The dissemination and persistence of coronavirus disease 2019 (COVID-19) worldwide have increased recognition of the ability of this disease to cause brain lesions. Herein, we describe a patient with COVID-19-associated leukoencephalopathy with microhemorrhages, a pattern that has been previously described1 , 2.
A 62-year-old male patient with hypertension (managed with losartan, 100 mg/day) presented with upper respiratory symptoms that persisted for seven days, along with myalgia. Real-time reverse-transcription polymerase chain reaction testing of a nasopharyngeal swab sample confirmed SARS-CoV-2 infection. The patient was on mechanical ventilation for 37 days, and the lowest recorded blood oxygen saturation level was 90%. The platelet count was normal (311,000/mL).
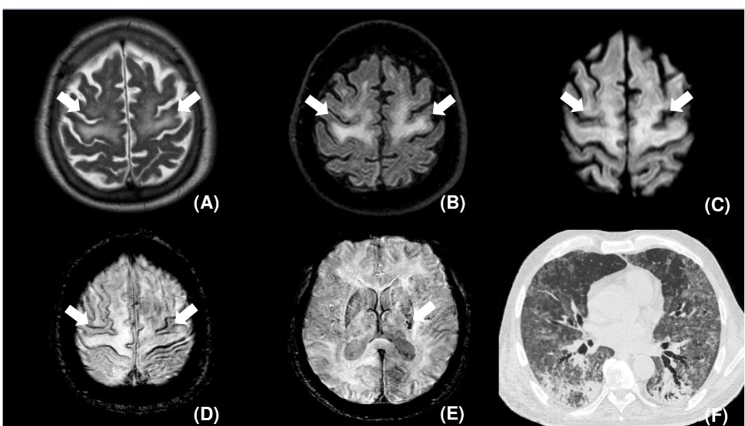
A brain magnetic resonance imaging (MRI) scan showed confluent symmetric T2 hyperintensity and restricted diffusion in the subcortical white matter of the precentral gyrus and the centrum semiovale, with small punctate hemorrhagic foci in the posterior limb of the left internal capsule and the subcortical white matter (Figure 1A-E ). Chest computed tomography revealed ground-glass opacities and consolidations in both lungs (Figure 1F ). The patient died three days after MRI.
FIGURE 1: Axial T2 (A), FLAIR (B), and diffusion (C) weighted images demonstrating symmetric diffuse hyperintensity (arrows) and mild restricted diffusion (arrows) involving the subcortical white matter in the precentral gyrus and the posterior portions of the superior and middle frontal gyrus. Axial susceptibility-weighted images, (D) and (E), depict punctate microhemorrhagic foci on the cortical surface of the precentral gyrus, middle frontal gyrus, and superior frontal gyrus (arrows in D) and in the posterior limb of the internal capsule (arrow in E). Chest CT, pulmonary window, axial: diffuse areas of ground-glass opacities and consolidations (F).
Although the findings in this case were nonspecific and may be observed in vasculitides1 , 3, acute hemorrhagic encephalomyelitis1 and delayed post-hypoxic leukoencephalopathy2, leukoencephalopathy, and microhemorrhages in critically ill patients with COVID-19 may be related to demyelination, endothelial lesions, and cytokine release syndrome1 , 2. These lesions may be viewed as potential late brain complications of COVID-19 in patients with a diminished mental status, and these patients usually have a poor prognosis1 , 2.
ACKNOWLEDGMENTS
We offer our deepest thanks to the institutions that provided technical support for the development and implementation of this study.
Footnotes
Financial Support: None.
REFERENCES
- 1.Sachs JR, Gibbs KW, Swor DE, Sweeney AP, Williams DW, Burdette JH, et al. COVID-19-associated leukoencephalopathy. Radiology. 2020;296(3):E184-E185. doi: 10.1148/radiol.2020201753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radmanesh A, Derman A, Lui YW, Raz E, Loh JP, Hagiwara M, et al. COVID-19-associated diffuse leukoencephalopathy and microhemorrhages. Radiology. 2020;297(1):E223-E227. doi: 10.1148/radiol.2020202040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Amorim JC, Torricelli AK, Frittoli RB, Lapa AT, Dertkigil SSJ, Reis F, et al. Mimickers of neuropsychiatric manifestations in systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2018;32(5):623–639. doi: 10.1016/j.berh.2019.01.020. [DOI] [PubMed] [Google Scholar]