Abstract
PURPOSE:
Although hope has been explored in patients, few studies have investigated hopefulness in health care professionals. We surveyed oncology professionals within the SWOG Cancer Research Network, exploring relationships among personal hopefulness, social support, work stress, burnout, and life satisfaction. We hypothesized that hope would mediate the relationships between these other variables and life satisfaction.
METHODS:
SWOG members were randomly selected for an online survey containing measures of hope, social support, work stress, burnout, and satisfaction with life. Of 1,000 invitees, 226 responded.
RESULTS:
We tested a multiple mediational model using Hayes' bootstrapping approach (ie, PROCESS v3.4). As hypothesized, hope partially mediated the relationships between burnout and life satisfaction as well as between social support and life satisfaction. In particular, hopefulness was associated with lower burnout (−0.23; P = .005), greater social support (0.23; P = .005), and greater life satisfaction (0.50; P < .001). Work stress was associated with greater burnout (0.57; P < .001) but was not associated with general life satisfaction. Finally, social support was associated with lower burnout (−0.16; P = .005) and greater life satisfaction (0.24; P < .001).
CONCLUSION:
Our results suggest that hope may mitigate the effects of burnout. The combination of hope and social support may prove helpful for reducing burnout and improving life satisfaction. Single-session hope-enhancement interventions incorporating both hope and social support have previously been shown to increase hope and well-being in non–health care professionals. Such interventions for health care providers warrant further study.
INTRODUCTION
For many patients and their caregivers, treatment trials in oncology constitute a mechanism for restoring hopefulness in clinical contexts that are potentially dire.1 This intense craving for hope is manifest in patients' willingness to participate in risk-laden studies (eg, testing orphan drugs for rare diseases)2 and even to enroll in phase I trials where cure is effectively unattainable.3
However, clinical investigators may have a more complex relationship with hope than the patients they recruit to participate in studies. A recent statistical analysis of the content of nearly two decades of articles in two high-impact journals (Journal of Clinical Oncology and JAMA Oncology) found that investigators appear increasingly reluctant to use the language of hope when publishing original research, even as cancer death rates have dropped.4 Curiously, authors use the word hope significantly more frequently in narrative essays in these same journals, which seems to affirm the importance of hope in investigators' own lives.
Little is known empirically about the role of hope in the lives of oncology investigators and providers. What is increasingly recognized, however, are the pernicious effects of work stress and burnout for health care providers in general and cancer care clinicians in particular. On average, health care professionals experience relatively high levels of work stress,5-8 which in turn predict burnout.9,10 Much has been written about physician burnout in recent years, particularly given its relationships with poorer patient care11,12 and the increased costs to the medical system attributable to lost clinical hours and job turnover.13,14 Similar concerns have been noted in other health care professions.15
There is reason to believe that higher hope is associated with lower burnout. Rushton et al16 found correlations (r's = −0.31 to −0.34) between hope and burnout among nurses working in six highly stressful units (two pediatric or neonatal, two oncology, and two adult critical care) in four hospitals. Sherwin et al17 observed a similar relationship among nurses in chronic-care rehabilitation units. This relationship has also been documented in samples of social workers,18 first responders,19 and assisted living employees (eg, certified nursing assistants and dieticians).20 Finally, one study examined this relationship in physicians finding a similar association between hopefulness and lower burnout (among members of the Society of Gynecologic Oncology).21
Authors frequently call for an increased focus on the well-being of health care professionals, which is often used as an antonym for burnout.22 Well-being is a much broader term, of course, encompassing overall satisfaction with life, not merely a lack of difficulties at work. In comparison with burnout, less is known about the factors that predict life satisfaction among physicians and other health care professionals. To what degree and how burnout plays a role in overall life satisfaction are still open questions. As is well-known, however, physicians have elevated rates of suicidality compared with the general population.23,24 Accordingly, the American Foundation for Suicide Prevention produced a consensus statement calling for research concerning possible risk and protective factors related to the mental health and well-being of physicians.25 Hope may constitute one such protective factor.
C. R. Snyder's Hope Theory26 is the most extensively cited conceptualization of hope in the social science research literature. Hope Theory defines hope as a measurable, cognitive, goal-directed phenomenon. In particular, Snyder et al operationalize hope as a “cognitive set that is based on a reciprocally-derived sense of successful agency (goal-directed determination) and pathways (planning to meet goals).” Within this model, goals consist of anything that individuals desire to get, do, be, experience, or create. Agency consists of people's beliefs regarding their ability to initiate and maintain movement toward goals. These agency beliefs provide motivation, particularly when faced with setbacks. Finally, pathways are plans or strategies that one believes will lead to goals. People high in hope tend to habitually produce many pathways toward goals in anticipation of potential obstacles. In sum, people are hopeful when they believe they are likely (through their motivated action and plans) to reach desired outcomes.
A self-report measure of this model of hope, the Adult Hope Scale, includes items tapping goal-directed agency and pathways.26 Multiple studies show links between this measure and greater life satisfaction in a variety of populations, including college students,27,28 adolescents and adults,29 individuals with mild intellectual disability,30 and patients with cancer.31 In addition, higher levels of hope appear to be related to better health, whether physical or emotional. Higher hope is associated with being a nonsmoker,32 regular physical activity,33 and salutary dietary habits.34,35 People with higher hope cope better with chronic pain than their lower-hope counterparts and also report lower levels of depression and anxiety.36,37 Finally, women with breast cancer who have higher hope tend to cope in ways consistent with a fighting spirit, whereas lower-hope women are more likely to report a sense of helplessness or anxious preoccupation with the disease.38
In addition to hope, another factor associated with life satisfaction is social support. Perceived support from family and friends has been shown to robustly and consistently relate to life satisfaction in populations including young adults,39 older adults,40 individuals with end-stage renal disease,41 and people living with HIV.42 Moreover, in a recent survey of health care professionals working in hospice and palliative care settings, more than half cited “talking with family, friends, and significant others for support” as an essential strategy they use to manage burnout.6 Thus, any investigation of the factors associated with life satisfaction or burnout should include social support.
To clarify the relationships among hope, social support, job stress, burnout, and satisfaction with life, we conducted a survey of oncology professionals within the SWOG Cancer Research Network, an organization comprising clinical practitioners, investigators, and other professionals dedicated to cancer prevention and care delivery. Although hope and its relationship to life satisfaction have been studied relatively extensively in patients, they have been studied infrequently in health care professionals. Moreover, although informative, none of the research detailed above examined the simultaneous relationships among hope, social support, work stress, burnout, and life satisfaction. In the present study, we test the relationships among these variables in a single statistical model. This is important because the determinants of outcomes such as life satisfaction and burnout are likely to be multifactorial. Consequently, we use a multiple mediation model to examine the interrelatedness of these factors.
METHODS
Participants
A total of 1,000 SWOG members were randomly selected from the organization's membership database and invited to participate in the survey. Random selection reflected a cross-section of professions most commonly represented in SWOG (see Table 1 for sample characteristics). To maintain anonymity, invitation emails were sent directly from the SWOG operations office; names and other identifying information were not collected. The survey was voluntary, and there was no material incentive to participate. For four consecutive months (September-December 2019), members were sent reminder emails. The study was approved by the SWOG Executive Committee and Santa Clara University Institutional Review Board.
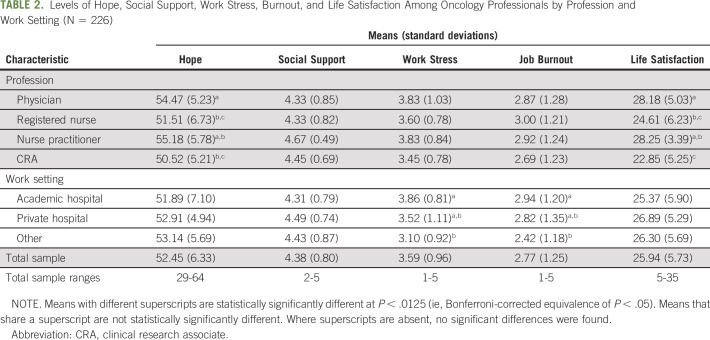
TABLE 1.
Sample Demographics (N = 226)
Instruments and Data Collection
Participants clicked on a link in the invitation email and were taken to an online survey, which was field-tested to confirm that it required < 10 minutes. After providing informed consent, participants completed the following measures: Hope was assessed using the Adult Hope Scale,26 a 12-item measure yielding scores from 8 to 64 (α = .87); higher scores represent greater hopefulness. General life satisfaction was assessed using the Satisfaction with Life Scale,43 a five-item measure yielding scores from 7 to 35 (α = .89); higher scores indicate greater life satisfaction. Single items assessed work stress (Please choose a number on the scale below to indicate the degree of stress you experience in your work), burnout (Please choose a number on the scale below to indicate the degree to which you consider yourself burned out in your work), and social support (Please choose a number on the scale below to indicate the degree to which you believe you have social and emotional support in your personal life—eg, spouse, family, friends, etc). These items were rated on five-point Likert scales. Finally, demographics were collected, including age, gender, ethnicity, profession, and work environment (academic, private, and other).
Statistical Analysis
Demographic data were summarized using descriptive statistics (counts, percentages, means, and standard deviations). Bivariate relationships among continuous variables were analyzed using Pearson correlations, and analysis of variance (ANOVA) was used to compare means of continuous variables between groups (eg, professions and work settings). Statistical modeling was performed via Hayes' bootstrapping approach to multiple mediation using PROCESS v3.4 within the SPSS software package.44 As mentioned, the PROCESS procedure allows researchers to analyze the relationships among a variety of variables simultaneously. In the case of the present study, this analysis facilitated a more comprehensive assessment of the factors that combine to predict participants' satisfaction with life.
RESULTS
Demographics
Of the 1,000 members invited to participate, 226 completed the survey, a response rate (22.6%) similar to past surveys of medical professional organizations.21 Table 1 describes sample characteristics. The most frequent age group was 35-44 years (32.3%) and most respondents were female (73.7%) and White (77.9%). The sample included a range of professions, with medical oncologists (n = 47) and registered nurses (RNs; n = 46) being the most common. The Other category (n = 49) consisted of a highly heterogeneous mixture of professionals, with the most frequently cited being clinical research coordinators (n = 7) and pharmacists (n = 3). Most participants reported working in academic medical centers (52.7%), with fewer working in private medical centers (21.7%) and other work environments (25.7%) such as community hospitals (n = 5), private practices (n = 4), and Veterans Affairs hospitals (n = 3).
Associations of Hope, Social Support, Work Stress, Burnout, and Life Satisfaction With Profession and Work Setting
Table 2 describes levels of hope, social support, job stress, burnout, and life satisfaction across professions and work settings. We first performed ANOVAs to test for differences among professions on these variables. It should be noted that a number of professions were only endorsed by a small number of participants. Therefore, to ensure more stable mean comparisons, we limited our analyses to professions endorsed by 10 or more participants (Table 2). Because two physician specialties (radiation oncology and palliative medicine) were represented by fewer than 10 participants, we combined all physicians into a single category.
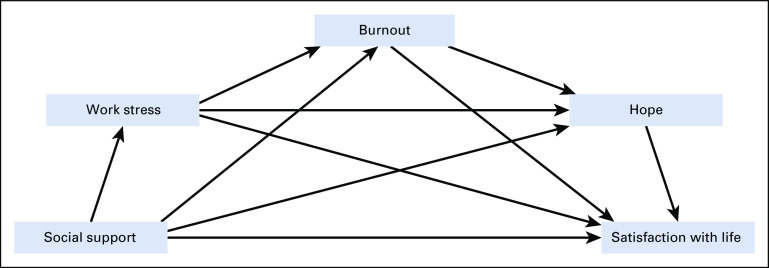
TABLE 2.
Levels of Hope, Social Support, Work Stress, Burnout, and Life Satisfaction Among Oncology Professionals by Profession and Work Setting (N = 226)
Statistically significant differences among professions emerged only for hope (F(3,149) = 4.78; P = .003) and life satisfaction (F(3,149) = 4.78; P = .003). Although these omnibus ANOVAs were statistically significant, follow-up analyses revealed relatively few differences once Bonferroni corrections were applied. As can be seen in Table 2, there were higher mean levels of hope for physicians (54.47) than RNs (51.51) and clinical research associates (CRAs; 50.52). For life satisfaction, there were higher mean levels for physicians (28.18) than RNs (24.61) and CRAs (22.85), as well as higher mean levels for nurse practitioners (28.25) than CRAs (22.85). According to established cutoff scores for the Satisfaction with Life Scale, 0.4% of the total sample was classified as highly dissatisfied with life, 4.4% as dissatisfied, 8.8% as slightly dissatisfied, 18.1% as slightly satisfied, 34.1% as satisfied, and 29.2% as highly satisfied.45
Regarding work settings, no differences in hope, life satisfaction, or social support were found. However, the omnibus ANOVA for work stress (F(2,221) = 14.00; P < .001) and job burnout (F(2,221) = 3.60; P = .03) were statistically significant. Follow-up analyses revealed mean differences only between individuals who reported working in academic medical center environments (3.86 and 2.94 for stress and burnout, respectively) and those choosing the other work environment option (3.10 and 2.42 for stress and burnout, respectively).
Mediational Modeling of Factors Accounting for Burnout and Life Satisfaction
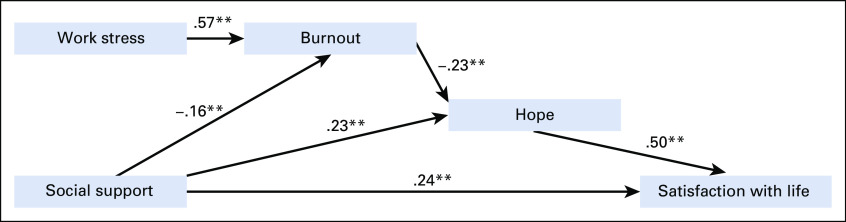
Bivariate Pearson correlations for continuous variables are presented in Table 3. Mediational analyses were performed via Hayes' bootstrapping approach to multiple mediation (model 6 in PROCESS v3.4).44 This procedure allows for the simultaneous evaluation of the statistical effects of multiple factors on an outcome. Figure 1 depicts the hypothesized model. This diagram proceeds from left to right, with variables to the left hypothesized to predict variables to the right and variables in the middle serving as mediators. As can be seen, hope is hypothesized to mediate the relationships of work stress, job burnout, and social support with general life satisfaction. In addition, greater social support is hypothesized to have a direct relationship with higher life satisfaction. Finally, work stress is expected to be directly associated with job burnout.
TABLE 3.
Pearson Correlations Among Oncology Professionals (N = 226)
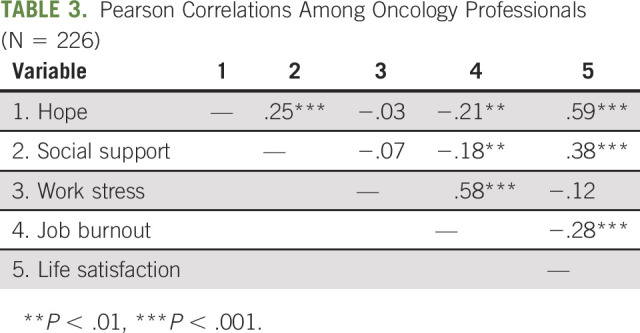
FIG 1.
Hypothesized model.
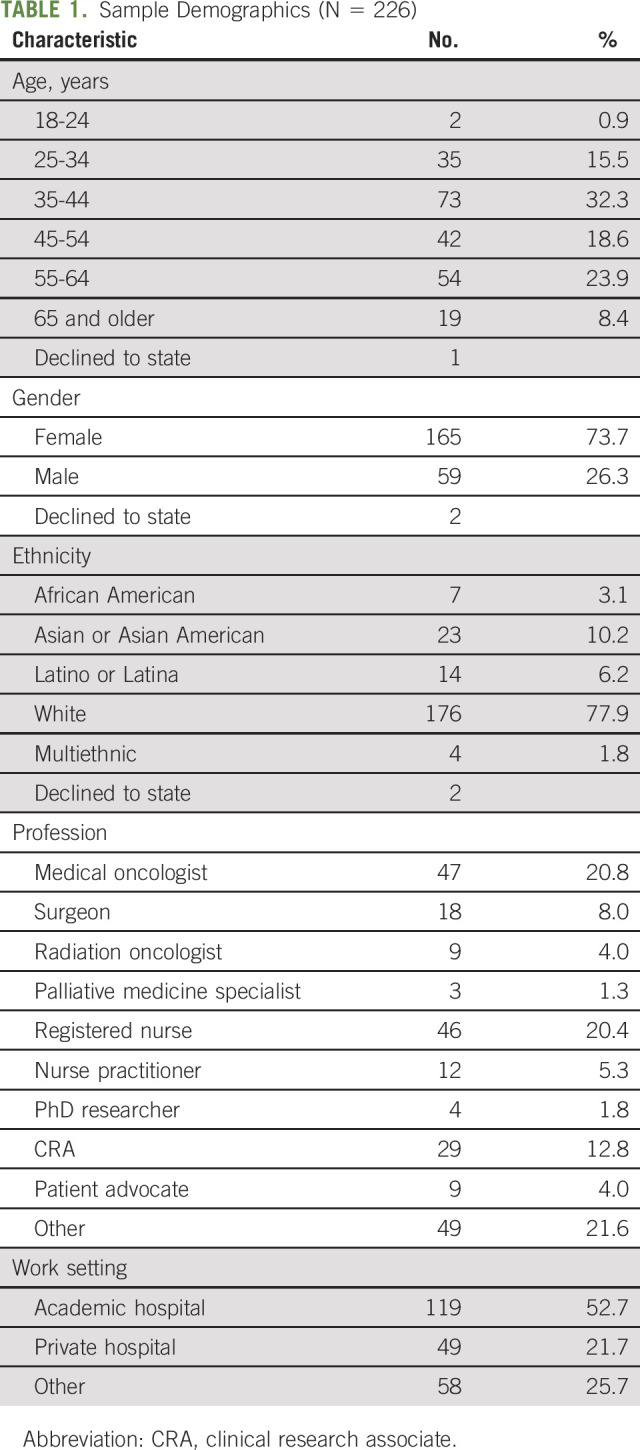
Figure 2 depicts statistically significant paths after performing the analysis. Standardized coefficients represent the strengths of relationships. The relationship between social support and life satisfaction was partially mediated by burnout and hope, as indicated by the fact that the values falling between the lower limit (BootLLCI = 0.031) and upper limit (BootULCI = 0.292) of the 95% bootstrapping CI for this mediated path did not include zero. That is, there were statistically significant paths from social support to burnout (−0.16; P = .005), from burnout to hope (−0.23; P = .005), and from hope to life satisfaction (0.50; P < .001). Hope, by itself, further mediated the relationship between social support and life satisfaction (BootLLCI = 0.371, BootULCI = 1.369), which is represented by the statistically significant paths from social support to hope (0.23; P = .001) and from hope to life satisfaction (0.50; P < .001). In addition, there was a direct relationship from social support to life satisfaction (0.24; P < .001).
FIG 2.
Statistically significant paths with standardized coefficients. **P < .01.
Finally, work stress was directly associated with job burnout (0.57; P < .001). Of note, however, neither work stress nor burnout was directly associated with life satisfaction. Instead, as previously mentioned, the relationship between higher burnout and lower life satisfaction was mediated through lower hope. Finally, the direct relationship between hope and life satisfaction was significant and relatively large (0.50; P < .001).
DISCUSSION
During the past two decades, investigators have endeavored to identify alterable factors contributing to burnout in health care environments.11,46 Perhaps not surprisingly, in the present study, we observed a direct relationship between work stress and job burnout. However, neither work stress nor burnout had direct relationships with life satisfaction when all variables were considered together in the mediational analysis. Instead, the relationship between burnout and life satisfaction was mediated by hope. This demonstrates the value of testing a collective statistical model; our model allows for the determination that burnout's apparent relationship with life satisfaction is due almost entirely to both these variables' relationships with hope. Although relatively little research has tested the association between job burnout and overall life satisfaction, an earlier study noted a similar lack of direct relationship.47
Hope's robust (0.50) relationship with life satisfaction is also consistent with past research, which has found a similar relationship in college students,27,28 adolescents and adults,29 individuals with mild intellectual disability,30 and patients with cancer,31 among other populations. As measured in this study, hope is conceptualized as a positive perception of the future on the basis of a combination of pathways (goal-directed planning) and agency (goal-directed motivation). Research demonstrates that this sense of goal-directed hope predicts later accomplishment of goals.48 To the degree that people create satisfying lives through pursuing and accomplishing goals, it makes sense that hope would be strongly related to their overall positive assessment of life.
Social support also exhibited a direct relationship with life satisfaction. This finding is consistent with aforementioned research demonstrating that support from family and friends predicts satisfaction with life in a variety of populations.39-42 To our knowledge, this is the first study to document this relationship in health care professionals. In the present study, social support also exhibited relationships with hope and burnout. In fact, in addition to mediating between burnout and life satisfaction, hope also mediated the relationship between social support and life satisfaction.
As with all research, the present study has limitations. First, it was cross-sectional, so appropriate caution should be used in drawing causal conclusions. Second, single-item measures were used to assess work stress, burnout, and social support. As is common practice, this was done to keep the survey to a manageable length and maximize participation. Given our results, however, researchers should consider replicating the present relationships using longer-form, standardized measures of these factors. Finally, given the particular age range and imbalanced gender distribution of the sample, care should be taken in generalizing the results.
Despite these limitations, these findings have potential implications for increasing life satisfaction in oncology professionals. As mentioned, our cross-sectional design prohibits drawing causal conclusions. Nonetheless, our results are consistent with the notion that job stress and burnout may not directly affect individuals' life satisfaction. Instead, these variables may decrease life satisfaction through their ability to affect hope. In addition, support from family and friends may increase hopefulness as well as life satisfaction. Therefore, practitioners and administrators motivated to improve health care professionals' overall satisfaction with life may consider investing in interventions emphasizing hope and social support, not simply job stress or burnout interventions, per se.
Brief, cost-effective interventions to enhance hope already exist. These are typically delivered in group formats, which also encourage social support. Feldman and Dreher,49 for instance, developed a single-session group hope workshop, with demonstrated capacity to increase hope and sense of meaning or purpose in participants' lives and work. The same intervention was also shown to predict goal achievement and grade point average among college students.50 More intensive, multisession hope interventions have also been applied to adult outpatients with a variety of mental disorder diagnoses,51 African American gay men with HIV,52 and older adults with depression,53 among other populations.
Informed by these findings, SWOG leadership (C. Blanke, personal communication, July 2020) has agreed to pilot test a hope-enhancement workshop for members participating in the organization's semi-annual group meeting. At present, there are plans to offer the workshop to three separate populations: physicians, nurses, and patient advocates. Given current COVID-19 social distancing guidelines and diminished opportunity for traditional in-person meetings, the aforementioned Feldman and Dreher intervention49 is being converted to a virtual platform. Downstream, it is possible that such workshops will also be studied as an adjunct to treatment trials for patients with cancer conducted by the SWOG Cancer Research Network. Such efforts may afford further insights regarding the methods and effects of fostering hope and life satisfaction in providers and patients.
Footnotes
D.B.F. and B.W.C. contributed equally to this work.
AUTHOR CONTRIBUTIONS
Conception and design: David B. Feldman, Mark A. O'Rourke, Marie A. Bakitas, Heidi E. Deininger, Benjamin W. Corn
Administrative support: David B. Feldman, Mark A. O'Rourke, Marie A. Bakitas
Financial support: Marie A. Bakitas
Provision of study materials or patients: David B. Feldman, Marie A. Bakitas
Collection and assembly of data: David B. Feldman, Marie A. Bakitas, Robert S. Krouse
Data analysis and interpretation: David B. Feldman, Marie A. Bakitas, Robert S. Krouse, Matthew F. Hudson
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Hope, Burnout, and Life Satisfaction: An Intriguing Trinity Among Investigators of the SWOG Cancer Research Network
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.Sapir E, Corn BW.Clinical trialism and the bedrock of hope Int J Radiat Oncol Biol Phys 108876–8782020 [DOI] [PubMed] [Google Scholar]
- 2.Wastfelt M, Fadeel B, Henter JI.A journey of hope. Lessons from studies on rare diseases and orphan drugs J Intern Med 2601–102006 [DOI] [PubMed] [Google Scholar]
- 3.Weinfurt K, Castel LD, Li Y, et al. The correlation between patient characteristics and expectations of benefit from phase I clinical trials Cancer 98166–1752003 [DOI] [PubMed] [Google Scholar]
- 4.Corn BW, Feldman DB, Schapira L, et al. Oncologists reluctance to use the terms hope and cure: A bibliometric analysis from two high-impact journals. JNCI Cancer Spectrum. 2020 doi: 10.1093/jncics/pkaa065. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaghini F, Biagioli V, Proietti M, et al. The role of occupational stress in the association between emotional labor and burnout in nurses: A cross-sectional study. Appl Nurs Res. 2020;54:151277. doi: 10.1016/j.apnr.2020.151277. [DOI] [PubMed] [Google Scholar]
- 6.Kamal AH, Bull JH, Wolf SP, et al. Prevalence and predictors of burnout among hospice and palliative care clinicians in the US J Pain Symptom Manage 596–132020 [DOI] [PubMed] [Google Scholar]
- 7.Siegrist J, Shackelton R, Link C, et al. Work stress of primary care physicians in the US, UK and German health care systems Soc Sci Med 71298–3042010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virtanen P, Oksanen T, Kivimäki M, et al. Work stress and health in primary health care physicians and hospital physicians Occup Environ Med 65364–3662008 [DOI] [PubMed] [Google Scholar]
- 9.Peiró JM, González-Romá V, Tordera N, et al. Does role stress predict burnout over time among health care professionals? Psychol Health 16511–5252001 [DOI] [PubMed] [Google Scholar]
- 10.Wu SY, Li HY, Wang XR, et al. A comparison of the effect of work stress on burnout and quality of life between female nurses and female doctors Arch Environ Occup Health 66193–2002011 [DOI] [PubMed] [Google Scholar]
- 11.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program Ann Intern Med 136358–3672002 [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons Ann Surg 251995–10002010 [DOI] [PubMed] [Google Scholar]
- 13.Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States Ann Intern Med 170784–7902019 [DOI] [PubMed] [Google Scholar]
- 14.Willard-Grace R, Knox M, Huang B, et al. Burnout and health care workforce turnover Ann Fam Med 1736–412019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoff T, Carabetta S, Collinson GE.Satisfaction, burnout, and turnover among nurse practitioners and physician assistants: A review of the empirical literature Med Care Res Rev 763–12019 [DOI] [PubMed] [Google Scholar]
- 16.Rushton CH, Batcheller J, Schroeder K, et al. Burnout and resilience among nurses practicing in high-intensity settings Am J Crit Care 24412–4202015 [DOI] [PubMed] [Google Scholar]
- 17.Sherwin ED, Elliott TR, Rybarczyk BD, et al. Negotiating the reality of caregiving: Hope, burnout and nursing J Soc Clin Psychol 11129–1391992 [Google Scholar]
- 18.Schwartz RH, Tiamiyu MF, Dwyer DJ.Social worker hope and perceived burnout: The effects of age, years in practice, and setting Adm Soc Work 31103–1192007 [Google Scholar]
- 19.Yotsidi V, Kourmousi N, Dermitzaki E, et al. “Add Flow to the Fire”: Flow and hope as a shield against burnout of fire service workers Psychology 291291–13052018 [Google Scholar]
- 20.Simmons BL, Gooty J, Nelson DL, et al. Secure attachment: Implications for hope, trust, burnout, and performance J Org Behav 30233–2472009 [Google Scholar]
- 21.Vetter MH, Vetter MK, Fowler J.Resilience, hope and flourishing are inversely associated with burnout among members of the Society for Gynecologic Oncology Gynecol Oncol Rep 2552–552018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shanafelt TD, Dyrbye LN, West CP.Addressing physician burnout: The way forward JAMA 31901–9022017 [DOI] [PubMed] [Google Scholar]
- 23.Schernhammer ES, Colditz GA.Suicide rates among physicians: A quantitative and gender assessment (meta-analysis) Am J Psychiatry 1612295–23022004 [DOI] [PubMed] [Google Scholar]
- 24.McFarland DC, Hlubocky F, Susaimanickam B, et al. Addressing depression, burnout, and suicide in oncology physicians Am Soc Clin Oncol Educ Book 39590–5982019 [DOI] [PubMed] [Google Scholar]
- 25.Davis M, Detre T, Ford DE, et al. Confronting depression and suicide in physicians: A consensus statement JAMA 2893161–31662003 [DOI] [PubMed] [Google Scholar]
- 26.Snyder CR, Harris C, Anderson JR, et al. The will and the ways: Development and validation of an individual differences measure of hope J Personal Soc Psychol 60570–5851991 [DOI] [PubMed] [Google Scholar]
- 27.Bailey TC, Eng W, Frisch MB, et al. Hope and optimism as related to life satisfaction J Posit Psychol 2168–1752007 [Google Scholar]
- 28.Thakur MB.Examining the association between hope, optimism, self-esteem and life satisfaction: The Indian Context J Psychosoc Res 1323–312018 [Google Scholar]
- 29.Bronk KC, Hill PL, Lapsley DK, et al. Purpose, hope, and life satisfaction in three age groups J Posit Psychol 4500–5102009 [Google Scholar]
- 30.Santilli S, Nota L, Ginevra MC, et al. Career adaptability, hope and life satisfaction in workers with intellectual disability J Voc Behav85:67-74, 2014 [Google Scholar]
- 31.Jafari E, Najafi M, Sohrabi F, et al. Life satisfaction, spirituality well-being and hope in cancer patients Proc Soc Behav Sci 51362–13662010 [Google Scholar]
- 32.Berg AT, Shauer GG, Rodgers K, et al. College student smokers: Former versus current and non-smokers Am J Prev Med 43S229–S23620125 suppl 3 [DOI] [PubMed] [Google Scholar]
- 33.Anderson CL, Feldman DB.Hope and physical exercise: The contributions of hope, self-efficacy, and optimism in accounting for variance in exercise frequency Psychol Rep 1231145–11592020 [DOI] [PubMed] [Google Scholar]
- 34.Nolen N, Befort C, Pulvers K, et al. Demographic and psychological factors associated with increased fruit and vegetable consumption among smokers enrolled in public housing enrolled in a ransomed trial Health Psychol 27S252–S2592008 [DOI] [PubMed] [Google Scholar]
- 35.Nothwehr F, Clark DO, Perkins A.Hope and the use of behavioral strategies related to diet and physical activity J Hum Nutr Diet 26159–1632013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hood A, Pulvers K, Carrillo J, et al. Positive traits linked to less pain through lower pain catastrophizing Pers Individ Diff 52401–4052012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Howell AJ, Jacobsen RM, Larsen DJ.Enhanced psychological health among chronic pain clients engaged in hope-focused group counseling Couns Psychol 43586–6132015 [Google Scholar]
- 38.Hasson-Ohayon I, Braun M, Galinsky D, et al. Religiosity and hope: A path for women coping with a diagnosis of breast cancer Psychosomatics 50525–5332009 [DOI] [PubMed] [Google Scholar]
- 39.Trepte S, Dienlin T, Reinecke L.Influence of social support received in online and offline contexts on satisfaction with social support and satisfaction with life: A longitudinal study Media Psychol 1874–1052015 [Google Scholar]
- 40.Gow AJ, Pattie A, Whiteman MC, et al. Social support and successful aging: Investigating the relationships between lifetime cognitive change and life satisfaction J Individ Diff 28103–1152007 [Google Scholar]
- 41.Soykan A, Arapaslan B, Kumbasar H.Suicidal behavior, satisfaction with life, and perceived social support in end-stage renal disease Transplant Proc 351290–12912003 [DOI] [PubMed] [Google Scholar]
- 42.Heckman TG, Somlai AM, Sikkema KJ, et al. Psychosocial predictors of life satisfaction among persons living with HIV infection and AIDS J Assoc Nurses AIDS Care 821–301997 [DOI] [PubMed] [Google Scholar]
- 43.Diener E, Emmons RA, Larsen RJ, et al. Satisfaction with life scale (SWLS) J Personal Assess 4971–751985 [DOI] [PubMed] [Google Scholar]
- 44.Hayes AF. Introduction to Mediation, Moderation and Conditional Process Analysis. ed 2. New York, NY: Guilford Press; 2018. [Google Scholar]
- 45.Pavot W, Diener E. The Satisfaction with Life Scale (SWL). Measurement Instrument Database for the Social Sciences. 2013. www.midss.ie [Google Scholar]
- 46.West CP, Dyrbye LN, Sinsky C, et al. Resilience and burnout among physicians and the general US working population. JAMA Netw Open. 2020;3:e209385. doi: 10.1001/jamanetworkopen.2020.9385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hombrados-Mendieta I, Cosano-Rivas F.Burnout, workplace support, job satisfaction and life satisfaction among social workers in Spain: A structural equation model Int Soc Work 56228–2462013 [Google Scholar]
- 48.Feldman DB, Rand KL, Kahle-Wrobleski K.Hope and goal attainment: Testing a brief basic prediction of hope theory J Soc Clin Psychol 28479–4972009 [Google Scholar]
- 49.Feldman DB, Dreher DE.Can hope be changed in 90 minutes? Testing the efficacy of a single-session goal-pursuit intervention for college students J Happiness Stud 13745–7592012 [Google Scholar]
- 50.Davidson OB, Feldman DB, Margalit M.A focused intervention for first-year college students: Promoting hope, sense of coherence and self-efficacy J Psychol Interdiscip Appl 146333–3522012 [DOI] [PubMed] [Google Scholar]
- 51.Cheavens JS, Feldman DB, Gum A, et al. Hope therapy in a community sample: A pilot investigation Soc Indic Res 7761–782006 [Google Scholar]
- 52.Hergenrather KC, Geishecker S, Clark G, et al. A pilot test of the HOPE Intervention to explore employment and mental health among African American gay men living with HIV/AIDS: Results from a CBPR study AIDS Educ Prev 25405–4222013 [DOI] [PubMed] [Google Scholar]
- 53.Klausner EJ, Snyder CR, Cheavens J.A hope-based group treatment for depressed older adult outpatients Physical Illness and Depression in Ilder Adults Boston, MA: Springer; 2002295–310 [Google Scholar]