Implication Statement
The COVID-19 pandemic has limited in-person experiences for medical students, especially in situations involving aerosol-generating procedures. We designed a video in situ simulation to orient students to critical steps in COVID-19 intubation algorithms. Small groups of students were paired virtually with facilitators (faculty and residents) and watched a video of an in situ simulation of emergency staff performing a protected intubation, with discussion points appearing on screen at discrete times. The simple design drives engagement, discussion and allows for scheduling flexibility with no risk to the learners. It can be adapted to several different scenarios or levels of training.
Énoncé des implications de la recherche
La pandémie de la COVID-19 a limité les expériences en personne pour les étudiants en médecine, en particulier les interventions qui produisent des aérosols. Nous avons conçu une simulation in situ par vidéo portant sur les étapes critiques des algorithmes de l’intubation dans les cas de COVID-19. De petits groupes d’étudiants, jumelés virtuellement avec des animateurs (enseignants et résidents), ont regardé une vidéo de la simulation in situ d’une intubation sécuritaire effectuée par une équipe d’urgence. À des moments précis de la simulation, des points de discussion apparaissaient à l’écran. Cette formule simple, sans risque pour les apprenants, favorise l’engagement et la discussion et elle permet la planification en toute souplesse. Elle peut être adaptée à plusieurs scénarios et à divers niveaux de formation.
Introduction
The COVID-19 pandemic and resultant physical distancing requirements have greatly restricted clinical education and training.1 Simulation, often used to expose medical students to high-acuity cases, has been particularly affected.2 Various groups have adapted simulation to online formats to safely comply with physical distancing.3 Based on a previously described video in situ simulation used for protected intubation protocol development,4 we adapted this model for medical students.
Innovation
In small groups, students viewed a video-recorded in situ simulation via teleconference under the guidance of a resident or staff physician. The nine-minute video followed a patient with respiratory failure secondary to COVID-19 requiring intubation. It was recorded in situ with clinicians, including nurses, respiratory therapists and physicians, in their native environment and without interruptions or prompting. Integrated within the video were six-freeze frames with discussion points aligned with video content. For example, the first point pertains to team members involved in protected intubations and appears on the screen as the team lead assigns roles (Figure 1). This encourages students to reflect on what they had seen in real time while providing opportunities for discussion. Teaching points were tailored to medical students, and included: protected intubation principles, crisis resource management principles including closed-loop communication, and use of negative pressure rooms and personal protective equipment.
Figure 1.
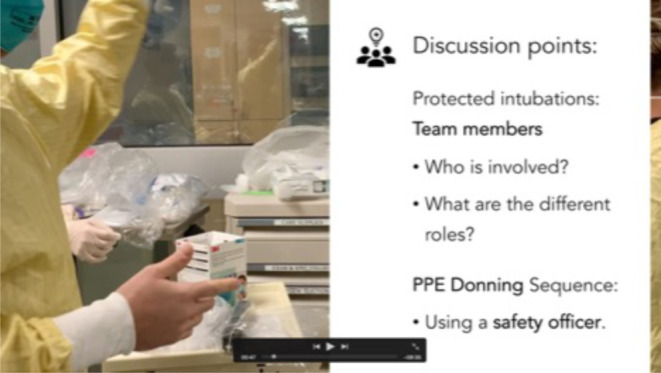
Screen shot of the video depicting the first freeze-frame with discussion points.
The right-sided bar appears as the video content pauses and prompts the group lead to guide the group through relevant discussion points. These discrete pauses also allow for group check-ins, giving participants the opportunity to ask questions throughout (as opposed to end-of-simulation debrief).
This session was integrated into the emergency medicine core clerkship at McMaster University, in part replacing in-person simulation sessions that were limited by distancing requirements. While medical students are currently not participating in the care of COVID-19 patients at McMaster, they will rapidly transition to residency where they will be expected to care for these patients. Therefore, this simulation served as a key introduction to the principles of resuscitation of COVID-19 patients.
Evaluation
We collected feedback assessing learner comfort from two cohorts of students using pre- and post-session surveys. McMaster HiREB granted an ethics exemption for this data collection. Of the 45 participants, 15 paired surveys were returned, representing a response rate of 33%. Most survey respondents (14/15, 93%) either agreed or strongly agreed that the learning atmosphere was comfortable, and 67% (10/15) either agreed or strongly agreed that it was easy to get actively involved in the session. When comparing pre-and post-session surveys, 93% of respondents reported an increased level of comfort with protected intubation following the session.
Conclusions
This student-led initiative represents a novel and low-stakes means of introducing junior medical learners to simulation and protected intubations, while circumventing issues related to the COVID-19 pandemic. Preliminary data suggest that the session provided a safe and effective learning environment. Compared to the benefits of traditional scripted education videos on learning and motivation, this offers the additional advantage of increased interactivity and exposure to unscripted errors and debriefs unique to simulation.5,6 Limitations to implementation relate to technical requirements and the ability to facilitate the initial simulation. Interpretation of results is limited by their subjective nature, thus necessitating future evaluation of objective learning outcomes. Given the ease of use and safety for learners, this design can be expanded to other topics.
Footnotes
Funding: There was no funding for this work
References
- 1.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131-2132. 10.1001/jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 2.Heitz C, Ten Eyck R, Smith M, Fitch MT. Simulation in medical student education: survey of clerkship directors in emergency medicine. West J EM. 2011;12(4):455-460. 10.5811/westjem.2011.3.2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaplin T, McColl T, Petrosoniak, Koch Hall A. “Building the plane as you fly”: simulation during the COVID-19 pandemic. CJEM 2020; epub:1-3, 10.1017/cem.2020.398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanel E, Bilic M, Hassall K, et al. Virtual application of in situ simulation during a pandemic. CJEM 2020; epub:1-6, 10.1017/cem.2020.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young TP, Guptill M, Thomas T, Mellick L. Effective Educational Videos in Emergency Medicine. AEM Educ Train. 2018; 2(Suppl Suppl 1): S17-S24. 10.1002/aet2.10210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi HJ, Johnson SD. The effect of context-based video instruction on learning and motivation in online courses. Am J Dist Educ. 2005;19:215–227. [Google Scholar]


