This is the first of a two-part editorial on the chronic overcrowding in medical school curricula, the implications. In the second part, we will describe some barriers and outline a strategy for moving forward.
Introduction
2020 and 2021 were tremendously challenging years for medical schools across the globe as they responded to the COVID-19 pandemic. In addition, the societal upheavals that ensued from the racial reckoning precipitated by the murder of George Floyd sent tremors not just throughout the United States but to every corner of the world. These events have prompted medical schools to examine their own cultures, learning environments, and curricula, and have led to an old challenge dressed up in new clothes: How to fit all of the new potential curricular content associated with these past pandemic years into an already overcrowded curriculum? There is substantial clinical and scientific content related to COVID-19 but there’s also vaccine hesitancy, underfunding of the public health system, failures in disaster preparedness, and understanding and addressing the social determinants of health.
There seems to be no end to the relevant new content that needs to be included; but where do we fit it in and how? We believe we need to first address the current level of overcrowding in medical school curricula while we make room for vital new topics.
In this perspective we will: 1) review the history and persistence of overcrowding in the medical curriculum, 2) describe the impact of content overload on student learning and well-being, 3) speculate on prominent sources of resistance to reducing content, and 4) suggest how we may approach such resistance in order to produce balanced curricula that can admit new crucial content.
Concerns about excessive content and curricular overcrowding in medical education have existed for more than a century. In 1910, Abraham Flexner noted that the packed medical school curriculum would “tax the memory, not the intellect.”1 The Rappleye Commission Report on Medical Education published in 1932 stated that “the almost frantic attempts to put into the medical course teaching in all phases of scientific and medical knowledge, and the tenacity with which traditional features of teaching are retained have been responsible for great rigidity, overcrowding, and a lack of proper balance in the training.”2 Since then, periodic concerns have been raised about this ongoing problem, notably in the Association of American Medical Colleges' Panel on the General Professional Education of the Physician (GPEP report) in 1984 and the Assessing Change in Medical Education (ACME-TRI) report in 1993, among others.3-6
The problem has only worsened in the years preceding the pandemic. New pharmaceutical agents seem to appear daily, while our understanding of pathophysiology of disease continues to expand. In addition, we have needed to consider new and vital subjects such as cultural competence, care of LGBTQ patients, teamwork and interprofessional care, health care quality and safety, medical humanities, narrative medicine, and even wellness curricula, that have added pressure to the preclerkship phase of medical school, as ever more content is added. And little has been removed.
We see little evidence that medical schools have taken effective steps to address this content overload problem. This is a problem of “filter failure.” Medical education leaders who are empowered to make decisions about what is most important to teach have not successfully managed the content. This failure has allowed the curriculum to become bloated.7 Jamshidi and Cook stated plainly that medical education lacks a functioning excretory system.5 We need more than that, but let’s start with a nutrition plan.
Implications for learning
Students often describe the preclerkship curriculum as a binge/purge experience in which they stuff as many facts as possible into their heads before each exam, and then feel that much of this knowledge decays rapidly as they face the next flood of material preceding the ensuing exam. Many students feel like their memory is poor, when in reality, the decline in knowledge simply reflects the human capacity to store information in long-term memory. Long-term memory requires time to develop deep understanding of the main ideas through semantic learning.8 The precipitous decline in knowledge is a predictable (but unnecessary) product of the overcrowded curriculum. Shooting content from a water cannon forces students into surface learning and short-term memory. Indeed, in three studies of long-term retention of basic science material (ranging from one to three years later), the failure rate on reexamination was an astounding 90%.9-11 Medical schools pump out ever more content in increasing detail thus denying students the time and energy to learn important material so that it lasts.
Additional analogical evidence exists that excessive amounts of content harm student learning and retention. Many cleave to the false belief that if we teach more content then students will learn and retain more. In no human endeavor do outcomes continue to rise with an increase in one variable. The Yerkes Dodson Curve elegantly captures this principle.
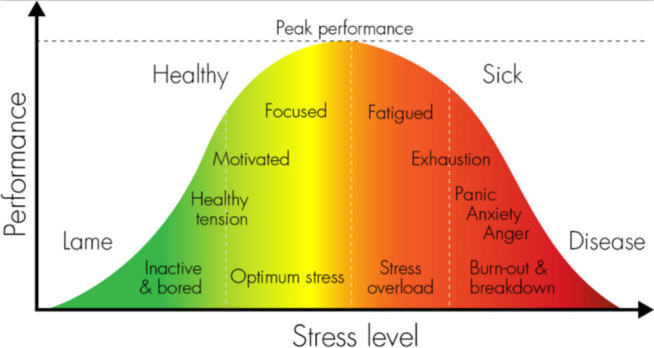
Figure 1
Stress on the horizontal axis can be replaced by the amount of information taught. The experience of many students in the preclerkship phase is that they live too far on the right side of the Yerkes Dodson curve. Not only does their learning suffer, their mental health does as well, as we describe in the next section.
Implications for well-being
In recent years, more researchers have reported high rates of depression burnout, suicidal ideation, and psychological distress among medical students.12-14 The sheer volume of information we teach students in the preclerkship years is a major source of distress even in pass/fail schools.13,14 The negative impact of content overload on vulnerable populations of students (first to attend college and students from populations underrepresented in medicine) is likely even greater.
Medical schools have consequently ramped up their well-being efforts, focusing much of their attention on promoting well-being through individual strategies such as mindfulness, yoga, encouraging exercise and healthy diets, and stress-management activities. Unfortunately, these initiatives and programs seem to be having little positive impact on student well-being.12.14 Perceived stress, exhaustion, and disengagement as measured by the AAMC Y2Q survey have all worsened in three recent years despite the multitude of well-intentioned well-being initiatives.15,16
We believe that we are unlikely to significantly or materially improve student mental health in the preclerkship phase until we begin to view the problem as an environmental health issue. The answer is not to task students to learn how to manage the distress that we cause them or fail to prevent through our inability or unwillingness to curate effectively the content we insist they master. We need to mitigate the main drivers of distress for preclerkship students by substantially reducing and better managing the amount and nature of the content that we teach.
In the next issue, we will complete our editorial by looking at some of the barriers to change and mapping a strategy for moving forward.
One entire special issue will be devoted to articles related to the change process and managing barriers to change. In this regular issue we offer a wide variety of topics from what patients think about helping to train the next generation of doctors to the plight of IMGs in a Canadian health care system that needs more physicians. We hope you enjoy the articles in this issue which may whet your appetite for reading about ways to facilitate the transformation of the medical education enterprise.
Major Contributions
In the article, A qualitative study of patients’ and caregivers’ perspectives on educating healthcare providers by Holly Adam and co-authors,19 they studied what patients thought about their involvement in the education of healthcare providers. Their results highlighted that many patients wanted to be involved in healthcare education in a meaningful way.
In Examining the accuracy of residents’ self-assessments and faculty assessment behaviours in anesthesiology,20 Cofie and co-authors considered the accuracy of residents’ self-assessed global entrustment scores and compared whether self-assessed scores differed from faculty assessed scores. Their findings showed that two out of three resident self-assessments were inaccurate and that residents are often under-confident in their assessments.
Motor vehicle incidents in postgraduate trainees in British Columbia by Louise Cassidy and co-authors21 determined the number of motor vehicle incidents (MVIs) during the commutes of medical trainees. They found that two thirds of trainees reported that the safety of their commute had been impacted by fatigue, and trainees with longer and more frequent commutes had an increased risk of MVIs. They concluded that their results called for safer alternatives for trainee commutes.
Not wanted on the voyage: highlighting intrinsic CanMEDS gaps in Competence by Design curricula by Joan Binnendyk and team22 evaluated national Canadian curricula to determine representation for each enabling CanMEDS competency. Their results showed which competency roles were less frequently mapped. They hoped that early identification of these gaps will lead to assessing how to best teach the underrepresented competencies.
Developing a dashboard for faculty development in competency-based training programs: a design-based research project by Yilmaz et al.23 identified the needs of faculty members within a Competency Based Medical Education (CBME) system and created a prototype dashboard to meet them. They focused on visualizing faculty assessment data to support faculty development within competency-based programs. They anticipate faculty dashboards will become an important part of CBME programs as institutions advance their use of data.
Brief Reports
Comparison of perceived educational value of an in-person versus virtual medical conference by Chan et al.24 compared perspectives from a 2019 in-person medical conference with the subsequent virtual conference held in 2020. They found that while the virtual conference was more accessible to attendees, the in-person conference better met overall learning objectives.
Community organization feedback about an undergraduate medical education service learning program by Berrington and team25 reported on the feedback from community organizations involved with service learning about their experiences working with undergraduate students. They hope the feedback, such as sharing learning objectives with community partners, will lead to further discussion and improvements for the SL program.
Impact of accreditation on Caribbean medical schools’ processes by Arja et al.26 surveyed medical school leaders’ perceptions of the Caribbean medical school accreditation mandate. Their results showed unanimous support for the accreditation requirement and felt it was an opportunity for growth and improvement within their programs.
In their work, Criteria for selection to anesthesia residency programs: a survey of Canadian anesthesia program directors, Niburski and Buu identified desired attributes of anesthesia applications through a survey of anesthesia program directors. Their survey reported that program directors valued candidates with good academic performance and anesthesia elective experience as the most important aspects of the application package.
Review Papers and Meta-Analyses
Impact of physical therapy and occupational therapy student placements on supervisor productivity: a scoping review by Coleman and co-authors28 mapped the impact of physical and occupational therapy student placements on the time and productivity of supervisors. The reviewed studies suggested that the supervision of students does not negatively impact productivity despite clinicians perceiving that students slow them down.
Black Ice
In their article, Six ways to get a grip by calling-out racism and enacting allyship in medical education by Lyn Sonnenberg and team,29 they provided tips on ways to practice allyship, promote inclusivity, and actively support equity and diversity. They hope that their guide can be a starting point for recognizing racism and advocating for change in medical education and beyond.
Program foundations and beginning of concerns (part one of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training,30 Formal remediation and probation (part two of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training,31 and The appeal process and beyond (part three of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training32 by Karen Schultz and co-authors is a three-part series that presented steps for terminating resident training that is fair for both the learner and the program. Their steps intended to reduce academic decisions being overturned, and delays to the resident finding another career path.
Canadiana
When a Canadian is not a Canadian: marginalization of IMGs in the CaRMS match by Malcolm MacFarlane33 presented an overview of the Canadian Residency Matching Service Match (CaRMS) system, evidence of Internal Medical Graduate (IMG) marginalization within the system, and human rights implications of the current CaRMS system. He concluded by offering suggestions for changes to the current system to bring the process more in line with Canadian values.
You Should Try This
Video in situ simulation for medical student education during the COVID-19 pandemic by Monika Bilic and team34 described a student-led initiative using a video in situ simulation to orient students to critical steps in COVID-19 intubation. They found that the simulation was safe, easy to use, and led to increased engagement.
In their article, Hybrid-virtual simulations for Canadian medical students during the COVID-19 pandemic, Reels et al.35 developed virtual simulations where remote learners directed an in-person assistant. This hybrid model allowed students to practice real-time clinical decision-making while still abiding by public health guidelines. They found that their approach was more engaging than entirely virtual simulations and could be used in the future for rural healthcare students without local simulation centres.
Evaluating and implementing an opportunity for diversity and inclusion in case-based learning by Bowden, Kirubarajan, and co-authors36 used a student-developed framework to determine the social identity of fictional patients in case-based learning (CBL) cases. Their innovation, which included creating a diverse name bank as a resource for naming the fictional patients, aimed to improve the diversity of social identities in their curriculum and prepare students for diversity in clinical practice.
The “virtual OR:” creation of a surgical video-based gynaecologic surgery teaching session to improve medical student orientation and supplement surgical learning during COVID-19 by Jocelyn Stairs and co-authors37 outlined a resident-led “virtual OR” session for medical students that provides an orientation of the OR through operative footage. This learning experience was a valuable supplemental learning experience for medical students, and it increased their preparedness in the operating room.
Works-in-Progress
Examining student perceptions of a COVID-19 service-based learning elective by Button and Cameron38 described an opportunity to dispense the COVID-19 vaccine across Northern First Nations fly in/remote communities. They will examine the relationship between social accountability and a service-based learning experience.
Images
In her collage, Plastic waters, plastic land. Pandemic pollution,39 Efthimia Kosmas expressed concern over the increased pollution from single-use masks. She created a poster made of masks she used over the course of two months to demonstrate that while masks are an essential item in the protection against COVID-19, they are also damaging the ecosystem.
Our cover image from Miao and Miao, A doctor’s compassionate touch40 featured photography and digital watercolor painting. It symbolized the bond between a physician and patient during end of life care.
Conferences
Finally, A new world of residency education: game changers and proven practices41 contains the abstracts from the 2021 Virtual International Conference on Residency Education.
Enjoy!
Marcel D’Eon, MEd, PhD
Editor, CMEJ
References
- 1.Flexner A. Medical education in the united states and Canada: a report to the Carnegie Foundation for the advancement of teaching. New York: Carnegie Foundation; 1910. [PMC free article] [PubMed] [Google Scholar]
- 2.Rappleye WC. Medical education: final report of the commission on medical education. New York: Association of American Medical Colleges Commission on Medical Education; 1932. [Google Scholar]
- 3.Association of American Medical Colleges. Project panel on the general professional education of the physician, et al. Physicians for the twenty-first century: report of the project panel on the general professional education of the physician and college preparation for medicine. J Med Educ. 1984;59(11): 1-208. 10.1097/00001888-198411000-00001 [DOI] [PubMed] [Google Scholar]
- 4.Swanson AG, Anderson MB. Educating medical students. Assessing change in medical education–the road to implementation. Acad Med. 1993;68(6):S1-46. 10.1097/00001888-199306000-00014 [DOI] [PubMed] [Google Scholar]
- 5.Jamshidi HR, Cook DA. Some thoughts on medical education in the twenty-first century, Med Teach. 2003;25(3):229–238. 10.1080/0142159031000100256 [DOI] [PubMed] [Google Scholar]
- 6.D'Eon M, Crawford R. The elusive content of the medical-school curriculum: a method to the madness. Med Teach. 2005;27(8):699-703. 10.1080/01421590500237598 [DOI] [PubMed] [Google Scholar]
- 7.Asay M. “Shirky: problem is filter failure, not info overload.” CNET. 2009. https://www.cnet.com/news/shirky-problem-is-filter-failure-not-info-overload/ [accessed June 1, 2021].
- 8.Baddeley AD. The influence of acoustic and semantic similarity on long-term memory for word sequences. Q J Exp Psychol. 1966;18(4):302–9. 10.1080/14640746608400047 [DOI] [PubMed] [Google Scholar]
- 9.Mateen FJ, D’Eon MF. Neuroanatomy: a single institution study of knowledge loss. Med Teach. 2008;30(5):537-539. 10.1080/01421590802064880 [DOI] [PubMed] [Google Scholar]
- 10.Wilhelmsson N, Bolander-Laksov K, Dahlgren LO, et al. Long-term understanding of basic science knowledge in senior medical students. Int J Med Educ. 2013;4:193-7. 10.5116/ijme.5232.2de4 [DOI] [Google Scholar]
- 11.Schneid SD, Pashler H, Armour C. How much basic science content do second-year medical students remember from their first year? Med Teach. 2019February1;41(2):231-3. 10.1080/0142159X.2018.1426845 [DOI] [PubMed] [Google Scholar]
- 12.Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and metaanalysis. Jama. 2016;316(21):2214-36. 10.1001/jama.2016.17324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dyrbye LN, Lipscomb W, Thibault G. Redesigning the learning environment to promote learner well-being and professional development. Acad Med. 2020;95(5):674-8. 10.1097/ACM.0000000000003094 [DOI] [PubMed] [Google Scholar]
- 14.D’Eon M, Thompson G, Stacey A, et al. The alarming situation of medical student mental health. CMEJ. 2021. 10.36834/cmej.70693 [DOI] [PMC free article] [PubMed]
- 15.Slavin S. Reflections on a decade leading a medical student well-being initiative. Acad Med. 2019;94(6):771-4. 10.1097/ACM.0000000000002540 [DOI] [PubMed] [Google Scholar]
- 16.Wasson LT, Cusmano A, Meli L, et al. Association between learning environment interventions and medical student well-being: a systematic review. Jama. 2016;316(21):2237-52. 10.1001/jama.2016.17573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Medical School Year 2 Questionnaire, 2020. All Schools Summary Report https://www.aamc.org/media/52141/download [Accessed May 24, 2021]
- 18.Medical School Year 2 Questionnaire, 2018. All Schools Summary Report https://www.aamc.org/media/9931/download [Accessed May 24, 2021]
- 19.Adam H, Giroux C, Eady K, Moreau K. A qualitative study of patients’ and caregivers’ perspectives on educating healthcare providers. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Heer S, Cofie N, Gutiérrez G, Upagupta C, Szulewski A, Chaplin T. Shaken and stirred: emotional state, cognitive load, and performance of junior residents in simulated resuscitation Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cassidy L, Croft E, Erdelyi S, Brubacher J. Motor vehicle incidents in postgraduate trainees in British Columbia Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Binnendyk J, Pack R, Field E, Watling C. Not wanted on the voyage: highlighting intrinsic CanMEDS gaps in Competence by Design curricula. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.70950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yilmaz Y, Carey R, Chan T, et al. Developing a dashboard for faculty development in competency-based training programs: a design-based research project. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.72067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan A, Cao A, Kim L, et al. Comparison of perceived educational value of an in-person versus virtual medical conference. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berrington R, Condo N, Rubayita F, Cook K, Jalloh C. Community organization feedback about an undergraduate medical education service learning program. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arja SB, Arja SB, Fatteh S, Challa KT, Somagutta MKR, Blouin D. Impact of accreditation on Caribbean medical schools’ processes.Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niburski K, Buu N. Criteria for selection to anesthesia residency programs: a survey of Canadian anesthesia program directors. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coleman J, Knott K, Jung B. Impact of physical therapy and occupational therapy student placements on productivity: a scoping review. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.69298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sonnenberg LK, Do V, LeBlanc C, Busari JO. Six ways to get a grip by calling-out racism and enacting allyship in medical education. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schultz K, Risk A, Newton L, Snider N. Program foundations and beginning of concerns (part one of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.70170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schultz K, Risk A, Newton L, Snider N. Formal remediation and probation (part two of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.72735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schultz K, Risk A, Newton L, Snider N. The appeal process and beyond (part three of 3). When residents shouldn’t become clinicians: getting a grip on fair and defensible processes for termination of training. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.72736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacFarlane MM. When a Canadian is not a Canadian: marginalization of IMGs in the CaRMS match. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bilic M, Nagji A, Hanel E. Video in situ simulation for medical student education during the COVID-19 pandemic. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reel R, Gunther K, Kirk S, Landells D, Theilmann A, Haines M. Hybrid-virtual simulations for Canadian medical students during the COVID-19 pandemic. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bowden S, Kirubarajan A, Balbaa A, et al. Evaluating and implementing an opportunity for diversity and inclusion in case-based learning. Can. Med. Ed. J. 2021;12(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stairs J, Amir B, Vair B. The. “virtual OR:” creation of a surgical video-based gynaecologic surgery teaching session to improve medical student orientation and supplement surgical learning during COVID-19. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.72081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Button BL, Cameron E. Examining student perceptions of a COVID-19 service-based learning elective. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.72353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kosmas E. Plastic waters, plastic land. Pandemic pollution. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.72051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miao JH, Miao KH. A doctor’s compassionate touch. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.71177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.International Conference on Residency Education . A new world of residency education: game changers and proven practices. Can. Med. Ed. J. 2021;12(4). 10.36834/cmej.73400 [DOI] [PMC free article] [PubMed] [Google Scholar]


