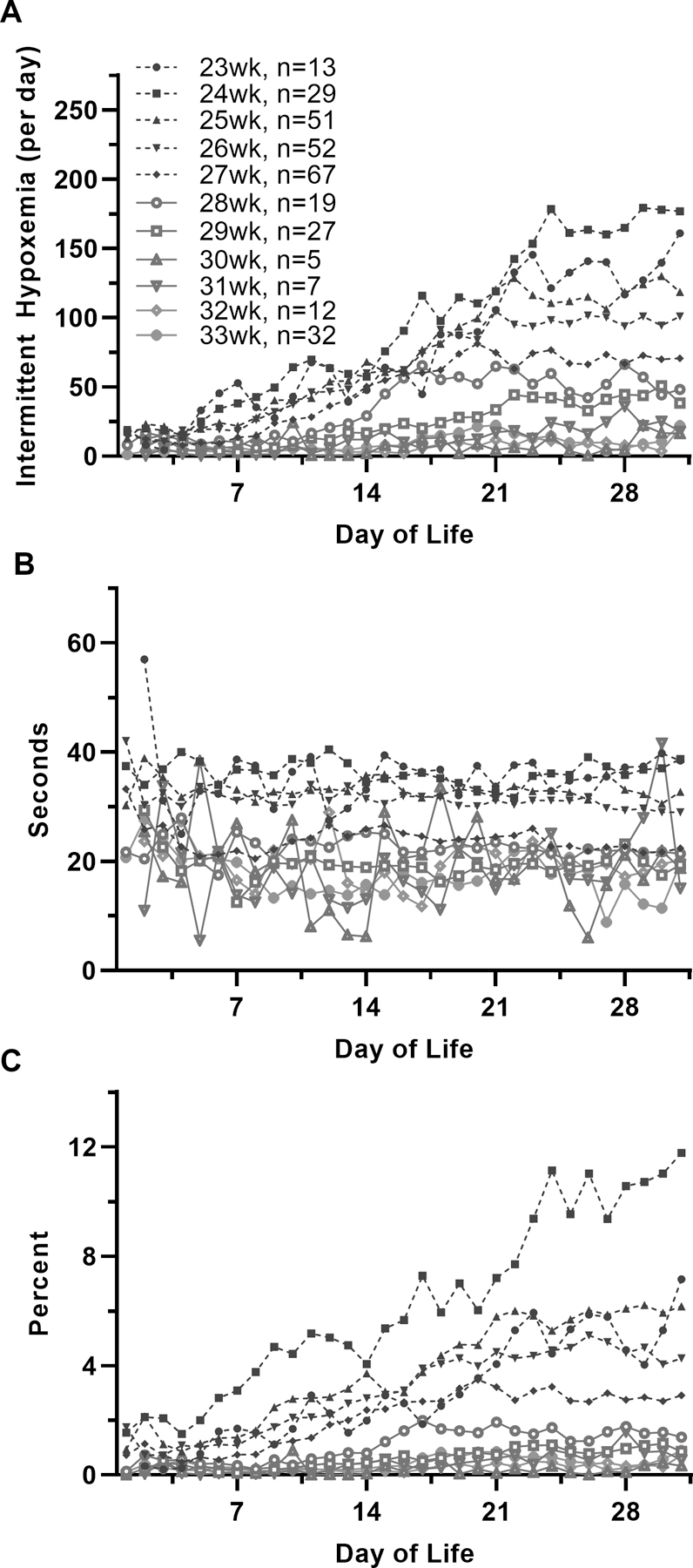
Frequency and Duration of Intermittent Hypoxemia (IH) Events and Percent Time in Hypoxemia (SpO2 <80%) with Increasing Gestational Age. A) Frequency of IH events B) Duration of IH events, and C) Percent time in hypoxemia.
Figure 2.
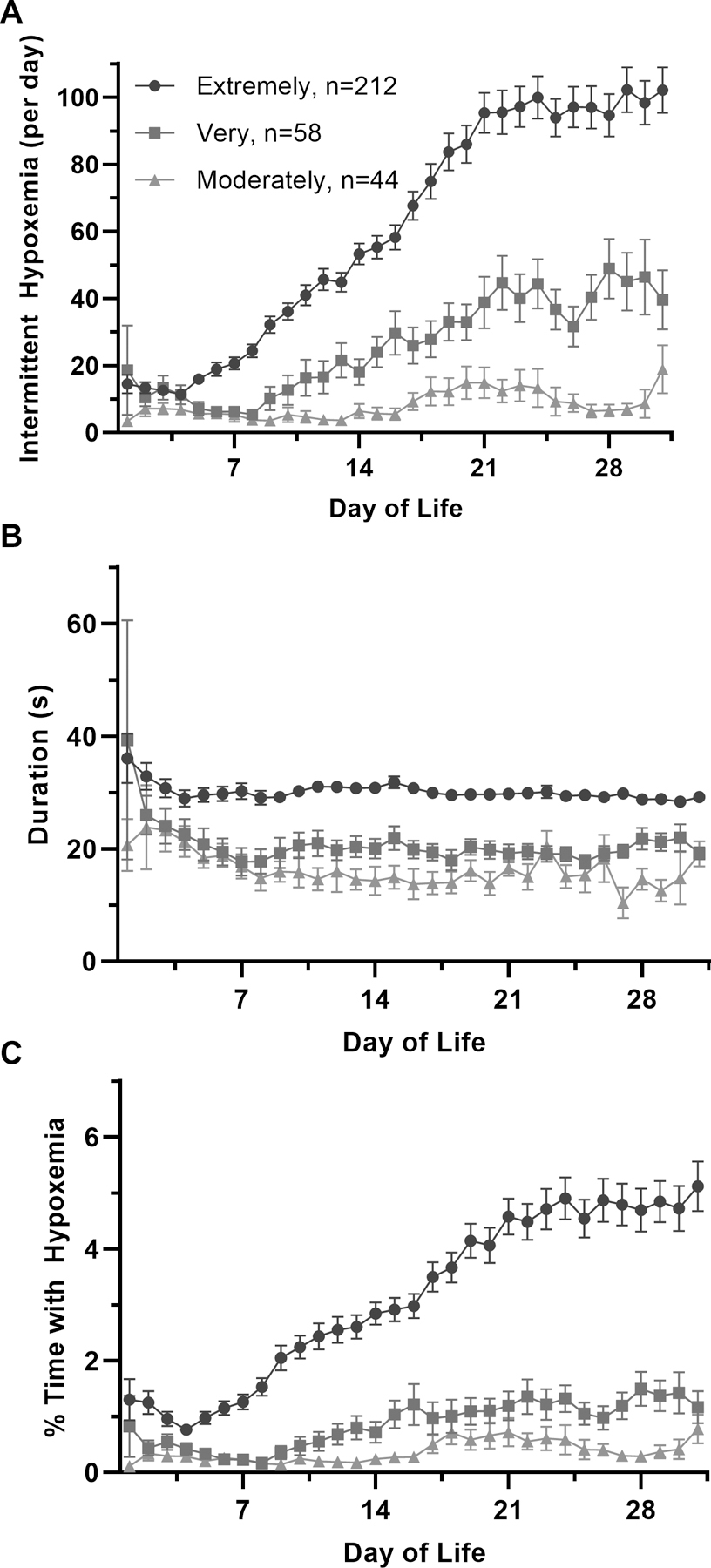
Frequency and Duration of Intermittent Hypoxemia (IH) Events and Percent Time in Hypoxemia (SpO2 <80%) Stratified by Degree of Maturation (Extremely, Very and Moderately Preterm Infants). A) Frequency of IH events B) Duration of IH events, and C) Percent time in hypoxemia. (Mean ±SEM)
In extremely preterm infants the mean duration of IH plateaued to ~30 seconds by the 2nd–4th weeks of life. In contrast, overall IH duration was significantly shorter in the very (p<0.0001) and moderately (p=0.009) preterm infants plateauing at ~ 15–20 sec with no difference between the very and moderately preterm infant groups (p=0.89).
Extremely preterm infants spent up to 5% of the time in hypoxemia by the 4th week of life. In contrast, very and moderately preterm infants had a significantly lower overall percentage of time in hypoxemia (p<0.0001 and p<0.003 versus extremely preterm infants, respectively) with <1% of the time in hypoxemia throughout the monitoring period (p=0.94, very versus moderately preterm infants).
Discussion/Conclusion
This study revealed a lower frequency and abrupt shortening of IH events in very and moderately preterm infants versus extremely preterm infants resulting in less time in hypoxemia. In contrast, IH patterns and cumulative IH exposure were similar between very and moderately preterm infants. The initial rise in IH events after the first week of life within each age group could be attributed to upregulation of brainstem-mediated inhibitory pathways, altered peripheral chemosensitivity, and decreased central chemosensitivity during the fetal to neonatal transition period. Early development of residual lung disease could also play a role. In the most immature infants at 23–27 weeks gestation the lung is at the canalicular stage of fetal lung development initiating growth of the respiratory bronchioles. By 28 weeks gestation transition to the saccular stage begins with progression of alveolar ducts, alveoli, and alveolar duct arteries initiating alveolar capillary growth4. It is therefore possible that the acute shortening of IH duration is a reflection of this early alveolar developmental phase of lung maturity leading to improved oxygenation and more rapid recovery from an IH event in the more mature infant groups. Lastly, although the moderately preterm infants are of older gestation, the comparable IH duration in the very and moderately preterm infants suggests that respiratory control and/or lung function needed to resolve the event may not markedly differ between these two infant groups.
This study provides a basis for the characterization of age based acute alterations in oxygen stability during early postnatal life. The lack of statistically significant findings in IH frequency between very and moderately preterm infants may be due to overlap at the beginning and end of the study period or insufficient sample size. Ongoing multicenter trials with continuous recordings of oxygen saturation5 and a larger infant cohort could add to these hypothesis generating findings.
In conclusion, this brief report documents the progression of IH events in preterm infants during early postnatal life. The lowest incidence of IH events occurs during the first week of life followed by a gestational age dependent transient increase with advancing postnatal age. In contrast to extremely preterm infants, very and moderately preterm infants had a lower frequency of IH events and shorter IH duration with no differences between the more mature infant groups. Understanding the interaction between maturation and the natural progression of IH events should assist clinicians and families in managing expectations for resolution of IH events during early postnatal life.
What is already known on this topic:
Intermittent hypoxemia events are ubiquitous in extremely preterm infants.
Intermittent hypoxemia is linked to impaired outcomes.
There is a paucity of data characterizing IH events in very and moderately preterm infants.
What this study adds:
This study characterizes age based acute alterations in intermittent hypoxemia during early postnatal life.
This study revealed a lower frequency of IH events in very and moderately preterm infants versus extremely preterm infants.
This study revealed an abrupt shortening of IH events in very and moderately preterm infants versus extremely preterm infants.
Funding Sources
The study was funded in part by: (1) The Gerber Foundation, University of Kentucky (EGA, PI), (2) University of Kentucky’s National Center for Advancing Translational Sciences, UL1RR033173. (3) TMR is supported by NIH K08HL133459-03 grant, (4) The Gerber Foundation, Case Western Reserve University (JMD, Co-I; Peter MacFarlane, PI).
Abbreviations:
- GA
Gestational Age
- IH
Intermittent Hypoxemia
- SpO2
Oxygen Saturation
- wks
Weeks
Footnotes
Disclosure Statement
The authors have no conflicts of interest to declare.
Data availability statements
This study contains data from 2 university hospital sites. Re-use of the data is not permitted. Deindified data are available upon reasonable request from the authors http://orcid.org/0000-0003-4414-7007
References
- 1.Poets CF, Roberts RS, Schmidt B, et al. Association Between Intermittent Hypoxemia or Bradycardia and Late Death or Disability in Extremely Preterm Infants. JAMA. 2015;314(6):595–603. [DOI] [PubMed] [Google Scholar]
- 2.Fairchild KD, Nagraj VP, Sullivan BA, Moorman JR, Lake DE. Correction: Oxygen desaturations in the early neonatal period predict development of bronchopulmonary dysplasia. Pediatr Res. 2020. [DOI] [PubMed]
- 3.Bancalari E, Claure N. Respiratory Instability and Hypoxemia Episodes in Preterm Infants. Am J Perinatol. 2018;35(6):534–536. [DOI] [PubMed] [Google Scholar]
- 4.Hislop A Developmental biology of the pulmonary circulation. Paediatr Respir Rev. 2005;6(1):35–43. [DOI] [PubMed] [Google Scholar]
- 5.Dennery PA, Di Fiore JM, Ambalavanan N, et al. Pre-Vent: the prematurity-related ventilatory control study. Pediatr Res. 2019;85(6):769–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study contains data from 2 university hospital sites. Re-use of the data is not permitted. Deindified data are available upon reasonable request from the authors http://orcid.org/0000-0003-4414-7007


