Abstract
PURPOSE:
For patients with cancer who are older than 65 years, the 2018 ASCO Guideline recommends geriatric assessment (GA) be performed. However, there are limited data on providers’ practices using GA. Therefore, ASCO’s Geriatric Oncology Task Force conducted a survey of providers to assess practice patterns and barriers to GA.
METHODS:
Cancer providers treating adult patients including those ≥ 65 years completed an online survey. Questions included those asking about awareness of ASCO’s Geriatric Oncology Guideline (2018), use of validated GA tools, and perceived barriers to using GA. Descriptive statistics and statistical comparisons between those aware of the Guideline and those who were not were conducted. Statistical significance was set at P < .05.
RESULTS:
Participants (N = 1,277) responded between April 5 and June 5, 2019. Approximately half (53%) reported awareness of the Guideline. The most frequently used GA tools, among those aware of the Guideline and those who were not, assessed functional status (69% v 50%; P < .001) and falls (62% v 45%; P < .001). Remaining tools were used < 50% of the time, including tools assessing weight loss, comorbidities, cognition, life expectancy, chemotherapy toxicity, mood, and noncancer mortality risk. GA use was two to four times higher among those who are aware of the Guideline. The most frequent barriers for those who reported being Guideline aware were lack of resources, specifically time (81.7%) and staff (77.0%). In comparison, those who were unaware of the Guideline most often reported the following barriers: lack of knowledge or training (78.4%), lack of awareness about tools (75.2%), and uncertainty about use of tools (75.0%).
CONCLUSION:
Among providers caring for older adults, 52% were aware of the ASCO Guideline. Some domains were assessed frequently (eg, function, falls), whereas other domains were assessed rarely (eg, mood, cognition). Guideline awareness was associated with two to four times increased use of GA and differing perceived barriers. Interventions facilitating Guideline-consistent implementation will require various strategies to change behavior.
INTRODUCTION
In the United States, 70% of patients with cancer will soon be ≥ 65 years of age, representing an increase in incidence in this population from 1.6 to 2.3 million—a 67% increase.1 Furthermore, it is estimated that the proportion of cancer survivors in the United States aged ≥ 65 years will reach 73% by the year 2040.2 By 2030, the global population of people in this age group will reach approximately 1 billion, with the number of new cancer cases per year among older individuals exceeding 13 million.3,4 Recognizing these trends, ASCO, the US Food and Drug Administration, the National Institutes of Health, and others have undertaken a multipronged strategy to improve the evidence base regarding the treatment of older adults with cancer,5-7 to enhance the education and training for oncology providers globally who care for adults with cancer,6,8,9 and to create guidelines aimed at improving the quality of care for the increasing number of older adults with cancer.
There is increasing evidence supporting the use of geriatric assessment (GA) to address the unique care needs of older patients with cancer. GA is a collection of validated tools to assess specific domains (eg, physical function, comorbidities, cognition) known to be associated with worse outcomes.10-14 GA is the standard of care for assessing vulnerabilities in older patients with cancer to guide communications, decision-making, and management.15-17 Importantly, randomized trial data show that GA-guided therapy can reduce treatment toxicity.18,19 Accordingly, in 2018, ASCO created its first formal guideline for the care of older adults with cancer in which national experts on the care of this patient group synthesized the evidence.20 Based on this guideline, ASCO recommends that GA “be used to identify vulnerabilities that are not routinely captured in oncology assessments” and that “evidence supports [an] assessment of function, comorbidity, falls, depression, cognition, and nutrition.”20 Furthermore, on the basis of a Delphi consensus of geriatric oncology experts, the guideline recommends that GA deficits be used to inform patients about risks, adjust treatment choices, and implement appropriate interventions.20
Whether and how often cancer providers use GA tools when treating older adults is not known. There remain limited data on providers’ baseline knowledge and practices regarding the use of reliable and valid GA tools. Also, whether providers are aware of the ASCO Guideline (hereafter, Guideline) and whether an awareness is associated with different practice patterns is not known. Therefore, it is important to evaluate providers’ knowledge of GA tools, awareness of the Guideline, and likelihood of practicing in accordance with Guideline recommendations. Recognizing these knowledge gaps, ASCO’s Addressing Cancer Health Disparities Among Older Adults Task Force (hereafter, the Task Force) conducted an international online survey of the oncology workforce to assess providers’ awareness of the Guideline, practice patterns regarding GA, and perceptions of barriers to using GA when treating patients ≥ 65 years old. The findings of the survey are summarized in this report.
METHODS
Survey Development
An online questionnaire was developed to assess oncology provider practice patterns and perceptions regarding the use of GA, both formal and informal, when treating patients aged ≥ 65 years who have cancer. Formal GA uses validated surveys and administered tests to assess specific domains in patients with cancer, such as activities of daily living for functional losses or a cognition screen. Informal GA refers to age-specific judgements without using validated tools, such as mobility as judged on the use of an assist device or cognitive deficits based on conversations with patients. The questionnaire and the administration plan were developed and reviewed by the Task Force members who are coauthors of this paper (W.D., G.R.W., A.M., E.S., R.M., and H.D.K.). Questionnaire domains included respondent characteristics (ie, professional degree, geographic location, clinical practice setting, disease sites most frequently treated, years of experience); awareness (or not) of the Guideline; whether older patients were assessed and/or treated differently than younger patients when making treatment decisions; and frequency of performing either an informal assessment or a formal GA using validated tools at two different times (ie, at initial presentation and later in disease course). If use of a formal GA was endorsed, the frequency of use was ascertained as “always,” “most of the time,” “some of the time,” “little of the time,” or “none of the time” for both time points. Finally, questions about perceived barriers to performing a GA for older patients were asked, including about resource limitations, perceived value of the GA, and perceived validity of existing GA tools (Data Supplement, online only).
Study Sample
The inclusive target sample was composed of cancer care providers including physicians of any specialty (eg, oncologists, surgeons, radiation oncologists, primary care), nurses (including nurse practitioners), physician assistants, and any other members of the cancer clinical care team (eg, social work, physical therapists) who currently treat patients with cancer. The online survey invited anyone currently treating patients with cancer aged ≥ 65 years and was not targeted to specific groups. This included any oncology providers, whether they were ASCO members or not, and respondents could be located in any country. Those who do not currently treat patients with cancer clinically in some way were identified via a screening question and excluded (Data Supplement).
Recruitment of Respondents
The online survey was administered using SurveyMonkey (San Mateo, CA) between April 5, 2019, and June 5, 2019. Several audiences were invited. During that time, for example, ASCO members were sent direct e-mail invitations to participate in the survey; the e-mail was sent to 11,221 members who were either full members, advanced practice providers, or affiliated health professionals. In addition, the survey was advertised during ASCO’s 2019 Annual Meeting (May 31-June 4) and actively promoted via popular social media channels, including Twitter, Instagram, and LinkedIn, to any oncology providers, whether associated with ASCO or not. No financial incentives were offered to respondents to complete the survey. By design based on pilot testing, the time to complete the survey was < 10 minutes.
Data Analysis
Summary descriptive analyses were conducted for responses to survey questions. Although our recruitment strategy was broader than ASCO members, as already described, for context, the demographic and clinical characteristics of survey respondents are presented alongside the demographic characteristics of ASCO members, based on membership data available as of August 1, 2019. Then, survey responses were compared on the basis of current knowledge of the Guideline to evaluate differences between these groups. Responses to questions related to the use of the GA were dichotomized between those who reported performing a GA either always, most of the time, or some of the time, and those who reported performing it little of the time or none of the time; the differences were compared with χ2 testing, as appropriate. We analyzed the proportion of respondents who used GA tools always or most of the time or some of the time according to their awareness of the Guidelines. Similarly, barriers to performing the GA (yes or no) were compared between the two groups with χ2 tests. Differences were considered significant if P < .05.
RESULTS
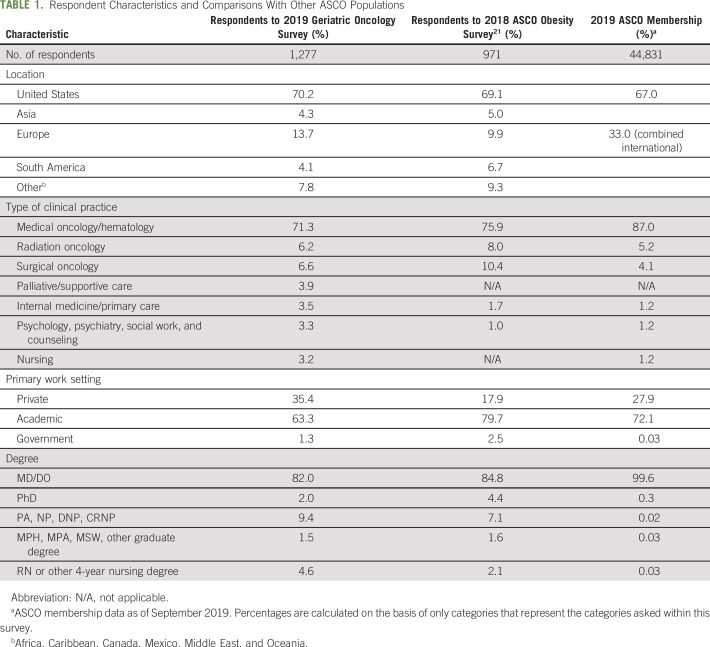
A total of 1,277 providers responded to the survey between April 5, 2019, and June 5, 2019. Of those, 1,240 (97%) were actively treating patients with cancer and were invited to complete the survey. Demographic and practice characteristics of respondents are listed in Table 1. A majority had a doctoral degree (MD and/or PhD; 82%), were located in the United States (70%), and were practicing in an academic medical center or university (61%). Medical oncology represented the primary specialty category (61%), followed by hematology (7%) and surgical oncology (7%). The majority of respondents considered themselves specialists (58%) rather than generalists (39%), with breast, lung, and colorectal cancers reported as the most frequently treated disease sites by 48%, 37%, and 30% of respondents, respectively. The survey population was similar to overall ASCO membership as well as a sample for a previous survey of obesity in patients with cancer who were recruited in a similar way (Table 1).21 The primary differences between survey respondents and ASCO membership overall is reflected in the requirement for our respondents to be clinically active cancer providers, resulting in a greater percentage of MDs compared with PhDs in this sample. We also note that the majority of respondents (63%) reported being in academic medicine than in private practice (35%), which differs a bit from ASCO’s overall ratio (72% to 29%, respectively).
TABLE 1.
Respondent Characteristics and Comparisons With Other ASCO Populations
Participants were asked how frequently they assess older patients differently than younger patients when making treatment decisions, and 63% reported “always” or “most of the time,” 28% reported “some of the time,” and 9% reported “rarely” or “never.” When asked in what ways participants assess older patients differently than younger patients, 29% reported formally using specific validated tools, whereas 69% reported an informal assessment based on their own judgment. Participants then reported on how often they performed a multidimensional GA using validated tools, and 21% reported “always” or “most of the time,” 22% reported “some of the time,” and 57% reported “rarely” or “never.”
Clinical Practice Patterns Based on Awareness of ASCO Guidelines
Slightly more than half of respondents (53%) reported awareness of the Guideline (Fig 1). Overall, those aware of the Guidelines were more likely than those not aware to assess patients aged ≥ 65 years differently than younger patients (aware v unaware: 65% v 60%; P < .01). In addition, Guideline awareness was positively associated with a greater frequency of performing a multidimensional GA using validated tools (aware v unaware: 55% v 31%; P < .01; data available on request). Of note, respondents from academic practice compared with private (ie, community) practice had no statistically significant differences in their responses; similarly, there were no differences between those with different academic degrees (results not shown).
Fig 1.
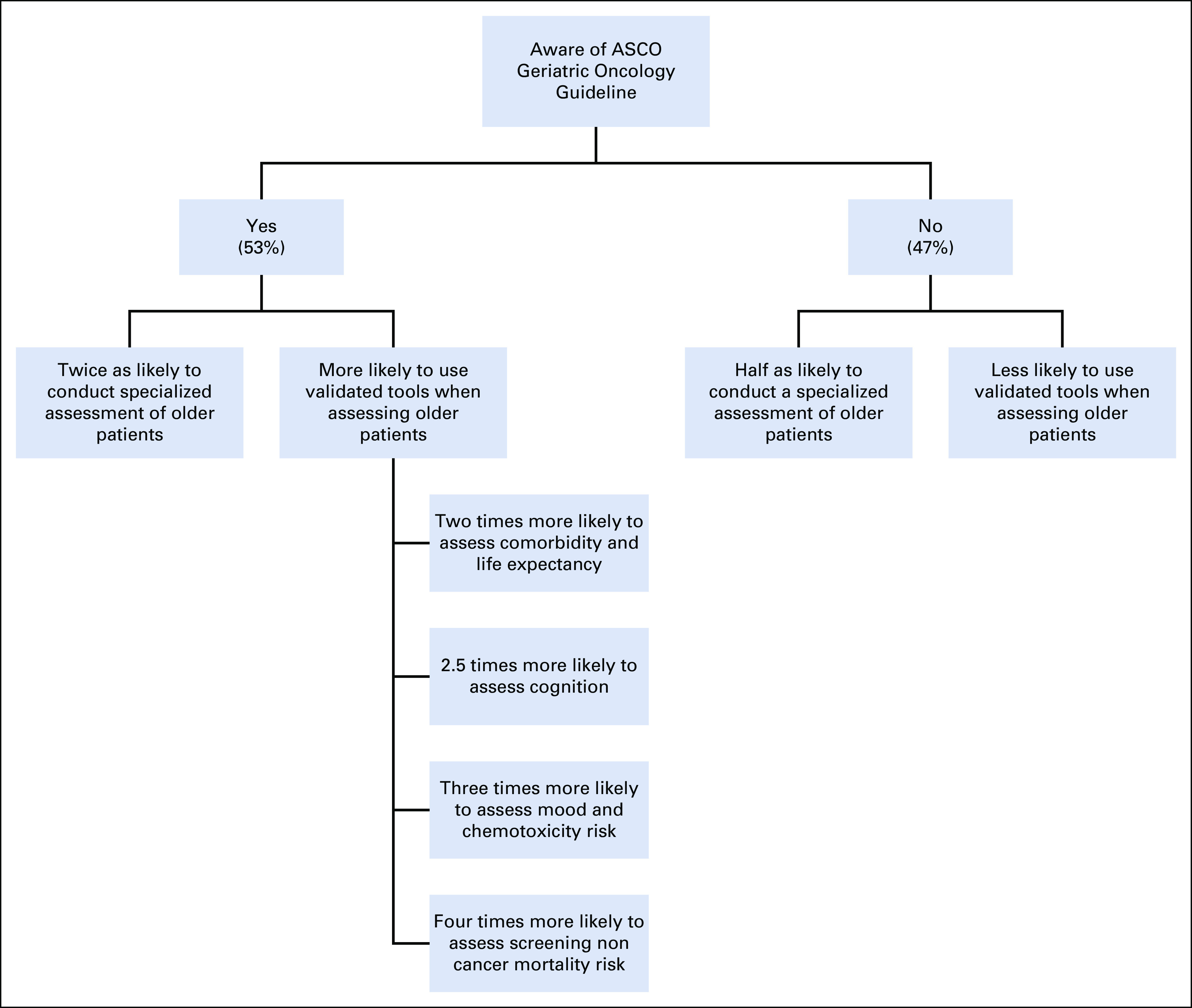
Summary of differences between those who are aware of the ASCO Geriatric Oncology Guideline and those who are not.20
Considering each of the GA domains independently (Fig 2), the patterns were similar for each group. For example, the most likely assessed domain for each group was functional status (aware v unaware: 69% v 50%; P < .001) and the least likely was noncancer mortality risk (aware v unaware: 22% v 5%; P < .001). Other domains of note, with data for the Guideline-aware group presented first, included falls (62% v 45%; P < .001), cognition (37% v 15%; P < .001), and mood (26% v 8%; P < .001). Notably, most domains are assessed by less than half of all providers, and several are assessed by < 20%, including cognition, mood, and chemotherapy toxicity risk.
Fig 2.

Use of validated tools to assess domains in older adults with cancer, comparing those aware of ASCO guidelines with those who are not: percentage responding “yes” to each domain. P < .001 for all domains.
Use of Validated GA Tools
Participants were asked about their use of the various tools included in the GA both at baseline (before starting treatment) and after treatment had been started (Fig 3). The GA domains assessed were functional status, nutritional status, social activity, physical performance, and cognition; all were assessed significantly more often by those aware of the Guidelines. The most widely used tool for functional assessment was used at baseline by nearly 70% of those who were aware of the ASCO Guidelines and by 57% of those who were not (P < .001). The least commonly assessed domain was cognition, assessed by 32% of those aware of Guideline and < 20% of those not aware. Nutrition, social activity, and physical performance fell in between. All comparisons were significant at the P < .01 level (Fig 3).
Fig 3.
Geriatric assessment domains assessed with specific tools, comparing those aware of ASCO guidelines with those who are not: percentage responding “always” or “most of the time.” (A) Before initiating chemotherapy. P < .001 for all domains except nutritional status (P = .0011). (B) After initiating chemotherapy. P < .001 for functional status, social activity, and cognition; P = .0011 for physical performance; P = .0015 for nutritional status.
Barriers to Performing a GA in Oncology Practice
The most common barriers cited overall were lack of time, lack of support staff, and lack of training or knowledge about GA. Only one-quarter of respondents in both groups felt there was insufficient evidence to support the use of the GA in oncology practice (aware v unaware: 25.8% v 23.6% [not statistically significantly different]). Another less commonly cited concern was the lack of direct reimbursement for conducting a GA (aware v unaware: 32.8% v 45.8%; Fig 4). There were interesting similarities, but also important differences, between respondents who were aware of the Guideline and those who were not. For those who were aware of the Guideline, the most common barriers included lack of time (82%), lack of support staff (77%), lack of training or knowledge (58%), and lack of awareness of validated tools (57%). Conversely, the most common barriers cited by those unaware of Guideline were a lack of training or knowledge (76%), lack of awareness of validated tools (75%), and uncertainty about which tools to use (73%).
Fig 4.
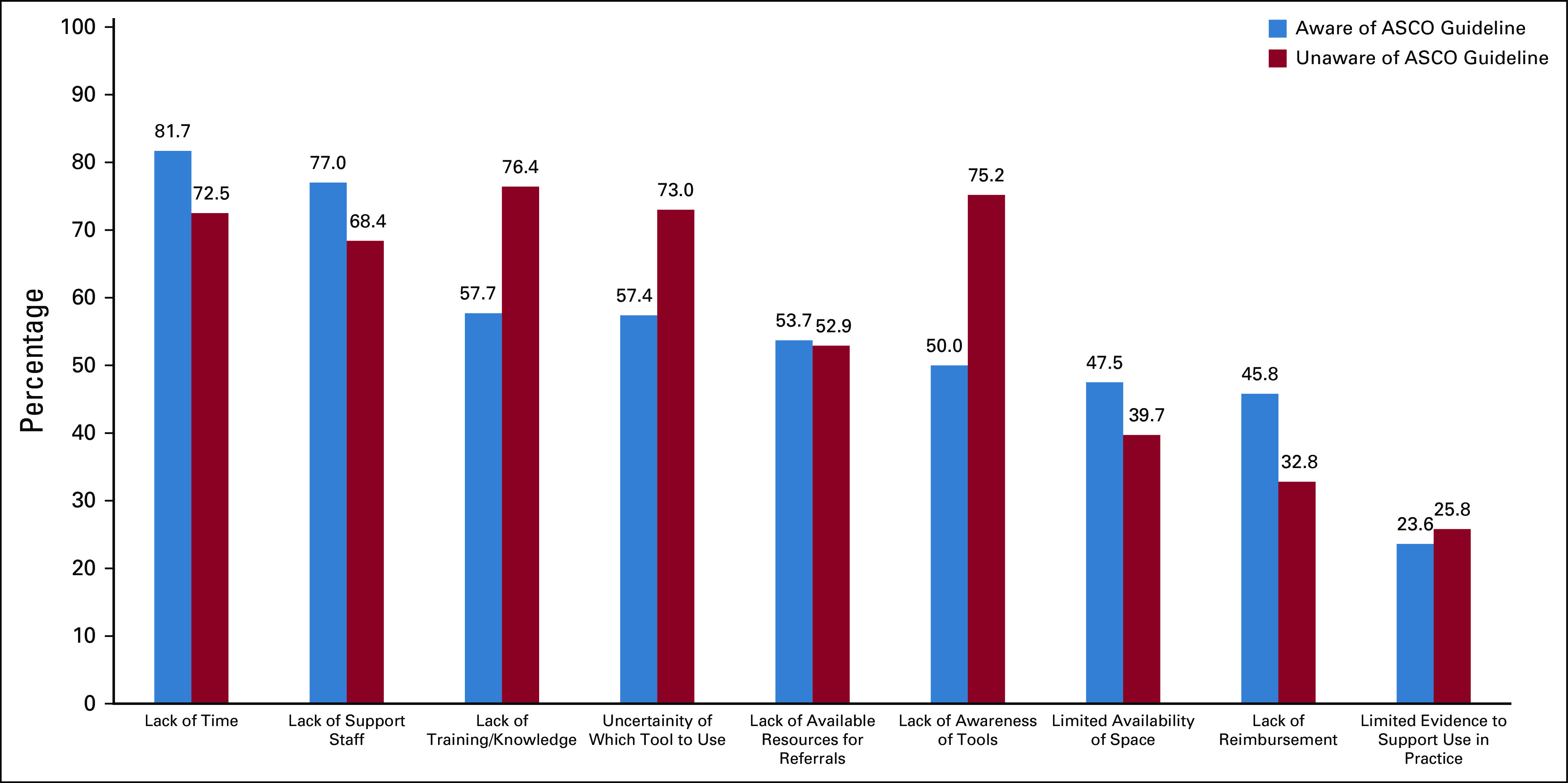
Barriers to performing geriatric assessments, comparing those aware of ASCO guidelines with those not aware: percentage responding “strongly agree” or “agree.” P < .001 for lack of time, lack of reimbursement, lack of training/knowledge, lack of awareness of tools, and uncertainty of which tool to use; P = .002 for lack of support staff; P =.014 for limited availability of space; P =.796 for lack of available resources for referrals; P =.452 for limited evidence to support use in practice.
DISCUSSION
In this large survey evaluating how oncology providers report caring for older adults with cancer, with a focus on the use of a validated GA, there were both encouraging and concerning findings. Encouragingly, the majority endorsed the evaluation of functional status and falls, whereas approximately one-half of respondents reported evaluating unintentional weight loss and performing a comorbidity assessment, all of which are important. Of some concern, several aspects of the GA are used by only a minority of providers, including mood assessment, noncancer mortality risk, and cognitive evaluation. Although the majority reported assessing their older patients differently than their younger patients, most oncology providers used informal, unvalidated assessments and rarely or never used a formal GA.
These findings are significant because there is increasing evidence that conducting a GA can lead to adaptations in clinical management and improved outcomes for older adults with cancer. At the time this survey was conducted, published data showed that if oncologists are aware of GA results indicating functional or cognitive impairment, they would decrease their likelihood of giving full-dose chemotherapy.18,19,22-24 A randomized trial showed that use of a GA could minimize toxicities without affecting survival in patients with advanced-stage lung cancer.18,19 More recently, studies have shown that conducting a GA and giving the results to providers leads to significantly improved communications among patients, caregivers, and oncologists.17 Furthermore, chemotherapy toxicities can be reduced, hospitalizations decreased, and quality of life increased when GA-guided interventions are used, even in frail older adults.25-27 Although data from additional, definitive randomized controlled trials of survival and GA are emerging, the impact on overall survival remains to be established.25-28 To avoid the consequences of overtreatment and undertreatment of older adults, a GA needs to be the centerpiece of any intervention.28 In short, emerging evidence continues to support the Guideline recommendation for use of GA, and efforts to ensure implementation into practice are critical.
Given the centrality of GA to care patterns, an awareness of the ASCO Guideline is notable. A crucial finding was the substantial differences between those who reported being aware of the recently published Guideline and those who were not.29-31 Those who were aware of the Guideline were two to four times more likely to conduct specific aspects of a formal GA (Fig 1). Although we are unable to attribute a causal relationship in this cross-sectional survey between knowing about the Guideline and use of GA, it is encouraging that Guideline awareness was strongly associated with the use of the GA in practice. Guidelines remain a promising component of a campaign for improving the likelihood of an evidence-based approach to care for older adults.
Encouragingly, the perceived value of GA is well accepted.22,32-36 Only one in four providers, independent of Guideline awareness, said that limited evidence was a barrier; this is an important recognition of the value of the GA and the growing evidence-base behind its use in cancer care. Also encouraging was that fewer than half of respondents cited a lack of reimbursement or limited clinical space as significant barriers.
Still, important barriers to the adoption of the GA in routine practice remain. Overall, perceived barriers to implementation of GA were discouragingly high. For example, more than half of respondents acknowledged that lack of referral sources for GA-guided interventions, such as physical therapy or social work, were barriers to implementing GA in practice, pointing toward the importance of creating multidisciplinary teams with geriatric expertise across care delivery settings. Additional barriers can be characterized into two separate groups based on provider awareness of the ASCO Guideline. The first are system- or resource-related constraint barriers37,38 and the second are barriers of knowledge and training regarding the use of GA tools.
Those who were aware of the Guidelines were more likely to point to lack of resources (ie, time, support staff, and referral options) as barriers to implementation of the GA. In contrast, for those unaware of the Guideline, lack of awareness of GA tools, uncertainty about which tools to use, and lack of training in how to use the tools were most important. An implication of the differing perceptions of barriers is the approach to designing education, training, and resources to support the practical implementation of GA. For those familiar with the tools but unable to identify resources (ie staff, space, and time), the focus should be on obtaining those resources and minimizing the burdens of their implementation.39-41 For those less familiar with GA tools and uncertain of their use, training programs29,42,43 could focus on demonstrating their utility in cancer care, showing GA tool awareness and availability, and on helping smoothly integrate them into standard clinical practice. In developing new care models, matching the implementation approach to the needs is crucial in taking the next steps for integrating GA into everyday clinical practice across any setting.44
There are limitations to this study.Although the sample size was large and generally reflected the much larger ASCO membership, the sample was not necessarily generalizable to either ASCO’s membership nor all cancer providers and represented a small proportion of those potentially eligible for the survey. Our survey was focused on active providers of care to older patients with cancer, with a need for brevity, and not on in-depth inquiry. It is possible that respondents reflected a population of providers who were already interested in this topic, resulting in an overestimate of Guideline awareness and use of GA. Although this was an international study, with respondents from many places across the globe, the majority of respondents were from the United States. It is encouraging that those aware of the relatively new ASCO geriatric oncology guideline were more likely to be convinced of the value of the GA and to use it in practice. This suggests additional efforts to disseminate the Guideline to a wider audience would be an important next step in leading to greater adoption in practice. However, this is a cross-sectional study not a longitudinal one, and causality cannot be determined regarding the noted association. Finally, although we have identified a variety of important barriers to GA implementation, evidence of the most effective specific interventions to increase the use of GA await more study.
In conclusion, across a wide-range of providers of cancer care, older adults are often assessed differently than younger patients. There is overall acceptance that the GA is an evidence-based way to evaluate older adults with cancer, and certain domains, such as functional status and falls, are used by a majority of providers. However, most assessments are informal and based on the providers’ own judgment, and other evidence-based GA domains, including cognition, chemotherapy toxicity, life expectancy, and mood, are infrequently evaluated. Notably, a strong association was found between awareness of the recent ASCO Guidelines and the use of the GA in practice, suggesting further dissemination as part of any strategy. While there remain barriers for integrating GA into the care of older adults with cancer, overcoming those barriers differs between those who know the Guideline and those who do not. This difference has important implications for the best strategies for increasing the uptake of the GA across oncology practices.
ACKNOWLEDGMENT
The authors thank and acknowledge the contributions of the members of the ASCO Health Equity Committee, especially the newest members of the Task Force, Drs. Reginald Tucker-Seeley and Sailaja Kamaraju, as well as members of the Cancer and Aging Research Group for their input on the survey and manuscript. The members of the Task Force are indebted to Dr. Arti Hurria, who started the ASCO Geriatric Oncology Special Interest Group, the predecessor of the Task Force, who died tragically in an accident on November 7, 2018.
Grant R. Williams
Honoraria: Carevive Systems, Cardinal Health
Amy MacKenzie
Stock and Other Ownership Interests: Tenet Healthcare (I)
Honoraria: Merck
Enrique Soto-Perez-de-Celis
Research Funding: Roche (I)
Ronald Maggiore
Open Payments Link: https://openpaymentsdata.cms.gov/physician/1120798/summary
Heidi D. Klepin
Consulting or Advisory Role: Genentech
Patents, Royalties, Other Intellectual Property: UptoDate contributor
Uncompensated Relationships: Genentech
No other potential conflicts of interest were reported.
Footnotes
Reprint Requests: American Society of Clinical Oncology, 2318 Mill Rd, Suite 800, Alexandria, VA 22314; e-mail: Cancerpolicy@asco.org.
AUTHOR CONTRIBUTIONS
Conception and design: William Dale, Grant R. Williams, Amy MacKenzie, Enrique Soto-Perez-de-Celis, Ronald Maggiore, Kimberly T. Smith, Heidi D. Klepin
Administrative support: William Dale, Janette Merrill, Kimberly T. Smith,
Collection and assembly of data: All authors
Data analysis and interpretation: William Dale, Grant R. Williams, Amy MacKenzie, Enrique Soto-Perez-de-Celis, Ronald Maggiore, Sweatha Katta, Heidi D. Klepin
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
How Is Geriatric Assessment Used in Clinical Practice for Older Adults with Cancer? A Survey of Cancer Providers by the American Society of Clinical Oncology
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Grant R. Williams
Honoraria: Carevive Systems, Cardinal Health
Amy MacKenzie
Stock and Other Ownership Interests: Tenet Healthcare (I)
Honoraria: Merck
Enrique Soto-Perez-de-Celis
Research Funding: Roche (I)
Ronald Maggiore
Open Payments Link: https://openpaymentsdata.cms.gov/physician/1120798/summary
Heidi D. Klepin
Consulting or Advisory Role: Genentech
Patents, Royalties, Other Intellectual Property: UptoDate contributor
Uncompensated Relationships: Genentech
No other potential conflicts of interest were reported.
REFERENCES
- 1.Smith BD, Smith GL, Hurria A, et al. Future of cancer incidence in the United States: Burdens upon an aging, changing nation J Clin Oncol 272758–27652009 [DOI] [PubMed] [Google Scholar]
- 2.Parry C, Kent EE, Mariotto AB, et al. Cancer survivors: A booming population Cancer Epidemiol Biomarkers Prev 201996–20052011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Institute on Aging: World’s older population grows dramatically: NIH-funded Census Bureau report offers details of global aging phenomenon. 2016. https://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically.
- 4.Soto-Perez-de-Celis E, de Glas NA, Hsu T, et al. Global geriatric oncology: Achievements and challenges J Geriatr Oncol 8374–3862017 [DOI] [PubMed] [Google Scholar]
- 5. National Institutes of Health: Inclusion across the lifespan grants & funding: NIH Central Resource for grants and funding information. https://grants.nih.gov/policy/inclusion/lifespan.htm.
- 6.Levit LA, Singh H, Klepin HD, et al. Expanding the evidence base in geriatric oncology: Action items from an FDA-ASCO workshop J Natl Cancer Inst 1101163–11702018 [DOI] [PubMed] [Google Scholar]
- 7.Singh H, Beaver JA, Kim G, et al. Enrollment of older adults on oncology trials: An FDA perspective J Geriatr Oncol 8149–1502017 [DOI] [PubMed] [Google Scholar]
- 8.Hurria A, Levit LA, Dale W, et al. Improving the evidence base for treating older adults with cancer: American Society of Clinical Oncology statement J Clin Oncol 333826–38332015 [DOI] [PubMed] [Google Scholar]
- 9.Levit LA, Singh H, Klepin HD.Cancer and aging activities at the American Society of Clinical Oncology and beyond: Reflections on the legacy of Dr. Arti Hurria J Geriatr Oncol 11151–1532020 [DOI] [PubMed] [Google Scholar]
- 10. Ward KT, Reuben DB: Comprehensive geriatric assessment. UpToDate. https://www.uptodate.com/contents/comprehensive-geriatric-assessment?search=comprehensive-geriatric-%20assessment&source=search_result&selectedTitle=1~71&usage_type=default&display_rank=1.
- 11.Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: A prospective multicenter study J Clin Oncol 293457–34652011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams GR, Dunham L, Chang Y, et al. Geriatric assessment predicts hospitalization frequency and long-term care use in older adult cancer survivors J Oncol Pract 15e399–e4092019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurria A, Gupta S, Zauderer M, et al. Developing a cancer-specific geriatric assessment: A feasibility study Cancer 1041998–20052005 [DOI] [PubMed] [Google Scholar]
- 14.Klepin HD, Geiger AM, Tooze JA, et al. Geriatric assessment predicts survival for older adults receiving induction chemotherapy for acute myelogenous leukemia Blood 1214287–42942013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohile SG, Velarde C, Hurria A, et al. Geriatric assessment-guided care processes for older adults: A Delphi consensus of geriatric oncology experts J Natl Compr Canc Netw 131120–11302015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wildiers H, Heeren P, Puts M, et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer J Clin Oncol 322595–26032014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohile SG, Epstein RM, Hurria A, et al. Communication with older patients with cancer using geriatric assessment: A cluster-randomized clinical trial from the National Cancer Institute Community Oncology Research Program JAMA Oncol 6196–2042020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gajra A, Loh KP, Hurria A, et al. Comprehensive geriatric assessment-guided therapy does improve outcomes of older patients with advanced lung cancer J Clin Oncol 344047–40482016 [DOI] [PubMed] [Google Scholar]
- 19.Corre R, Greillier L, Le Caër H, et al. Use of a comprehensive geriatric assessment for the management of elderly patients with advanced non–small-cell lung cancer: The phase III randomized ESOGIA-GFPC-GECP 08-02 study J Clin Oncol 341476–14832016 [DOI] [PubMed] [Google Scholar]
- 20.Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology J Clin Oncol 362326–23472018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ligibel JA, Jones LW, Brewster AM, et al. Oncologists’ attitudes and practice of addressing diet, physical activity, and weight management with patients with cancer: Findings of an ASCO survey of the oncology workforce J Oncol Pract 15e520–e5282019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamaker ME, Te Molder M, Thielen N, et al. The effect of a geriatric evaluation on treatment decisions and outcome for older cancer patients - a systematic review J Geriatr Oncol 9430–4402018 [DOI] [PubMed] [Google Scholar]
- 23.Caillet P, Canoui-Poitrine F, Vouriot J, et al. Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA Study J Clin Oncol 293636–36422011 [DOI] [PubMed] [Google Scholar]
- 24.Mohile SG, Magnuson A, Pandya C, et al. Community oncologists’ decision-making for treatment of older patients with cancer J Natl Compr Canc Netw 16301–3092018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mohile SG, Refaat Mohamed M, Culakova E, et al: A geriatric assessment (GA) intervention to reduce treatment toxicity in older patients with advanced cancer: A University of Rochester Cancer Center NCI community oncology research program cluster randomized clinical trial (CRCT). J Clin Oncol 38:12009, 2020 (15 suppl) [Google Scholar]
- 26. Li D, Sun C-L, Kim H, et al: Geriatric assessment-driven intervention (GAIN) on chemotherapy toxicity in older adults with cancer: A randomized controlled trial. J Clin Oncol 38:12010, 2020 (15 suppl) [Google Scholar]
- 27. Soo W-K, King M, Pope A, et al: Integrated geriatric assessment and treatment (INTEGERATE) in older people with cancer planned for systemic anticancer therapy. J Clin Oncol 38:12011, 2020 (15 suppl) [Google Scholar]
- 28. doi: 10.1200/JCO.19.02809. DuMontier C, Loh KP, Bain PA, et al: Defining undertreatment and overtreatment in older adults with cancer: A scoping literature review. J Clin Oncol 38:2558-2569, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maggiore RJ, Dale W, Hurria A, et al. Hematology-oncology fellows’ training in geriatrics and geriatric oncology: Findings from an American Society of Clinical Oncology-sponsored national survey J Oncol Pract 13e900–e9082017 [DOI] [PubMed] [Google Scholar]
- 30.Hsu T, Soto-Perez-de-Celis E, Burhenn PS, et al. Educating healthcare providers in geriatric oncology–a call to accelerate progress through identifying the gaps in knowledge J Geriatr Oncol 111023–10272020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirkhus L, Šaltytė Benth J, Rostoft S, et al. Geriatric assessment is superior to oncologists’ clinical judgement in identifying frailty Br J Cancer 117470–4772017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moth EB, Kiely BE, Stefanic N, et al. Oncologists’ perceptions on the usefulness of geriatric assessment measures and the CARG toxicity score when prescribing chemotherapy for older patients with cancer J Geriatr Oncol 10210–2152019 [DOI] [PubMed] [Google Scholar]
- 33.Festen S, Kok M, Hopstaken JS, et al. How to incorporate geriatric assessment in clinical decision-making for older patients with cancer. An implementation study J Geriatr Oncol 10951–9592019 [DOI] [PubMed] [Google Scholar]
- 34. doi: 10.1016/j.jgo.2015.07.005. Baitar A, Kenis C, Moor R, et al: Implementation of geriatric assessment-based recommendations in older patients with cancer: A multicentre prospective study. J Geriatr Oncol 6:401-410, 2015 [Erratum: J Geriatr Oncol 7:142-143, 2016] [DOI] [PubMed] [Google Scholar]
- 35.Kenis C, Heeren P, Bron D, et al. Multicenter implementation of geriatric assessment in Belgian patients with cancer: A survey on treating physicians’ general experiences and expectations J Geriatr Oncol 5431–4382014 [DOI] [PubMed] [Google Scholar]
- 36.Kenis C, Decoster L, Flamaing J, et al. Adherence to geriatric assessment-based recommendations in older patients with cancer: A multicenter prospective cohort study in Belgium Ann Oncol 291987–19942018 [DOI] [PubMed] [Google Scholar]
- 37.Kenis C, Heeren P, Decoster L, et al. A Belgian survey on geriatric assessment in oncology focusing on large-scale implementation and related barriers and facilitators J Nutr Health Aging 2060–702016 [DOI] [PubMed] [Google Scholar]
- 38.Jonker JM, Smorenburg CH, Schiphorst AH, et al. Geriatric oncology in the Netherlands: A survey of medical oncology specialists and oncology nursing specialists Eur J Cancer Care (Engl) 23803–8102014 [DOI] [PubMed] [Google Scholar]
- 39.Loh KP, Ramsdale E, Culakova E, et al. Novel mHealth app to deliver geriatric assessment-driven interventions for older adults with cancer: Pilot feasibility and usability study. JMIR Cancer. 2018;4:e10296. doi: 10.2196/10296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nathwani N, Kurtin SE, Lipe B, et al. Integrating touchscreen-based geriatric assessment and frailty screening for adults with multiple myeloma to drive personalized treatment decisions JCO Oncol Pract 16e92–e992020 [DOI] [PubMed] [Google Scholar]
- 41.McCleary NJ, Wigler D, Berry D, et al. Feasibility of computer-based self-administered cancer-specific geriatric assessment in older patients with gastrointestinal malignancy Oncologist 1864–722013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. doi: 10.1016/j.jgo.2019.10.020. Hsu T, Soto-Perez-de-Celis E, Burhenn PS, et al: Educating healthcare providers in geriatric oncology—A call to accelerate progress through identifying the gaps in knowledge. J Geriatr Oncol 11:1023-1027, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maggiore RJ, Callahan KE, Tooze JA, et al. Geriatrics fellowship training and the role of geriatricians in older adult cancer care: A survey of geriatrics fellowship directors Gerontol Geriatr Educ 39170–1822018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Magnuson A, Dale W, Mohile S.Models of care in geriatric oncology Curr Geriatr Rep 3182–1892014 [DOI] [PMC free article] [PubMed] [Google Scholar]