Abstract
Training programs have the dual responsibility of providing excellent training for their learners and ensuring their graduates are competent practitioners. Despite everyone’s best efforts a small minority of learners will be unable to achieve competence and cannot graduate. Unfortunately, program decisions for training termination are often overturned, not because the academic decision was wrong, but because fair assessment processes were not implemented or followed. This series of three articles, intended for those setting residency program assessment policies and procedures, outlines recommendations, from establishing robust assessment foundations and the beginning of concerns (Part One), to established concerns and formal remediation (Part Two) to participating in formal appeals and after (Part Three). With these 14 recommendations on how to get a grip on fair and defensible processes for termination of training, career-impacting decisions that are both fair for the learner and defensible for programs are indeed possible. They are offered to minimize the chances of academic decisions being overturned, an outcome which wastes program resources, poses patient safety risks, and delays the resident finding a more appropriate career path. This article (Part Two in the series of three) will focus on what to do when concerns become established, and a formal remediation or probation is necessary.
Abstract
Les programmes de formation ont la double responsabilité de fournir une excellente formation aux apprenants et de s’assurer qu’à l’issue de celle-ci les diplômés sont des praticiens compétents. Malgré tous les efforts déployés, une petite minorité d’apprenants ne parviendra pas à atteindre le niveau de compétence requis pour obtenir son diplôme. Malheureusement, la décision de la direction du programme de mettre fin à la formation d’un étudiant est souvent annulée, non pas parce qu’elle n’était pas académiquement fondée, mais parce qu’on a omis d’appliquer ou de suivre un processus d’évaluation juste. Cette série de trois articles, destinée aux responsables des politiques et procédures d’évaluation des programmes de résidence, présente des recommandations concernant l’établissement de bases d’évaluation solides et l’émergence de préoccupations quant à la progression d’un résident dans le programme (première partie), les préoccupations confirmées et la remédiation formelle (deuxième partie), et enfin le processus d’appel formel et ses suites (troisième partie). La mise en œuvre de ces 14 recommandations sur la définition de processus justes et légitimes pour mettre fin à la formation d’un apprenant devrait permettre de prendre des décisions aux répercussions importantes pour la carrière qui sont néanmoins à la fois justes envers la personne et justifiées du point de vue du programme. Elles sont proposées pour éviter la révision des décisions de nature académique, qui entraîne un gaspillage de ressources pour le programme, pose des risques pour la sécurité des patients et retarde la recherche d’un cheminement de carrière plus approprié pour le résident. Cet article (le deuxième d’une série en trois parties) traite de ce qu’il faut faire lorsque les préoccupations sont établies et qu’une remédiation formelle ou une probation est nécessaire.
Introduction
This is the second article in a series of three (Parts One, Two, and Three) that outlines 14 recommendations for fair and defensible termination of residency training. This series is divided into five sections starting with A. Program Foundations followed by B. Beginnings of Concerns (Part One)1 C. Established concerns and Formal remediation/probation (Part Two) D. Legal challenges, and E. After the legal challenges (Part Three)2 (Table 1). The first article of this series outlined sections A. the program foundations that should be afforded all residents to optimize their competency development and B. steps to be taken when there are beginnings of concerns about a resident’s performance (Table 1). With these strong program foundations, most residents will progress as expected and develop into competent independent practitioners. A small number will struggle. Of these most will get back on track with individualized support. Despite adequate time and support however a small minority are unable to progress as required. There may be a failed rotation/clinical experience, significant professionalism issues, or stalled or regressing competency development. This second article, Part Two of the series of three, describes recommendations 7-10 of 14 on steps to take when there are established and persistent concerns.
Table 1.
Summary of recommended steps for fair and defensible processes leading to termination of training
| Steps for fair and defensible processes leading to termination of residency training | Core concepts | |
|---|---|---|
| Part One | ||
| A. | Program Foundations: | |
| 1. | Ensure trustworthy assessment practices | Multiple expert assessors assessing the desired competencies using performance standards, doing this over time and contexts, documenting these assessments and having a system to interpret the collated data looking for patterns and trajectory |
| 2. | Ensure fair assessment practices | Clear relevant documented performance standards, opportunities for competency development, observation by informed assessors, clear feedback with ideas for improvement, followed by more opportunities for improvement |
| 3. | Provide holistic resident support | Evaluating for and attending to other factors that could be impacting resident performance |
| B. | Beginnings of Concerns: | |
| 4. | Make an educational diagnosis | Consideration of the situation holistically to determine the issue(s) negatively impacting clinical performance and addressing those |
| 5. | Bring concerns forward to an educational group | Separate informed body to review assessment data and any performance impacting factors to inform learning plans and summative decisions if need be |
| 6. | Start a documentation trail early | Documentation of all discussions and interventions pertaining to items 1-3, dated to create a timeline |
| Part Two | ||
| C. | Established Concerns | |
| 7. | Carefully create the remediation/probation plan | Use of an institutional template if available using deliberate unambiguous language with attention to practical and achievable interventions considering the reality of the workplace |
| 8. | Disseminate and review the plan with all involved. | Review of the plan with all involved ensuring program personnel (supervisors, education leaders) understand and can meet the requirements laid out in the plan and the resident has understood the plan and signed and dated each page as evidence of that understanding |
| 9. | Carryout the plan | Scrupulous attention to carrying out all elements of the plan. Support for all throughout |
| 10. | Determine the outcome | Outcome decision made by an independent assessment group |
| Part Three | ||
| D. | Challenges to program decisions: | |
| 11. | Preparation for the review | Review of all documentation and legal submissions and compiling evidence to justify the program decision |
| 12. | Participation in the review | Being adequately prepared for cross-examination both with documentation and mental mind set |
| E. | After the review. | |
| 13. | Improve program processes | Use of the review board’s findings to improve any weaknesses in assessment processes |
| 14. | Support the learner. | Career counselling if training is terminated |
C. Established concerns
At this point a formal remediation or probation (R/P) will be undertaken. In most settings there will be an institutional policy (e.g. an Assessment, Promotions and Appeal Policy) that will outline the process for remediation or probation and may include templates for formal R/P plans. R/P involves four fundamental steps—creating, disseminating/reviewing and carrying out the plan, and deciding on the outcome.
Recommendation 7: carefully create the remediation/probation plan
This plan will likely be drafted by an individual within the program, often the program director. Once drafted it should be reviewed by the program’s assessment group (e.g. competency committee or residency program committee) looking for inconsistencies and omissions with an eye to practicality. When completing the plan, it is critical to be very deliberate about wording and process. Expectations for all aspects of the plan (e.g. expectations for what constitutes a successful outcome, what resources will be provided, what assessments will be done and when, when feedback meetings will occur) should be clear and unambiguous to minimize loopholes, while also being practical and achievable, with forethought given to the reality of the plan’s execution in the busy clinical environment. Perfection, when it comes to executing plans in the clinical setting, is nearly impossible. Case law supports that process need not be perfect if fairness is not compromised because of deviation from a plan.3 However, any time there is a deviation (e.g. a feedback meeting is delayed by more than a few days or a daily assessment isn’t documented (if it isn’t documented it is assumed not to have occurred)) the review board must determine if it was significant enough to affect the resident’s likelihood of success. Minimizing the need for them to deliberate about any deviations and the extent of the resulting impact, through careful forethought of realistic plan execution, is time well spent.
In our institution we have another level of review of R/P plans, that of an Educational Advisory Board. This group of educators from a number of different programs reviews all R/P plans from all residency programs before they are put in place. The EAB affords another opportunity to look for issues with the R/P plan. In addition, this group has built up a repository of resources for remediation and, through following outcomes of different R/Ps have been able to iteratively build up ideas about best procedural practices for R/P, more so than any one program director from any single program could. Their input is very valuable.
Recommendation 8: disseminate and review the plan with all involved
Everyone involved in the R/P should be aware of the details of the plan. The resident must be given the opportunity to review the plan, understand the objectives of the remediation plan, their responsibilities and clarify any aspects of the plan they are unsure about. They should initial and date each page and fully sign and date the last page, providing evidence of this review. A list summarizing what was reviewed at the end of the plan for the resident to tick and sign is helpful (Figure 1). Documenting this meeting provides further evidence of that review. Going over the plan with the preceptor(s), and the resident’s academic advisor or competency coach if they have one, ensures they too understand the objectives of the remediation and their roles and responsibilities.
Figure 1.
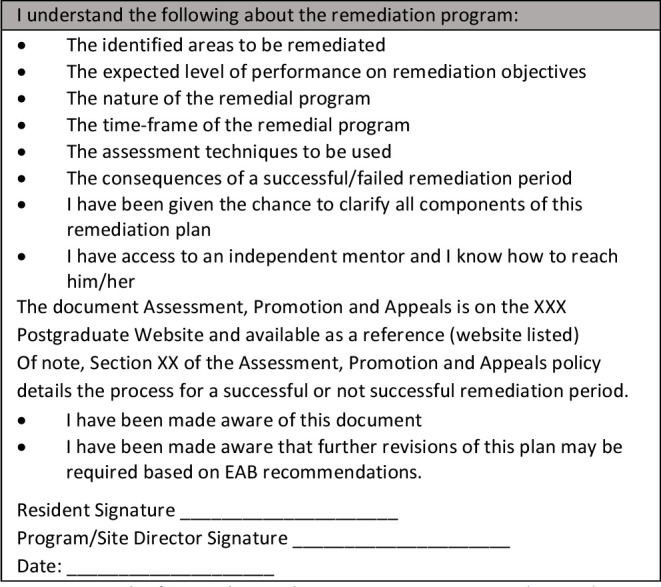
Example of a remediation plan summary questions. A probation plan would have a similar list. Each item should be reviewed and checked off by the resident, with a full signature of the resident and Program (or Site) Director and date. (EAB= education advisory board which is a board at our institution that reviews all R/P plans and makes suggestions for improvement before their implementation)
It is helpful to develop a checklist about critical information for those meetings (Figure 2). If preceptors have concerns that elements of the plan cannot be carried out in their environment, then adaptations (and re-review with the resident) must be made or a new preceptor/setting found, as all gaps in process will be challenged by the resident’s lawyer as failures in fulfilling the program’s obligations and, as a result, denial of a fair assessment process. Stress to the preceptors the critical importance of feedback, particularly around the identified areas for improvement outlined in the remediation plan, and need for fulsome explicit narrative in assessment documents, both as evidence of clear guidance for the resident and so that the review board will have illustrative examples of performance that informed final decisions. Reviewing best feedback practices, including providing literature4 to preceptors, is helpful. This will take preceptors more time than usual and may require additional compensation.
Figure 2.
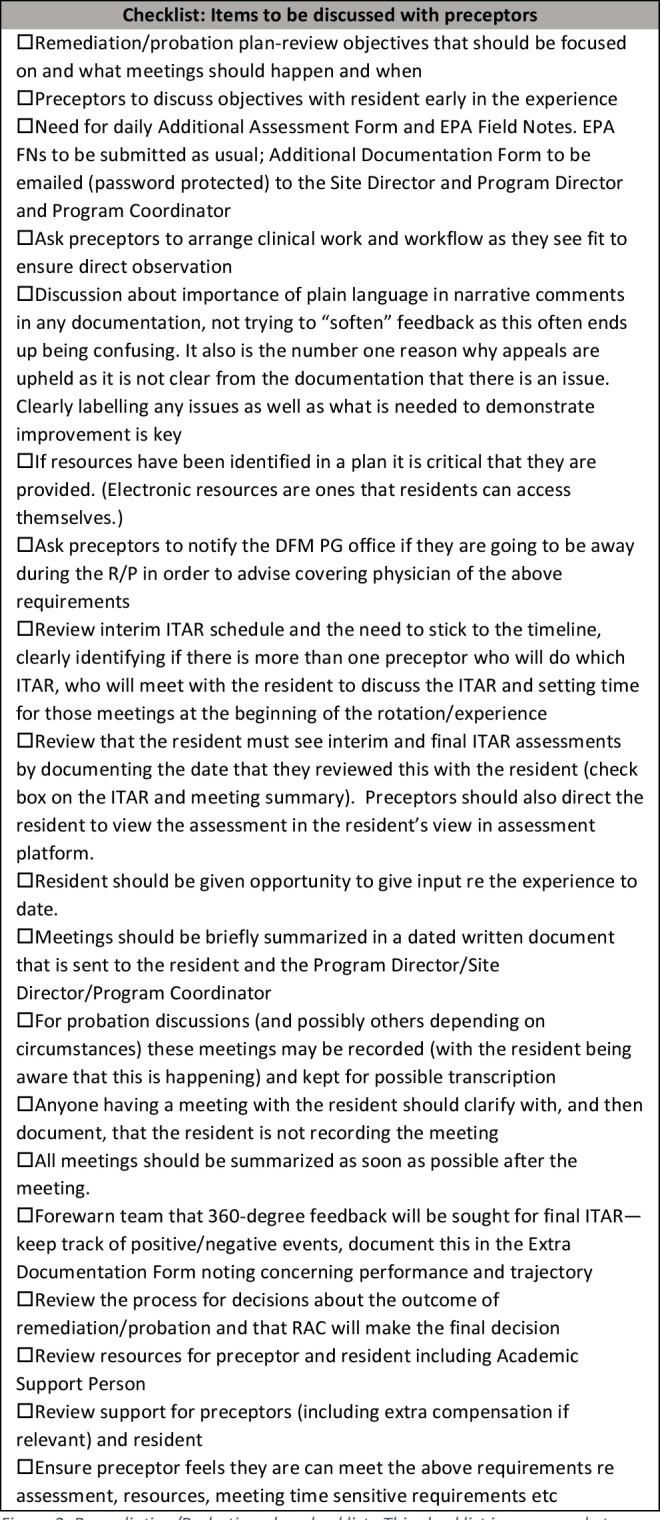
Remediation/Probation plan checklist. This checklist is an example to ensure all key aspects of a remediation/probation are carried out and important aspects are reviewed with preceptors. (AA=Academic Advisor, AC=Assessment Coordinator, APA=PGME Assessment Promotion and Appeals Policy, AD=Assessment Director, ASP=Academic Support Person, PC=Program Coordinator, PD=Program Director, PGEC=Department of Family Medicine’s Postgraduate Education Committee, PGMEC=University Faculty of Health Sciences Postgraduate Medical Education Committee, RAC=Resident Assessment Committee, SC=Site Coordinator, SD=Site Director) *Resident Information Package is a local resource for residents outlining the remediation/probation process, relevant learning resources and an article on how to receive feedback. **Preceptor Information Package is a local resource for preceptors outlining the remediation/probation process, local teaching resources and best feedback information
Recommendation 9: carry out the plan
As the plan is being executed it is critical to pay scrupulous attention to all elements of the plan. Assessments and meetings must happen when scheduled (it is advisable to build in some flexibility by not establishing a set date but by stating an interval (e.g. “1/3 of the way through the remediation or as close to as possible”)). Using a work-flow plan (Appendix A) listing steps, dates to be done by, and the person/people responsible for checking completion can help prevent procedural lapses. Redundancy of responsibility is useful for time-sensitive items so that two people (e.g. the program director and program assistant) are checking these happen as planned (assume busy preceptors will lose track of time!). This minimizes the risk of these being missed due to vacations, busy periods, etc.
R/P is stressful for everyone. Offering residents support through third party counselling, encouraging them to reach out to other support networks and their family physician, and asking preceptors to watch for evidence of escalating stress is essential. Preceptors are also often stressed. Their role in R/P and its stakes are different from their usual precepting. Contacting them regularly, not only to ensure that they continue to feel able to carry out the R/P plan but to offer support, is important. R/P is also stressful for the program director, again highlighting the importance of bringing concerns early to a larger group rather than having this sit solely with the program director.
Recommendation 10: determine the outcome
It can be helpful to take away the ultimate responsibility for the weighty and distressing decision about a failed R/P from the preceptor, many of whom are reluctant to make this decision,5 and instead have the program assessment committee decide this (i.e. preceptors assess the R/P as either “passed” or “requires committee review”). Having this neutral body review the information and invite resident input prior to a final decision is also an important part of fair process. The minutes of this meeting will be subpoenaed should the outcome be appealed. There will need to be quorum (if some are joining in by phone they will need to verbalize and have documented their presence at the beginning and end of the meeting) and the terms for the decision-making process for the committee followed. Minutes should be carefully reviewed, keeping in mind that if the outcome is appealed, it will be legally scrutinized, before being formally accepted.
Conclusion
This article has built on the recommendations in Part One of this series and will lead into Part Three. For the minority of residents requiring formal remediation or probation a plan that addresses the concerns identified in a way that is achievable in the realities of the busy clinical environment and is understood and agreed to by all will be necessary. This will require scrupulous attention to carrying out all aspects of the plan at the time(s) outlined. Redundancy of responsibility (resident, preceptors, administrators) will help ensure all aspects of the plan are addressed. Anytime the outcome of the plan impacts a resident’s career trajectory they have the right to appeal that decision. Most institutions will have levels of appeal, ranging from within the program to the dean of the medical school and/or the larger institution (university and/or hospital). The last article in this series will provide recommendations regarding those appeals.
Appendix A. Workflow: remediation and probation (r/p) rotations
Resident:
Rotation:
Primary supervisor:
Academic Advisor:
Site Director:
| Workflow Stage | Who oversees | Completed (date) | Comments |
|---|---|---|---|
| Stage One: Problem Identification – Process Initiation | |||
| i) Review situation at RAC, review and implement university APA | AC to add to agenda, RAC | ||
| ii) Prepare R/P plan, daily additional assessment form (to match R/P plan objectives) | PD and SD and/or ASP | ||
| iii) Determine preceptors and confirm | PD and/or SD | ||
| iv) +/- request to PGME for funding if applicable and resident needs extra supervision | PD or SD and PC | ||
| v) Communicate with resident (cc AA) to arrange meeting re next steps, supports. | PD or SD | ||
| Stage Two: Finalize Plan & Support Process | |||
| i) Send plan to EAB and revise as needed | PD | ||
| ii) Share revisions with RAC | PD | ||
| iii) Review final plan with resident; have them initial each page and sign 2 copies. Provide copy to resident. Provide resident with Information Package for Residents on Remediation or Probation*. | PD or SD | ||
| iv) Signed plan to PC | PD or SD | ||
| v) Signed plan to PGME with a copy to the resident’s file | PC | ||
| Stage Three: Working with Preceptor/Team & Resident Follow-up | |||
| i)Send a copy of the final plan + assessment form(s) + meeting template to preceptor(s), AA, SD and SC +/- ASP if they are involved in the plan. | PD or SD and PC | ||
| ii)Send the Information Package for Preceptors** to the preceptors. | PD or SD and PC | ||
| iii) If changes to schedule required (e.g. temporary hold or extra supervision on call) send information to those in charge of the call schedule and notify preceptor(s) on call. | PC and/or SC | ||
| iv) Ask preceptors to arrange clinical work and workflow as they see fit to ensure direct observation | PD or SD | ||
| v) If applicable to support other residents, inform locum organizer re: clinical coverage needs | PD or SD and/or PC or SC | ||
| vi) Ask preceptor and relevant administrative assistants to block time in calendars for meetings as outlined in the R/P Plan (e.g. with PD, SD, AA, preceptors) | PD or SD and/or PC or SC | ||
| vii) Ask resident to review plan with preceptors on day one and to schedule meeting times as outlined in the R/P plan (e.g. with preceptor, AA, PD, SD) | PD or SD and Resident | ||
| vi) Plan phone call or meeting with preceptor(s) to review R/P (see checklist below for items to cover) | PD or SD | ||
| Stage Four: During the rotation/experience | |||
| i) Resident to summarize meetings with preceptors and PD/SD as soon as possible after the meeting and send summaries by password protected email to PD and SD and PC | Resident and PC | ||
| ii) Preceptors to keep additional assessment forms and email (password protected) or arrange for secure pick-up | Preceptor to send and PD or SD and PC to ensure they are receiving these | ||
| iii) Set assessment system to send interim and final ITARS as per plan | PC and AC | ||
| iv) Email preceptor if ITARs and/or meeting records (from preceptor, AA, PD and/or SD) are not received within 2 days of timeline | PC | ||
| Stage Five: Outcome Management | |||
| i) Review outcome at RAC, ensure AA is informed of outcome | RAC/AC | ||
| ii) Inform PGEC of outcome | AD | ||
| iii) Outcome document to EAB | PD or SD and PC | ||
| iv) Outcome letter to Post Grad Associate Dean | AD or PD | ||
Footnotes
Conflicts of Interest: The Authors do not have any conflicts of interest to declare.
Funding: There was no funding for this work
References
- 1.Schultz K, Risk A, Newton L, Snider N. Program foundations and beginning of concerns (part one of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training. Can Med Ed J. 2021. 10.36834/cmej.70170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schultz K, Risk A, Newton L, Snider N. The appeal process and beyond (part three of 3) When residents shouldn’t become clinicians: Getting a grip on fair and defensible processes for termination of training. Can Med Ed J. 2021. 10.36834/cmej.72736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sardar v. University of Ottawa, 2014ONSC 3562.
- 4.Ramani S, Krackov S. Twelve tips for giving feedback effectively in the clinical environment, Med Teach. 2012; 34:10, 787-791, 10.3109/0142159X.2012.684916 [DOI] [PubMed] [Google Scholar]
- 5.Yepes-Rios M, Dudek N, Duboyce R, Curtis J, Allard RJ, Varpio L. The failure to fail underperforming trainees in health professions education: a BEME systemic review : BEME guide 42. Med Teach 2016; 38: 1092-1099. 10.1080/0142159X.2016.1215414 [DOI] [PubMed] [Google Scholar]


