Implication Statement
The COVID-19 pandemic resulted in changes to clinical clerkship delivery including decreased surgical exposure. The Department of Obstetrics and Gynaecology at Dalhousie University developed a novel, resident-led learning experience using a curated presentation of operative footage. This session aimed to improve medical students’ orientation to the operative environment and supplement teaching on pelvic anatomy and gynaecologic surgery in response to decreased exposure during the COVID-19 pandemic. Medical students perceived this session as valuable and felt it improved their preparedness for the operating room. This initiative has the potential to improve medical student orientation to the operative environment.
Énoncé des implications de la recherche
La pandémie de la COVID-19 a entraîné des changements dans le déroulement des stages d’externat, notamment une diminution l’exposition clinique en chirurgie. Le département d’obstétrique et de gynécologie de l’Université Dalhousie a mis au point une activité d’apprentissage novatrice, dirigée par des résidents, au moyen d’une présentation de vidéos opératoires. La séance visait à faciliter l’accueil des étudiants en médecine dans l’environnement opératoire, ainsi qu’à compléter l’enseignement de l’anatomie pelvienne et de la chirurgie gynécologique compte tenu de l’exposition clinique réduite pendant la pandémie de la COVID-19. Les étudiants ont jugé cette séance utile et ils s’estiment, grâce à elle, mieux préparés pour la salle d’opération. Cette initiative a le potentiel d’améliorer l’accueil des étudiants en médecine dans l’environnement opératoire.
Introduction
COVID-19 posed unprecedented challenges to medical education including the temporary interruption of clinical clerkship in Canada. With medical students’ subsequent reintegration into clinical training, educators required creativity and innovation to deliver adequate education during truncated rotations.1
Positive surgical experience is integral to medical students’ consideration of surgical disciplines.2 The operating room (OR) poses particular challenges to promoting these positive experiences including a unique physical environment, unclear relevance to clerkship learning objectives, and hierarchical social relations.3 Medical students’ failure to understand team members’ roles and OR routines may hinder their pace of learning in this environment.4 Equipping medical students to navigate the OR setting and promoting a positive experience `is particularly crucial in the setting of condensed rotations. Providing effective orientation and introducing concepts in environments with gradually increasing fidelity are established methods of preparing medical students for these novel experiences.5,6
Innovation
We developed a resident-led, “virtual OR” session for medical students that provides an orientation to the OR and an overview of clerkship objective level pelvic anatomy and gynaecologic surgery in a lower fidelity environment. We delivered this session to students prior to their gynaecologic surgery clinical experience.
A resident-staff team compiled recordings of common gynaecologic surgeries from YouTube and the American Association of Gynecologic Laparoscopists (AAGL) surgical video repository. A staff member had an existing AAGL membership, so there was no cost to the creation of this resource. Publicly available videos accessible through YouTube would also provide sufficient content. The team spent approximately 3-4 hours reviewing videos to ensure they were relevant and chose 1-2 minutes from each video to create a series of high yield clips. These videos were embedded into a PowerPoint presentation (Microsoft Office 365 for Mac 2019) with accompanying slides that addressed OR etiquette, patient positioning, pelvic anatomy, common procedures, and pre/postoperative considerations. These topics were identified via team consensus based on medical student rotation feedback and feedback from faculty, residents, and OR nursing staff.
We delivered the “virtual OR” as a compulsory teaching session using a remote learning platform during the first week of the obstetrics and gynaecology (Ob/Gyn) rotation for all medical students in the Class of 2021 who completed their rotation after clerkship resumed. We played the clips on mute so that residents could provide accompanying live commentary that included a review of the medical student’s role, tips for success, and relevant clerkship objectives for each topic. We encouraged students to ask questions and integrate prior operative exposure. A faculty member supervised the sessions.
Evaluation
When clerkship resumed in June 2020, the Dalhousie Ob/Gyn clerkship rotation length decreased from six to four weeks. Medical students previously had six to eight days of gynaecologic operative experience. This decreased to two days due to OR slow-downs and shorter rotations.
Thirty-two medical students from the Class of 2021 completed their Ob/Gyn rotation during the study period and attended the “virtual OR” session and were therefore eligible to participate. Nineteen students responded to the survey (19/32, 59% response rate). We obtained IWK REB approval for this study (No. 1026302).
Eighty-four percent (16/19) of participants felt that this session was helpful or very helpful to their learning about surgical gynaecology. Most participants (18/19, 95%) felt that it made them more prepared to attend gynaecologic ORs. All participants felt that the content was an appropriate level for clerkship students (Figure 1).
Figure 1.
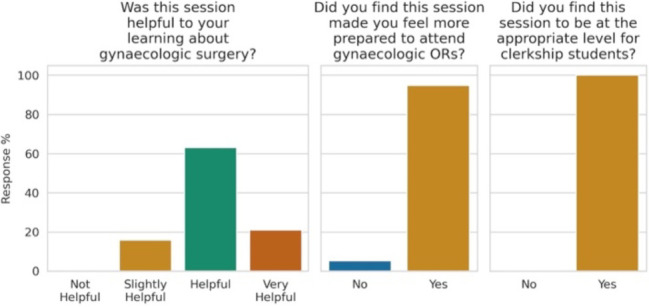
Medical students’ evaluation of the “Virtual OR” session
Next steps
This novel teaching session to enhance medical students’ gynaecologic surgical experience during the COVID-19 pandemic helped to fulfill goals of orienting medical students to the OR environment, and introducing gynaecologic surgery and pelvic anatomy learning objectives in a lower fidelity environment prior to students’ introduction to the gynaecology OR. We hypothesize that this session contributed to learner perception of preparedness by addressing unit-specific knowledge and roles and expectations. These reflect domains of orientation that learners identified as contributing to preparedness in a prior study.6 Further, this lower fidelity “virtual OR” experience helps to decrease the number of unfamiliar elements of the clinical operative experience, thereby decreasing cognitive load and allowing learning to happen more effectively. This gradual increase in fidelity reflects the best practices for decreasing cognitive load.5 Future work should evaluate how students perceive this learner-centered session contributes to their feelings of preparedness and could explore learners’ experience of transitioning to this novel environment through qualitative methods.
Acknowledgments
Acknowledgements: Janet Slaunwhite for her assistance in survey administration and Dr. Finlay Maguire for his assistance in figure creation.
Footnotes
Conflicts of Interest: None.
Funding: None.
References
- 1.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131. 10.1001/jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 2.Marshall D, Salciccioli J, Walton S-Jet al.. Medical student experience in surgery influences their career choices: a systematic review of the literature. J Surg Educ. 2015May;72(3):438–45. 10.1016/j.jsurg.2014.10.018 [DOI] [PubMed] [Google Scholar]
- 3.Lyon P. Making the most of learning in the operating theatre: student strategies and curricular initiatives. Med Educ. 2003August;37(8):680–8. 10.1046/j.1365-2923.2003.01583.x [DOI] [PubMed] [Google Scholar]
- 4.Poncelet A, O’Brien B. Preparing medical students for clerkships: a descriptive analysis of transition courses: Acad Med. 2008;83(5):444–51. 10.1097/ACM.0b013e31816be675 [DOI] [PubMed] [Google Scholar]
- 5.Leppink J, Duvivier R. Twelve tips for medical curriculum design from a cognitive load theory perspective. Med Teach. 2016;38(7):669–74. 10.3109/0142159x.2015.1132829 [DOI] [PubMed] [Google Scholar]
- 6.Beavers L, Christofilos V, Duclos Cet al. Perceptions of preparedness: How hospital-based orientation can enhance the transition from academic to clinical learning. Can Med Educ J. 2020;11(4):e62-e69. 10.36834/cmej.61649 [DOI] [PMC free article] [PubMed] [Google Scholar]


